Abstract
Background and Objective
Patients’ perceptions and experiences of medication efficacy, medication adverse events, dosing frequency, and dosing complexity have been found to influence adherence to injectable disease-modifying treatments (DMTs) in patients with multiple sclerosis (MS). The aim of this study was to quantify patient preferences for features of injectable DMTs for MS.
Methods
Adult patients in the United States (US) with a self-reported diagnosis of MS completed an online discrete-choice experiment survey to assess preference for a number of features of a hypothetical injectable DMT. Patients chose hypothetical treatments in paired comparisons, where each treatment was described by features or attributes, including the number of years until disability progression, the number of relapses in the next 4 years, injection time, the frequency of injections, the occurrence of flu-like symptoms (FLS), and severity of injection-site reactions. Random-parameters logit regression parameters were used to calculate preference weights of attribute levels and the relative importance of changes in treatment features.
Results
Of the 205 patients who completed the survey, 192 provided sufficient data for analysis. The results indicated a broad range of tradeoffs that patients would be willing to make. With regard to this, the relative importance of an improvement in the number of years until disability progression from 1 to 2 (i.e., vertical distance between preference weights for these attribute levels) was 0.9 [95 % confidence interval (CI) 0.5–1.2], the relative importance of this change was approximately equivalent to that of an improvement from 12 injections per month to two (mean 0.8, 95 % CI 0.4–1.2), or approximately equivalent to a decrease from four to one relapses in the next 4 years (mean 0.8, 95 % CI 0.5–1.2), or FLS 3 days after every injection to 3 days after some injections (mean 1.0, 95 % CI 0.6–1.4).
Conclusions
These results suggest that an improvement in treatment efficacy may be as important as a reduction in injection frequency or a reduction in some adverse events for patients who self-administer injectable DMTs for MS. Understanding the preferences of patients who use injectable treatments will inform the development of such treatments, which may in turn improve patient medication adherence and well-being.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study, conducted with a sample of individuals in the US with self-reported multiple sclerosis (MS), employed a discrete-choice experiment to quantify patient preferences for disease-modifying treatment (DMT) features associated with medication adherence. |
Patients reported that certain changes in injection frequency were as important as changes in DMT efficacy and adverse events; as such, injection frequency may be an important factor for patients with MS in determining their adherence to DMTs. |
The importance that patients place on MS treatment attributes may be of interest to healthcare providers, as well as to those who influence the selection of MS treatments. |
1 Introduction
Recently, there have been a number of approvals of new multiple sclerosis (MS) therapies. Yet despite this, current first-line treatments still include injectable disease-modifying treatments (DMTs) that were introduced in the early- to mid-1990s [1]. These treatments are likely to remain the mainstay of MS therapy, given their well-established efficacy and safety record [2]. However, numerous studies have concluded that adherence (defined as the extent to which a patient acts in accordance with the prescribed interval and dose of a dosing regimen [3]) to injectable DMTs for patients with MS is suboptimal [4, 5]. Studies in patients with MS [4–10] have reported rates of medication adherence ranging from 27 to 83 %, depending on the methodology and whether the study used claims data to calculate indirect measures of adherence [6, 7, 11, 12] or surveys to collect self-reported measures of adherence [4, 5, 8, 13].
Patients’ perceptions and experiences of medication efficacy, medication adverse events, dosing frequency, and dosing complexity have been found to influence adherence to injectable DMTs in patients with MS [4, 5, 8–16]. Adherence to injectable DMTs is typically higher when dosing frequency is lower [4, 5, 11–13, 17]; injection fatigue and injection fear, as well as injection-related adverse events [e.g., flu-like symptoms (FLS) and injection-site reactions (ISR)] are also common reasons cited for non-adherence [4, 9]. These results imply that experiences and/or perceptions of discomfort and inconvenience affect the choice of and the adherence to self-administered injectable DMTs. Several authors have suggested that improvements in administration of these treatments, such as a reduced dosing frequency, may reduce patient burden and improve adherence, as well as having economic benefits through fewer hospitalizations and emergency room visits [4, 6, 7, 12, 18]. Improvements in the dosing frequency and tolerability of DMTs may therefore improve adherence and directly reduce the number of injection-related adverse events.
This study was designed to assess the relative importance of a number of features of a (hypothetical) injectable DMT for patients with MS in the United States (US), using a discrete-choice experiment (DCE). The study investigators employed a broad set of features related to treatment with an injectable DMT such as efficacy and adverse events, as well as features describing administration, including dosing frequency and injection time. Previous studies have used similar methods to quantify patient preference for MS treatments, although with fewer/different parameters than this study [19, 20]. Patient preference studies for features of injectable DMTs provide information on the relative importance of these treatment features with respect to patient treatment choice and adherence. Collectively, data from these studies inform physicians on what features of treatment regimens and modalities are important to their patients and the associated burden of treatment [5, 8, 14], as well as informing healthcare providers and payors of any potential (direct and indirect) economic benefits that may arise from increased treatment efficacy and adherence [7]. Therefore, the objective of this study was to quantify the relative importance of the features of injectable DMTs that are associated with treatment choice and medication adherence in patients with MS.
2 Methods
2.1 Study Design
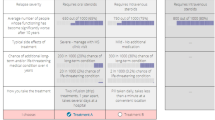
DCE studies [21–25] are based on the premise that medical treatments can be described as combinations of different features, or attributes. Attributes are defined in more detail in terms of levels; for instance, dosing frequency is an attribute with levels that could include daily, weekly, or monthly. The treatment attributes and attribute levels used to describe hypothetical MS treatments in this study were informed by (1) the characteristics of currently available injectable DMTs; (2) selected clinical study findings; and (3) consultation with clinical experts. The selection of attributes and levels is described in more detail in an appendix in the Electronic Supplementary Material. Based on this information, the set of six treatment attributes chosen for this study were the number of years until MS symptoms get worse (i.e., disability progression with a focus on ambulation), the number of relapses in the next 4 years, injection time, frequency of injections, FLS, and ISR (Table 1). A broad range of attribute levels was included to simulate the real tradeoffs that patients with MS would have to make when deciding among injectable DMTs and to avoid a narrow focus on a limited range of treatment attributes, which might bias study results.
The survey design, administration, and analysis followed current good research guidelines [21]. The draft survey instrument was pretested using in-depth, in-person interviews with 15 adult patients with a self-reported physician diagnosis of MS. Treatment cost was not considered as an attribute; patients were asked to assume that all the medications would have the same cost. The final survey instrument is available as an appendix in the Electronic Supplementary Material.
In a series of treatment-choice questions, patients were asked to choose one of two hypothetical injectable treatment pairs for MS, defined by their attributes and attribute levels (Table 1). Figure 1 presents a sample treatment-choice question from the online survey instrument.
The experimental design followed good practice guidelines [26] and was generated using SAS® 9.3 analytics software (SAS Institute, Cary, NC, USA), which allowed for the optimization of design efficiency, level balance, correlations between level differences, and number of choice tasks [27–31]. The experimental design comprised 48 different treatment pairs. In order to maximize the quality of response and minimize fatigue or cognitive burden [32–34], the 48 paired comparisons in the experimental design were divided into six survey versions, each version containing eight treatment-choice questions. Each patient was randomly assigned to one of the six versions, and the order of the treatment-choice questions was randomized for each patient. In addition, one of the treatment-choice questions was repeated later in the sequence. To evaluate the stability of patients’ choices, we calculated the percentage of patients who provided the same answer to both the original and the repeated treatment-choice questions. In total, patients answered nine treatment-choice questions. In addition, the final survey collected data on patient demographic and socioeconomic characteristics and experiences with MS and MS treatments.
To ensure that all patients were thinking about the same baseline, or initial MS symptoms, patients read a hypothetical reference scenario. Using a reference scenario ensured that each patient was considering the same initial disability level and the same change in disability. This, in turn, ensured that disability progression as a result of treatment was exogenous and that the changes in disability progression due to treatment were always improvements. Specifically, patients were asked to suppose that they had mild symptoms, as described using the Hohol, or Disease Steps, scale [35]. Patients were also asked to suppose that when their MS symptoms progressed, they would have moderate symptoms, again as described by the Hohol scale. The Hohol scale was selected because of the simplicity of the scale compared with the Expanded Disability Status Scale.
2.2 Study Sample
The target sample size for this study was 200 individuals. While the minimum required sample size for a DCE depends on a number of criteria [26], this sample size was within the range of sample sizes observed in most published studies [44].
Patients were recruited by All Global, a healthcare research firm, from an online panel of consumers in the US engaged for the purpose of survey research. All patients were aged 18 years or older and had a self-reported physician diagnosis of MS. The 25-min online survey was administered in May 2013. Patients were given a US$49 cash honorarium if they completed at least one treatment-choice question in the survey. The study was approved by institutional review boards of the Research Triangle Institute (RTI). All patients provided informed consent prior to their inclusion in the study.
2.3 Analysis
To analyze the treatment-choice data and estimate preferences for the attribute levels, a random-parameters logit (RPL) model was approximated using NLOGIT Software version 5.0 (Econometric Software, Inc., Plainview, NY, USA). The RPL model accounted for the panel nature of the dataset (multiple observations obtained from the same respondent over time) and allowed for preference heterogeneity from patients by estimating a distribution of preferences for each parameter as well as a mean preference parameter [36, 37]. The dependent variable was the treatment choice, Medicine A or Medicine B. The independent variables were the levels for each of the attributes included in the study. All independent variables were effects-coded categorical variables, which allowed for the estimation of a unique parameter for each attribute level in the model [38]. All parameters were specified to be normally distributed random parameters.
The marginal log-odds resulting from the RPL model could be interpreted as ‘preference weights’, which indicate the relative importance of each attribute level. All mean attribute effects were normalized to be zero; the preference weight for each attribute level was then estimated relative to the mean effect for that attribute. To be able to compare the levels within an attribute, the 95 % confidence interval (CI) was calculated for each preference weight using the RPL estimate of the mean preference weight corresponding to the attribute level and the estimated standard error of that mean. If the 95 % CIs around any two attribute levels did not overlap, the estimates were statistically different from each other at the 5 % level of significance or better.
The mean preference weights indicate the average relative importance of each attribute level in the sample and can be interpreted in two ways [36–38]. First, the vertical distance between any two preference weights for attribute levels, within a given attribute, indicate the importance of moving from one level of the attribute to the second level of the same attribute: the greater the difference, the more important the change from one level to the second level. Second, the relative importance of changes within an attribute could be compared with the relative importance of changes within a different attribute. This interpretation would be used to examine the tradeoffs that patients would be willing to make across treatment features.
In addition, to examine whether preferences for any treatment attributes depended on the levels of other treatment attributes, we included interactions between effects-coded (independent) variables. To examine whether preferences for any treatment attributes varied within subgroups, we included interactions between effects-coded (independent) variables and patient characteristics.
3 Results
To recruit respondents, All Global made the survey link available to web panelists who logged onto their account. From their account, interested panelists could learn about the survey opportunity and click through to the survey. We do not have information on the number of respondents who were provided the opportunity to be screened. A total of 498 patients opted to respond to the open survey, of whom 205 (41 %) met the inclusion criteria and completed at least one choice question in the survey. Thirteen patients (6 %) always chose either Medicine A or Medicine B in each of the treatment-choice questions and were excluded because this may indicate that these patients did not pay close attention to the choice questions. The final sample size for analysis was 192 patients. On average, patients had a 12-year diagnosis of MS [standard deviation (SD), 7]. The majority were female (78 %). More than two-thirds (68 %) reported having relapsing-remitting MS (RRMS). To manage MS symptoms, 45 % received regular injections. Sixty-five percent of patients not receiving regular injections at the time of the survey reported having received regular injections in the past. Thus, 81 % of patients had current or prior experience with injectable DMTs. Using the Hohol scale [35], 16 % of patients reported having mild symptoms of MS on most days, whereas 29 % reported having moderate symptoms. On average, patients reported experiencing four relapses (SD, five) within the last 2 years. A majority of patients (55 %) reported having experienced FLS resulting from MS treatments. Among patients with injection experience, 71 % reported having experienced a mild ISR (Table 2).
The test of the stability of patients’ choices indicated that most patients (158 of 192, or 82 %) provided the same response to both the original and repeated treatment-choice questions. This stability test result was similar to what has been observed in other studies [19, 39]. There are several reasons that respondents may have unstable responses to choice questions, including learning and fatigue while answering the series of choice questions. Also, respondents’ choice in any particular DCE question may depend on the content of previously answered choice tasks. While the stability test cannot distinguish the reason for response instability, we use this crude assessment as an indicator of the extent to which instability may be present in the study. Using an RPL model, no statistically significant differences were shown between RPL model results with and without the repeated question (data not shown). Therefore, repeated questions were included in the overall analysis, and no patients were removed due to the stability of their response.
Figure 2 presents the results of the RPL estimation, including preference weights and 95 % CIs for the attribute levels. Patient preferences were consistent with the expectation that better outcomes (e.g., better efficacy, fewer adverse events, more convenient administration) would be preferred to worse outcomes, providing evidence for internal validity of the study. For example, delaying MS disability progression by 4 years was preferred to delaying progression by 2 years, and delaying MS disability progression by 2 years was preferred to delaying progression by 1 year. The differences between the preference weights for these attribute levels were statistically significant (P < 0.05).
The mean relative importance of an improvement in the number of years until disability progression from 1 to 2 years was 0.9 (the vertical distance between preference weights for these attribute levels) (95 % CI 0.5–1.2; Fig. 2; Table 3). The relative importance of this change in disability progression was approximately equivalent to the relative importance of the number of relapses in the next 4 years from four to one (mean relative importance = 0.8; 95 % CI 0.5–1.2), the frequency of injections per month from 12 to two times (mean relative importance = 0.8; 95 % CI 0.4–1.2), and FLS from 3 days after every injection to 3 days after some injections (defined as “about one-half” of injections) (mean relative importance = 1.0; 95 % CI 0.6–1.4).
The mean relative importance of an improvement in the number of years until disability progression from 1 to 2 years was approximately twice (0.9 ÷ 0.5) as important as the mean relative importance of reducing the number of relapses in the next 4 years from three to one, three times (0.9 ÷ 0.3) as important as the mean relative importance of improving ISR from mild to none, and approximately four times (0.9 ÷ 0.2) as important as the mean relative importance of decreasing injection time in seconds from 10 to 3.
To assess whether preferences for selected attribute levels (i.e., levels of injection time, FLS, and ISR) varied systematically with treatment frequency, three additional RPL models with interaction terms were generated. The first of these models examined interactions between injection frequency and injection time, the second examined interactions between injection frequency and FLS, and the third examined interactions between injection frequency and ISR. None of these were statistically significant (P > 0.05), suggesting that there was no observed dependence of these three parameters on the level of injection frequency. In addition, interaction models examined the preference differences between four pairs of the following subgroups in the sample: 131 patients with RRMS and 61 patients with all other types of MS, 11 treatment-naïve patients and 181 patients who were not treatment-naïve, 37 injection-naïve patients and 155 patients who were not injection-naïve, and 144 patients who reported that their current MS-related symptoms were moderate or worse and 48 patients who reported that their current MS-related symptoms were mild or better. All tests of the joint significance of the interaction terms indicated that there were no differences in joint preferences for treatment attributes between any of the two groups (P > 0.05). Tests of differences in individual preference weights showed only one notable difference in all four comparisons: patients with mild or better symptoms placed greater weight on decreasing the number of relapses from four relapses over the next 4 years to one relapse (P < 0.01) than patients with moderate or worse symptoms.
4 Discussion
Studies in MS have assessed adherence to injectable DMTs and associated adherence with features of injectable treatments, including injection frequency and injection-related adverse events (e.g., FLS and ISR) [4, 5, 9, 11–13, 17]. Such findings suggest that improvements in the dosing frequency of DMTs will improve adherence and, therefore, treatment outcomes. This study quantifies preferences of patients with MS for features of injectable DMTs, ranging from efficacy and levels of adverse events to features describing administration, such as dosing frequency.
This study found that increasing the time until disability progression and reducing FLS associated with injections were key drivers of patient preference. These features have previously been identified as among the most important treatment features affecting adherence to injectable DMTs [4, 5, 8–16]. Some improvements in DMT injection frequency were as important to patients as improvements in efficacy or injection-related adverse events. In particular, injections administered weekly or less often (i.e., two times per month or once per month) were preferred to injections administered daily or three times weekly. Reducing dosing frequency from three injections per week to two injections per month was as important to patients as lengthening the time until disability progression from 1 to 2 years or improving FLS from 3 days after each injection to 3 days after some injections. In some patients, frequent FLS are correlated with injection frequency; therefore, reducing dose frequency could reduce experiencing injection-related adverse events. However, a long time between injections also increases the incidence and severity of FLS, so the ‘real-world experience’ may be more complex [40]. Reducing dosing frequency from daily to monthly injections was similarly important to patients as lengthening the time until disability progression from 2 to 4 years or improving FLS from 3 days after some injections to none. Given the evidence that injection fatigue, injection fear, and injection-related adverse events are associated with non-adherence [4, 9], these results indicate that changes in injection frequency may be as important as changes in efficacy or experiencing adverse events in determining a patient’s choice of and adherence to injectable DMTs in MS.
Reducing the number of relapses was less important than delaying disability progression but still desirable to patients. Lengthening the time until disability from 1 to 4 years was 2.6 times more important than reducing the number of relapses over 4 years from four to one. This finding is consistent with the findings reported in Johnson et al. [19], in which delaying disease progression was more than twice as important as relapses. Because DMTs reduce relapses [41], physicians emphasize early initiation of treatment and reducing relapses (and, therefore, disability due to relapses) when prescribing treatment. The results of our study suggest that patients’ opinions may differ from physicians’ in that they appear to be more concerned about disability progression than relapses per se. Perhaps these results reflect recognition by patients that relapses often resolve over time, whereas disability progression is permanent. However, it is important to note that our study defined relapses such that they did not cause residual disability, which is not always the case. This was because this definition allowed us to independently identify the importance that patients place on relapse and disability progression, although it does not accurately represent the process by which disability can progress in patients with RRMS.
The preference weights for the different levels of injection time that were used in this study were not statistically different, indicating that patients did not distinguish between the levels of these attributes or had no pronounced preference for one attribute level to another. Furthermore, interactions between injection frequency and injection time, FLS, and ISR were not statistically significant. We therefore did not find any evidence that preferences for these three attributes were dependent on the level of injection frequency. Finally, the results of the study indicated that preferences for the treatment attributes did not differ among subgroups defined by whether the patients had treatment experience, whether the patients had injection experience, and whether the patients had RRMS or other types of MS. This could be a consequence of providing the participants with a reference scenario prior to taking part in the study. It could also be the result of insufficient sample sizes to detect differences in preferences between the subgroups. The only statistically significant difference that the study identified was that patients in this study with mild or better symptoms placed greater weight on reducing relapses than patients with moderate or worse symptoms. Although this suggests that MS-related symptoms may influence preference for a reduction in the number of relapses, we cannot determine whether these differences are due to patient perceptions that vary with disability levels or differences in information provided to patients with different disability levels.
There are a number of limitations to the study which are important when interpreting these results. One limitation is that 19 % of patients were injection-naïve; however, we found no evidence that preferences among patients with and without injection experience were statistically different from one another (data not shown). These results suggest that injection-naïve patients have well-formed preferences regarding features of injectable DMTs, although these patients do not have actual experience with injectable DMTs. Similarly, our analyses indicated that treatment-experienced and treatment-naïve patients had statistically similar preferences. Approximately 13 % of patients had not experienced a relapse in the previous 2 years and 12 patients reported never having experienced a relapse. Furthermore, stability testing suggested that only 82 % of patients were consistent with their choices.
While the use of DCEs in health applications to elicit preferences has been increasing [42–44], there are several potential limitations of this type of assessment. One inherent limitation is that the patients evaluated hypothetical injectable DMT profiles, and their choices among these injectable DMT profiles do not have the same significance as choices involving actual treatments. In addition, patients’ actual treatment choices may reveal different implicit preference weights because actual treatment choices depend on a number of contextual factors (e.g., institutional and financial factors such as formulary status or treatment cost, respectively) that were beyond the scope of this study.
As in any survey research study, sample representativeness may be a potential study limitation. One of the inclusion criteria for survey respondents was that the patient had a self-reported physician diagnosis of MS. Although it is possible that some survey respondents did not actually have MS and simply participated in the survey to earn the modest compensation, the study was designed to minimize this possibility. When invited to take the survey, patients were not told about the subject of the survey. To screen respondents for self-reported physician diagnosis of MS, there was a question asking respondents to select from a list of health conditions that had been diagnosed by a healthcare provider. Only those selecting “multiple sclerosis” from that list were included in the study. The majority of the sample was female, which is consistent with the fact that MS is two to three times more common in women than in men [45]. Another limitation was that the sample was small relative to the population. We cannot fully judge how representative our sample of patients with MS was or whether our results are generalizable to all individuals with MS in the US.
One must use caution in the interpretation of the study results. They should not be used to indicate the overall importance of treatment attributes, but rather the importance of changes in attribute levels that lie within the ranges of attribute levels include in this study. Also, while several of the treatment attributes in this study have been found to influence adherence in other studies, this study does not assess actual adherence, or intended adherence. These choices reflect respondents’ assessments of how variations in attribute levels might affect adherence to hypothetical injectable MS treatments.
The study has a number of strengths derived from the use of best practices [21]. In particular, the survey was carefully designed in collaboration with clinical experts, was pretested using in-depth interviews with patients with MS in the US, and employed a state-of-the-art experimental design. The treatment-choice data were analyzed using advanced RPL methods that avoid estimation bias from unobserved variation in preferences across the sample and within-sample correlation in the choice sequence for each patient. We also tested for the effect of systematic preference differences by treatment experience and disability level.
5 Conclusion
This study provides evidence that patients with MS place approximately equal importance on changes in dosing frequency as they place on delays in disability progression and improvements in FLS caused by some injectable DMTs. The importance that patients place on dosing frequency and other MS treatment attributes may be of interest to healthcare providers recommending treatments to patients, as well as those who influence the selection of MS treatments when writing treatment guidelines, managing formularies, and/or developing reimbursement regimes.
References
Markowitz CE. The current landscape and unmet needs in multiple sclerosis. Am J Manag Care. 2010;16(8 suppl):S211–8.
Cross AH, Naismith RT. Established and novel disease-modifying treatments in multiple sclerosis. J Intern Med. 2014;275:350–63.
Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11:44–7.
Devonshire V, Lapierre Y, Macdonell R, et al. The Global Adherence Project (GAP): a multicenter observational study on adherence to disease-modifying therapies in patients with relapsing-remitting multiple sclerosis. Eur J Neurol. 2011;18:69–77.
Treadaway K, Cutter G, Salter A, et al. Factors that influence adherence with disease-modifying therapy in MS. J Neurol. 2009;256:568–76.
Steinberg S, Faris R, Chang C, et al. Impact of adherence to interferons in the treatment of multiple sclerosis. Clin Drug Investig. 2010;30:89–100.
Tan H, Qian C, Agarwal S, et al. Impact of adherence to disease-modifying therapies on clinical and economic outcomes among patients with multiple sclerosis. Adv Ther. 2010;27:1–11.
Riñon A, Buch M, Holley D, et al. The MS Choice Survey: findings of a study assessing physician and patient perspectives on living with and managing multiple sclerosis. Patient Prefer Adher. 2011;5:629–43.
Giovannoni G, Southam E, Waubant E. Systematic review of disease-modifying therapies to assess unmet needs in multiple sclerosis: tolerability and adherence. Mult Scler. 2012;18:932–46.
Patti F. Optimizing the benefit of multiple sclerosis therapy: the importance of treatment adherence. Patient Prefer Adher. 2010;4:1–9.
Halpern R, Agarwal S, Dembek C, et al. Comparison of adherence and persistence among multiple sclerosis patients treated with disease modifying therapies: a retrospective administrative claims analysis. Patient Prefer Adher. 2011;5:73–84.
Fernández O, Aguera J, Izquierdo G, et al. Adherence to interferon beta-1b treatment in patients with multiple sclerosis in Spain. PLoS One. 2012;7:1–7.
Fox R, Salter A, Tyry T, et al. Treatment discontinuation and disease progression with injectable disease-modifying therapies. Int J MS Care. 2013;15:194–201.
Tremlett H, Oger J. Interrupted therapy: Stopping and switching of the beta-interferons prescribed for MS. Neurology. 2003;61:551–4.
Costello K, Kennedy P, Scanzillo J, et al. Recognizing nonadherence in patients with multiple sclerosis and maintaining treatment adherence in the long term. Medscape J Med. 2008;10:225.
Portaccio E, Zipoli V, Siracusa G, et al. Long-term adherence to interferon beta therapy in relapsing-remitting multiple sclerosis. Eur Neurol. 2008;59:131–5.
Chen C, Baraban E, Stuchiner T, et al. Evaluating medication adherence to disease modifying therapy (DMT) and the associated factors, using data from the Pacific Northwest MS Registry (PNWMSR) [poster]. 29th Congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS), Copenhagen; 2–5 Oct 2013.
Deleu D, Alsharoqi I, Al Jumah MA, et al. Will new injection devices for interferon beta-1a s.c. affect treatment adherence in patients with multiple sclerosis? An expert opinion in the Middle East. Int J Neurosci. 2011;121:171–5.
Johnson F, Van Houtven G, Ozdemir S, et al. Multiple sclerosis patients’ benefit-risk preferences: serious adverse event risks versus treatment efficacy. J Neurol. 2009;256:554–62.
Shingler S, Swinburn P, Ali S, et al. A discrete choice experiment to determine patient preferences for injection devices in multiple sclerosis. J Med Econ. 2013;16:1036–42.
Bridges JFP, Hauber AB, Marshall D, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14:403–13.
Gan TJ, Lubarsky DA, Flood EM, et al. Patient preferences for acute pain treatment. Br J Anaesth. 2004;92:681–8.
Johnson F, Ozdemir S, Mansfield C, et al. Crohn’s disease patients’ risk-benefit preferences: serious adverse event risks versus treatment efficacy. Gastroenterology. 2007;133:769–79.
Bryan S, Buxton M, Sheldon R, et al. Magnetic resonance imaging for the investigation of knee injuries: an investigation of preferences. Health Econ. 1998;7:595–603.
Ryan M, McIntosh E, Shackley P. Methodological issues in the application of conjoint analysis in health care. Health Econ. 1998;7:373–8.
Johnson FR, Lancsar E, Marshall D, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR conjoint analysis discrete-choice experiment experimental design good research practices task force. Value Health. 2013;16:3–13.
Huber J, Zwerina K. The importance of utility balance and efficient choice designs. J Mark Res. 1996;33:307–17.
Kanninen B. Optimal design for multinomial choice experiments. J Mark Res. 2002;39:214–27.
Dey A. Orthogonal fractional factorial designs. New York: Halstead Press; 1985.
Kuhfeld W, Tobias F, Garratt M. Efficient experimental design with marketing research applications. J Mark Res. 1994;31:545–57.
Kuhfeld W. Marketing research methods in SAS: experimental design, choice, conjoint, and graphical techniques. Cary: SAS Institute Inc.; 2010.
Bech M, Kjaer T, Lauridsen J. Does the number of choice sets matter? Results from a web survey applying a discrete choice experiment. Health Econ. 2011;20:273–86.
Maddala T, Philips KA, Johnson FR. An experiment simplifying conjoint analysis designs for measuring preferences. Health Econ. 2003;12:1035–47.
Swait J, Adamowicz W. The influence of task complexity on consumer choice: a latent class model of decision strategy switching. J Consum Res. 2003;28:135–48.
Hohol M, Orav E, Weiner H. Disease steps in multiple sclerosis: a simple approach to evaluate disease progression. Neurology. 1995;45:251–5.
Train K, Sonnier G. Mixed logit with bounded distributions of correlated partworths. In: Scarpa R, Alberini A, editors. Applications of simulation methods in environmental and resource economics. Dordrecht: Springer; 2005. p. 117–34.
Train K. Discrete choice methods with simulation. Cambridge: Cambridge University Press; 2003.
Hensher DA, Rose JM, Greene WH. Applied choice analysis. Cambridge: Cambridge University Press; 2005.
Johnson F, Ozdemir S, Manjunath R, et al. Factors that affect adherence to bipolar disorder treatments. A stated-preference approach. Med Care. 2007;45:545–52.
Panitch H, Goodin D, Francis G, et al. Randomized, comparative study of interferon β-1a treatment regimens in MS: the EVIDENCE trial. Neurology. 2002;59:1496–506.
Hauser S, Chan J, Oksenberg J. Multiple sclerosis: prospects and promise. Ann Neurol. 2013;74:317–27.
Bridges J, Kinter E, Kidane L, et al. Things are looking up since we started listening to patients. Patient. 2008;1:273–82.
De Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21:145–72.
Marshall D, Bridges J, Hauber AB, et al. Conjoint analysis applications in health—how are studies being designed and reported? An update on current practice in the published literature between 2005 and 2008. Patient. 2010;3:249–56.
Markowitz CE. Multiple sclerosis update. Am J Manag Care. 2013;19:s294–300.
Acknowledgments
The authors express their gratitude to Juan Marcos Gonzalez and A. Brett Hauber of RTI Health Solutions for their contributions to the data analysis in this study. The authors would also like to acknowledge Alex Goonesinghe and Neil Marmont (CircleScience) for their support in preparation of this manuscript, which was funded by Biogen.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Poulos and J. Posner are employees of RTI Health Solutions, an independent scientific research organization; J. C. Yang was an employee of RTI Health Solutions at the time of the study. The study that is the subject of this manuscript was conducted by RTI Health Solutions and funded by Biogen. E. Kinter is an employee of Biogen. J. F. P. Bridges and A. Reder were expert consultants who were paid by Biogen for reviewing the protocol and the survey and participating in this research study, but not for the contributions on authoring this paper. Biogen has two injectable treatments that are approved by the US Food and Drug Administration (FDA)/European Medicines Agency (EMA): Avonex® and Plegridy™. The authors have full control of all primary data and agree to allow the journal to review the data if requested.
Contribution of each author
Dr Poulos contributed to the study design, data analysis, interpretation of results, and writing and reporting. Dr Kinter contributed to the study design, interpretation of results, and reporting. Ms Yang contributed to the study design, data analysis, interpretation of results, and reporting. Dr Bridges contributed to the data analysis, interpretation of results, and writing and reporting. Mr Posner contributed to the study design, data analysis, and writing and reporting. Dr Reder contributed to the study design, interpretation of results, and reporting to ensure the clinical applicability and relevance of the survey instrument, data, and study results. All authors approved the manuscript.
Ethical standards
The study was approved by an institutional review board (IRB) in the USA. The IRB operates under a Federal Wide Assurance (#3331) and is registered with both the Office for Human Research Protections and the US FDA. The study was reviewed for compliance with relevant US human subjects regulations (45 CFR 46). All patients provided informed consent prior to their inclusion in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Poulos, C., Kinter, E., Yang, JC. et al. Patient Preferences for Injectable Treatments for Multiple Sclerosis in the United States: A Discrete-Choice Experiment. Patient 9, 171–180 (2016). https://doi.org/10.1007/s40271-015-0136-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-015-0136-x