Abstract
Background
α2-Adrenoceptor agonists are used adjunctively to psychostimulants in treating attention-deficit/hyperactivity disorder (ADHD) when psychostimulants alone do not sufficiently reduce symptoms. However, data on the pharmacokinetic profiles and safety of combination treatments in ADHD are needed.
Objective
The primary objective of this study was to evaluate the pharmacokinetic profiles of guanfacine extended release (GXR) and methylphenidate hydrochloride (MPH) extended release, alone and in combination.
Study Design
This was an open-label, randomized, three-period crossover, drug–drug interaction study.
Setting
The study was conducted at a single clinical research center.
Participants
Thirty-eight healthy adults were randomized in this study.
Interventions
Subjects were administered single oral doses of GXR (Intuniv®; Shire Development LLC, Wayne, PA, USA) 4 mg, MPH (Concerta®; McNeil Pediatrics, Titusville, NJ, USA) 36 mg, or GXR and MPH combined.
Main Outcome Measures
Guanfacine, dexmethylphenidate (d-MPH), and l-methylphenidate (l-MPH) levels were measured with blood samples collected predose and up to 72 h postdose. Safety evaluations included treatment-emergent adverse events (TEAEs), vital signs, and electrocardiograms (ECGs).
Results
Thirty-five subjects completed the study. Analyses of the 90 % confidence intervals (CIs) for the geometric mean ratios of the maximum plasma concentration (Cmax) and area under the concentration–time curve extrapolated to infinity (AUC∞) values for guanfacine and d-MPH following administration of GXR or MPH alone or combined met strict bioequivalence criteria (90 % CIs within the interval of 0.80–1.25). Overall, combining GXR and MPH did not alter the pharmacokinetic parameters of either medication. Sixteen subjects (42.1 %) had at least one TEAE. The most commonly reported TEAEs included headache and dizziness following GXR, MPH, and GXR and MPH combined. Two subjects had clinically significant abnormalities in ECG results following coadministration: both events were mild and resolved the same day.
Conclusions
In this short-term, open-label study of healthy adults, coadministration of GXR and MPH did not result in significant pharmacokinetic drug–drug interactions. No unique TEAEs were observed with coadministration of GXR and MPH compared with either treatment alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
α2-Adrenoceptor agonists such as clonidine and guanfacine are used as adjunctive treatments to psychostimulants in the treatment of attention-deficit/hyperactivity disorder (ADHD) when the response to psychostimulants alone is suboptimal [1–4]. Guanfacine extended release (GXR), a selective α2A-adrenoceptor agonist, is approved by the US Food and Drug Administration as monotherapy and as adjunctive therapy to psychostimulant medications for the treatment of ADHD in children and adolescents aged 6–17 years [5].
The safety and efficacy of GXR in combination with psychostimulants were demonstrated in two trials. An open-label, 9-week study of 75 children and adolescents with ADHD who had operationally defined suboptimal responses to a psychostimulant found that the addition of GXR did not result in unique adverse events (AEs) compared with those reported historically with either treatment alone, and was associated with significant improvements in ADHD symptoms [4]. In addition, a large, multicenter, double-blind, randomized, placebo-controlled study of GXR as adjunctive therapy to psychostimulants in children and adolescents aged 6–17 years with ADHD who exhibited suboptimal responses to psychostimulants alone confirmed the results of the earlier open-label investigation and provided further support for the effectiveness of GXR as an adjunctive therapy to psychostimulants in this age group [6]. Since methylphenidate hydrochloride (MPH) is considered among first-line treatments for ADHD because of its established efficacy and safety profile [7], the potential for pharmacokinetic drug–drug interactions between GXR and MPH requires thorough investigation.
Although guanfacine is known to be metabolized by the cytochrome p450 (CYP) 3A4 pathway [5], MPH is primarily metabolized by de-esterification [8]. Even though MPH is not metabolized by the CYP system and is neither an inducer nor an inhibitor of the system [8, 9], it is important to study the pharmacokinetics of GXR in combination with MPH to confirm the lack of metabolic interactions between these two therapies.
Although data on the pharmacokinetics of GXR used in combination with MPH are limited, the pharmacokinetic profiles of GXR or MPH alone have been well characterized [5, 10]. GXR is readily absorbed and is approximately 70 % bound to plasma proteins, independent of the drug concentration [5]. Oral administration of single doses of GXR in adults leads to a maximum guanfacine plasma concentration (Cmax) in approximately 5 h [5, 11]. A single-dose pharmacokinetic study of GXR in healthy adults demonstrated that the single-dose pharmacokinetic parameters of GXR 1-, 2-, and 4-mg tablets were statistically linear, with the Cmax, area under the plasma concentration–time curve (AUC) to the last measurable concentration at time t (AUCt), and AUC extrapolated to infinity (AUC∞) for guanfacine increasing with dose [11]. MPH is also readily absorbed, with MPH mean concentrations initially plateauing at 1–4 h and ascending to maximum plasma concentrations between 6–10 h after administration [10, 12].
The safety profiles of both GXR and MPH alone have also been examined in previous studies. The most common treatment-emergent AEs (TEAEs) reported in the short-term pivotal studies of GXR included somnolence, fatigue, upper abdominal pain, and sedation [13, 14]. The most common adverse reactions reported in clinical trials of MPH included upper abdominal pain, vomiting, dizziness, and insomnia [10]. The effects of these medications on cardiovascular parameters have also been examined. In subjects who received GXR in clinical trials, systolic blood pressure (SBP), diastolic blood pressure (DBP), and pulse rate decreased as actual doses increased, and they then returned toward baseline as doses stabilized and were tapered down [13–15]. These changes were expected, given that immediate-release guanfacine was initially used as an antihypertensive agent. In contrast, increases in SBP, DBP, and pulse rate are often reported with MPH treatment [16, 17]. Consequently, there is a need to investigate the impact of coadministration of GXR and MPH on these parameters as well as the overall safety of this combination.
The primary purpose of the present study (ClinicalTrials.gov identifier: NCT00901576) was to evaluate the pharmacokinetic profiles of GXR and MPH, alone and in combination, in healthy adults. Evaluating the safety of GXR, MPH, and coadministration of both drugs was a secondary objective of this study.
2 Materials and Methods
This open-label, randomized, single-center, three-period crossover, drug–drug interaction study was conducted from 18 May to 6 July 2009. Healthy adults were randomized to receive single doses of GXR (Intuniv®; Shire Development LLC, Wayne, PA, USA) 4 mg, MPH extended release (Concerta®; McNeil Pediatrics, Titusville, NJ, USA) 36 mg, and the combination of GXR 4 mg and MPH 36 mg. Institutional review board approval was received to conduct the study, and informed consent was provided by all subjects. The study was conducted in accordance with current applicable regulations, International Conference on Harmonisation (ICH) Good Clinical Practice (GCP) Guideline E6, local ethical and legal requirements, and the principles of the 18th World Medical Assembly and amendments.
2.1 Subjects
The study subjects were healthy volunteers aged 18–45 years who exhibited no significant or relevant abnormalities in medical history, physical examination, vital signs, or laboratory evaluation that were reasonably likely to interfere with the subject’s participation in or ability to complete the study. Normal or clinically insignificant electrocardiogram (ECG) findings were also required for inclusion in the study.
The study exclusion criteria included current or recurrent disease (such as cardiovascular, renal, liver, or gastrointestinal diseases, malignancy, or other conditions) that could affect clinical or laboratory assessments or the action, absorption, or disposition of the investigational agents. Cardiac conditions, including a history of hypertension or a known family history of sudden cardiac death or ventricular arrhythmia, were also exclusionary. Other exclusion criteria included current use of any medication (with the exception of hormone replacement therapy or hormonal contraceptives), use of tobacco in any form, routine consumption of more than 2 units of caffeine per day, or the presence of a medical or psychiatric disorder that may have required treatment or made the subject unlikely to comply with the study’s requirements or complete the study.
2.2 Study Design
The study subjects were randomly assigned to one of six administration sequences, each consisting of three treatment periods separated by a washout period of at least 7 days in duration. The subjects were allocated a 4-digit randomization number, starting at 1001, immediately prior to the predose pharmacokinetic blood draw after eligibility was determined. At least six subjects were to be randomized to each of the six possible treatment sequences (1: GXR, MPH, GXR + MPH; 2: GXR, GXR + MPH, MPH; 3: MPH, GXR, GXR + MPH; 4: MPH, GXR + MPH, GXR; 5: GXR + MPH, GXR, MPH; 6: GXR + MPH, MPH, GXR).
The study medication was administered at a clinical research center that was supervised by clinical staff. The subjects were required to fast for approximately 10 h prior to the administration of each dose of study medication. All study medication was given with water in the morning. A moderate-fat lunch was provided 4 h after dose administration. The subjects were confined at the center during each treatment period and remained there until all discharge procedures were completed, approximately 72 h after the subjects received the treatment.
2.3 Pharmacokinetic and Safety Assessments
Vital signs were monitored, blood samples collected, and ECG data obtained before administration of the study medication for each treatment period. Guanfacine, dexmethylphenidate (d-MPH), and l-methylphenidate (l-MPH) levels were measured in plasma produced from blood samples collected predose and at 0.5, 1.0, 1.5, 2.0, 3.0, 4.0, 6.0, 8.0, 12, 24, 30, 48, and 72 h postdose. Immediately after blood collection, the blood samples were kept on ice until they were centrifuged, within 30 min following the blood draw.
Plasma concentrations of guanfacine, d-MPH, and l-MPH were measured using liquid chromatography with tandem mass spectrometry (LC–MS/MS) detection methods that were validated for the quantitation of guanfacine, d-MPH, and l-MPH in human K3-EDTA plasma. The method utilized a liquid-liquid extraction procedure prior to LC–MS/MS analysis. The stable isotope-labeled compounds guanfacine (13C15N3) and MPH-D9 were used as the internal standards for guanfacine and d/l-MPH, respectively.
For guanfacine, the LC–MS/MS analysis was carried out with a Sciex 4000 mass spectrometer coupled with a Shimadzu liquid chromatography (LC) pump (model LC-10AT) and Perkin-Elmer 200 series autosampler. The chromatographic separation was achieved on a XBridge phenyl, 3.5 μm, 4.60 × 50 mm LC column, with a mobile phase. The mass spectrometer was operated in positive electrospray ionization mode, and the resolution settings used were unit for Q1 and low for Q3. The multiple reaction monitoring (MRM) transition was m/z 246 → 60 for guanfacine, and the MRM transition was m/z 250 → 159 for the internal standard, guanfacine (13C15N3).
For d/l-MPH, the LC–MS/MS analysis was carried out with a Sciex 5000 mass spectrometer coupled with a Shimadzu LC pump (model LC-10AT) and a Perkin-Elmer 200 series autosampler. The chromatographic separation was achieved on a ChiralPak AD-H, 4.60 × 150 mm, 5 μm LC–MS column, with a mobile phase. The mass spectrometer was operated in positive mode, and the resolution setting used was unit for both Q1 and Q3. The MRM transition was m/z 234 → 84 for MPH, and the MRM transition was m/z 243 → 93 for the internal standard, MPH-D9.
The assay ranges were from 0.05 to 50 ng/mL for guanfacine analysis, based on a plasma sample volume of 200 μL, and from 0.25 to 100 ng/mL for d-MPH and l-MPH analysis, based on a plasma sample volume of 100 μL.
Safety was evaluated by collecting data on reported AEs, physical examination findings, vital signs, and 12-lead ECGs. At the end of each treatment period, biochemical and hematologic assessments were performed and urinalysis was conducted. Staff contacted subjects 7 days after the last dose of the last investigational agent to collect data on new-onset AEs and other treatment-related concerns.
2.4 Statistical Methods
The primary analysis was the pharmacokinetic analysis performed using data from the pharmacokinetic population. This population consisted of all subjects who received at least one dose of study medication, had at least one postdose safety assessment, and had evaluable concentration–time profiles for guanfacine, d-MPH, or l-MPH.
Pharmacokinetic parameters were determined from the plasma concentration–time data by noncompartmental analysis and included Cmax, time to Cmax (tmax), AUCt, AUC∞, apparent elimination half-life (t½), apparent oral-dose clearance (CL/F), and apparent volume of distribution during the terminal phase after oral administration (Vλz/F). CL/F and Vλz/F were corrected for bodyweight.
Summary statistics, including the numbers of observations, means, standard deviations (SDs), medians, maximums, minimums, and geometric means, were determined for all pharmacokinetic parameters for all treatment regimens.
The means of the log-transformed pharmacokinetic parameters were compared among (between) treatments, using an analysis of variance (ANOVA) with sequence, period, and treatment as fixed effects, and subject nested within sequence as a random effect for a crossover study design. To estimate the magnitude of the treatment differences in Cmax and AUC∞, the geometric mean ratio (GMR, defined as the least squares mean difference in the log-transformed parameters back-transformed to the original scale) and their 90 % confidence intervals (CIs) were also calculated.
The hypothesis of a drug interaction of GXR and MPH would be rejected if either of the following were to fall within the interval of 0.80–1.25: (i) the 90 % CIs of the GMR of guanfacine following GXR alone to guanfacine following GXR in combination with MPH; or (ii) the 90 % CIs of the GMR of d-MPH following MPH alone to d-MPH following MPH in combination with GXR. If the CIs were not entirely contained within the interval of 0.80–1.25, then the clinical significance of such mean ratio estimates and CIs would be interpreted within the context of the therapeutic index.
The available within-subject estimates of the SDs of the log-transformed parameters AUC∞ (SD = 0.26) and Cmax (SD = 0.31) for GXR were pooled from previous studies of GXR. Data from the ‘Summary Basis of Approvable/Approval’ letter for MPH indicated that the intrasubject coefficient of variation for MPH was 9.6 %, based on AUC∞ (approximates to a within-subject SD of 9.5 for log-transformed AUC∞). A previous study of MPH reported a within-subject SD of Cmax and AUC∞ of 0.18 [18]. To demonstrate equivalence, allowing for a 5 % difference in true means, if the true within-subject SD was 0.25 (based on the higher of the AUCs between GXR and MPH), 36 subjects (six per sequence) were required to achieve 90 % power.
3 Results
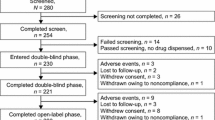
Thirty-eight subjects were randomized, and 35 (92.1 %) completed the study. No subject withdrew because of an AE, and there were no substantial differences among treatment sequences in the reasons for study discontinuation. Three subjects did not complete the study: two withdrew from the study and one was withdrawn by the study investigator before she received GXR and MPH in combination, because she had tolerated GXR and MPH poorly when each was administered alone. Demographics and baseline characteristics are reported in Table 1.
3.1 Pharmacokinetic Results
A summary of pharmacokinetic parameters of guanfacine and d-MPH following administration of GXR alone, MPH alone, and GXR and MPH in combination is presented in Table 2.
The mean plasma guanfacine concentrations following administration of GXR alone and in combination with MPH are shown in Fig. 1. No noteworthy differences in guanfacine Cmax, AUC∞, and bodyweight-normalized CL/F and Vλz/F were noted after administration of GXR alone or in combination with MPH. The 90 % CIs of the GMRs for Cmax and AUC∞ for guanfacine following GXR alone or in combination with MPH met strict bioequivalence criteria requiring 90 % CIs to fall within the interval of 0.80–1.25 (Cmax GMR 1.065, 90 % CI 0.945–1.200; AUC∞ GMR 1.109, 90 % CI 0.997–1.235), indicating that GXR alone and GXR in combination with MPH met the criteria for bioequivalence.
Mean plasma guanfacine concentrations over time following administration of guanfacine extended release (GXR) alone and in combination with methylphenidate hydrochloride (MPH). A time shift has been applied to the figure; values have been slightly staggered on the x-axis for clarity, as some values were similar between the two treatment regimens
The mean plasma concentrations of d-MPH following administration of MPH alone and in combination with GXR are shown in Fig. 2. Maximum plasma concentrations of d-MPH were observed at a median of 6 h when MPH was administered alone and at 8 h when MPH was administered in combination with GXR (Table 2). Cmax, AUC∞, and bodyweight-normalized CL/F and Vλz/F results for d-MPH were similar after administration of MPH alone and in combination with GXR. In addition, no noteworthy differences in l-MPH concentrations following administration of MPH alone or in combination with GXR were noted (Table 2). Moreover, the 90 % CIs of the GMRs for Cmax and AUC∞ with d-MPH following MPH alone or in combination with GXR met strict bioequivalence criteria requiring 90 % CIs to fall within the interval of 0.80–1.25 (Cmax GMR 0.957, 90 % CI 0.907–1.01; AUC∞ GMR 1.001, 90 % CI 0.958–1.046), demonstrating the bioequivalence of MPH alone and with GXR.
Mean plasma dexmethylphenidate (d-MPH) concentrations over time following administration of methylphenidate hydrochloride (MPH) alone and in combination with guanfacine extended release (GXR). A time shift has been applied to the figure; values have been slightly staggered on the x-axis for clarity, as some values were similar between the two treatment regimens
3.2 Safety Results
Sixteen subjects (42.1 %) had at least one TEAE. The most commonly reported TEAEs included headache (5.4, 10.5, and 8.1 % following GXR, MPH, and GXR and MPH combined, respectively), dizziness (2.7, 5.3, and 2.7 %, respectively), and postural dizziness (8.1, 0.0 and 0.0 %, respectively). The TEAEs observed were consistent with the known effects of GXR and MPH administered alone.
One event (orthostatic syncope) was considered serious but was mild in severity and did not lead to study discontinuation. The subject was a 22-year-old male who had no relevant history, no history of syncope, and no recent illness. The event occurred 2 h after he received his first treatment, which was a single oral dose of GXR 4 mg alone. The event lasted less than 1 minute, and the subject recovered spontaneously and completed the study.
No subject had a severe AE or an AE leading to withdrawal. The majority of TEAEs were mild, and no differences in the types, incidences, or severity of TEAEs were reported across treatments. No clinically meaningful differences in biochemistry, hematology, or urinalysis results across treatment groups were noted.
The effects of monotherapy with GXR or MPH on vital signs, including SBP, DBP, and supine pulse rate, were as expected. Figure 3 shows the mean supine pulse rates over the course of 12 h following administration of GXR, MPH, and GXR and MPH. Following administration of GXR, there was a modest decrease in the mean pulse rate, which started returning to baseline levels 6 h postdose. In contrast, a modest increase in the mean supine pulse rate was seen with MPH.
Changes in supine SBP (Fig. 4a) and DBP (Fig. 4b) were also noted after administration of GXR and MPH alone. Modest decreases in blood pressure (BP) were seen with GXR, and small increases in BP were reported with MPH.
As shown in Figs. 3 and 4, the results for GXR and MPH combined suggested a potential offsetting effect on pulse rate (Fig. 3) and BP (Fig. 4) with coadministration, compared with the effects observed when each medication was administered alone. Postural orthostatic changes in pulse rate and BP after coadministration of GXR and MPH were highly variable. There did not appear to be clinically important postural orthostatic changes in pulse rate or BP following coadministration of GXR and MPH compared with GXR alone.
Two subjects had potentially clinically significant abnormalities in ECG results based upon prespecified parameters (asymptomatic supraventricular extrasystoles and a wandering atrial pacemaker). Both abnormalities occurred 2 h after coadministration of GXR and MPH, were mild in severity, and resolved the same day. These abnormalities were determined not to be clinically meaningful ECG changes; overall, ECG results were consistent with the known effects of these compounds.
4 Discussion
In clinical practice, α2-adrenoceptor agonists such as GXR have been coadministered with psychostimulants such as MPH to treat ADHD, and GXR is now indicated as adjunctive therapy to psychostimulant medications for the treatment of ADHD [2, 19]. Although guanfacine is known to be metabolized by the CYP3A4 system [5], and MPH is neither an inducer nor an inhibitor of that system, it was considered prudent to evaluate the pharmacokinetics of this combination.
In this study of healthy adults, no pharmacokinetic drug interactions were observed with coadministration of GXR and MPH. No noteworthy differences in pharmacokinetic parameters were observed with GXR and MPH in combination compared with either medication alone. In fact, analyses of the 90 % CIs of the GMRs for Cmax and AUC∞ of guanfacine alone or in combination with MPH, or MPH alone or in combination with GXR, met strict bioequivalence criteria (90 % CIs within the interval of 0.80–1.25).
The TEAEs reported in this study were expected and consistent with those observed historically with psychostimulants administered alone or with GXR [5, 10, 13, 14, 20]. No differences in the type, incidence, or severity of TEAEs among treatment groups were observed, and no subject discontinued treatment because of a TEAE.
No clinically meaningful changes in ECG results, laboratory parameters, or physical examination findings were noted during the study. Modest changes in BP and supine pulse rate were seen with GXR and MPH treatment alone and were expected. When GXR and MPH were coadministered as single doses, data from this study indicated a potential offsetting effect on pulse rate and BP, compared with the effects typically observed with either treatment alone. Because this study evaluated the impact of only a single dose of GXR and MPH, alone and in combination, it is unknown if this effect would continue with longer-term therapy.
This study had several limitations. It was a small, short-term, open-label study that only included healthy adult men and women. This population is not representative of the range of patients who are treated with GXR coadministered with a stimulant. Additionally, patients with ADHD have a higher prevalence of comorbid disorders, such as depression, anxiety, and oppositional disorder, compared with control subjects, and subjects with those disorders were excluded [21]. As this was a single-dose study, rather than a multiple-dose study, the effects seen in the study may not be representative of those seen at steady state. Because of these limitations, the findings of this study may not be readily extrapolated to the therapeutic setting. Moreover, because of the short-term nature of the study, the implications of the results for long-term management of ADHD with a combination of GXR and MPH are also unknown.
This study was not designed to robustly assess the cardiovascular effects of either GXR or MPH alone or in combination. In fact, the study excluded subjects with comorbidities that might contribute to cardiac AEs and subjects with medical or psychiatric disorders. Therefore, it is important to be cautious when generalizing from the results of this study.
5 Conclusions
In this short-term, open-label study of healthy adults, coadministration of GXR and MPH did not result in significant pharmacokinetic drug–drug interactions. In addition, no unique TEAEs were observed with coadministration of GXR and MPH compared with either treatment alone.
References
Adler LA, Reingold LS, Morrill MS, et al. Combination pharmacotherapy for adult ADHD. Curr Psychiatry Rep. 2006;8(5):409–15.
Popper CW. Combining methylphenidate and clonidine: pharmacologic questions and news reports about sudden death. J Child Adolesc Psychopharmacol. 1995;5(3):157–66.
Brown TE. Atomoxetine and stimulants in combination for treatment of attention deficit hyperactivity disorder: four case reports. J Child Adolesc Psychopharmacol. 2004;14(1):129–36.
Spencer TJ, Greenbaum M, Ginsberg LD, et al. Safety and effectiveness of coadministration of guanfacine extended release and psychostimulants in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19(5):501–10.
Intuniv (package insert). Wayne: Shire Pharmaceuticals Inc.; 2011.
Wilens TE, Bukstein O, Brams M, et al. A controlled trial of extended-release guanfacine and psychostimulants for attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2012;51(1):74–85.
Pliszka SR, Crismon ML, Hughes CW, The Texas Consensus Conference Panel on Pharmacotherapy of Childhood Attention-Deficit/Hyperactivity Disorder, et al. The Texas Children’s Medication Algorithm Project: revision of the algorithm for pharmacotherapy of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2006;45(6):642–57.
McNeil Specialty Pharmaceuticals. Concerta (methylphenidate hydrochloride) extended-release tablets: briefing document. FDA PAC Mar 2006. http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4210b_14_McNeil%20FDA%20PAC%20March%2006%20Briefing%20Document.pdf. Accessed 26 Apr 2012.
Greenblatt DJ, Von Moltke LL, Harmatz JS, et al. Pharmacokinetics, pharmacodynamics, and drug disposition. In: Davis KL, Charney D, Coyle JT, Nemeroff C, editors. Neuropsychopharmacology: the fifth generation of progress. Philadelphia: Lippincott Williams & Wilkins; 2002.
Concerta (package insert). Titusville: McNeil Pediatrics; 2010.
Swearingen D, Pennick M, Shojaei A, et al. A phase I, randomized, open-label, crossover study of the single-dose pharmacokinetic properties of guanfacine extended-release 1-, 2-, and 4-mg tablets in healthy adults. Clin Ther. 2007;29(4):617–25.
Markowitz JS, Straughn AB, Patrick KS, et al. Pharmacokinetics of methylphenidate after oral administration of two modified-release formulations in healthy adults. Clin Pharmacokinet. 2003;42(4):393–401.
Biederman J, Melmed RD, Patel A, The SPD503 Study Group, et al. A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics. 2008;121(1):e73–84.
Sallee F, McGough J, Wigal T, The SPD503 Study Group, et al. Guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder: a placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2009;48(2):155–65.
Biederman J, Melmed RD, Patel A, et al. Long-term, open-label extension study of guanfacine extended release in children and adolescents with ADHD. CNS Spectr. 2008;13(12):1047–55.
Adler LA, Zimmerman B, Starr HL, et al. Efficacy and safety of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, double-blind, parallel group, dose-escalation study. J Clin Psychopharmacol. 2009;29(3):239–47.
Biederman J, Mick E, Surman C, et al. A randomized, placebo-controlled trial of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2006;59(9):829–35.
Meyer MC, Straughn AB, Jarvi EJ, et al. Bioequivalence of methylphenidate immediate-release tablets using a replicated study design to characterize intrasubject variability. Pharm Res. 2000;17(4):381–4.
Pohl GM, Van Brunt DL, Ye W, et al. A retrospective claims analysis of combination therapy in the treatment of adult attention-deficit/hyperactivity disorder (ADHD). BMC Health Serv Res. 2009;9:95.
Wilens TE, Spencer TJ. The stimulants revisited. Child Adolesc Psychiatr Clin N Am. 2000;9(3):573–603. viii.
Secnik K, Swensen A, Lage MJ. Comorbidities and costs of adult patients diagnosed with attention-deficit hyperactivity disorder. Pharmacoeconomics. 2005;23(1):93–102.
Acknowledgments
With great sadness, the authors wish to acknowledge the passing of our colleague, Mary Haffey, and recognize her contributions to this article.
Funding and Individual Contributions
This clinical research was funded by the sponsor, Shire Development LLC (Wayne, PA, USA). Under direction from the authors, Jennifer Steeber PhD [an employee of SCI Scientific Communications & Information (SCI); Parsippany, NJ, USA] provided writing assistance for this publication. Editorial assistance in the form of proofreading, copy editing, and fact checking was also provided by SCI. Additional editorial support was provided by Wilson Joe, PhD, of MedErgy (Yardley, PA, USA). Jonathan Rubin MD MBA, Carla White BSc CStat, Edward Johnson, Michael Kahn, and Gina D’Angelo PharmD MBA from Shire Development LLC, and Sharon Youcha MD (who was an employee at Shire Development LLC at the time of the study) also reviewed and edited the manuscript for scientific accuracy. Shire Development LLC provided funding to SCI and MedErgy for support in writing and editing this manuscript. Although the sponsor was involved in the design, collection, analysis, interpretation, and fact checking of information, the content of this manuscript, the ultimate interpretation, the accuracy of the study results, and the decision to submit it for publication in Drugs in R&D was made by the authors independently.
Conflict of Interest Disclosures
Benno Roesch is an employee of Advanced Biomedical Research, Inc. (Hackensack, NJ, USA). Mary Corcoran, Phillip Wang, Jaideep Purkayastha, and James Ermer are employees of Shire Development LLC (Wayne, PA, USA) and hold stock and/or stock options in Shire. Mary Haffey was an employee of Shire Development LLC and held stock and/or stock options in Shire. Annette Stevenson is a consultant of Shire Development LLC. Patrick Martin is an employee of Shire Development LLC. James Ermer received financial support from Shire Development LLC for travel to meetings for this study. The authors have no other conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Haffey: deceased.
Clinical trial registration number (ClinicalTrials.gov): NCT00901576.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Roesch, B., Corcoran, M., Haffey, M. et al. Pharmacokinetics of Coadministration of Guanfacine Extended Release and Methylphenidate Extended Release. Drugs R D 13, 53–61 (2013). https://doi.org/10.1007/s40268-013-0009-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-013-0009-5