Abstract
Perimenopause marks the transition from a woman’s reproductive stage to menopause. Usually occurring between 42 and 52 years of age, it is determined clinically by the onset of irregular menstrual cycles or variable cycle lengths. Women are at an increased risk of depression and anxiety during perimenopause and the menopausal transition. Depressive symptoms experienced in perimenopause are often more severe compared to pre- and post-menopause. During menopausal transition, the impact of fluctuating estrogen in the central nervous system (CNS) can have negative psychological effects for some women. Traditional first-line management of menopausal depression involves antidepressants, with modest outcomes. The positive effects of estrogen treatment in the CNS are becoming increasingly recognised, and hormonal therapy (HT) with estrogen may have a role in the treatment of menopausal depression. In this review we will outline the prevalence, impact and neurochemical basis of menopausal-associated depression, as well as hormone-based approaches that have increasing promise as effective treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Women are at an increased risk for depression and anxiety during perimenopause and the menopausal transition. |
During menopausal transition, the impact of fluctuating estrogen in the central nervous system (CNS) can cause depression and anxiety in some women. |
Traditional first-line management of menopausal depression involves antidepressants, with modest or poor outcomes. |
The positive effects of estrogen treatment in the CNS are becoming increasingly recognized, and hormonal therapy (HT) with estrogen may have a role in the treatment of menopausal depression. |
1 Introduction
Perimenopause marks the transition from a woman’s reproductive stage to menopause. Usually occurring between 42 and 52 years of age, perimenopause is determined clinically by the onset of irregular menstrual cycles or variable cycle lengths [1]. According to the Stages of Reproductive Age Workshop (STRAW) [2], cycle lengths must differ by at least 7 days, and after a woman has had 1 year without a menstrual period, she has completed the transition into menopause. In addition to numerous somatic symptoms, one in three women will experience significant psychological changes during the transition into menopause [3]. Previous studies have demonstrated that women are not only at an increased risk of depression and anxiety during perimenopause and the menopausal transition (MT) [4,5,6], but also that depressive symptoms experienced in perimenopause are of higher severity compared with pre- and postmenopause [7, 8]. We note of course that many women have no mental health issues related to menopause transition.
However, depression associated with menopause is becoming increasingly more recognized. Although sparse, human studies have shown that estrogen is involved in the modulation of neurocircuitry contributing to the development of depression, including at the serotonergic, noradrenergic, and dopaminergic systems [9, 10]. Estrogen’s neuroprotective effects have been shown in neurodegenerative diseases, where it may be protective against Alzheimer’s disease (AD) and Parkinson’s disease [11, 12]. It makes sense therefore that during menopause, with fluctuating and decreasing estrogen levels in the central nervous system (CNS), that a subsequent diminution of estrogenic neuroprotective effects could have negative psychological effects on some women. Furthermore, reproductive ageing involves physical changes, loss of certain bodily functions, and changes to feelings of femininity [13]. Compounding this are symptoms of menopause that can significantly impact a woman’s quality of life. In adjusted analysis of health-related quality of life, the Study of Women’s Health Across the Nation showed that menopausal symptoms, and not menopause itself, had a significant negative impact on the overall emotional functioning of women in the perimenopausal period [14]. Adequate control of depressive disorders and symptoms throughout the MT is therefore of utmost importance. Traditional first-line management of menopausal depression involves antidepressants, but the positive effects of estrogen on the CNS are becoming increasingly recognized, and hormonal therapy (HT) with estrogen may have a role in the treatment of depression associated with menopause.
In this review, we outline the prevalence, impact and neurochemical basis of menopausal-associated depression, as well as provide emerging evidence for the consideration of hormone-based treatments, particularly for women with severe, persistent depression related to menopause that has not responded to treatment with antidepressant medications.
2 Epidemiology
The most recent Australian data on mental health showed that women experience higher rates of mental illness than men, with twice as many women than men developing major depressive disorders [15]. Gender is clearly implicated in the type and degree of mental illness, with the detrimental outcome of suicide alarmingly increasing for women over the past decade [16]. Genetics, previous mental health disorders, stressful life events and sexual violence are also believed to be involved in the increasing rate of female depression [16,17,18]. In particular, the repeated endocrinological changes occurring in women around puberty, partum, post-partum and menopause could be the reason that the higher risk of depression for women than men persists from puberty through to old age [17, 19]. Interestingly, there may even be a female-specific reproductive phenotype for depression that makes certain women more susceptible to hormonal fluctuations during reproductive events [17]. The MT is independently associated with a high risk of developing depressive symptoms. Multiple studies have shown that women, even without a previous history of depression, are more likely to develop symptoms during the perimenopause compared with other periods of their life [3, 10, 20].
3 Neurobiological Changes in Menopause
Estrogen is a cholesterol-derived sex steroid with three subtypes: estrone ‘E1’ is the main subtype present in menopausal women; estradiol ‘E2’ is the most potent subtype and is highly abundant in premenopausal women; and estriol ‘E3’, is the weakest of the three subtypes, secreted by the placenta during pregnancy [11]. As a metabolic steroid, estrogen production occurs via adrenal, ovarian, adipose, testicular, and placental pathways. In females, it is secreted cyclically at menstruation and exerts negative feedback modulation on the hypothalamic-pituitary-ovarian (HPO) axis. The HPO axis governs ovarian cyclicity and comprises the hypothalamus, pituitary gland, hypothalamic gonadotropin-releasing hormone (GnRH) neurons, and the female gonadal structures. During the luteal phase of the menstrual cycle, pituitary gonadotropes respond to pulsatile release of GnRH by secreting the gonadotropins follicle-stimulating hormone (FSH) and luteinizing hormone (LH) [21,22,23]. The gonadotropins stimulate ovarian folliculogenesis, as well as steroid and inhibin production [22, 23]. As levels of estrogen and inhibin B rise during the luteal phase of the cycle, the steroid and peptide dually suppress hypothalamic and gonadotropic neurons, coordinating a highly organized negative feedback loop [21, 24].
Estrogen has two signalling pathways. The classical pathway involves the nuclear receptors ER-α and ER-β, to which estrogen binding triggers changes in gene transcription [11, 25]. The non-classical pathway involves the G-protein-coupled-receptor GPER1, to which estrogen binding triggers the cyclic adenosine monophosphate/mitogen-activated protein kinase (c-AMP/MAPK) signalling pathway moderated by protein kinases [26]. All three receptors are differentially expressed in tissues throughout the body, with ER-β being the predominant receptor in the CNS [11, 25]. Estrogen’s hormonal influence contributes to biological changes underlining menopausal symptoms [27, 28]. Physiologically, the menopausal transition involves fluctuating levels of gonadal steroids in ovarian and uterine tissue and in the CNS via the HPO axis [29]. Ovarian senescence causes hypoestrogenism that induces a climacteric state with insomnia, bleeding irregularity, urogenital atrophy, breast aches, sexual dysfunction and vasomotor changes [30, 31]. Changes in mood, cognition and memory have also been associated with the onset of menopause [32, 33].
Estrogen fluctuations and related shifts in the neurochemicals it modulates have been implicated in the aetiology of menopausal depression, despite views that menopausal depression may merely be caused by the unpleasant experience of vasomotor symptoms (VMS) [27, 28]. The matter is made even more complex by the fact that certain symptoms of depression, such as changes in concentration and fatigue, are also independently associated with menopause [32]. However, the physiological process of VMS and the aetiology of menopausal depression are likely independent hormonal interplays.
3.1 Vasomotor Symptoms, Neurological Impacts and Menopausal Depression
Menopausal VMS describe hot flushes and night sweats that affect 80% of menopausal women [34]. They may begin in the perimenopausal period and are associated with a fluctuation and decline in ovarian hormones [35]. Hot flushes in particular can be quite disturbing for women, ranging from a state of transient warming to a sudden reddening of the skin with flushing and severe diaphoresis. Changes in heart rate, pressure in the head or chest, nausea and anxiety can also occur [34]. Cutaneous vasodilation and, to a lesser extent, sweating, underlines the physical expression of a hot flush [36]. LH shows pulsatile activity that synchronizes with the occurrence of hot flashes [36, 37]. Underlying mechanisms of VMS are thought to involve thermoregulatory dysfunction, hippocampal connectivity dysfunction, and changes in neuronal opioid activity [34, 38, 39]. The thermoregulatory hypothesis of VMS involves impaired signalling between the neuroendocrine, autonomic and somatomotor pathways. As the major temperature regulatory pathway in the brain, the hypothalamus receives afferent neurological signals about temperature from the periphery. Under normal conditions, it responds with efferent signals to cause vasodilation and vasoconstriction in response to increased and decreased temperature, respectively. In menopause, it is thought that VMS arise from an exaggerated response to small increases in temperature [34]. The hippocampal hypothesis associates hot flushes with increased levels of connectivity in the default mode network (DMN)—the region of the brain usually active in the absence of external stimuli. Interestingly, hyperactivity in the DMN is seen in both hot flushes and major depression, independently [38]. The opioid hypothesis maintains that endogenous opioid binding capacity and opioid-mediated inhibition of GnRH declines in menopause [40, 41]. A study on ovariectomized rats treated with morphine showed that opioid withdrawal triggered similar body temperature surges to those seen in menopausal hot flushes [39]. Finally, numerous animal experiments by Rance et al. have shown that the KNDy peptide, a co-expression of kisspeptin, neurokinin B and dynorphin, is involved in hypothalamic signalling mechanisms that contribute to VMS [37]. In a study on female rats, it was found that KNDy neurons not only project to the very hypothalamic regions believed to control temperature reduction (the median preoptic nucleus) but also converge with GnRH neurons. As GnRH controls the pulsatile activity of LH, and LH release is thought to be temporally correlated to hot flushes, KNDy neuronal activity could explain the relationship between LH pulsatility and hot flushes [37]. Moreover, in a similar experiment, Rance et al. found that the skin tail temperature of KNDy neuron-ablated rats was reduced compared with control rats, indicating that KNDy neurons may promote cutaneous vasodilation, a major sign of hot flushes [37, 42].
Despite a number of reports that hot flushes accentuate the risk of depressive symptoms in perimenopause [3, 43], multiple high-quality studies have showed that there is an increased risk of having depression in the menopausal transition, even when controlled for hot flashes and life stressors [5, 7, 44].
3.2 Menopausal Depression
The neurobiological basis of depression is not fully understood but is thought to involve dopaminergic/serotonergic pathways. In healthy individuals, dopaminergic neurons in the mesolimbic pathway regulate motivation, reward, and pleasure. Many of these dopaminergic pathways are modulated by serotonergic neurons [45]. Models of depression demonstrate altered mesolimbic signalling and dysfunction of the amygdala pathways involved in emotional control [45, 46]. Symptoms are reversed with agents that increase dopaminergic and serotonergic transmission [46, 47], indicating that depression is associated with a decline in serotonin and dopamine. Estrogen itself is believed to be involved with the modulation of serotonin via modulation of serotonin receptor expression [25]. Estrogen levels fluctuate during menopause, causing destabilizing effects on mood and levels of serotonergic neurotransmitters [48, 49]. Changes in major neuropeptide pathways can also affect mood in menopause. Dehydroepiandrosterone sulphate (DHEAS) is an endogenous steroid hormone and neuroregulator of serotonergic and γ-aminobutyric acid (GABA) neurotransmitter signalling. Levels of DHEAS decline with ageing, and a 2001 study by Morrison et al. found that there may be a relationship between lower levels of DHEAS in older women and increasing symptoms of depression [50]. In 2002, Schmidt and colleagues showed that DHEAS levels in depressed perimenopausal and postmenopausal women were significantly lower than that of non-depressed controls [35]. As DHEAS is an adrenal precursor to estrogen, perhaps low levels of DHEAS may interact with declining and fluctuating levels of estrogen to increase the risk of depressive symptoms in the menopausal period [35, 51]. Similarly, a decline in GABAergic inhibitory function is seen in postmenopausal depression [52]. The GABAergic influence over postmenopausal depression parallels the reduced levels of GABA implicated in major depression [53]. Finally, endogenous opioid dysfunction may be involved in the pathophysiology of major depressive disorder [54], and perhaps the change in neuronal opioid activity during menopause may be involved in the pathophysiology of associated depression.
4 Neuroprotective Effects of Estrogen and Associations with Menopause
Estrogen continually contributes to brain growth and development via regulating cell survival, differentiation, proliferation and migration [11, 26], and is ultimately involved in neurogenesis [55]. Estrogen decline is associated with reduced levels of brain-derived neurotropic factor (BDNF) [56], indicating that estrogen is essential to maintaining growth factors. In the study by Woolley et al., estrogen-treated ovariectomized rats had increased density of hippocampal neurone synapses and apical dendritic spines [57]. Similarly, animal modelling of multiple sclerosis showed that estrogen treatment resulted in increased axonal remyelination and preserved axonal integrity, compared with controls [58]. Animal and human studies have demonstrated that estrogen improves the activity of neuronal antioxidants [59, 60], thereby protecting against neurodegenerative diseases [11]. Brain metabolism is also affected by estrogen. Estrogen may enhance glucose metabolism by augmenting glucose transporters to enable better glucose utilization [61, 62], a process paramount to neuronal homeostasis. Moreover, estradiol-treated patients have reduced hippocampal atrophy, preserved age-related loss of gray matter, and improved cerebral blood flow [63,64,65]. A preliminary neuroimaging study of elderly Mexican women showed that those receiving estrogen therapy (ET) had larger magnetic resonance imaging (MRI)-measured hippocampal brain volume compared with untreated women [63]; however, their menopausal status was not mentioned. Boccardi and colleagues also conducted a neuroimaging study on women to evaluate the effect of ET on cerebral matter [64]. Participants, who were all postmenopausal, were assessed using MRI to detect gray matter volume in those previously and currently treated with ET, and those untreated. Current ET comprised of transdermal estradiol 50–100 ug/day, and past ET was not explicitly defined. Both current and past ET use was associated with larger gray matter MRI-measured volumes compared with no ET use [64]. Finally, a Finnish study investigated changes in carotid artery pulsatility index in postmenopausal women. After treatment with oral or transdermal sequential cyclical combined HT for 12 months, mean carotid artery pulsatility significantly decreased with oral and transdermal HT; increased cerebral vascularity was likely due to nitrous oxide-induced vasodilation from estrogen [65]. As such, trophic molecular effects demonstrate that estrogen’s protective effect on the brain may prevent neurodegenerative disease.
In the study by Maggioli et al., ovariectomized mice exhibited increased levels of Annexin A1 (ANXA1) after treatment with estradiol [66]. ANXA1 is an anti-inflammatory protein that regulates blood–brain barrier (BBB) endothelial tight junctions, thereby limiting permeation of toxic substances into the brain. Estrogen treatment increased levels of CNS ANXA1, reduced endothelial paracellular permeability, and inhibited lymphocyte migration into the brain. The effect of estrogen on the inflammatory response has also been shown in a small human study by Puder et al., where six postmenopausal women were tested for their response to endotoxin administration both with and without ET [67]. There was a significantly diminished endotoxin-induced release of inflammatory cytokines (specifically, interleukin-6, tumour necrosis factor-α and interleukin-1 receptor antagonist) after treatment with transdermal estrogen 100 µg/day for 1 month, compared with no treatment [67]. Thus, estrogen may also modulate inflammatory cytokines and limit BBB penetrability and lymphocyte transmigration, thereby protecting against inflammation implicated in certain cerebrovascular diseases.
Estrogen loss associated with menopause is perhaps the reason that women are not only at an increased risk of AD than men [68] but also experience a more accelerated cognitive decline [11]. AD may be less common in postmenopausal women who use ET [69,70,71,72]. However, there is conflicting evidence regarding the association between HT and AD. Early observational studies indicated that the use of HT with estrogen in particular reduced the risk of, and improved cognition of patients with, AD [73,74,75], while a double-blinded, randomized controlled trial (RCT; the Women’s Health Initiative Memory Study [WHIMS]) showed an increased risk for AD in women using HT [76,77,78]. In the two-arm study, both ET and estrogen/progesterone combination therapy increased the risk of AD compared with placebo [77, 78]. However, women who participated in the WHIMS study were beyond the mean age of menopause onset and usual age of HT initiation in clinical practice. More recent studies have shown that HT is protective against dementia if administered within a critical window of time [69, 79]. The critical period hypothesis suggests that HT may delay the progression and/or reduce the risk of AD if administered within the early menopause period [80, 81]. However, a recent Finnish study opposes the critical period hypothesis, showing that long-term use of systemic HT increases the risk of AD regardless of age at initiation [80].
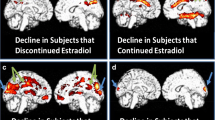
Overall, the positive effects of estrogen on brain structure, function and integrity, independent of age, are clear and may make menopause a time of increased risk of neurological disease for women. Mosconi et al. demonstrated that women exhibit higher rates of amyloid deposition, accelerated hippocampal volume loss, and reduced glucose utilization across the menopausal transition, but particularly within the early stage of perimenopause to menopause [33, 69]. The specific period of perimenopause itself poses an increased risk of AD. A 2021 study on brain connectivity in women found that when adjusted for women who had a positive apolipoprotein E4 (APOE-4) phenotype, amyloid-β deposition was higher in peri- and postmenopausal women compared with premenopausal women [33]. Amyloid-β deposition is one of the main mechanisms underlying the pathophysiology of AD. Possession of an APOE-4 genotype increases the risk for developing inherited forms of AD. The stage of menopausal transition appears to have an effect on human brain structure, metabolism, and connectivity regardless of age [33].
5 Treatment of Menopause-Associated Depression
There is a gap in research studying treatments for menopause-associated depression. In the study by Soares et al., HT was superior to placebo in treating perimenopausal depression [44]. Although not yet approved in Australia and other countries for the treatment of depression associated with menopause, recent studies using HT with estrogen have shown that estrogen is efficacious in treating psychological conditions in women [82, 83]. However, HT is contraindicated in women with a history of breast cancer [84]. Similarly, some women will need to use progesterone in addition to estrogen rather than sole estrogen HT, the combination of which is not ideal for all women, as we explore below [84]. The selective estrogen receptor modulators (SERMs) emulate estrogen’s neuroprotective effect in the CNS while not affecting breast and endometrial tissue [85, 86]. SERMs bypass the need for adjunctive progesterone and offer an alternative avenue of HT for PD, although they have yet to be approved for use in menopausal depression.
5.1 Antidepressants and Perimenopausal Depression
Menopausal depressive symptoms are highest during the early perimenopause period [3, 10, 20], and thus perimenopause presents an opportunity for effective treatment of menopausal depression. Current guidelines recommend traditional antidepressants, psychological therapy, and lifestyle changes as first-line management of depression during menopause [84, 87]; however, antidepressants may not be efficacious for every woman. Some postmenopausal women with major depressive disorder may not respond to the widely used selective serotonin reuptake inhibitor (SSRI) escitalopram [88], and it is also possible for older women to develop tachyphylaxis to the SSRIs [89]. Desvenlafaxine 50 mg daily was found to be significantly efficacious in treating major depressive disorder in peri- and postmenopausal women in a large randomized, placebo-controlled study by Kornstein et al. [90]; however, it is the only antidepressant that has been studied in a large placebo-controlled trial on the treatment of perimenopausal depression in participants with clearly defined menopausal status.
5.2 Traditional Hormone Therapy
To date, HT is the most efficacious treatment for VMS and vulvovaginal atrophy [87]. As most symptoms of menopause are caused by the estrogen deficit accompanying ovarian senescence, treatment with estrogen can provide symptom relief. The mechanism of action of HT involves similar pathways to endogenous estrogen action at estrogen receptors, whereby estrogen binds to its nuclear receptors or GPCR to regulate gene transcription [91]. The effect of estrogen on multiple symptoms occurs due to the differential expression of estrogen receptors in the body and its distinct action on cells. Despite its beneficial effects in treating menopausal symptoms, ET alone increases the risk of endometrial thickening and endometrial tumours [73, 92]. Progesterone causes endometrial shedding and interferes with estrogen binding to estrogen receptors, thereby counteracting estrogen’s proliferative effect on uterine tissue [93]. Therefore, progesterone is used in combined hormonal replacement therapy to stabilize the uterine endometrium tissue and attenuate the risk. Progesterone therapy can be administered as cyclic or continuous. Cyclic therapy has a 40% incidence of breakthrough bleeding, considered an endometrial secretory ‘withdrawal bleed’, which is annoying for many women compromise treatment adherence [73]. Continuous formulations reduce this bleeding irregularity and are a potential alternative option for women. However, continuous therapy with some types of synthetic progesterones may increase the risk of breast cancer [94,95,96], likely due to effects on breast tissue proliferation [94]. Based on a recent systematic review of the impact of menopausal hormone therapy (MHT) containing micronized progesterone on the mammary gland, an international expert panel recommended that estrogens combined with oral (approved) or vaginal (off-label use) micronized progesterone do not increase breast cancer risk for up to 5 years of treatment duration. There is limited evidence that estrogens combined with oral micronized progesterone applied for more than 5 years are associated with an increased breast cancer risk [97]. Despite its favourable effect on lipids and the belief that it may be beneficial in preventing cardiovascular disease [98, 99], HT (especially with oral estrogen) may increase coagulability and has not been shown to protect against cardiovascular disease or stroke [73, 100,101,102].
Ultimately, the benefits of HT in symptomatic women appear to outweigh the risks and it is therefore recommended as first-line medical treatment for vasomotor and urogenital symptoms in menopause [84, 87]. Certainly, there are many HT formulations available suited to an individual’s symptoms, comorbidities, and risk factors [103, 104]. Treatment should be individualized based on the woman’s treatment preferences.
5.3 Estrogen Therapy
In addition to its protective effects against cognitive decline, estrogen has been shown to be efficacious in treating psychological conditions in women [44, 82, 83]. Schmidt et al. evaluated the role of ET in perimenopausal women with major or minor depression [105]. In their double-blind RCT, women were treated with transdermal 17β-estradiol 0.5 mg/day or placebo patches for 3 weeks. Depression rating scale scores were significantly lower in the treatment group compared with controls at the end of the initial 3 weeks [105]. In secondary analysis, both the treatment and placebo groups were treated with a further 3 weeks of transdermal 17β-estradiol 0.5 mg/day. At the end of the total 6 weeks, the treatment group maintained their reduced scores compared with baseline [105]. Placebo patients showed significantly improved depression rating scores at the end of the 6 weeks compared with the initial 3 weeks without active treatment [105]. A more recent double-blind RCT of 17β-estradiol found that women with endocrinologically confirmed perimenopause had significantly reduced depressive symptoms with estrogen treatment compared with placebo [44]. The trial by Soares and colleagues used 100 µg of transdermal 17β-estradiol compared with identical placebo patches for a treatment duration of 12 weeks. The majority of women treated with 17β-estradiol also had complete remission of depressive symptoms, with comparable adverse effects to the placebo group [44]. Other studies have shown that combination therapy with traditional antidepressants plus estrogen is more efficacious in treating depression during menopause than using either antidepressants or estrogen alone [106, 107]. Nagata et al. compared the use of sole ET, consisting of conjugated equine estrogens 0.3125 mg/day, with estrogen plus fluvoxamine 50 mg daily therapy in oophorectomized women [106]. During the 8 weeks of trial treatment, participants receiving combination ET plus SSRI had significantly improved symptoms of depression compared with those receiving ET alone [106]. Participants in the double-blind study by Schneider et al. who were treated with any form of ET plus fluoxetine 20 mg daily had significantly improved depression rating scores compared with those receiving fluoxetine 20 mg daily alone [107, 108]. Kulkarni et al. demonstrated a similar augmentation of psychological therapy in their double blind placebo controlled trial studying the use of estrogen augmented antipsychotic treatment in schizophrenia [109]. In their study, 102 women in either an acute or chronic phase of schizophrenia, schizoaffective disorder or schizophreniform disorder were randomized to receive either 100 µg estradiol transdermal patch or identical placebo patches in adjunct to their regular antipsychotic medication regimen. The addition of estradiol significantly reduced psychopathological symptoms compared with sole antipsychotic therapy [109]. These studies may suggest that estrogen has a role to play in the treatment of menopause-associated depression. However, as outlined above, sole ET can increase the risk of certain cancers, and the addition of progesterone may reduce the psychological benefits of ET [73].
5.4 Selective Estrogen Receptor Modulators
The SERMs offer a unique alternative to HT as they possess the beneficial therapeutic effects of estrogen on bone, lipids and brain, while minimizing adverse effects on the uterus and breast [91, 110]. SERMS are estrogen receptor ligands that bind the estrogen receptor ER-α and/or ER-β, resulting in a conformational change in the estrogen receptor binding domain [110]. Their competitive inhibition of estrogen at estrogen receptors has downstream effects on gene transcription by altering the way in which the receptor complex interacts with estrogen response elements (EREs) on cognate DNA, and by interacting with various molecules that regulate receptor function (coactivators, corepressors, and gene transcription factors) [91, 110]. The distinct effect of SERMs on particular tissues is directed by the differential expression of estrogen receptor subtypes in various tissues, as well as the type of ligand-receptor complex formed (and its subsequent effects on gene expression) from drug binding [110]. Raloxifene is a benzothiophene used for the prevention of postmenopausal osteoporosis [91]. It is an estrogen receptor antagonist in breast tissue and an agonist in bone tissue with no agonistic properties in the uterus [110]. It is used in breast cancer treatment but, unlike tamoxifen, does not increase the risk of endometrial cancer with chronic use [91]. Raloxifene may also have effects on neuronal tissue by blocking endogenous estrogen activation of EREs on DNA, modulating the serotonin receptors, and mimicking estrogen’s prolific effects on BDNF [91]. It may also exert positive effects on memory and hypoxia-induced brain injury [91, 111]. Moreover, a 2016 study by Kulkarni et al. found that higher doses of raloxifene (120 mg/day orally) improved treatment refractory schizophrenia from an illness severity and clinical response perspective [85]. A study of 62 women with menopause-related depression with MHT randomized to four treatment groups (raloxifene 60 mg/day; a phytoestrogen, Rimostil; transdermal estradiol [TE; 100 μg/day]; or placebo). No improvement in depression was described after the 8-week study for the women in any treatment arm [112]. The authors concluded “No differences were observed between raloxifene and either TE or placebo in any scale score”. Hamilton Rating Scale for Depression (HRSD) scores in women assigned to TE were improved compared with those taking Rimostil during weeks 6 and 8 (p = 0.0008 and 0.0011, respectively). The small sample size, low dose of raloxifene, and length of the trial could all be confounding factors in this study.
Tibolone is another SERM with promising neuronal and psychological effects. It may be neuroprotective via antioxidant production at a cellular level [113] and is a promising treatment for perimenopausal depression. A recent study found that tibolone was effective, compared with placebo, in reducing depression symptoms in postmenopausal women [86]. Unlike tamoxifen and raloxifene, it reduces menopausal VMS and vaginal dryness with less bleeding irregularities than that of HRT [114]. Tibolone’s structure differs from raloxifene and estrogen. It has two active metabolites that lend its estrogenic, progestogenic and androgenic effects in preventing estrogen stimulation at the endometrium, preserving trabecular and cortical bone length, inhibiting mammary tissue proliferation, and counteracting vaginal dryness [115]. Finally, tissue selective estrogen complex (TSEC) describes the SERM bazedoxifene combined with conjugated estrogens. In animal studies, bazedoxifene has anti-estrogenic effects on uterine and breast tissue. TSEC appears to improve climacteric and psychological symptoms of menopause, with a 2017 study showing that it improved mood, emotions and overall quality of life in menopausal women [116]. Another important consideration is the link between menopause and cognition. Early reviews claimed that there were no substantial or clinically relevant changes in cognitive functioning associated with the menopause [117, 118]. The timing of menopause studied, ages of women, and the effects of cognitive aging in women at retirement age were often not measured [119]. However, more recent data from the Penn Ovarian Aging Study, which aimed to determine whether the menopausal transition is associated with age-independent cognitive decline, found that verbal fluency, but not psychomotor speed, is linked to reproductive senescence independent of age [120]. The ‘critical period’ hypothesis coined by Resnick and Henderson [121] states that hormone treatment of women closer to the menopausal transition might be more beneficial to cognition. However, two recent randomized trials (WHIMS-Y and KEEP-Cog) testing this hypothesis showed neither harm nor benefit of HT interventions closer to menopause [81, 122,123,124]. In view of the discrepancy in results, future research with the SERMs in particular, which are purported to have greater direct CNS impact, is critical for the future cognitive wellbeing for women.
The SERMs may be a promising alternative to HT in not only the climacteric symptoms of menopause but also in the treatment of menopausal-associated psychological and cognitive symptoms, particularly in view of the better breast, uterine and ovarian tissue safety aspects of SERMs compared with standard MHT. Certainly, the clues that point towards the possibility that hormone therapy with SERMs is useful as a treatment for menopause are evident in the theoretical animal literature, and studies in schizophrenia indicate that SERMs may well have a role in managing symptoms of mental illness.
However, robust data are needed from large clinical trials that are well-powered to account for the many confounding factors, including the heterogeneity of depression itself, to truly understand whether SERM treatment in menopause-associated depression is effective or not. Hence, to date, SERMs have not yet been approved for the treatment of depression or changes in cognition associated with menopause.
6 Discussion
There is no Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) definition or clear classification for perimenopausal depression, and this omission demonstrates the lack of understanding of the connection between the MT process and the well-noted rise in depression in middle-aged women.
The increased risk of depression in the perimenopause transition period appears to encompass two different groups of women. The first group includes women with no past history of depression who experience a fourfold increase in depression when they become menopausal [39]. The second group includes women with a past history of depressive disorders, who are at an even greater increased risk of further depressive episodes during menopause. In clinical populations, women with pre-existing psychiatric conditions account for the majority of presentations [125]. In a cross-sectional study, 57% of women with previously diagnosed depression suffered a relapse during the MT, with an increase in the severity of menopausal depressive symptoms experienced [7].
The evidence to date supports the notion that women with menopause-associated depression do not suffer from a gonadal hormone abnormality as such but have a brain response to the hormonal fluctuations, leading to depression associated with the MT [29].
Along with psychological and social factors, this brain hormone response is a critical aetiological factor for perimenopausal depression in some women. Following this aetiological clue, new lines of treatments with gonadal hormone modulators show promise as potential treatments, either alone or as adjuncts to antidepressant medications.
It is therefore surprising that there are very few clinical treatment trials examining hormone treatments for menopausal women with either first-time depression or a relapse. Future large-scale clinical trials are required to determine the efficacy of standard hormone therapy or SERMs in the treatment of menopausal depression
7 Conclusion
The mood and cognitive effects of menopause are manifold and better constructed clinical trials of the newer forms of HT are urgently needed. All women experience menopause and unfortunately many women experience debilitating depression. New, effective, and safe treatments with HTs are an obvious option and further clinical trials are required to improve outcomes for many women.
Change history
19 October 2022
Missing Open Access funding information has been added in the Funding Note
References
Perimenopause or Menopausal Transition. Australian Menopause Society; 2017. Available at: https://www.menopause.org.au/hp/information-sheets/1057-perimenopause. Accessed 11 May 2021.
Soules MR, Sherman S, Parrott E, Rebar R, Santoro N, Utian W, Woods N. Executive summary: stages of reproductive aging workshop (STRAW). Fertil Steril. 2001;76(5):874–8. https://doi.org/10.1016/s0015-0282(01)02909-0.
Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63(4):385–90. https://doi.org/10.1001/archpsyc.63.4.385.
Steiner M, Dunn E, Born L. Hormones and mood: from menarche to menopause and beyond. J Affect Disord. 2003;74:67–83. https://doi.org/10.1016/S0165-0327(02)00432-9.
Bromberger JT, Kravitz HM, Chang YF, Cyranowski JM, Brown C, Matthews KA. Major depression during and after the menopausal transition: study of Women’s Health Across the Nation (SWAN). Psychol Med. 2011;41:1879–88. https://doi.org/10.1017/S003329171100016X.
Bromberger JT, Matthews KA, Schott LL, Brockwell S, Avis NE, Kravitz HM, et al. Depressive symptoms during the menopausal transition: the study of Women’s Health Across the Nation (SWAN). J Affect Disord. 2007;103(1–3):267–72. https://doi.org/10.1016/j.jad.2007.01.034.
Steinberg EM, Rubinow DR, Bartko JJ, Fortinsky PM, Haq N, Thompson K, et al. A cross-sectional evaluation of perimenopausal depression. J Clin Psychiatry. 2008;69(6):973–80. https://doi.org/10.4088/JCP.v69n0614.
Chedraui P, Pérez-López FR, Morales B, Hidalgo L. Depressive symptoms in climacteric women are related to menopausal symptom intensity and partner factors. Climacteric. 2009;12:395–403. https://doi.org/10.1080/13697130902718150.
Jacobs EG, Holsen LM, Lancaster K, Makris N, Whitfield-Gabrieli S, Remington A, et al. 17β-Estradiol differentially regulates stress circuitry activity in healthy and depressed women. Neuropsychopharmacology. 2015;40(3):566–76. https://doi.org/10.1038/npp.2014.203.
Freeman EW, Sammel MD, Liu L, Gracia CR, Nelson DB, Hollander L. Hormones and menopausal status as predictors of depression in women in transition to menopause. Arch Gen Psychiatry. 2004;61(1):62–70. https://doi.org/10.1001/archpsyc.61.1.62.
Bustamante-Barrientos FA, Méndez-Ruette M, Ortloff A, Luz-Crawford P, Rivera FJ, Figueroa CD, et al. The Impact of estrogen and estrogen-like molecules in neurogenesis and neurodegeneration: beneficial or harmful? Front Cell Neurosci. 2021;15: 636176. https://doi.org/10.3389/fncel.2021.636176.
Genazzani AR, Lucchesi A, Stomati M, Catarsi S, Genazzani AD, Criscuolo M, et al. Effects of sex steroid hormones on the neuroendocrine system. Eur J Contracept Reprod Heal Care. 1997;2(1):63–9. https://doi.org/10.1080/13625189709049935.
Nappi RE, Lachowsky M. Menopause and sexuality: prevalence of symptoms and impact on quality of life. Maturitas. 2009;63(2):138–41. https://doi.org/10.1016/j.maturitas.2009.03.021.
Avis NE, Ory M, Matthews KA, Schocken M, Bromberger J, Colvin A. Health-related quality of life in a multiethnic sample of middle-aged women: study of women’s health across the nation (SWAN). Med Care. 2003;41(11):1262–76. https://doi.org/10.1097/01.MLR.0000093479.39115.AF.
Australian Bureau of Statistics. National Survey of Mental Health and Wellbeing: Summary of Results. Australian Buerau of Statistics; 2008.
Mishra GD, Chung H-F, Dobson A. The current state of women’s health in Australia: Informing the development of the National Women’s Health Strategy 2020–2030. Jean Hailes for Women’s Health; July 2018. Available at: https://consultations.health.gov.au/population-health-and-sport-division-1/establishing-a-national-womens-health-strategy/supporting_documents/Evidence ReviewThe current state of womens health.pdf. Accessed 2 Aug 2021.
Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4(2):146–58. https://doi.org/10.1016/S2215-0366(16)30263-2.
Avis NE, Brambilla D, McKinlay SM, Vass K. A longitudinal analysis of the association between menopause and depression Results from the Massachusetts women’s health study. Ann Epidemiol. 1994;4(3):214–20. https://doi.org/10.1016/1047-2797(94)90099-X.
Kulkarni J. Perimenopausal depression—an under-recognised entity. Aust Prescr. 2018;41(6):183–5. https://doi.org/10.18773/AUSTPRESCR.2018.060.
Maartens LWF, Knottnerus JA, Pop VJ. Menopausal transition and increased depressive symptomatology: a community based prospective study. Maturitas. 2002;42(3):195–200. https://doi.org/10.1016/S0378-5122(02)00038-5.
Messinisi IE. Ovarian feedback, mechanism of action and possible clinical implications. Hum Reprod Update. 2006;12(5):557–71. https://doi.org/10.1093/humupd/dml020.
Padmanabhan V, Puttabyatappa M, Cardoso RC. Hypothalamus-pituitary-ovary axis. Encycl Reprod. 2018;107:377–422. https://doi.org/10.1016/B978-0-12-801238-3.64632-9.
Burger H. The menopausal transition. Endocrinol J Sex Med. 2008;5(10):2266–73. https://doi.org/10.1111/j.1743-6109.2008.00921.x.
Lamberts SWJ, Van Den Beld AW, Van Der Lely AJ. The endocrinology of aging. Science. 1997;278(5337):419–24. https://doi.org/10.1126/science.278.5337.419.
Rubinow DR, Schmidt PJ, Roca CA. Estrogen-serotonin interactions: implications for affective regulation. Biol Psychiatry. 1998;44(9):839–50. https://doi.org/10.1016/S0006-3223(98)00162-0.
Pinceti E, Shults CL, Rao YS, Pak TR. Differential effects of E2 on MAPK activity in the brain and heart of aged female rats. PLoS ONE. 2016;11(8): e0160276. https://doi.org/10.1371/journal.pone.0160276.
Burger HG, Hale GE, Dennerstein L, Robertson DM. Cycle and hormone changes during perimenopause: the key role of ovarian function. Menopause. 2008;15(4 Pt 1):603–12. https://doi.org/10.1097/gme.0b013e318174ea4d.
Kulkarni J. How to treat-perimenopausal depression. Austr Doctor. 2017;2:17–24.
Liu N, Zhang Y, Liu S, Zhang X, Liu H. Brain functional changes in perimenopausal women: an amplitude of low-frequency fluctuation study. Menopause. 2021;28(4):384–90. https://doi.org/10.1097/GME.0000000000001720.
McKinlay SM, Brambilla DJ, Posner JG. The normal menopause transition. Maturitas. 1992;14(2):103–15. https://doi.org/10.1016/0378-5122(92)90003-M.
Bungay GT, Vessey MP, McPherson CK. Study of symptoms in middle life with special reference to the menopause. Br Med J. 1980;281(6234):181–3. https://doi.org/10.1136/bmj.281.6234.181.
Maki PM, Kornstein SG, Joffe H, Bromberger JT, Freeman EW, Athappilly G, et al. Guidelines for the evaluation and treatment of perimenopausal depression: Summary and recommendations. J Women’s Health. 2019;28(2):117–34. https://doi.org/10.1089/jwh.2018.27099.mensocrec.
Mosconi L, Berti V, Dyke J, Schelbaum E, Jett S, Loughlin L, et al. Menopause impacts human brain structure, connectivity, energy metabolism, and amyloid-beta deposition. Sci Rep. 2021;11(1):10867. https://doi.org/10.1038/s41598-021-90084-y.
Deecher DC, Dorries K. Understanding the pathophysiology of vasomotor symptoms (hot flushes and night sweats) that occur in perimenopause, menopause, and postmenopause life stages. Arch Womens Ment Health. 2007;10(6):247–57. https://doi.org/10.1007/s00737-007-0209-5.
Schmidt PJ, Murphy JH, Haq N, Danaceau MA, St Clair LS. Basal plasma hormone levels in depressed perimenopausal women. Psychoneuroendocrinology. 2002;27(8):907–20. https://doi.org/10.1016/S0306-4530(02)00004-5.
Kronenberg F. Menopausal hot flashes: a review of physiology and biosociocultural perspective on methods of assessment. J Nutr. 2010;140(7):1380S-S1385. https://doi.org/10.3945/jn.109.120840.
Rance NE, Dacks PA, Mittelman-Smith MA, Romanovsky AA, Krajewski-Hall SJ. Modulation of body temperature and LH secretion by hypothalamic KNDy (kisspeptin, neurokinin B and dynorphin) neurons: a novel hypothesis on the mechanism of hot flushes. Front Neuroendocrinol. 2013;34(3):211–27. https://doi.org/10.1016/j.yfrne.2013.07.003.
Thurston RC, Maki PM, Derby CA, Sejdić E, Aizenstein HJ. Menopausal hot flashes and the default mode network. Fertil Steril. 2015;103(6):1572-1578.e1. https://doi.org/10.1016/j.fertnstert.2015.03.008.
Simpkins JW, Katovich MJ, Cheng SI. Similarities between morphine withdrawal in the rat and the menopausal hot flush. Life Sci. 1983;32(17):1957–66. https://doi.org/10.1016/0024-3205(83)90047-4.
Zubieta JK, Dannals RF, Frost JJ. Gender and age influences on human brain mu-opioid receptor binding measured by PET. Am J Psychiatry. 1999;156(6):842–8. https://doi.org/10.1176/ajp.156.6.842.
Abel TW, Rance NE. Proopiomelanocortin gene expression is decreased in the infundibular nucleus of postmenopausal women. Mol Brain Res. 1999;69(2):202–8. https://doi.org/10.1016/S0169-328X(99)00111-4.
Mittelman-Smith MA, Williams H, Krajewski-Hall SJ, McMullen NT, Rance NE. Role for kisspeptin/neurokinin B/dynorphin (KNDy) neurons in cutaneous vasodilatation and the estrogen modulation of body temperature. Proc Natl Acad Sci U S A. 2012;109(48):19846–51. https://doi.org/10.1073/pnas.1211517109.
Reed SD, Ludman EJ, Newton KM, Grothaus LC, LaCroix AZ, Nekhlyudov L, et al. Depressive symptoms and menopausal burden in the midlife. Maturitas. 2009;62(3):306. https://doi.org/10.1016/j.maturitas.2009.01.002.
De Novaes SC, Almeida OP, Joffe H, Cohen LS. Efficacy of estradiol for the treatment of depressive disorders in perimenopausal women: a double-blind, randomized, placebo-controlled trial. Arch Gen Psychiatry. 2001;58(6):529–34. https://doi.org/10.1001/archpsyc.58.6.529.
Dunlop BW, Nemeroff CB. The role of dopamine in the pathophysiology of depression. Arch Gen Psychiatry. 2007;64(3):327–37. https://doi.org/10.1001/archpsyc.64.3.327.
Fitzgerald PB, Laird AR, Maller J, Daskalakis ZJ. A meta-analytic study of changes in brain activation in depression. Hum Brain Mapp. 2008;29(6):683–95. https://doi.org/10.1002/hbm.20426.
Jakobsen JC, Katakam KK, Schou A, Hellmuth SG, Stallknecht SE, Leth-Møller K, et al. Selective serotonin reuptake inhibitors versus placebo in patients with major depressive disorder. A systematic review with meta-analysis and trial sequential analysis. BMC Psychiatry. 2017;17:58. https://doi.org/10.1186/s12888-016-1173-2.
Freeman EW, Sammel MD, Lin H, Nelson DB. Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry. 2006;63(4):375–82. https://doi.org/10.1001/archpsyc.63.4.375.
Halbreich U. Gonadal hormones, reproductive age, and women with depression. Arch Gen Psychiatry. 2000;57(12):1163–4. https://doi.org/10.1001/archpsyc.57.12.1163.
Morrison MF, Ten Have T, Freeman EW, Sammel MD, Grisso JA. DHEA-S levels and depressive symptoms in a cohort of African American and Caucasian women in the late reproductive years. Biol Psychiatry. 2001;50(9):705–11. https://doi.org/10.1016/S0006-3223(01)01169-6.
Labrie F, Bélanger A, Cusan L, Candas B. Physiological changes in dehydroepiandrosterone are not reflected by serum levels of active androgens and estrogens but of their metabolites: Intracrinology. J Clin Endocrinol Metab. 1997;82(8):2403–9. https://doi.org/10.1210/jcem.82.8.4161.
Wang Z, Zhang A, Zhao B, Gan J, Wang G, Gao F, et al. GABA+ levels in postmenopausal women with mild-to-moderate depression A preliminary study. Med (United States). 2016;95(39): e4918. https://doi.org/10.1097/MD.0000000000004918.
Levinson AJ, Fitzgerald PB, Favalli G, Blumberger DM, Daigle M, Daskalakis ZJ. Evidence of cortical inhibitory deficits in major depressive disorder. Biol Psychiatry. 2010;67(5):458–64. https://doi.org/10.1016/j.biopsych.2009.09.025.
Kennedy SE, Koeppe RA, Young EA, Zubieta JK. Dysregulation of endogenous opioid emotion regulation circuitry in major depression in women. Arch Gen Psychiatry. 2006;63(11):1199–208. https://doi.org/10.1001/archpsyc.63.11.1199.
McClure RES, Barha CK, Galea LAM. 17β-Estradiol, but not estrone, increases the survival and activation of new neurons in the hippocampus in response to spatial memory in adult female rats. Horm Behav. 2013;63(1):144–57. https://doi.org/10.1016/j.yhbeh.2012.09.011.
Chhibber A, Woody SK, Karim Rumi MA, Soares M, Zhao L. Estrogen receptor β deficiency impairs BDNF-5-HT 2A signaling in the hippocampus of female brain: A possible mechanism for menopausal depression. Psychoneuroendocrinology. 2017;82:107–16.
Woolley CS, McEwen BS. Estradiol mediates fluctuation in hippocampal synapse density during the estrous cycle in the adult rat. J Neurosci. 1992;12(7):2549–54. https://doi.org/10.1523/jneurosci.12-07-02549.1992.
Kumar S, Patel R, Moore S, Crawford DK, Suwanna N, Mangiardi M, et al. Estrogen receptor β ligand therapy activates PI3K/Akt/mTOR signaling in oligodendrocytes and promotes remyelination in a mouse model of multiple sclerosis. Neurobiol Dis. 2013;56:131–44. https://doi.org/10.1016/j.nbd.2013.04.005.
Moorthy K, Sharma D, Basir SF, Baquer NZ. Administration of estradiol and progesterone modulate the activities of antioxidant enzyme and aminotransferases in naturally menopausal rats. Exp Gerontol. 2005;40(4):295–302. https://doi.org/10.1016/j.exger.2005.01.004.
Bellanti F, Matteo M, Rollo T, De Rosario F, Greco P, Vendemiale G, et al. Sex hormones modulate circulating antioxidant enzymes: Impact of estrogen therapy. Redox Biol. 2013;1(1):340–6. https://doi.org/10.1016/j.redox.2013.05.003.
Cheng CM, Cohen M, Wang J, Bondy CA. Estrogen augments glucose transporter and IGF1 expression in primate cerebral cortex. FASEB J. 2001;15(6):907–15. https://doi.org/10.1096/fsb2fj000398com.
Eberling JL, Wu C, Tong-Turnbeaugh R, Jagust WJ. Estrogen- and tamoxifen-associated effects on brain structure and function. Neuroimage. 2004;21(1):364–71. https://doi.org/10.1016/j.neuroimage.2003.08.037.
Eberling JL, Wu C, Haan MN, Mungas D, Buonocore M, Jagust WJ. Preliminary evidence that estrogen protects against age-related hippocampal atrophy. Neurobiol Aging. 2003;24(5):725–32. https://doi.org/10.1016/S0197-4580(02)00056-8.
Boccardi M, Ghidoni R, Govoni S, Testa C, Benussi L, Bonetti M, et al. Effects of hormone therapy on brain morphology of healthy postmenopausal women: A Voxel-based morphometry study. Menopause. 2006;13(4):584–91. https://doi.org/10.1097/01.gme.0000196811.88505.10.
Cacciatore B, Paakkari I, Toivonen J, Tikkanen M, Ylikorkala O. Randomized comparison of oral and transdermal hormone replacement on carotid and uterine artery resistance to blood flow. Obstet Gynecol. 1998;92(4 Pt 1):563–8. https://doi.org/10.1016/s0029-7844(98)00269-5.
Maggioli E, McArthur S, Mauro C, Kieswich J, Kusters DHM, Reutelingsperger CPM, et al. Estrogen protects the blood–brain barrier from inflammation-induced disruption and increased lymphocyte trafficking. Brain Behav Immun. 2016;51:212–22. https://doi.org/10.1016/j.bbi.2015.08.020.
Puder JJ, Freda PU, Goland RS, Wardlaw SL. Estrogen modulates the hypothalamic-pituitary-adrenal and inflammatory cytokine responses to endotoxin in women. J Clin Endocrinol Metab. 2001;86(6):2403–8. https://doi.org/10.1210/jc.86.6.2403.
Paganini-hill A, Henderson VW. Estrogen deficiency and risk of alzheimer’s disease in women. Am J Epidemiol. 1994;140(3):256–61. https://doi.org/10.1093/oxfordjournals.aje.a117244.
Mosconi L, Rahman A, Diaz I, Wu X, Scheyer O, Hristov HW, et al. Increased Alzheimer’s risk during the menopause transition: a 3-year longitudinal brain imaging study. PLoS ONE. 2018;13(12): e0207885. https://doi.org/10.1371/journal.pone.0207885.
Gatto NM, Deapen D, Stoyanoff S, Pinder R, Narayan S, Bordelon Y, et al. Lifetime exposure to estrogens and Parkinson’s disease in California teachers. Park Relat Disord. 2014;20(11):1149–56. https://doi.org/10.1016/j.parkreldis.2014.08.003.
Currie LJ, Harrison MB, Trugman JM, Bennett JP, Wooten GF. Postmenopausal estrogen use affects risk for Parkinson disease. Arch Neurol. 2004;61(6):886–8. https://doi.org/10.1001/archneur.61.6.886.
Zandi PP, Carlson MC, Plassman BL, Welsh-Bohmer KA, Mayer LS, Steffens DC, et al. Hormone replacement therapy and incidence of Alzheimer disease in older women: the Cache County Study. J Am Med Assoc. 2002;288(17):2123–9. https://doi.org/10.1001/jama.288.17.2123.
Wood AJJ, Belchetz PE. Hormonal treatment of postmenopausal women. N Engl J Med. 1994;330(15):1062–71. https://doi.org/10.1056/nejm199404143301508.
Kawas C, Resnick S, Morrison A, Brookmeyer R, Corrada M, Zonderman A, et al. A prospective study of estrogen replacement therapy and the risk of developing Alzheimer’s disease: the Baltimore Longitudinal Study of Aging. Neurology. 1997;48(6):1517–21. https://doi.org/10.1212/WNL.48.6.1517.
Waring SC, Rocca WA, Petersen RC, O’Brien PC, Tangalos EG, Kokmen E. Postmenopausal estrogen replacement therapy and risk of AD: a population-based study. Neurology. 1999;52(5):965–70. https://doi.org/10.1212/wnl.52.5.965.
Coker LH, Espeland MA, Rapp SR, Legault C, Resnick SM, Hogan P, et al. Postmenopausal hormone therapy and cognitive outcomes: the Women’s Health Initiative Memory Study (WHIMS). J Steroid Biochem Mol Biol. 2010;118:304–10. https://doi.org/10.1016/j.jsbmb.2009.11.007.
Shumaker SA, Legault C, Kuller L, Rapp SR, Thal L, Lane DS, et al. Conjugated equine estrogens and incidence of probable dementia and mild cognitive impairment in postmenopausal women: Women’s Health Initiative Memory Study. JAMA. 2004;291(24):2947–58. https://doi.org/10.1001/jama.291.24.2947.
Shumaker SA, Legault C, Rapp SR, Thal L, Wallace RB, Ockene JK, et al. Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women—the women’s health initiative memory study: a randomized controlled trial. J Am Med Assoc. 2003;289(20):2651–62. https://doi.org/10.1001/jama.289.20.2651.
Henderson VW, Benke KS, Green RC, Cupples LA, Farrer LA. Postmenopausal hormone therapy and Alzheimer’s disease risk: interaction with age. J Neurol Neurosurg Psychiatry. 2005;76(1):103–5. https://doi.org/10.1136/jnnp.2003.024927.
Savolainen-Peltonen H, Rahkola-Soisalo P, Hoti F, Vattulainen P, Gissler M, Ylikorkala O, et al. Use of postmenopausal hormone therapy and risk of Alzheimer’s disease in Finland: nationwide case-control study. BMJ. 2019;364: l665. https://doi.org/10.1136/bmj.l665.
Wharton W, Gleason CE, Miller VM, Asthana S. Rationale and design of the Kronos Early Estrogen Prevention Study (KEEPS) and the KEEPS cognitive and affective sub study (KEEPS Cog). Brain Res. 2013;1514:12–7. https://doi.org/10.1016/j.brainres.2013.04.011.
Lascurain MB, Camuñas-Palacín A, Thomas N, Breadon C, Gavrilidis E, Hudaib AR, et al. Improvement in depression with oestrogen treatment in women with schizophrenia. Arch Womens Ment Health. 2020;23(2):149–54. https://doi.org/10.1007/s00737-019-00959-3.
Kulkarni J, Gavrilidis E, Wang W, Worsley R, Fitzgerald PB, Gurvich C, et al. Estradiol for treatment-resistant schizophrenia: a large-scale randomized-controlled trial in women of child-bearing age. Mol Psychiatry. 2015;20(6):695–702. https://doi.org/10.1038/mp.2014.33.
RANZCOG. Managing menopausal symptoms 2020. Available at: https://ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27s Health/Statement and guidelines/Clinical-Gynaecology/Managing-Menopausal-Symptoms-(C-Gyn-9)_September-2020.pdf?ext=.pdf. Accessed 20 Aug 2021.
Kulkarni J, Gavrilidis E, Gwini SM, Worsley R, Grigg J, Warren A, et al. Effect of adjunctive raloxifene therapy on severity of refractory schizophrenia in women: a randomized clinical trial. JAMA Psychiat. 2016;73(9):947–54. https://doi.org/10.1001/jamapsychiatry.2016.1383.
Kulkarni J, Gavrilidis E, Thomas N, Hudaib AR, Worsley R, Thew C, et al. Tibolone improves depression in women through the menopause transition: a double-blind randomized controlled trial of adjunctive tibolone. J Affect Disord. 2018;236:88–92. https://doi.org/10.1016/j.jad.2018.04.103.
Stuenkel CA, Davis SR, Gompel A, Lumsden MA, Murad MH, Pinkerton JAV, et al. Treatment of symptoms of the menopause: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(11):3975–4011. https://doi.org/10.1210/jc.2015-2236.
Soares CN, Thase ME, Clayton A, Guico-Pabia CJ, Focht K, Jiang Q, et al. Open-label treatment with desvenlafaxine in postmenopausal women with major depressive disorder not responding to acute treatment with desvenlafaxine or escitalopram. CNS Drugs. 2011;25(3):227–38. https://doi.org/10.2165/11586460-000000000-00000.
Grigoriadis S, Kennedy SH, Bagby RM. A comparison of antidepressant response in younger and older women. J Clin Psychopharmacol. 2003;23(4):405–7. https://doi.org/10.1097/01.jcp.0000085415.08426.c6.
Kornstein SG, Jiang Q, Reddy S, Musgnung JJ, Guico-Pabia CJ. Short-term efficacy and safety of desvenlafaxine in a randomized, placebo-controlled study of perimenopausal and postmenopausal women with major depressive disorder. J Clin Psychiatry. 2010;71(8):1088–96. https://doi.org/10.4088/JCP.10m06018blu.
Littleton-Kearney MT, Ostrowski NL, Cox DA, Rossberg MI, Hurn PD. Selective estrogen receptor modulators: tissue actions and potential for CNS protection. CNS Drug Rev Fall. 2002;8(3):309–30. https://doi.org/10.1111/j.1527-3458.2002.tb00230.x.
Lacey JV, Mink PJ, Lubin JH, Sherman ME, Troisi R, Hartge P, et al. Menopausal hormone replacement therapy and risk of ovarian cancer. J Am Med Assoc. 2002;288(3):334–41. https://doi.org/10.1001/jama.288.3.334.
Staland B. Continuous treatment with a combination of estrogen and gestagen—a way of avoiding endometrial stimulation: clinical experiences with kliogest. Acta Obstet Gynecol Scand. 1981;3(2):145–56. https://doi.org/10.3109/00016348509157144.
Schairer C, Lubin J, Troisi R, Sturgeon S, Brinton L, Hoover R. Menopausal estrogen and estrogen-progestin replacement therapy and breast cancer risk. J Am Med Assoc. 2000;283(4):485–91. https://doi.org/10.1001/jama.283.4.485.
Olsson HL, Ingvar C, Bladström A. Hormone replacement therapy containing progestins and given continuously increases breast carcinoma risk in Sweden. Cancer. 2003;97(6):1387–92. https://doi.org/10.1002/cncr.11205.
Fournier A, Berrino F, Clavel-Chapelon F. Unequal risks for breast cancer associated with different hormone replacement therapies: Results from the E3N cohort study. Breast Cancer Res Treat. 2008;107(1):103–11. https://doi.org/10.1007/s10549-007-9523-x.
Stute P, Wildt L, Neulen J. The impact of micronized progesterone on breast cancer risk: a systematic review. Climacteric. 2018;21(2):111–22. https://doi.org/10.1080/13697137.2017.1421925.
Jacoby VL, Grady D, Wactawski-Wende J, Manson JE, Allison MA, Kuppermann M, et al. Oophorectomy vs ovarian conservation with hysterectomy: cardiovascular disease, hip fracture, and cancer in the women’s health initiative observational study. Arch Intern Med. 2011;171(8):760–8. https://doi.org/10.1001/archinternmed.2011.121.
Rivera CM, Grossardt BR, Rhodes DJ, Brown RD Jr, Roger VL, Melton LJ III, Rocca WA. Increased cardiovascular mortality following early bilateral oophorectomy. Menopause. 2009;16(1):15–23.
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the women’s health initiative randomized controlled trial. J Am Med Assoc. 2002;288(3):321–33. https://doi.org/10.1001/jama.288.3.321.
Simon JA, Hsia J, Cauley JA, Richards C, Harris F, Fong J, et al. Postmenopausal hormone therapy and risk of stroke: the Heart and Estrogen-progestin Replacement Study (HERS). Circulation. 2001;103(5):638–42. https://doi.org/10.1161/01.CIR.103.5.638.
Shuster LT, Gostout BS, Grossardt BR, Rocca WA, Rocca WA. Prophylactic oophorectomy in premenopausal women and long-term health. Menopause Int. 2008;14(3):111–6. https://doi.org/10.1258/mi.2008.008016.
Järvinen A, Nykänen S, Paasiniemi L. Absorption and bioavailability of oestradiol from a gel, a patch and a tablet. Maturitas. 1999;32(2):103–13. https://doi.org/10.1016/S0378-5122(99)00021-3.
Diem SJ, Guthrie KA, Mitchell CM, Reed SD, Larson JC, Ensrud KE, et al. Effects of vaginal estradiol tablets and moisturizer on menopause-specific quality of life and mood in healthy postmenopausal women with vaginal symptoms: a randomized clinical trial. Menopause. 2018;25(10):1086–93. https://doi.org/10.1097/GME.0000000000001131.
Schmidt PJ, Nieman L, Danaceau MA, Tobin MB, Roca CA, Murphy JH, et al. Estrogen replacement in perimenopause-related depression: a preliminary report. Am J Obstet Gynecol. 2000;183(2):414–20. https://doi.org/10.1067/mob.2000.106004.
Nagata H, Nozaki M, Nakano H. Short-term combinational therapy of low-dose estrogen with selective serotonin re-uptake inhibitor (fluvoxamine) for oophorectomized women with hot flashes and depressive tendencies. J Obstet Gynaecol Res. 2005;31(2):107–14. https://doi.org/10.1111/j.1447-0756.2005.00254.x.
Schneider LS, Small GW, Hamilton SH, Bystritsky A, Nemeroff CB, Meyers BS. Estrogen replacement and response to fluoxetine in a multicenter geriatric depression trial. Am J Geriatr Psychiatry Spring. 1997;5(2):97–106. https://doi.org/10.1097/00019442-199721520-00002.
Tollefson GD, Bosomworth JC, Heiligenstein JH, Potvin JH, Holman S. A double-blind, placebo-controlled clinical trial of fluoxetine in geriatric patients with major depression. Int Psychogeriatrics Spring. 1995;7(1):89–104. https://doi.org/10.1017/S1041610295001888.
Kulkarni J, de Castella A, Fitzgerald PB, Gurvich CT, Bailey M, Bartholomeusz C, et al. Estrogen in severe mental illness. Arch Gen Psychiatry. 2008;65(8):955–60. https://doi.org/10.1001/archpsyc.65.8.955.
Dutertre M, Smith CL. Molecular mechanisms of selective estrogen receptor modulator (SERM) action. J Pharmacol Exp Ther. 2000;295(2):431–7.
Rzemieniec J, Litwa E, Wnuk A, Lason W, Kajta M. Bazedoxifene and raloxifene protect neocortical neurons undergoing hypoxia via targeting ERα and PPAR-γ. Mol Cell Endocrinol. 2018;461:64–78. https://doi.org/10.1016/j.mce.2017.08.014.
Schmidt PJ, Wei SM, Martinez PE, Dor RRB, Guerrieri GM, Palladino PP, et al. The short-term effects of estradiol, raloxifene, and a phytoestrogen in women with perimenopausal depression. Menopause. 2021;28(4):369–83. https://doi.org/10.1097/GME.0000000000001724.
Cardona-Gómez GP, Mendez P, DonCarlos LL, Azcoitia I, Garcia-Segura LM. Interactions of estrogens and insulin-like growth factor-I in the brain: implications for neuroprotection. Brain Res Rev. 2001;37(1–3):320–34. https://doi.org/10.1016/S0165-0173(01)00137-0.
Hammar M, Christau S, Nathorst-Böös J, Rud T, Garre K. A double-blind, randomised trial comparing the effects of tibolone and continuous combined hormone replacement therapy in postmenopausal women with menopausal symptoms. Br J Obstet Gynaecol. 1998;105(8):904–11. https://doi.org/10.1111/j.1471-0528.1998.tb10237.x.
Kloosterboer HJ. Tissue-selectivity: the mechanism of action of tibolone. Maturitas. 2004;48(Suppl 1):S30-40. https://doi.org/10.1016/j.maturitas.2004.02.012.
Lello S, Capozzi A, Scambia G. The tissue-selective estrogen complex (bazedoxifene/conjugated estrogens) for the treatment of menopause. Int J Endocrinol. 2017;2017:5064725. https://doi.org/10.1155/2017/5064725.
Henderson VW, Sherwin BB. Surgical versus natural menopause: cognitive issues. Menopause May-Jun. 2007;14(3 Pt 2):572–9. https://doi.org/10.1097/gme.0b013e31803df49c.
Henderson VW, Guthrie JR, Dudley EC, Burger HG, Dennerstein L. Estrogen exposures and memory at midlife: a population-based study of women. Neurology. 2003;60(8):1369–71. https://doi.org/10.1212/01.WNL.0000059413.75888.BE.
Shanmugan S, Epperson CN. Estrogen and the prefrontal cortex: towards a new understanding of estrogen’s effects on executive functions in the menopause transition. Hum Brain Mapp. 2014;35(3):847–65. https://doi.org/10.1002/hbm.22218.
Epperson CN, Sammel MD, Freeman EW. Menopause effects on verbal memory: findings from a longitudinal community cohort. J Clin Endocrinol Metab. 2013;98(9):3829–38. https://doi.org/10.1210/jc.2013-1808.
Resnick SM, Henderson VW. Hormone therapy and risk of Alzheimer disease: a critical time. J Am Med Assoc. 2002;288(17):2170–2. https://doi.org/10.1001/jama.288.17.2170.
Harman SM, Brinton EA, Cedars M, Lobo R, Manson JE, Merriam GR, et al. KEEPS: the kronos early estrogen prevention study. Climacteric. 2005;8(1):3–12. https://doi.org/10.1080/13697130500042417.
Shumaker SA, Reboussin BA, Espeland MA, Rapp SR, McBee WL, Dailey M, et al. The women’s health initiative memory study (WHIMS): a trial of the effect of estrogen therapy in preventing and slowing the progression of dementia. Control Clin Trials. 1998;19(6):604–21. https://doi.org/10.1016/S0197-2456(98)00038-5.
Resnick SM, Coker LH, Maki PM, Rapp SR, Espeland MA, Shumakerb SA. The women’s health initiative study of cognitive aging (WHISCA): a randomized clinical trial of the effects of hormone therapy on age-associated cognitive decline. Clin Trials. 2004;1(5):440–50. https://doi.org/10.1191/1740774504cn040oa.
Sajatovic M, Friedman SH, Schuermeyer IN, Safavi R, Ignacio RV, Hays RW, et al. Menopause knowledge and subjective experience among peri- and postmenopausal women with bipolar disorder, schizophrenia and major depression. J Nerv Ment Dis. 2006;194(3):173–8. https://doi.org/10.1097/01.nmd.0000202479.00623.86.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Conflicts of interest
Megan Herson has no conflicts of interest to declare. Jayashri Kulkarni has no conflicts of interest to declare.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
MH performed most of the literature search and synthesised the review. JK developed the concept and performed editing and formulated responses to reviewers. Both authors reviewed and approved the final version.
Additional information
The original online version of this article was revised: The Open Access funding information was missed and published in the original version.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Herson, M., Kulkarni, J. Hormonal Agents for the Treatment of Depression Associated with the Menopause. Drugs Aging 39, 607–618 (2022). https://doi.org/10.1007/s40266-022-00962-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-022-00962-x