Abstract
Background
Hypertension and diabetes mellitus are independent risk factors for cardiovascular diseases. Due to the cardioprotective nature of angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs), they are recommended for patients with comorbid hypertension and diabetes. However, poor adherence to ACEIs/ARBs among older adults is a major public health concern. This study aimed to assess the effectiveness of a telephonic motivational interviewing (MI) intervention conducted by pharmacy students among a nonadherent older population (≥ 65 years old) with diabetes and hypertension.
Methods
Patients continuously enrolled in a Medicare Advantage Plan who received an ACEI/ARB prescription between July 2017 and December 2017 were identified. Group-based trajectory modeling (GBTM) was used to identify distinct patterns of ACEI/ARB adherence during the 1-year baseline period: adherent, gaps in adherence, gradual decline, and rapid decline in adherence. Patients from the three nonadherent trajectories were randomized into MI intervention or control group. The intervention consisted of an initial call and five follow-up calls administered by MI-trained pharmacy students and tailored to the baseline ACEI/ARB adherence trajectories. The primary outcome was adherence to ACEI/ARB during the 6- and 12-month periods post-MI implementation. The secondary outcome was discontinuation, defined as no refills for ACEI/ARB during the 6- and 12-month periods post-MI implementation. Multivariable regression analyses examined the impact of MI intervention on ACEI/ARB adherence and discontinuation while adjusting for baseline covariates.
Results
A total of 240 patients in the intervention group and 480 patients as randomly selected controls were included in this study. At 6 months, patients receiving the MI intervention had significantly better adherence (β = 0.06; p = 0.03) compared with the controls. Linear and logistic regression models also showed patients in the intervention group were more likely to be adherent than controls within 12 months of intervention implementation (β = 0.06; p = 0.02 and OR: 1.46; 95% CI 1.05–2.04, respectively). MI intervention did not have any significant impact on the ACEI/ARB discontinuation.
Conclusion
Patients who received the MI intervention were more likely to be adherent at 6 and 12 months following the intervention initiation, despite gaps in the follow-up calls due to COVID-19. Pharmacist-led MI intervention is an effective behavioral strategy to improve medication adherence among older adults and tailoring the intervention to past adherence patterns may enhance the intervention effectiveness.
This study was registered with the United States National Institutes of Health (ClinicalTrials.gov identifier NCT03985098).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Phone-based motivational interviewing intervention conducted by student pharmacists has a promising effect on improving adherence to antihypertensive medications among the nonadherent older population. |
Tailoring interventions based on past adherence trajectories may enhance intervention effectiveness due to providing more insight into patient behavior. |
1 Introduction
Hypertension frequently coexists with diabetes mellitus and is responsible for 75% of cardiovascular events in the diabetic population as both conditions are recognized as the leading risk factors for heart disease and stroke in the United States [1]. Data from The Centers for Disease Control and Prevention (CDC) shows about 877,500 Americans die annually due to cardiovascular diseases (CVD) [1]. Approximately 116 million of US adults (47%) have hypertension with only one fourth of those being under control [2]. Findings from the National Health and Nutrition Examination Survey (NHANES) conducted between 2015 and 2018 revealed that nearly 60% of patients have uncontrolled blood pressure (≥ 140/90 mm Hg) despite being treated with hypertension medications [2]. Failure to take medications as prescribed may play a significant role in having poor blood pressure (BP) control [3].
Pharmacotherapy of hypertension is critical in patients with diabetes as it is associated with lower risk of cardiovascular events and all-cause mortality [4]. Angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) have established benefits for treating hypertension in individuals with diabetes [5,6,7,8]. The beneficial effects go beyond blood pressure control, lowering the risk of micro- and macrovascular adverse events in addition to decreasing all-cause mortality, cardiac morbidity, and mortality [5, 7,8,9,10,11,12]. However, adherence to antihypertensive medications—defined as the extent to which a patient follows the physician’s prescription order—is a common concern [13]. Poor medication adherence including failure to initiate the treatment, implement the dosing regimen, or persist on therapy, results in suboptimal BP control and hence higher risk of cardiovascular-related complications, mortality, and healthcare costs [14,15,16,17].
Different strategies have been studied to enhance patient adherence to medications used for chronic illnesses. However, a majority of the currently used methods are ineffective and complex [18]. Motivational interviewing (MI) is a patient-centered type of counseling which focuses on enhancing self-motivation and commitment to behavior change through a collaborative and supportive communication with a healthcare provider [19,20,21]. MI-based interventions have demonstrated promising effects in improving medication adherence across a wide range of chronic conditions [22].
In observational studies using pharmacy claims databases, medication possession ratio (MPR) and proportion of days covered (PDC) are common methods for measuring medication adherence. However, in recent years, the use of group-based trajectory modeling (GBTM) has been growing due to the advantages over traditional techniques. Unlike PDC that is calculated as a single number to characterize adherence within a specified time, GBTM creates trajectory groups that incorporate both quantity and timing of medication availability throughout the study period [23, 24]. GBTM describes longitudinal patterns of adherence instead of grouping patients as adherent versus nonadherent, which provides invaluable information on patient behavior and underlying barriers to medication adherence. In addition, GBTM creates clusters of patients sharing common characteristics that could better inform the development of tailored interventions for nonadherent individuals [23, 25,26,27,28,29].
This study aimed to examine the effect of a phone-based MI intervention conducted by trained student pharmacists on improving adherence and persistence to ACEIs/ARBs among nonadherent hypertension and diabetes patients enrolled in a Medicare Advantage Plan (MAP). Building upon the prior research, the objective of this study was to tailor the intervention further using adherence trajectories and enhance the intervention effectiveness.
2 Methods
2.1 Study Design
This prospective study was conducted among nonadherent patients enrolled in a Texas MAP from July 2016 to July 2021. The MAP provides comprehensive medical/drug coverage, combining all Medicare benefits into one, utilizing a designated network of doctors and hospitals who work together to provide the best care in a cost-effective manner. A previous phase I retrospective study identified nonadherent ACEI/ARB patients using GBTM [30]. This phase II prospective study involved conducting an MI intervention among the nonadherent patients identified in the phase I study and was followed-up for 1 year post-MI implementation. Figure 1 illustrates the study design and timeline. This study was registered with the United States National Institutes of Health (ClinicalTrials.gov identifier NCT03985098).
2.2 Identifying Patients for Telephonic Motivational Interviewing (MI) Intervention
A previous phase I retrospective cohort study identified patients with comorbid hypertension and diabetes mellitus with an ACEI/ARB prescription using the administrative claims data. Patients with an ACEI/ARB refill between July 2017 and December 2017 were included. Patients were also required to be continuously enrolled from July 2016 to December 2018. Patients were excluded from the study if they (a) disenrolled from the health plan, (b) had a diagnosis of dementia between July 2016 and July 2017, or c) had any contraindication for ACEI/ARB use such as angioedema, hyperkalemia, and renal artery stenosis between July 2016 and July 2017. A total of 22,774 patients met the inclusion criteria. Adherence to ACEI/ARB was measured using GBTM, and the model with four distinct trajectories of adherence was identified: adherent, rapid decline in adherence, gaps in adherence, and gradual decline in adherence (Fig. 2). A total of 7868 patients from the latter three nonadherent trajectories were randomized into the MI intervention and control groups. Of these, 5901 patients were randomized to the intervention group (3:1). Eligible candidates of the intervention group received a brief telephone intervention until a sample size of 250 was reached. Each intervention patient was randomly assigned two controls from the nonadherent cohort.
G-power 3.1 statistical software estimated that a total of 409 patients would be needed for a two-tailed analysis using logistic regression at a 0.05 α-level, 0.10 β-level (90% power), and a 1.5 odds ratio. Approximately 230 patients are needed for multiple linear regression analysis with an effect size of 0.10. A total of 500 patients (250 for intervention and control group each) would be needed to have enough power to detect differences at 12 months in case of a 5–7% patient disenrollment from the plan [29, 31].
2.3 MI Training
A telephone-based MI intervention was implemented by fourth-year pharmacy students (under the supervision of preceptors) who participated in 6-week Advanced Pharmacy Practice Experiences (APPE) rotations at the MAP. The pharmacy students attended a 3-day training session facilitated by an experienced researcher. The MI training included lectures, MI skill demonstration, and guided practice through role-playing. The pharmacy students also had several practice sessions with trained standardized patients. The MI trainer evaluated this practice session to ensure student proficiency in MI skills and MI spirit using a 7-point Likert-type scale (1 = poor/never to 7 = excellent/always) [32].
2.4 Customization of Intervention
During the phase I retrospective study, the GBTM identified various barriers to adherence like gender, age group 71–75 years, other languages, prevalent statin users, having ≥ 90-day refill, two or more concomitant medications on index date, and presence of comorbidities like myocardial infarction, end-stage renal disease, and depression [30]. MI-trained faculty and the MI trainer developed customized education material specific to each of the lower adherence trajectories (rapid decline, gradual decline, gaps in adherence) that could help students during the implementation of MI. The past adherence trajectories further guided the development of strategies to improve patient adherence. Additional adherence barriers were obtained from literature, including forgetfulness, cost, perception about the treatment/disease, regimen complexity, fear of adverse events, pharmacy/physician-related issues, and transportation [29, 33,34,35,36]. Finally, a protocol based on the Ask-Provide-Ask approach—a pharmacist adaptation for the Elicit-Provide-Elicit of MI—was developed for each of the lower adherence trajectories that summarized the customized education that is likely to benefit patients associated with each trajectory [37].
2.5 Implementation of Intervention
The MI-trained pharmacy students implemented the MI intervention from May 2019 to March 2021. The intervention consisted of an initial telephonic call followed by five follow-up calls supervised by pharmacy preceptors. The phone-based MI intervention helped reach patients that met the eligibility criteria regardless of their location in Texas, which was advantageous compared with conducting a physical intervention. The recruitment calls were predominantly placed before the COVID-19 pandemic, from May 2019 to February 2020. Only four initial calls were placed during the pandemic from June 2020 to July 2020. Due to the pandemic, there was a gap of four months as pharmacy students could not rotate at the MAP, and the intervention calls were not allowed to be placed outside the MAP due to confidentiality reasons. The first date of the intervention call was the study start date. During the initial call, students obtained informed consent from the patients and asked if they were interested in receiving the intervention. Additionally, the pharmacy students confirmed the diagnosis, the current list of medications, and the refill information. Furthermore, patients were also screened for depression using the Patient Health Questionnaire (PHQ-2)—a validated screening tool for depression [38]. Patients identified with depression were requested to schedule an appointment with a healthcare provider to address the issue. MI consistent intervention was provided in English. The MI scripts were adapted from an original script drafted by the MI-trained team of researchers and tailored to the different adherence trajectories determined from the retrospective phase of the study [33]. Since MI is a patient-centered approach, the scripts were used as a guide for students through the phone interview process. Students were trained to ask open-ended questions and were encouraged to allow participants to make choices and feel responsible for their decision making. The length of the calls was based on the patient’s need, and an initial call lasted for approximately 15 minutes, while the follow-up calls lasted for approximately 7 minutes. During the follow-up calls, students confirmed if the problem was resolved and provided patient education and positive reinforcement to improve adherence. In some instances, students also contacted the participant’s clinician or pharmacist to resolve any concerns raised by the participant. After each call, students documented the barriers and any concerns that were discussed. To ensure intervention fidelity, 20% of student phone calls were monitored for quality control and adherence to MI. The control group received the usual care from the pharmacist, which is the regular refill reminder calls. All the documents collected were deidentified and entered into an Excel sheet for further analysis. The intervention, scripts used for the MI intervention, and data collection were approved by the University of Houston Institutional Review Board.
2.6 Outcome Measures
The primary outcome was the adherence to ACEI/ARB during the 6 and 12 months post-MI implementation. Patients who were continuously enrolled for 1-year post-MI implementation were included. Adherence was calculated from the date of the initial call as it was hypothesized that the effect of intervention will start immediately after an intervention. PDC was used to calculate the adherence to ACEI/ARB, and it represents the total number of medications patients have on hand divided by the entire study period. Patients with a PDC of ≥ 0.80 were considered adherent. Use of the MPR was also considered for the outcome measurement, however, PDC is generally preferred as it is more operationally defined and provides conservative estimates in case of switching and concomitant therapy with multiple drugs within a class [39]. For the intervention group, an index date was defined as the initial intervention call date. An index day was assigned for the corresponding controls, which was the first day of the same month of the initial intervention to ensure the same length of follow-up between the controls and intervention. If patients had switched from an ACEI to an ARB or vice versa, then the days’ supply for both the medications would be summed.
The secondary outcome was discontinuation, defined as no refills for ACEI/ARB during 6 and 12 months after the initial MI implementation call.
2.7 Predictor Variables
All the predictor variables were identified during the previous phase 1 retrospective study. Sex, age (< 70 years versus ≥ 70 years), health plan (low-income subsidy versus no low-income subsidy), prescriber specialty (primary care physician versus specialty), refill type (<90 days versus ≥ 90 days), presence of comorbidities like myocardial infarction, end-stage renal disease, depression, congestive heart failure, stroke, and coronary artery disease, number of concomitant medications (≤ 2 versus >2), regimen complexity, prevalent users (prevalent versus incident users), prior hospitalizations (none versus ≥ 1), and CMS risk score. Regimen complexity was defined as the mean doses taken per day multiplied by total number of daily medications. Prevalent users were defined as patients who were prescribed ACEIs/ARBs within 6 months prior to the study. The CMS risk score accounted for medication burden and disease severity, and was calculated based on data taken from a large group of beneficiaries to estimate the average predicted costs for each of the components factors (e.g., age, sex, low-income status, individual disease groups). It consists of 189 disease classifications for use in risk adjusting of clinical outcomes in Medicare populations. The detailed definitions of other covariates are published elsewhere [30].
2.8 Statistical Analysis
The baseline characteristics were compared between the intervention and control group using chi-square tests for categorical variables and t-tests for the continuous variables. A multivariable logistic regression model with PDC as a categorical outcome (PDC ≥ 0.80 versus PDC < 0.80) was used to evaluate the effect of intervention on adherence at 6 and 12 months following the intervention initiation. A multiple linear regression modeled PDC as a continuous outcome (ranging from 0 to 1) for 6 and 12 months following the intervention. Finally, a logistic regression model was performed to assess the association between intervention and ACEI/ARB discontinuation during 6- and 12-months post-MI initiation. The major independent variable for all the models were intervention versus control group. Baseline adherence trajectories were controlled in all the models.
2.9 Sensitivity Analysis
Additional analysis was performed by including number of follow-up calls as the primary independent variable. Multiple logistic and linear regression models were performed to evaluate the impact of the number of follow-up calls on adherence. Separate logistic regression model was conducted to examine the impact of number of follow-up calls on discontinuation. All the statistical analysis was conducted using SAS 9.4 at a priori significance of 0.05.
3 Results
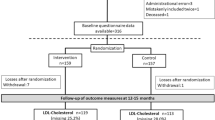
A total of 22,774 patients with comorbid diabetes and hypertension were identified. Among them, 7868 non-adherent ACEI/ARB patients were randomized to the intervention and control group. Of these, patients were randomized in a 3:1 ratio, resulting in 5901 patients in the intervention group and 1967 patients in the control group. Figure 3 describes the cohort formation flowchart. Of the 5901patients randomized to the intervention group, 2091 patients were outreached. A total of 247 patients agreed to participate in this study. Of them, seven patients were excluded as they were not continuously enrolled. The final intervention cohort was composed of 240 patients, of which 102 were in the ‘gaps in adherence’ trajectory group, 94 were in the ‘gradual decline’ trajectory group, and 44 patients were in the ‘rapid decline’ trajectory group. The number of patients who successfully completed each of the follow-up calls is as follows: 176 (73.33%) completed the second call, 108 (45%) completed the third call, 70 (29.16%) completed the fourth call, 41 (17.08%) completed the fifth call, and 31 (12.91%) completed the sixth call.
Of the 1967 patients randomized to the control group, 698 patients were excluded due to disenrollment. Of the remaining 1269 patients, 480 patients were randomly selected for the control group. All the baseline characteristics for 720 patients (240 interventions and 480 controls) are presented in Table 1. Significant differences across congestive heart failure, coronary heart disease, prevalent users, and CMS risk scores were observed between the intervention and control groups.
3.1 Results of the Regression Models at 6 Months
At 6 months, the logistic regression model reported that the MI intervention did not have a significant impact on the adherence to ACEI/ARB (Table 2). Patients associated with the ‘gaps in adherence’ trajectories (odds ratio [OR]: 2.61, 95% confidence interval [CI]: 1.69–4.04) or gradual decline in adherence (OR: 1.65, 95% CI 1.06–2.55) were significantly more likely to become adherent as compared with the patients in the ‘rapid decline’ trajectory (regardless of receiving the intervention or not). Prevalent users were more likely to be adherent compared with incident users (OR: 1.93, 95% CI 1.21–3.09).
The linear regression model determined that MI intervention was significantly associated with better adherence (β = 0.06; p = 0.03). Patients falling into the previous adherence trajectories like gaps in adherence (β = 0.25; p < 0.0001) or gradual decline in adherence (β = 0.16; p < 0.0001) were positively associated with improved adherence. Patients with congestive heart failure were positively associated with better adherence (β = 0.11; p = 0.04). Patients who had one or more previous hospitalizations were less likely to be adherent (β = − 0.11; p = 0.01). Finally, prevalent users were more likely to be associated with better adherence (β = 0.09; p = 0.01).
Furthermore, compared with the controls, patients receiving the intervention had less ACEI/ARB discontinuation over 6 months following the intervention initiation, and this was marginally significant (OR: 0.64; 95% CI 0.41–1.00). Baseline adherence trajectories like gaps in adherence (OR: 0.14; 95% CI 0.08–0.24) or gradual decline in adherence (OR: 0.34; 95% CI 0.21–0.54) were less likely to be associated with discontinuation of ACEIs/ARBs. Patients with congestive heart failure were less likely to discontinue (OR: 0.23, 95% CI 0.08–0.64). Patients who had one or more hospitalizations were more likely to discontinue ACEI/ARB (OR: 2.56; 95% CI 1.33–4.94) (Table 3).
3.2 Results of the Regression Models at 12 Months
Within 12 months of intervention implementation, patients who received the intervention had significantly better adherence to ACEIs/ARBs than controls (OR: 1.46; 95% CI 1.05–2.04) (Table 4). Patients who were in the ‘gaps in adherence’ trajectory (OR: 2.65; 95% CI 1.69–4.18) or ‘gradual decline’ trajectory (OR: 2.19; 95% CI 1.38–3.46) at baseline were more likely to be adherent than the patients in the ‘rapid decline’ trajectory. Prevalent users were more likely to be adherent than incident users (OR: 1.69; 95% CI 1.05–2.72).
The intervention group was more likely to be adherent at 1 year after the intervention compared with the control group (β = 0.06; p = 0.02). Similar to the regression model, baseline adherence trajectories (gaps in adherence: β = 0.24; p < 0.0001; gradual decline in adherence: β = 0.15; p < 0.0001) and prevalent users (β = 0.09; p = 0.006) were positively associated with better adherence after intervention. Finally, patients with prior hospitalizations were less likely to be adherent after the intervention (β = − 0.12; p = 0.01).
At 12 months, MI intervention did not have any significant impact on the discontinuation of ACEI/ARB (see electronic supplementary material [ESM]). Patients with depression, coronary artery disease, and previous hospitalization were more likely to discontinue ACEI/ARB. Patients grouped in the ‘gaps in adherence’ trajectory, ‘gradual decline’ trajectory, congestive heart disease, and prevalent users were less likely to be associated with discontinuation.
3.3 Sensitivity Analysis
3.3.1 Results of the Regression Models at 6 Months
Results of logistic regression for adherence showed that patients receiving three or more follow-up calls were more likely to be adherent (OR: 2.11; 95% CI 1.23–3.61) (see ESM). The linear regression model showed that patients receiving two or more follow-up calls were positively associated with better adherence (β = 0.08; p = 0.02). The logistic regression model for discontinuation at 6 months reported that patients receiving three or more follow-up calls were less likely to discontinue (OR: 0.41; 95% CI 0.17–0.97).
3.3.2 Results of the Regression Models at 12 Months
At 12 months post-MI implementation, patients who received two or more follow-up calls were more likely to be adherent (OR: 1.60; 95% CI 1.03–2.49). The same trend was preserved in the linear regression model (β = 0.08; p = 0.02). Finally, for the discontinuation outcome, no significant association between the number of calls and discontinuation was observed.
4 Discussion
The result of this prospective study concludes that a brief MI intervention implemented by pharmacy students among nonadherent ACEI/ARB patients has improved adherence at 1-year post-intervention. These results are consistent with the previous study that documented improved statin adherence among nonadherent patients by implementing MI intervention tailored to prior statin adherence [29]. In this current study, the beneficial effects of MI intervention on adherence were preserved even after having a 3- to 4-month gap in placing the intervention calls due to COVID-19. Discontinuation rates after 6 months post-MI intervention were lower, and this trend was marginally significant.
As of 2021, there were 48 million Medicare Part D beneficiaries [40], and > 70% of antihypertensive users are prescribed an ACEI/ARB [41,42,43]. Due to the reno-protective effect of ACEIs/ARBs, they are recommended as the first-line medication among elderly patients with comorbid diabetes and hypertension [44, 45]. Even after implementing the Centers for Medicare & Medicaid Services (CMS) Star Rating for medication adherence to ACEIs/ARBs, adherence among MAP beneficiaries is still suboptimal and remains an unmet challenge for various stakeholders [30, 46]. Adherence to ACEI/ARB is one of the quality measures in the CMS Star Rating program, which is used to evaluate health plan performance and is linked to reimbursement [47]. According to the Congressional Budget Office, among Medicare (the government health insurance program for individuals 65 years or older) beneficiaries, as the prescription refills increase by 1%, the medical costs fall by 0.2% [48]. Among Medicare patients with hypertension, a 1% increase in drug utilization results in the reduction of medical costs (excluding pharmacy costs) by 1.17% [49]. In addition, increasing adherence to ACEI/ARB among Medicare beneficiaries has resulted in potential cost savings associated with Medicare Part A and Part B services resulting in lower annual expenditures [50]. Medicare beneficiaries adherent to ACEI/ARB had lower healthcare resource utilization than nonadherent patients [41]. Hence, our study adds critical knowledge to the growing body of evidence that a customized intervention tailored to past adherence trajectories can improve adherence. Furthermore, the intervention was implemented by MI-trained pharmacy students at no additional cost. Fourth-year pharmacy students have the expertise and knowledge to improve medication adherence. Trained pharmacy students under the supervision of pharmacy preceptors or residents have demonstrated potential in effectively addressing barriers to medication adherence among patients with chronic illness [31, 51,52,53]. With the rising physician shortage and healthcare expenditures [52, 54], utilizing trained pharmacy students for disease management is worthwhile [29, 52].
After 1 year post-MI implementation, the intervention improved adherence among nonadherent hypertensive patients with diabetes. This may be due to the following reasons:
-
(1)
The intervention was tailored based on the predictors associated with lower adherence trajectories which were identified in phase I of the study. The major predictors associated with falling into the lower adherence trajectories were being male, refill type, age, having no low-income subsidy, end-stage renal disease, depression, stroke, myocardial infarction, coronary artery disease, number of concomitant medications, prior hospitalizations, and CMS risk score [30]. These predictors were incorporated while developing the scripts for MI intervention.
-
(2)
Incorporation of customized patient education and individualized self-management activities. Forgetfulness was one of the major barriers that was reported. MI-trained pharmacy students offered potential solutions to improve medication-taking behavior. These included using a pill box, keeping reminders for taking medications, and taking all medications at the same time [31, 55]. In this study, side effects and regimen complexity were other barriers of adherence [31]. Pill burden among patients with multimorbidity is a potential reason for suboptimal adherence [30]. Student pharmacists have also played a critical role in collaborating with other healthcare providers to address issues like increased costs, side effects, and regimen complexity [56]. Pharmacists educated the intervention group regarding the long-term consequences of nonadherence to antihypertensive medications. Tailored education consistent with adherence patterns in combination with MI have improved adherence.
-
(3)
MI intervention may have improved patient motivation, self-efficacy, and hence promoted a favorable and sustainable behavior change. Prior studies have documented that for interventions to be more effective, patients should be given autonomy to make decisions and they should be encouraged to be involved during decision making [31]. Pharmacists also played a significant role in positive reinforcement and thus patients felt empowered to follow the medication orders given by physicians [57].
-
(4)
With better patient–pharmacist interactions, patients may have felt motivated to improve their adherence [55]. Pharmacists were trained to provide nonjudgmental reflection to foster adherence. Positive relationships with healthcare providers can have a significant impact on adherence, especially among older adults [55]. Since patients interact with their pharmacists more often than with clinicians, pharmacists can educate and give appropriate counseling. These counseling strategies help to maximize patients’ engagement and reduce their resistance regarding denial of suboptimal adherence [55]. Furthermore, these strategies guided them to change their attitudes and beliefs leading to a ‘goal setting’ mentality to improve adherence [55].
-
(5)
The number of follow-up calls and length of intervention may have helped to improve patients’ perspectives towards adherence. This is consistent with the existing literature that more follow-up calls can help to sustain the behavior change. MI intervention with a higher number of calls was more likely to be effective compared with just one call [32, 58]. Another prospective study also reported that patients who received two or more calls were more likely to be adherent than those who received fewer than two calls [32]. Furthermore, the discontinuation rate was also significantly lower among the patients who received two or more follow-up calls [32]. Similarly, in this study patients who received two or more follow-up calls were more likely to be adherent.
Patients falling into the ‘gaps in adherence’ trajectory and ‘gradual decline’ trajectory were more likely to be adherent and less likely to discontinue ACEI/ARB at 6- and 12-months post-MI implementation than patients falling in the ‘rapid decline’ trajectory. This is consistent with a prior prospective study that documented patients associated with a ‘rapid decline’ trajectory were less likely to be adherent and more likely to discontinue statins 6 months after a tailored MI intervention [29]. The mean PDC for the ‘rapid decline’ trajectory was lower than other adherence trajectories. This indicates that adherence barriers associated with a ‘rapid decline’ trajectory may not have been fully addressed even after incorporating customized interventions, or more frequent calls may be warranted for this group of patients to better connect with the patient. Future studies should evaluate the potential reasons for the rapidly declining adherence pattern.
Prevalent users were more likely to be adherent and less likely to discontinue than incident users. The suboptimal adherence among incident users could be explained by the patient’s beliefs that antihypertensive medication is not needed due to the lack of symptoms. Furthermore, it could also be due to the fear of side effects and lack of awareness regarding the potential future benefits of antihypertensive medications [59, 60]. Patients with a history of hospitalization were associated with nonadherence and discontinuation, which is in line with prior literature [61, 62]. Patients with congestive heart failure were more likely to be adherent and less likely to discontinue, which is in concordance with published literature [63].
4.1 Limitations
In this study, medications refilled outside the health plan or by paying cash could not be captured. In addition, various sociodemographic factors like race, education, health literacy, and income level were not available. This study could not verify the reason for discontinuation of ACEI/ARB. Since the intervention was in English, Spanish-speaking patients could not be included in the study. Finally, while the initial plan for the intervention was to have monthly follow-up calls, due to the COVID-19 pandemic there were gaps in the intervention, which could have affected the results; other COVID-19-related factors such as the increased isolation and depression that accompanied the pandemic may have impacted the intervention’s effectiveness. It is also worth noting that despite the previous interventions conducted by the health plan for improving ACEI/ARB adherence (as a CMS Star measure), patients included in this study were still nonadherent; this may reflect the level of resistance and how it could impact effectiveness of such interventions among this population. Such interventions by the health plan were not controlled for in this study but were implemented among both controls and intervention patients.
5 Conclusion
The findings of this study demonstrate that despite the gaps in the intervention and the unprecedented COVID-19 situation, the customized MI intervention based on prior adherence trajectories improved adherence to ACEIs/ARBs among patients with comorbid hypertension and diabetes at 1 year. This reveals that a brief telephonic MI intervention may be effective in improving adherence and more research is needed to evaluate sustained behavior change over a longer period of time. Future studies should also develop interventions in other languages such as Spanish so as to improve adherence among racial and ethnic minorities.
References
Promotion NCfCDPaH. Heart Disease and Stroke. 2022 [cited; Available from: https://www.cdc.gov/chronicdisease/resources/publications/factsheets/heart-disease-stroke.htm#:~:text=Leading%20risk%20factors%20for%20heart,unhealthy%20diet%2C%20and%20physical%20inactivity. Accessed July 2022.
(CDC) CfDCaP. Hypertension Cascade: Hypertension Prevalence, Treatment and Control Estimates Among US Adults Aged 18 Years and Older Applying the Criteria From the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2015–2018. 2021.
McLean DL, Simpson SH, McAlister FA, Tsuyuki RT. Treatment and blood pressure control in 47,964 people with diabetes and hypertension: a systematic review of observational studies. Can J Cardiol. 2006;22(10):855–60.
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313(6):603–15.
Deedwania PC. Diabetes and hypertension, the deadly duet: importance, therapeutic strategy, and selection of drug therapy. Cardiol Clin. 2005;23(2):139–52.
Lopez-Jaramillo P, Lopez-Lopez J, Lopez-Lopez C, Rodriguez-Alvarez MI. The goal of blood pressure in the hypertensive patient with diabetes is defined: now the challenge is go from recommendations to practice. Diabetol Metab Syndr. 2014;6(1):1–10.
Investigators HOPES. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. The Lancet. 2000;355(9200):253–9.
Yusuf S, Sleight P, Pogue Jf, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342(3):145–53.
Cooke CE, Fatodu H. Physician conformity and patient adherence to ACE inhibitors and ARBs in patients with diabetes, with and without renal disease and hypertension, in a medicaid managed care organization. J Manag Care Pharm. 2006;12(8):649–55.
Adler AI, Stratton IM, Neil HAW, Yudkin JS, Matthews DR, Cull CA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321(7258):412–9.
Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford N, Schrier RW. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl J Med. 1998;338(10):645–52.
Investigators O. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358(15):1547–59.
Sabaté E, Sabaté E. Adherence to long-term therapies: evidence for action. World Health Organization; 2003.
Kronish IM, Thorpe CT, Voils CI. Measuring the multiple domains of medication nonadherence: findings from a Delphi survey of adherence experts. Transl Behav Med. 2021;11(1):104–13.
Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705.
Kettani F-Z, Dragomir A, Côté R, Roy L, Bérard A, Blais L, et al. Impact of a better adherence to antihypertensive agents on cerebrovascular disease for primary prevention. Stroke. 2009;40(1):213–20.
Degli Esposti L, Saragoni S, Benemei S, Batacchi P, Geppetti P, Di Bari M, et al. Adherence to antihypertensive medications and health outcomes among newly treated hypertensive patients. ClinicoEconomics Outcomes Res CEOR. 2011;3:47–54.
Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;2014(11):CD000011. https://doi.org/10.1002/14651858.CD000011.pub4.
Armstrong M, Mottershead T, Ronksley P, Sigal R, Campbell T, Hemmelgarn B. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2011;12(9):709–23.
Miller WR, Rollnick S. Motivational interviewing: Helping people change. Guilford Press; 2012.
Turner AP, Sloan AP, Kivlahan DR, Haselkorn JK. Telephone counseling and home telehealth monitoring to improve medication adherence: results of a pilot trial among individuals with multiple sclerosis. Rehabil Psychol. 2014;59(2):136.
Papus M, Dima AL, Viprey M, Schott A-M, Schneider MP, Novais T. Motivational interviewing to support medication adherence in adults with chronic conditions: systematic review of randomized controlled trials. Patient Educ Couns. 2022;105:3186–203.
Franklin JM, Shrank WH, Pakes J, Sanfélix-Gimeno G, Matlin OS, Brennan TA, et al. Group-based trajectory models: a new approach to classifying and predicting long-term medication adherence. Med care. 2013;51:789–96.
Franklin JM, Krumme AA, Tong AY, Shrank WH, Matlin OS, Brennan TA, et al. Association between trajectories of statin adherence and subsequent cardiovascular events. Pharmacoepidemiol Drug Saf. 2015;24(10):1105–13.
Vadhariya A, Fleming ML, Johnson ML, Essien EJ, Serna O, Esse T, et al. Group-based trajectory models to identify sociodemographic and clinical predictors of adherence patterns to statin therapy among older adults. Ame Health Drug Benefits. 2019;12(4):202.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6(1):109–38.
Franklin JM, Krumme AA, Shrank WH, Matlin OS, Brennan TA, Choudhry NK. Predicting adherence trajectory using initial patterns of medication filling. Am J Manag Care. 2015;21(9):e537–44.
Lo-Ciganic W-H, Donohue JM, Jones BL, Perera S, Thorpe JM, Thorpe CT, et al. Trajectories of diabetes medication adherence and hospitalization risk: a retrospective cohort study in a large state Medicaid program. J Gen Intern Med. 2016;31(9):1052–60.
Abughosh SM, Vadhariya A, Johnson ML, Essien EJ, Esse TW, Serna O, et al. Enhancing statin adherence using a motivational interviewing intervention and past adherence trajectories in patients with suboptimal adherence. J Manag Care Spec Pharm. 2019;25(10):1053–62.
Paranjpe R, Johnson ML, Essien EJ, Barner JC, Serna O, Gallardo E, et al. Group-based trajectory modeling to identify patterns of adherence and its predictors among older adults on Angiotensin-Converting Enzyme Inhibitors (ACEIs)/Angiotensin Receptor Blockers (ARBs). Patient Prefer Adherence. 2020;14:1935–47.
Abughosh SM, Wang X, Serna O, Henges C, Masilamani S, Essien EJ, et al. A Pharmacist telephone intervention to identify adherence barriers and improve adherence among nonadherent patients with comorbid hypertension and diabetes in a medicare advantage plan. J Manag Care Spec Pharm. 2016;22(1):63–73.
Abughosh S, Wang X, Serna O, Esse T, Mann A, Masilamani S, et al. A motivational interviewing intervention by pharmacy students to improve medication adherence. J Manag Care Spec Pharm. 2017;23(5):549–60.
Abughosh SM, Wang X, Serna O, Henges C, Masilamani S, James Essien E, et al. A pharmacist telephone intervention to identify adherence barriers and improve adherence among nonadherent patients with comorbid hypertension and diabetes in a medicare advantage plan. J Manag Care Spec Pharm. 2016;22(1):63–73.
van Der Wal MH, Jaarsma T, Moser DK, Veeger NJ, van Gilst WH, van Veldhuisen DJ. Compliance in heart failure patients: the importance of knowledge and beliefs. Eur Heart J. 2006;27(4):434–40.
van der Wal MH, Jaarsma T. Adherence in heart failure in the elderly: problem and possible solutions. Int J Cardiol. 2008;125(2):203–8.
Bohachick P, Burke LE, Sereika S, Murali S, Dunbar-Jacob J. Adherence to angiotensin-converting enzyme inhibitor therapy for heart failure. Prog Cardiovasc Nurs. 2002;17(4):160–6.
Koh-Knox CP. Motivational interviewing in health care: helping patients change behavior. Am J Pharm Educ. 2009;73(7):127.
Maurer DM. Screening for depression. Am Fam Physician. 2012;85(2):139–44.
Nau DP. Proportion of days covered (PDC) as a preferred method of measuring medication adherence, vol. 6. Springfield: Pharmacy Quality Alliance; 2012. p. 25.
Cubanski J, Damico A. Key facts about Medicare Part D enrollment, premiums, and cost sharing in 2021. Kaiser Family Foundation. 2021. https://www.kff.org/medicare/issue-brief/key-facts-about-medicare-part-d-enrollment-premiums-and-cost-sharing-in-2021. Accessed July 2022.
Campbell PJ, Axon DR, Taylor AM, Smith K, Pickering M, Black H, et al. Hypertension, cholesterol and diabetes medication adherence, health care utilization and expenditure in a Medicare Supplemental sample. Medicine (Baltimore). 2021;100(35): e27143.
Mohan A, Vadhariya A, Majd Z, Esse TW, Serna O, Abughosh SM. Impact of a motivational interviewing intervention targeting statins on adherence to concurrent hypertension or diabetes medications. Patient Educ Couns. 2021;104(7):1756–64.
Jackson SLNP, Chang A, Schieb L, et al. Antihypertensive and statin medication adherence among medicare beneficiaries. Am J Prev Med. 2022;63:313–23.
American DA. Standards of medical care in diabetes–2013. Diabetes Care. 2013;36(Suppl 1):S11-66.
Hou FF, Zhang X, Zhang GH, Xie D, Chen PY, Zhang WR, et al. Efficacy and safety of benazepril for advanced chronic renal insufficiency. N Engl J Med. 2006;354(2):131–40.
Majd Z, Mohan A, Paranjpe R, Abughosh SM. Identifying adherent patients to newly initiated statins using previous adherence to chronic medications. J Manag Care Spec Pharm. 2021;27(2):186–97.
Owen JA. Medicare star ratings: Stakeholder proceedings on community pharmacy and managed care partnerships in quality: American Pharmacists Association and Academy of Managed Care Pharmacy. J Am Pharm Assoc. 2014;54(3):228–40.
Lloyd JT, Maresh S, Powers CA, Shrank WH, Alley DE. How much does medication nonadherence cost the medicare fee-for-service program? Med Care. 2019;57(3):218–24.
Roebuck MC. Medical cost offsets from prescription drug utilization among Medicare beneficiaries. J Manag Care Spec Pharm. 2014;20(10):994–5.
Lopert R, Shoemaker JS, Davidoff A, Shaffer T, Abdulhalim AM, Lloyd J, et al. Medication adherence and Medicare expenditure among beneficiaries with heart failure. Am J Manag Care. 2012;18(9):556–63.
Wheat L, Roane TE, Connelly A, Zeigler M, Wallace J, Kim JH, et al. Using a pharmacist-community health worker collaboration to address medication adherence barriers. J Am Pharm Assoc (2003). 2020;60(6):1009–14.
Stanton-Robinson C, Al-Jumaili AA, Jackson A, Catney C, Veach S, Witry MJ. Evaluation of community pharmacist-provided telephone interventions to improve adherence to hypertension and diabetes medications. J Am Pharm Assoc (2003). 2018;58(4S):S20–4.
Ray S, Lokken J, Whyte C, Baumann A, Oldani M. The impact of a pharmacist-driven, collaborative practice on diabetes management in an Urban underserved population: a mixed method assessment. J Interprof Care. 2020;34(1):27–35.
Heiser S. AAMC report reinforces mounting physician shortage. Association of American Medical Colleges. https://www. aamc. org/news-insights/press-releases/aamc-reportreinforces-mounting-physician-shortage. 2021. Accessed July 2022.
Holt EW, Rung AL, Leon KA, Firestein C, Krousel-Wood MA. Medication adherence in older adults: a qualitative study. Educ Gerontol. 2014;40(3):198–211.
Presley B, Groot W, Pavlova M. Pharmacy-led interventions to improve medication adherence among adults with diabetes: A systematic review and meta-analysis. Res Social Adm Pharm. 2019;15(9):1057–67.
Albrecht S. The pharmacist’s role in medication adherence. US Pharm. 2011;36(5):45–8.
Menon U, Belue R, Wahab S, Rugen K, Kinney AY, Maramaldi P, et al. A randomized trial comparing the effect of two phone-based interventions on colorectal cancer screening adherence. Ann Behav Med. 2011;42(3):294–303.
Kurdi AI, Chen LC, Elliott RA. Exploring factors associated with patients’ adherence to antihypertensive drugs among people with primary hypertension in the United Kingdom. J Hypertens. 2017;35(9):1881–90.
Michel B, Brent ME. Adherence in hypertension. Circ Res. 2019;124(7):1124–40.
Shin S, Song H, Oh SK, Choi KE, Kim H, Jang S. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertens Res. 2013;36(11):1000–5.
Marcum ZA, Zheng Y, Perera S, Strotmeyer E, Newman AB, Simonsick EM, et al. Prevalence and correlates of self-reported medication non-adherence among older adults with coronary heart disease, diabetes mellitus, and/or hypertension. Res Social Adm Pharm. 2013;9(6):817–27.
Saadat Z, Nikdoust F, Aerab-Sheibani H, Bahremand M, Shobeiri E, Saadat H, et al. Adherence to antihypertensives in patients with comorbid condition. Nephrourol Mon. 2015;7(4): e29863.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the National Heart, Lung, and Blood Institute (NHLBI), 1R15HL135700-01A1.
Conflict of Interest
SA reports grants from CARsgen and Valeant Pharmaceuticals, outside the submitted work. JB reports personal fees from University of Houston during the conduct of the study and a grant from Centers for Disease Control, Texas Health and Human Services, and Pharmaceutical Research Manufacturers of America Foundation, outside the submitted work. MF reports grants from National Heart, Lung, and Blood Institute and National Institute on Minority Health and Health Disparities (U-54). MF also reports contracts from Texas Health and Human Services Commission and CoI funding on a grant from Texas Council for Developmental Disabilities, outside the submitted work. EG is an employee of CareAllies, a subsidiary of Cigna, outside of the submitted work. The other authors declare that they have no conflict of interest.
Availability of Data and Material
Not available.
Ethics Approval
The study was approved by the institutional review board at the University of Houston and is compliant with the Declaration of Helsinki.
Consent to Participate
Participants receiving the intervention consented verbally over the initial phone call to participation using a script in accordance with all NIH human subject ethical guidelines and the University of Houston IRB requirements for recruitment and informed consent.
Code Availability
Not available.
Authors’ Contributions
Design/conduct of the study (SA, MF, MH); acquisition of subjects and/or data (SA, EG, NO, OS); analysis and interpretation of data (AM, ZM, SA, MJ, JB, EE, MH); preparation of manuscript (AM, ZM, SA). All authors contributed to the review and editing and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mohan, A., Majd, Z., Johnson, M.L. et al. A Motivational Interviewing Intervention to Improve Adherence to ACEIs/ARBs among Nonadherent Older Adults with Comorbid Hypertension and Diabetes. Drugs Aging 40, 377–390 (2023). https://doi.org/10.1007/s40266-023-01008-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-023-01008-6