Abstract
Background
Most researchers in health economics cite random utility theory (RUT) when analysing discrete choice experiments (DCEs). Under RUT, the error term is associated with the analyst’s inability to properly capture the true choice processes of the respondent as well as the inconsistency or mistakes arising from the respondent themselves. Under such assumptions, it stands to reason that analysts should explore more complex nonlinear indirect utility functions, than currently used in healthcare, to strive for better estimates of preferences in healthcare.
Objective
To test whether complex indirect utility functions decrease error variance for models that either implicitly (i.e. the multinomial logit (MNL) model) or explicitly (i.e. entropy multinomial logit (EMNL) model) account for error variance in health(care)-related DCEs; and to determine the impact of complex indirect utility functions on willingness-to-pay (WTP) measures.
Methods
Using data from DCEs aimed at healthcare-related decisions, we empirically compared (1) complex and simple indirect utility specifications in terms of goodness of fit, (2) their impact on WTP measures, including confidence intervals (CIs) based on the Delta method, the Krinsky and Robb-procedure, and Bootstrapping, and (3) MNL and EMNL model results.
Results
Complex indirect utility functions had a better model fit than simple specifications (p < 0.05). WTP estimates were quite similar across alternative specifications. The Delta method produced the most narrow CIs. The EMNL model showed that respondents apply simplifying strategies when answering DCE questions.
Conclusion
Complex indirect utility functions reduce error arisen from researchers, which can have important implications for measures in healthcare such as the WTP, whereas EMNL provides insights into the behaviour of respondents when answering DCEs. Understanding how respondents answer DCE questions may allow researchers to construct DCEs that minimise scale differences, so that the decision error made across respondents is more homogeneous and therefore taken out as additional noise in the data. Hence, better estimates of preferences in healthcare can be provided.
Similar content being viewed by others
Notes
We use the term indirect utility function as opposed to (direct) utility function deliberately. The original derivations of McFadden [4], which have led to the discrete choice models discussed herein, work within the framework of indirect utility functions that he identifies via Roy’s Identity. The derivation of models based on direct utility functions, whilst possible, result in an alternative modelling approach, based on the Kuhn–Tucker conditions (Kuhn and Tucker [7]).
As in most studies, in this paper, we use the broad notion of the multinomial logit model as being a combination of multinomial logit and conditional logit. The original multinomial logit model uses only individual characteristics (also called covariates, for example gender) in the indirect utility functions, while the conditional logit model as proposed by McFadden [4] considers characteristics of the alternatives (such as cost). Often, both characteristics are included in the indirect utility functions.
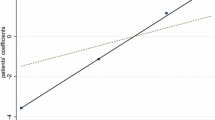
Equation 7 assumes constant marginal utility of income. Testing for this actually provides a test of whether the data are utility theoretic. If MUY is constant, the scatter plot of predicted utility against nominal cost should be linear [8]. We would not expect MUY to vary for costs that are small relative to disposable income.
References
Louviere JJ, Lancsar E. Choice experiments in health: the good, the bad, the ugly and toward a brighter future. Health Econ Policy Law. 2009;4(Pt 4):527–46.
Witt J, Scott A, Osborne RH. Designing choice experiments with many attributes: an application to setting priorities for orthopaedic waiting lists. Health Econ. 2009;18(6):681–96.
Manski C. The structure of random utility models. Theory Decis. 1977;8:229–54.
McFadden D. Conditional logit analysis of qualitative choice behavior. In: Zarembka P, editor. Frontiers in econometrics. New York: Academic Press; 1974. p. 105–42.
Fiebig DG, Knox S, Viney R, Haas M, Street DJ. Preferences for new and existing contraceptive products. Health Econ. 2011;20(Suppl 1):35–52.
Keane M. The generalized logit model: preliminary ideas on a research program Motorola-CenSoC meeting, Hong Kong; 2006.
Kuhn HW, Tucker AW. Nonlinear programming. In: Neyman J, editor. Proceedings of the Second Berkeley Symposium on Mathematical Statistics and Probability. Berkeley and Los Angeles: University of California Press; 1950. p. 481–492.
Johnson FR, Mohamed AF, Ozdemir S, Marshall DA, Phillips KA. How does cost matter in health-care discrete-choice experiments? Health Econ. 2011;20(3):323–30.
Kolstad JR. How to make rural jobs more attractive to health workers: findings from a discrete choice experiment in Tanzania. Health Econ. 2011;20(2):196–211.
Mark TL, Swait J. Using stated preference and revealed preference modeling to evaluate prescribing decisions. Health Econ. 2004;13(6):563–73.
Hole AR. A comparison of approaches to estimating confidence intervals for willingness to pay measures. Health Econ. 2007;16(8):827–40.
Swait J, Adamowicz W. Choice environment, market complexity, and consumer behavior: a theoretical and empirical approach for incorporating decision complexity into models of consumer choice. Organ Behav Hum Decis Process. 2001;86(2):141–67.
Fiebig DG, Keane MP, Louviere JJ, Wasi N. The generalized multinomial logit model: accounting for scale and coefficient heterogeneity. Mark Sci. 2010;29(3):393–421.
Louviere JJ, Carson RT, Ainslie A, Cameron TA, DeShazo JR, Hensher D, et al. Dissecting the random component of utility. Mark Lett. 2002;13:177–93.
Louviere JJ, Eagle T. Confound it! That pesky little scale constant messes up our convenient assumptions. In: Proceedings of 2006 sawtooth software conference. Sequem: Sawtooth Software; 2006. p. 211–28.
Louviere JJ, Street D, Burgess L, Wasi N, Islam T, Marley AAJ. Modeling the choices of individuals decision makers by combining efficient choice experiment designs with extra preference information. J Choice Model. 2008;1(1):128–63.
Meyer RJ, Louviere JJ. Formal choice models of informal choices: what choice modelling research can (and can’t) learn from behavioral theory. Rev Mark Res. 2007;4:3–32.
Knox SA, Viney RC, Gu Y, Hole AR, Fiebig DG, Street DJ, et al. The effect of adverse information and positive promotion on women’s preferences for prescribed contraceptive products. Soc Sci Med. 2013;83:70–80.
Ryan M, Gerard K. Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl Health Econ Health Policy. 2003;2(1):55–64.
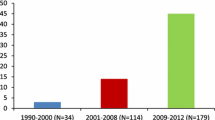
de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21(2):145–72.
Hall J, Kenny P, King M, Louviere J, Viney R, Yeoh A. Using stated preference discrete choice modelling to evaluate the introduction of varicella vaccination. Health Econ. 2002;11(5):457–65.
Maddala T, Phillips KA, Reed Johnson F. An experiment on simplifying conjoint analysis designs for measuring preferences. Health Econ. 2003;12(12):1035–47.
Ozdemir S, Mohamed AF, Johnson FR, Hauber AB. Who pays attention in stated-choice surveys? Health Econ. 2010;19(1):111–8.
Ryan M, Watson V. Comparing welfare estimates from payment card contingent valuation and discrete choice experiments. Health Econ. 2009;18(4):389–401.
Telser H, Zweifel P. Measuring willingness-to-pay for risk reduction: an application of conjoint analysis. Health Econ. 2002;11(2):129–39.
Reed Johnson F, Lancsar E, Marshall D, Kilambi V, Muhlbacher A, Regier DA, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health. 2013;16(1):3–13.
Viney R, Lancsar E, Louviere J. Discrete choice experiments to measure consumer preferences for health and healthcare. Expert Rev Pharmacoecon Outcomes Res. 2002;2(4):319–26.
Lancsar E, Savage E. Deriving welfare measures from discrete choice experiments: inconsistency between current methods and random utility and welfare theory. Health Econ. 2004;13(9):901–7.
Dellaert BGC, Brazell JD, Louviere JJ. The effect of attribute variation on consumer choice consistency. Mark Lett. 1999;10(2):139–47.
Keller KL, Staelin R. Effects of quality and quantity of information on decision effectiveness. J Consumer Res. 1987;14(2):200–13.
de Bekker-Grob EW, Essink-Bot ML, Meerding WJ, Koes BW, Steyerberg EW. Preferences of GPs and patients for preventive osteoporosis drug treatment: a discrete-choice experiment. Pharmacoeconomics. 2009;27(3):211–9.
de Bekker-Grob EW, Essink-Bot ML, Meerding WJ, Pols HA, Koes BW, Steyerberg EW. Patients’ preferences for osteoporosis drug treatment: a discrete choice experiment. Osteoporos Int. 2008;19(7):1029–37.
de Bekker-Grob EW, Rose JM, Donkers B, Essink-Bot ML, Bangma CH, Steyerberg EW. Men’s preferences for prostate cancer screening: a discrete choice experiment. Br J Cancer. 2013;108(3):533–41.
Daly A, Hess S, de Jong G. Calculating errors for measures derived from choice modelling estimates. Transp Res Part B. 2012;46(2):333–41.
Hess S, Rose JM. Can scale and coefficient heterogeneity be separated in random coefficients models? Transportation. 2012;39(6):1225–39.
Flynn TN, Louviere JJ, Peters TJ, Coast J. Using discrete choice experiments to understand preferences for quality of life: variance-scale heterogeneity matters. Soc Sci Med. 2010;70(12):1957–65.
Acknowledgments
EW de Bekker-Grob designed and conducted the DCE studies, contributed to the analyses and drafted the manuscript. JM Rose conceived the idea for the study, performed the analyses, and drafted the manuscript. MCJ Bliemer contributed to the formulas and analyses, and contributed to the writing of the manuscript. EW de Bekker-Grob and JM Rose have full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. EW de Bekker-Grob will act as the overall guarantor.
We would like to thank William Greene for his support with the Nlogit software, and Vereniging Trustfonds Erasmus University Rotterdam and the Department of Public Health, Erasmus MC – University Medical Centre Rotterdam for their financial support. EW de Bekker-Grob, JM Rose and MCJ Bliemer declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
de Bekker-Grob, E.W., Rose, J.M. & Bliemer, M.C.J. A Closer Look at Decision and Analyst Error by Including Nonlinearities in Discrete Choice Models: Implications on Willingness-to-Pay Estimates Derived from Discrete Choice Data in Healthcare. PharmacoEconomics 31, 1169–1183 (2013). https://doi.org/10.1007/s40273-013-0100-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-013-0100-3