Abstract
Background
Gout is a chronic and inflammatory form of arthritis that is often overlooked despite the associated pain caused by acute flares and associated joint damage caused by the development of debilitating tophi. The increasing burden of gout, due to an aging population and the increased prevalence of known risk factors for hyperuricaemia, means that there is a continued need for new and effective urate-lowering treatments. The evaluation of these treatments will require a comprehensive and comparative evidence base describing the economic and humanistic burden of gout, taken from the perspective of patients, the healthcare system, and wider society.
Objective
The objective of this study is to review and summarise the current evidence of the disease burden related to chronic gout, assessed in terms of both cost and health-related quality of life (HRQL), and to identify key factors correlated with an increased burden. The overall aim is to support the economic evaluation of new treatments for gout, and to highlight key data gaps that may need further study and exploration.
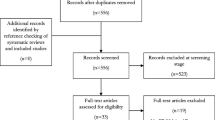
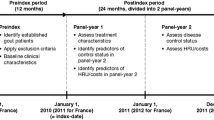
Methods
Relevant literature dating from January 2000 to July 2014 was sourced through searches of the MEDLINE database via PubMed and The Cochrane Library. Articles published in English and reporting either the economic burden (cost) or the humanistic burden (HRQL/utility) of gout were identified, and key data were extracted and summarised, with key themes and data gaps identified and discussed.
Results
Of the 323 studies identified, 39 met the inclusion criteria, of which 17 and 26 were relevant to the economic and humanistic burden, respectively. The economic burden of gout varied according to numerous factors, most notably serum urate acid levels and number of flares and tophi, resulting in higher healthcare resource use most often attributed to hospitalisation and inpatient stay. The incremental direct cost of gout has been suggested in the range of US$3165 to US$5515 (2004 and 2005 values, respectively) climbing to US$10,222 to US$21,467 (2008 values) per annum where patients are experiencing regular acute flares and have tophi present. The humanistic burden of gout was largely due to physical disability and pain resulting from chronic clinical manifestations. Short Form 6 dimensions (SF-6D) assessed utility weights are estimated at 0.53 for a patient with severe gout (≥3 flares/year and tophi) compared with 0.73 for an asymptomatic gout patient with serum acid levels <6 mg/dl.
Conclusions
The evidence confirms that gout has a growing overall prevalence and represents a significant burden in terms of both direct healthcare cost and HRQL outcomes. In light of this, effective urate-lowering treatments are likely to be valued if they can be clearly demonstrated to be both clinically effective and cost effective. Published data to support healthcare decision making in non-US countries with regards to treatments for gout are currently limited, which is a key limitation of the current evidence base. More research is also required to extend our understanding of the impact of gout on indirect costs, and a need also exists to develop a more comprehensive set of comparative HRQL utility assessments.

Similar content being viewed by others
References
National Health Service. NHS England advice on gout. 2014. http://www.nhs.uk/conditions/Gout/Pages/Introduction.aspx. Accessed 27 Aug 2014.
University of Maryland. Gout. 2014. http://umm.edu/health/medical/reports/articles/gout#ixzz3BzqKxW00. Accessed 1 Sept 2014.
National Health Service. NHS choices. Gout. 2014. http://www.nhs.uk/Conditions/Gout/Pages/Complications.aspx. Accessed 27 Aug 2014.
Roddy E, Doherty M. Epidemiology of gout. Arthritis Res Ther. 2010;12(6):223.
Rho YH, Zhu Y, Choi HK. The epidemiology of uric acid and fructose. Semin Nephrol. 2011;31(5):410–9.
Nuki G, Simkin PA. A concise history of gout and hyperuricemia and their treatment. Arthritis Res Ther. 2006;8(Suppl 1):S1.
Smith EU, Diaz-Torne C, Perez-Ruiz F, March LM. Epidemiology of gout: an update. Best Pract Res Clin Rheumatol. 2010;24(6):811–27.
Kuo CF, Grainge MJ, Mallen C, Zhang W, Doherty M. Rising burden of gout in the UK but continuing suboptimal management: a nationwide population study. Ann Rheum Dis. 2015;74(4):661–7.
Chen LX, Schumacher HR. Gout: an evidence-based review. J Clin Rheumatol. 2008;14(5 Suppl):S55–62.
Khanna D, Fitzgerald JD, Khanna PP, Bae S, Singh MK, Neogi T, et al. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res. 2012;64(10):1431–46.
Weaver AL. Epidemiology of gout. Cleve Clin J Med. 2008;75(Suppl 5):S9–12.
Doherty M. New insights into the epidemiology of gout. Rheumatology. 2009;48(Suppl 2):ii2–8.
Tausche AK, Jansen TL, Schroder HE, Bornstein SR, Aringer M, Muller-Ladner U. Gout–current diagnosis and treatment. Deutsches Arzteblatt Int. 2009;106(34–35):549–55.
Jordan KM, Cameron JS, Snaith M, Zhang W, Doherty M, Seckl J, et al. British society for rheumatology and british health professionals in rheumatology guideline for the management of gout. Rheumatology. 2007;46(8):1372–4.
Zhang W, Doherty M, Bardin T, Pascual E, Barskova V, Conaghan P, et al. EULAR evidence based recommendations for gout. Part II: management. Report of a task force of the EULAR standing committee for international clinical studies including therapeutics (ESCISIT). Ann Rheum Dis. 2006;65(10):1312–24.
US Food and Drug Administration. FDA Approves Colchicine for Acute Gout, Mediterranean Fever. 2009. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm174620.htm. Accessed 8 Apr 2015.
Khanna D, Khanna PP, Fitzgerald JD, Singh MK, Bae S, Neogi T, et al. 2012 American college of rheumatology guidelines for management of gout. Part 2: therapy and antiinflammatory prophylaxis of acute gouty arthritis. Arthritis Care Res. 2012;64(10):1447–61.
Pacher P, Nivorozhkin A, Szabo C. Therapeutic effects of xanthine oxidase inhibitors: renaissance half a century after the discovery of allopurinol. Pharmacol Rev. 2006;58(1):87–114.
Hande KR, Noone RM, Stone WJ. Severe allopurinol toxicity. Description and guidelines for prevention in patients with renal insufficiency. Am J Med. 1984;76(1):47–56.
Jennings CG, Mackenzie IS, Flynn R, Ford I, Nuki G, De Caterina R, et al. Up-titration of allopurinol in patients with gout. Semin Arthritis Rheum. 2014;44(1):25–30.
Riedel AA, Nelson M, Joseph-Ridge N, Wallace K, MacDonald P, Becker M. Compliance with allopurinol therapy among managed care enrollees with gout: a retrospective analysis of administrative claims. J Rheumatol. 2004;31(8):1575–81.
Robinson PC, Dalbeth N. Advances in pharmacotherapy for the treatment of gout. Expert Opin Pharmacother. 2015;16(4):533–46.
Crittenden DB, Pillinger MH. New therapies for gout. Annu Rev Med. 2013;64:325–37.
European Medicines Agency. Krystexxa, pegloticase. 2013. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002208/human_med_001591.jsp&mid=WC0b01ac058001d124. Accessed 8 Apr 2015.
US Food and Drug Administration. FDA approves new drug for gout. 2010. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm225810.htm. Accessed 8 Apr 2015.
AstraZeneca. AstraZeneca announces top-line results from the Phase III programme of lesinurad in combination with xanthine oxidase inhibitors in gout patients. 2014. http://www.astrazeneca.com/Media/Press-releases/Article/13082014–astrazeneca-announces-topline-results-from-the-phase. Accessed 8 Apr 2015.
AstraZeneca. Marketing Authorisation Application for gout treatment lesinurad accepted by European Medicines Agency. 2015. http://www.astrazeneca.com/Media/Press-releases/Article/20150122–marketing-authorisation-application-for-gout. Accessed 8 Apr 2015.
Edwards NL, So A. Emerging therapies for gout. Rheum Dis Clin N Am. 2014;40(2):375–87.
Drummond M, Sculpher M, Torrance G, O’Brien B, Stoddart G. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford University Press; 2005.
Jacobs P, Fassbender K. The measurement of indirect costs in the health economics evaluation literature. A review. Int J Technol Assess Health Care. 1998;14(4):799–808.
Organisation for Economic Co-operation and Development. PPPs and exchange rates. 2013. http://stats.oecd.org/Index.aspx?DataSetCode=SNA_Table4#. Accessed 18 Dec 2014.
Organisation for Economic Co-operation and Development. Consumer prices: consumer prices—annual inflation. 2014. http://stats.oecd.org/index.aspx?queryid=22519#. Accessed 18 Dec 2014.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Brook RA, Forsythe A, Smeeding JE, Lawrence Edwards N. Chronic gout: epidemiology, disease progression, treatment and disease burden. Curr Med Res Opin. 2010;26(12):2813–21.
Brook RA, Kleinman NL, Patel PA, Melkonian AK, Brizee TJ, Smeeding JE, et al. The economic burden of gout on an employed population. Curr Med Res Opin. 2006;22(7):1381–9.
Wu EQ, Patel PA, Yu AP, Mody RR, Cahill KE, Tang J, et al. Disease-related and all-cause health care costs of elderly patients with gout. J Manag Care Pharm. 2008;14(2):164–75.
Halpern R, Fuldeore MJ, Mody RR, Patel PA, Mikuls TR. The effect of serum urate on gout flares and their associated costs: an administrative claims analysis. J Clin Rheumatol. 2009;15(1):3–7.
Halpern R, Mody RR, Fuldeore MJ, Patel PA, Mikuls TR. Impact of noncompliance with urate-lowering drug on serum urate and gout-related healthcare costs: administrative claims analysis. Curr Med Res Opin. 2009;25(7):1711–9.
Hanly JG, Skedgel C, Sketris I, Cooke C, Linehan T, Thompson K, et al. Gout in the elderly–a population health study. J Rheumatol. 2009;36(4):822–30.
Wu EQ, Patel PA, Mody RR, Yu AP, Cahill KE, Tang J, et al. Frequency, risk, and cost of gout-related episodes among the elderly: does serum uric acid level matter? J Rheumatol. 2009;36(5):1032–40.
Edwards NL, Sundy JS, Forsythe A, Blume S, Pan F, Becker MA. Work productivity loss due to flares in patients with chronic gout refractory to conventional therapy. J Med Econ. 2011;14(1):10–5.
Park H, Rascati KL, Prasla K, McBayne T. Evaluation of health care costs and utilization patterns for patients with gout. Clin Ther. 2012;34(3):640–52.
Saseen JJ, Agashivala N, Allen RR, Ghushchyan V, Yadao AM, Nair KV. Comparison of patient characteristics and gout-related health-care resource utilization and costs in patients with frequent versus infrequent gouty arthritis attacks. Rheumatology. 2012;51(11):2004–12.
Wu EQ, Forsythe A, Guerin A, Yu AP, Latremouille-Viau D, Tsaneva M. Comorbidity burden, healthcare resource utilization, and costs in chronic gout patients refractory to conventional urate-lowering therapy. Am J Ther. 2012;19(6):e157–66.
Lynch W, Chan W, Kleinman N, Andrews LM, Yadao AM. Economic burden of gouty arthritis attacks for employees with frequent and infrequent attacks. Popul Health Manag. 2013;16(2):138–45.
Sicras-Mainar A, Navarro-Artieda R, Ibanez-Nolla J. Resource use and economic impact of patients with gout: a multicenter, population-wide study. Reumatol Clin. 2013;9(2):94–100.
Garg R, Sayles HR, Yu F, Michaud K, Singh J, Saag KG, et al. Gout-related health care utilization in US emergency departments, 2006 through 2008. Arthritis Care Res. 2013;65(4):571–7.
De Vera MA, Marcotte G, Rai S, Galo JS, Bhole V. Medication adherence in gout: a systematic review. Arthritis Care Res. 2014;66(10):1551–9.
Wertheimer A, Morlock R, Becker MA. A revised estimate of the burden of illness of gout. Curr Ther Res Clin Exp. 2013;75:1–4.
Chandratre P, Roddy E, Clarson L, Richardson J, Hider SL, Mallen CD. Health-related quality of life in gout: a systematic review. Rheumatology. 2013;52(11):2031–40.
Colwell HH, Hunt BJ, Pasta DJ, Palo WA, Mathias SD, Joseph-Ridge N. Gout assessment questionnaire: initial results of reliability, validity and responsiveness. Int J Clin Pract. 2006;60(10):1210–7.
Roddy E, Zhang W, Doherty M. Is gout associated with reduced quality of life? A case-control study. Rheumatology. 2007;46(9):1441–4.
Alvarez-Hernandez E, Pelaez-Ballestas I, Vazquez-Mellado J, Teran-Estrada L, Bernard-Medina AG, Espinoza J, et al. Validation of the health assessment questionnaire disability index in patients with gout. Arthritis Rheum. 2008;59(5):665–9.
Hirsch JD, Lee SJ, Terkeltaub R, Khanna D, Singh J, Sarkin A, et al. Evaluation of an instrument assessing influence of gout on health-related quality of life. J Rheumatol. 2008;35(12):2406.
Khanna D, Ahmed M, Yontz D, Ginsburg SS, Park GS, Leonard A, et al. The disutility of chronic gout. Qual Life Res. 2008;17(5):815–22.
Singh JA, Strand V. Gout is associated with more comorbidities, poorer health-related quality of life and higher healthcare utilisation in US veterans. Ann Rheum Dis. 2008;67(9):1310–6.
Taylor WJ, Colvine K, Gregory K, Collis J, McQueen FM, Dalbeth N. The health assessment questionnaire disability index is a valid measure of physical function in gout. Clin Exp Rheumatol. 2008;26(4):620–6.
Becker MA, Schumacher HR, Benjamin KL, Gorevic P, Greenwald M, Fessel J, et al. Quality of life and disability in patients with treatment-failure gout. J Rheumatol. 2009;36(5):1041–8.
Lee SJ, Hirsch JD, Terkeltaub R, Khanna D, Singh JA, Sarkin A, et al. Perceptions of disease and health-related quality of life among patients with gout. Rheumatology. 2009;48(5):582–6.
Hirsch JD, Terkeltaub R, Khanna D, Singh J, Sarkin A, Shieh M, et al. Gout disease-specific quality of life and the association with gout characteristics. Patient Relat Outcome Meas. 2010;1(2010):1–8.
Sarkin AJ, Levack AE, Shieh MM, Kavanaugh AF, Khanna D, Singh JA, et al. Predictors of doctor-rated and patient-rated gout severity: gout impact scales improve assessment. J Eval Clin Pract. 2010;16(6):1244–7.
van Groen MM, ten Klooster PM, Taal E, van de Laar MA, Glas CA. Application of the health assessment questionnaire disability index to various rheumatic diseases. Qual Life Res. 2010;19(9):1255–63.
Dalbeth N, Petrie KJ, House M, Chong J, Leung W, Chegudi R, et al. Illness perceptions in patients with gout and the relationship with progression of musculoskeletal disability. Arthritis Care Res. 2011;63(11):1605–12.
Khanna D, Sarkin AJ, Khanna PP, Shieh MM, Kavanaugh AF, Terkeltaub RA, et al. Minimally important differences of the gout impact scale in a randomized controlled trial. Rheumatology. 2011;50(7):1331–6.
Khanna PP, Perez-Ruiz F, Maranian P, Khanna D. Long-term therapy for chronic gout results in clinically important improvements in the health-related quality of life: short form-36 is responsive to change in chronic gout. Rheumatology. 2011;50(4):740–5.
ten Klooster PM, Oude Voshaar MA, Taal E, van de Laar MA. Comparison of measures of functional disability in patients with gout. Rheumatology. 2011;50(4):709–13.
DiBonaventura M, Andrews LM, Yadao AM, Kahler KH. The effect of gout on health-related quality of life, work productivity, resource use and clinical outcomes among patients with hypertension. Exp Rev Pharmacoecon Outcomes Res. 2012;12(6):821–9.
Khanna PP, Nuki G, Bardin T, Tausche AK, Forsythe A, Goren A, et al. Tophi and frequent gout flares are associated with impairments to quality of life, productivity, and increased healthcare resource use: Results from a cross-sectional survey. Health Qual Life Outcomes. 2012;10:117.
Taylor WJ, House M, Horne A, McQueen FM, Dalbeth N. The work instability scale predicts absenteeism in people with gout and suggests a higher risk for those in manual occupations. J Clin Rheumatol. 2012;18(8):405–10.
Hoy DG, Smith E, Cross M, Sanchez-Riera L, Buchbinder R, Blyth FM, et al. The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis. 2014;73(6):982–9.
Brown GC, Brown MM, Sharma S, Stein JD, Roth Z, Campanella J, et al. The burden of age-related macular degeneration: a value-based medicine analysis. Trans Am Ophthalmol Soc. 2005;103:173–86.
Beard S, von Scheele B, Nuki G, Pearson I. Cost-effectiveness of febuxostat in chronic gout. Eur J Health Econ. 2014;15(5):453–63.
Jutkowitz E, Choi HK, Pizzi LT, Kuntz KM. Cost-effectiveness of allopurinol and febuxostat for the management of gout. Ann Intern Med. 2014;161(9):617–26.
Spaetgens B, Tran-Duy A, Wijnands JM, van der Linden S, Boonen A. Health and utilities in patients with gout under care of a rheumatologist: which factors contribute? Arthritis Care Res. 2015. doi:10.1002/acr.22551
Buist AS, Vollmer WM, Sullivan SD, Weiss KB, Lee TA, Menezes AM, et al. the burden of obstructive lung disease initiative (BOLD): rationale and design. Copd. 2005;2(2):277–83.
Rutten-van Molken M. Raising the awareness: projecting the future burden of COPD with the BOLD model. Eur Respir J. 2009;34(4):787–9.
Buist AS, Vollmer WM, McBurnie MA. Worldwide burden of COPD in high- and low-income countries. Part I. The burden of obstructive lung disease (BOLD) initiative. Int J Tuberc Lung Dis. 2008;12(7):703–8.
Massi-Benedetti M. The cost of diabetes Type II in Europe: the CODE-2 Study. Diabetologia. 2002;45(7):S1–4.
Jonsson B. Revealing the cost of type II diabetes in Europe. Diabetologia. 2002;45(7):S5–12.
Bagust A, Beale S. Modelling EuroQol health-related utility values for diabetic complications from CODE-2 data. Health Econ. 2005;14(3):217–30.
Bloudek LM, Stokes M, Buse DC, Wilcox TK, Lipton RB, Goadsby PJ, et al. Cost of healthcare for patients with migraine in five European countries: results from the International Burden of Migraine Study (IBMS). J Headache Pain. 2012;13(5):361–78.
Stokes M, Becker WJ, Lipton RB, Sullivan SD, Wilcox TK, Wells L, et al. Cost of health care among patients with chronic and episodic migraine in Canada and the USA: results from the International Burden of Migraine Study (IBMS). Headache. 2011;51(7):1058–77.
Payne KA, Varon SF, Kawata AK, Yeomans K, Wilcox TK, Manack A, et al. The International Burden of Migraine Study (IBMS): study design, methodology, and baseline cohort characteristics. Cephalalgia. 2011;31(10):1116–30.
Acknowledgments
Shields GE and Beard SM are invited authors on this review paper and have not received payment, and have no financial relationship with any organization related to this manuscript. Beard SM has previously published work on the cost effectiveness of febuxostat for gout therapy (Beard SM, von Scheele BG, Nuki G, Pearson IV. Cost-effectiveness of febuxostat in chronic gout. Eur J Health Econ. 2014 Jun;15(5):453–63).
Author contributions
Beard SM and Shields GE were involved in the planning, completion and interpretation of the results of the systematic review. Shields GE led the drafting of the paper, with Beard SM providing guidance, reviews and revisions to all drafts. Both authors approved the final submitted version and guaranteed its content.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shields, G.E., Beard, S.M. A Systematic Review of the Economic and Humanistic Burden of Gout. PharmacoEconomics 33, 1029–1047 (2015). https://doi.org/10.1007/s40273-015-0288-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-015-0288-5