Abstract
Objective
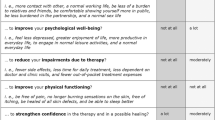
To assess patient preferences for psoriasis treatment features and to investigate the heterogeneity of preferences among patients with different socio-demographic and disease-related characteristics.
Methodology
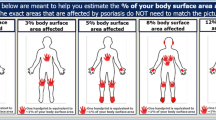
A discrete choice experiment was conducted on adult patients with moderate to severe plaque-type psoriasis during a routine visit to their physician at 15 centres in Italy. We investigated the preferences of patients with respect to five treatment attributes: (1) mode and frequency of administration; (2) time to improvement; (3) time free of symptoms; (4) unintended life expectancy reduction resulting from treatment; and (5) monthly treatment cost. The heterogeneity of preferences was investigated in a mixed logit model with normally distributed random coefficients.
Results
Overall, patients preferred the subcutaneous or intravenous route of administration (versus oral administration) and treatments that took less time to show improvement, ensured a longer time free of symptoms, involved a lesser reduction in life expectancy and had lower costs. There was significant preference heterogeneity for all attributes. The cost attribute was found to be significantly more important to females and to older patients (above 60 years of age). Older patients placed significantly greater emphasis on reduced life expectancy, whereas the time free of symptoms was significantly less important to them than to patients under 60 years of age. Patients with higher scores on the Dermatology Life Quality Index (DLQI) placed higher value on the time free of symptoms than those with lower DLQI scores. For the overall sample, the marginal willingness to pay (WTP) for a month’s reduction in the time to improvement was €32.4, whereas the WTP for one additional month without symptoms was significantly higher (€68.2).
Conclusion
Patient-centred policies should consider the heterogeneity of patients’ expectations to identify individualized treatments that would aid in optimizing patient satisfaction and wellbeing, as well as overall treatment effectiveness.

Similar content being viewed by others
References
Fairhurst DA, Ashcroft DM, Griffiths CE. Optimal management of severe plaque form of psoriasis. Am J Clin Dermatol. 2005;6(5):283–94.
Renzi C, Picardi A, Abeni D, Agostini E, Baliva G, Pasquini P, et al. Association of dissatisfaction with care and psychiatric morbidity with poor treatment compliance. Arch Dermatol. 2002;138(3):337–42.
Zaghloul SS, Goodfield MJ. Objective assessment of compliance with psoriasis treatment. Arch Dermatol. 2004;140(4):408–14. doi:10.1001/archderm.140.4.408.
Richards HL, Fortune DG, Griffiths CE. Adherence to treatment in patients with psoriasis. J Eur Acad Dermatol Venereol. 2006;20(4):370–9. doi:10.1111/j.1468-3083.2006.01565.x.
van de Kerkhof PC, de Hoop D, de Korte J, Cobelens SA, Kuipers MV. Patient compliance and disease management in the treatment of psoriasis in the Netherlands. Dermatology. 2000;200(4):292–8. doi:18390.
Coulter A. Partnerships with patients: the pros and cons of shared clinical decision-making. J Health Serv Res Policy. 1997;2(2):112–21.
Coulter A. Paternalism or partnership? Patients have grown up—and there’s no going back. BMJ. 1999;319(7212):719–20.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–77.
Augustovski F, Beratarrechea A, Irazola V, Rubinstein F, Tesolin P, Gonzalez J, et al. Patient preferences for biologic agents in rheumatoid arthritis: a discrete-choice experiment. Value Health. 2013;16(2):385–93. doi:10.1016/j.jval.2012.11.007.
Kjaer T, Bech M, Gyrd-Hansen D, Hart-Hansen K. Ordering effect and price sensitivity in discrete choice experiments: need we worry? Health Econ. 2006;15(11):1217–28. doi:10.1002/hec.1117.
de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21(2):145–72. doi:10.1002/hec.1697.
McFadden D, Train K. Mixed MNL models for discrete response. J Appl Econometr. 2000;5(5):447–70.
Hole AR. Modelling heterogeneity in patients’ preferences for the attributes of a general practitioner appointment. J Health Econ. 2008;27(4):1078–94. doi:10.1016/j.jhealeco.2007.11.006.
Hall J, Fiebig DG, King MT, Hossain I, Louviere JJ. What influences participation in genetic carrier testing? Results from a discrete choice experiment. J Health Econ. 2006;25(3):520–37. doi:10.1016/j.jhealeco.2005.09.002.
King MT, Hall J, Lancsar E, Fiebig D, Hossain I, Louviere J, et al. Patient preferences for managing asthma: results from a discrete choice experiment. Health Econ. 2007;16(7):703–17. doi:10.1002/hec.1193.
Kjaer T, Gyrd-Hansen D. Preference heterogeneity and choice of cardiac rehabilitation program: results from a discrete choice experiment. Health Policy. 2008;85(1):124–32. doi:10.1016/j.healthpol.2007.07.002.
Paterson RW, Boyle KJ, Parmeter CF, Neumann JE, De Civita P. Heterogeneity in preferences for smoking cessation. Health Econ. 2008;17(12):1363–77. doi:10.1002/hec.1336.
Ashcroft DM, Seston E, Griffiths CE. Trade-offs between the benefits and risks of drug treatment for psoriasis: a discrete choice experiment with U.K. dermatologists. Br J Dermatol. 2006;155(6):1236–41. doi:10.1111/j.1365-2133.2006.07535.x.
Seston EM, Ashcroft DM, Griffiths CE. Balancing the benefits and risks of drug treatment: a stated-preference, discrete choice experiment with patients with psoriasis. Arch Dermatol. 2007;143(9):1175–9. doi:10.1001/archderm.143.9.1175.
Hauber AB, Gonzalez JM, Schenkel B, Lofland JH, Martin S. The value to patients of reducing lesion severity in plaque psoriasis. J Dermatol Treat. 2011;22(5):266–75. doi:10.3109/09546634.2011.588193.
Schaarschmidt ML, Schmieder A, Umar N, Terris D, Goebeler M, Goerdt S, et al. Patient preferences for psoriasis treatments: process characteristics can outweigh outcome attributes. Arch Dermatol. 2011;147(11):1285–94. doi:10.1001/archdermatol.2011.309.
Schaarschmidt ML, Umar N, Schmieder A, Terris DD, Goebeler M, Goerdt S, et al. Patient preferences for psoriasis treatments: impact of treatment experience. J Eur Acad Dermatol Venereol. 2013;27(2):187–98. doi:10.1111/j.1468-3083.2011.04440.x.
Schmieder A, Schaarschmidt ML, Umar N, Terris DD, Goebeler M, Goerdt S, et al. Comorbidities significantly impact patients’ preferences for psoriasis treatments. J Am Acad Dermatol. 2012;67(3):363–72. doi:10.1016/j.jaad.2011.08.023.
Smith CH, Anstey AV, Barker JN, Burden AD, Chalmers RJ, Chandler DA, et al. British Association of Dermatologists’ guidelines for biologic interventions for psoriasis 2009. Br J Dermatol. 2009;161(5):987–1019. doi:10.1111/j.1365-2133.2009.09505.x.
Gelfand JM, Wan J, CallisDuffin K, Krueger GG, Kalb RE, Weisman JD, et al. Comparative effectiveness of commonly used systemic treatments or phototherapy for moderate to severe plaque psoriasis in the clinical practice setting. Arch Dermatol. 2012;148(4):487–94. doi:10.1001/archdermatol.2012.370.
Leonardi CL, Kimball AB, Papp KA, Yeilding N, Guzzo C, Wang Y, et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1). Lancet. 2008;371(9625):1665–74. doi:10.1016/S0140-6736(08)60725-4.
Lotti T, Chimenti S, Katsambas A, Ortonne JP, Dubertret L, Licu D, et al. Efficacy and safety of efalizumab in patients with moderate-to-severe plaque psoriasis resistant to previous anti-psoriatic treatment: results of a multicentre, open-label, phase IIIb/IV trial. Arch Drug Inf. 2010;3(1):9–18. doi:10.1111/j.1753-5174.2009.00026.x.
Barker J, Hoffmann M, Wozel G, Ortonne JP, Zheng H, van Hoogstraten H, et al. Efficacy and safety of infliximab vs. methotrexate in patients with moderate-to-severe plaque psoriasis: results of an open-label, active-controlled, randomized trial (RESTORE1). Br J Dermatol. 2011;165(5):1109–17. doi:10.1111/j.1365-2133.2011.10615.x.
Strober BE, Crowley JJ, Yamauchi PS, Olds M, Williams DA. Efficacy and safety results from a phase III, randomized controlled trial comparing the safety and efficacy of briakinumab with etanercept and placebo in patients with moderate to severe chronic plaque psoriasis. Br J Dermatol. 2011;165(3):661–8. doi:10.1111/j.1365-2133.2011.10419.x.
Bissonnette R, Bolduc C, Maari C, Nigen S, Webster JM, Tang L, et al. Efficacy and safety of topical WBI-1001 in patients with mild to moderate psoriasis: results from a randomized double-blind placebo-controlled, phase II trial. J Eur Acad Dermatol Venereol. 2012;26(12):1516–21. doi:10.1111/j.1468-3083.2011.04332.x.
Strohal R, Puig L, Chouela E, Tsai TF, Melin J, Freundlich B, et al. The efficacy and safety of etanercept when used with as-needed adjunctive topical therapy in a randomised, double-blind study in subjects with moderate-to-severe psoriasis (the PRISTINE trial). J Dermatol Treat. 2013;24(3):169–78. doi:10.3109/09546634.2012.658015.
Cham PM, Chen SC, Grill JP, Jonk YC, Warshaw EM. Reliability of self-reported willingness-to-pay and annual income in patients treated for toenail onychomycosis. Br J Dermatol. 2007;156(5):922–8. doi:10.1111/j.1365-2133.2006.07740.x.
Radtke MA, Schafer I, Gajur A, Langenbruch A, Augustin M. Willingness-to-pay and quality of life in patients with vitiligo. Br J Dermatol. 2009;161(1):134–9. doi:10.1111/j.1365-2133.2009.09091.x.
Schiffner R, Schiffner-Rohe J, Gerstenhauer M, Hofstadter F, Landthaler M, Stolz W. Willingness to pay and time trade-off: sensitive to changes of quality of life in psoriasis patients? Br J Dermatol. 2003;148(6):1153–60.
Carlsson F, Martinsson P. Design techniques for stated preference methods in health economics. Health Econ. 2003;12(4):281–94. doi:10.1002/hec.729.
Reed Johnson F, Lancsar E, Marshall D, Kilambi V, Muhlbacher A, Regier DA, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health. 2013;16(1):3–13. doi:10.1016/j.jval.2012.08.2223.
Hole AR, Kolstad JR. Mixed logit estimation of willingness to pay distributions: a comparison of models in preference and WTP space using data from a health-related choice experiment. Empir Econ. 2012;42:445–69.
Hole A. Esitmating mixed logit using maximum simulated likelihood. Stata J. 2007;7(3):388–401.
Hensher DA, Greene WH. The mixed logit model: the state of practice. Transportation. 2003;30:133–76.
Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13. doi:10.1016/j.jval.2010.11.013.
Umar N, Litaker D, Schaarschmidt ML, Peitsch WK, Schmieder A, Terris DD. Outcomes associated with matching patients’ treatment preferences to physicians’ recommendations: study methodology. BMC Health Serv Res. 2012;12:1. doi:10.1186/1472-6963-12-1.
Lamiraud K, Geoffard PY. Therapeutic non-adherence: a rational behavior revealing patient preferences? Health Econ. 2007;16(11):1185–204. doi:10.1002/hec.1214.
Basu A, Meltzer D. Value of information on preference heterogeneity and individualized care. Med Decis Making. 2007;27(2):112–27. doi:10.1177/0272989X06297393.
Acknowledgments
This study was funded by an institutional grant and honoraria from Janssen Italia SpA. A.T. and G.F. received grants from Janssen Italia SpA during the conduct of the study. F.A. served as a consultant to Janssen Italia SpA during the conduct of the study and outside the submitted work.
An independent contract research organization, paid by the funding source, was responsible for the study’s deployment and survey administration in the hospitals. The views expressed in this paper are solely those of the authors, who have no conflicts of interest directly relevant to the content of the paper. The publication of the study results was not contingent on the sponsor’s approval or censorship of the manuscript.
All authors contributed to the conception and design of the study. G.F. and F.A. were in charge of defining the study protocol, while A.T. was involved in the design of the DCE part of the survey and conducted analysis on the experiment data. All authors were involved in drafting the manuscript and revising it critically for important intellectual content. All authors gave final approval of the version to be published. A.T. and G.F. had full access to all of the data in the study, and they both take complete responsibility for the integrity of the data and the accuracy of the data analysis.
Authors are particularly thankful to Stefania Casalini and Antonio Castiglia from Janssen Italia SpA for their support and contribution to the realization of the research project. Finally, authors wish to express their gratitude to all study investigators from 15 hospitals participating in the study: 1) De Simone Clara, D'Agostino Magda (Policlinico Gemelli, Roma), 2) Simonacci Marco, Bettacchi Alberta (Ospedale di Macerata), 3) Papini Manuela, Cicoletti Michela (Azienda Ospedaliera Santa Maria di Terni), 4) Cottoni Francesca, Montesu M. Antonietta (Clinica Dermatologica Università di Sassari), 5) Micali Giuseppe, Musumeci Letizia (Azienda Ospedaliera Universitaria “Policlinico-Vittorio Emanuele”, Presidio Gaspare Rodolico, Catania), 6) La Greca Stefano, Massimino Daniela (Azienda Ospedaliera “Garibaldi-S.L.Currò-Ascoli Tomaselli”, Catania), 7) Patrizi Annalisa, Bardazzi Federico (Policlinico S. Orsola-Malpighi, Bologna), 8) Peserico Andrea, Piaserico Stefano (Azienda Ospedaliera Universitaria di Padova), 9) Girolomoni Giampiero, Del Giglio Micol (Ospedale Civile Maggiore-Università degli Studi di Verona), 10) Parodi Aurora, Cozzani Emanuele (Azienda Ospedaliera San Martino, Genova), 11) Cattaneo Angleo, Carrera Carlo (Ospedale Maggiore Policlinico, Mangiagalli e Regina Elena, Milano), 12) Colombo Enrico, Tiberio Rossana (Ospedale maggiore della Carità, Novara), 13) Valenti Giancarlo, D'Amico Domenico (Azienda Ospedaliera Pugliese Ciaccio, Catanzaro), 14) Balato Nicola (Università degli Studi di Napoli) 15) Griseta Vito, Lerario Andrea (Ospedale Generale Regionale "F. Miulli", Bari).
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Torbica, A., Fattore, G. & Ayala, F. Eliciting Preferences to Inform Patient-Centred Policies: the Case of Psoriasis. PharmacoEconomics 32, 209–223 (2014). https://doi.org/10.1007/s40273-013-0126-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-013-0126-6