Abstract
Background
Deprescribing has been shown to reduce potentially inappropriate or unnecessary medications; however, whether these benefits translate into improved quality of life (QOL) is uncertain.
Objective
The objective of this study was to isolate the impact of deprescribing on patient or designated representative reported QOL; satisfaction with care (SWC) and emergency department (ED) visits and hospitalizations were also investigated to further explore this question.
Methods
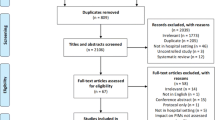
This systematic review searched the Cochrane Library, Cumulative Index to Nursing and Allied Health (CINAHL), MEDLINE, and EMBASE from database inception until November 2017. Randomized controlled trials and non-randomized prospective studies of older adults (> 65 years or older) and older persons with life-limiting conditions were included. Two reviewers independently assessed the search results and performed risk of bias assessments. Data on QOL, SWC, and ED visits and hospitalizations were extracted from all identified studies. Risk of bias of individual studies was assessed using measures recommended by the Cochrane Collaboration.
Results
Screening of 6543 eligible records identified 12 studies within 13 articles. In ten studies investigating the reduction of at least one medication deprescribed, compared with usual care, all but two found no difference in QOL. To date there has only been one study examining the impact of deprescribing on SWC, which was found to be not statistically significant. Four studies exploring the impact of deprescribing on ED visits and hospitalizations also found no significant difference. However, many studies were found to have a higher performance, detection, or other bias. We found considerable heterogeneity in patient populations, targeted medications for deprescribing, and QOL measurements used in these studies.
Conclusion
Based on a limited number of studies with varying methodological rigor, deprescribing may not significantly improve QOL or SWC; however, it may not contribute to additional ED visits and hospitalizations. Future controlled studies are needed.

Similar content being viewed by others
References
Saraf AA, Petersen AW, Simmons SF, et al. Medications associated with geriatric syndromes and their prevalence in older hospitalized adults discharged to skilled nursing facilities. J Hosp Med. 2016;11:694–700.
Morin L, Laroche ML, Texier G, Johnell K. Prevalence of potentially inappropriate medication use in older adults living in nursing homes: a systematic review. J Am Med Dir Assoc. 2016;17(862):e1–9.
Redston MR, Hilmer SN, McLachlan AJ, Clough AJ, Gnjidic D. Prevalence of potentially inappropriate medication use in older inpatients with and without cognitive impairment: a systematic review. J Alzheimers Dis. 2018;61:1639–52.
Harrison SL, O’Donnell LK, et al. Associations between the Drug Burden Index, potentially inappropriate medications and quality of life in residential aged care. Drugs Aging. 2018;35:83–91.
Marcum ZA, Gellad WF. Medication adherence to multidrug regimens. Clin Geriatr Med. 2012;28:287–300.
Pérez-Jover V, Mira JJ, Carratala-Munuera C, et al. Inappropriate use of medication by elderly, polymedicated, or multipathological patients with chronic diseases. Int J Environ Res Public Health. 2018;15(2):E310.
Eckerblad J, Theander K, Ekdahl A, et al. Symptom burden in community-dwelling older people with multimorbidity: a cross-sectional study. BMC Geriatr. 2015;15:1.
Deshields TL, Potter P, Olsen S, Liu J. The persistence of symptom burden: symptom experience and quality of life of cancer patients across one year. Support Care Cancer. 2014;22:1089–96.
Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175:827–34.
Thillainadesan J, Gnjidic D, Green S, Hilmer SN. Impact of deprescribing interventions in older hospitalised patients on prescribing and clinical outcomes: a systematic review of randomised trials. Drugs Aging. 2018;35:303–19.
Pruskowski J, Handler SM. The DE-PHARM Project: a pharmacist-driven deprescribing initiative in a nursing facility. Consult Pharm. 2017;32:468–78.
Wouters H, Scheper J, Koning H, et al. Discontinuing inappropriate medication use in nursing home residents: a cluster randomized controlled trial. Ann Intern Med. 2017;167:609–17.
Reeve E, To J, Hendrix I, Shakib S, Roberts MS, Wiese MD. Patient barriers to and enablers of deprescribing: a systematic review. Drugs Aging. 2013;30(10):793–807.
Stevenson J, Abernethy AP, Miller C, Currow DC. Managing comorbidities in patients at the end of life. BMJ. 2004;329:909–12.
Marcum ZA, Amuan ME, Hanlon JT, et al. Prevalence of unplanned hospitalizations caused by adverse drug reactions in older veterans. J Am Geriatr Soc. 2012;60:34–41.
Page AT, Clifford RM, Potter K, Schwartz D, Etherton-Beer CD. The feasibility and effect of deprescribing in older adults on mortality and health: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016;82:583–623.
Bandayrel K, Johnston BC. Recent advances in patient and proxy-reported quality of life research. Health Qual Life Outcomes. 2014;12:110.
Bladh L, Ottosson E, Karlsson J, Klintberg L, Wallerstedt SM. Effects of a clinical pharmacist service on health-related quality of life and prescribing of drugs: a randomised controlled trial. BMJ Qual Saf. 2011;20:738–46.
Gallagher PF, O’Connor MN, O’Mahony D. Prevention of potentially inappropriate prescribing for elderly patients: a randomized controlled trial using STOPP/START criteria. Clin Pharmacol Ther. 2011;89:845–54.
Gillespie U, Alassaad A, Hammarlund-Udenaes M, et al. Effects of pharmacists’ interventions on appropriateness of prescribing and evaluation of the instruments’ (MAI, STOPP and STARTs’) ability to predict hospitalization—analyses from a randomized controlled trial. PLoS One. 2013;8:e62401.
Spinewine A, Swine C, Dhillon S, et al. Effect of a collaborative approach on the quality of prescribing for geriatric inpatients: a randomized, controlled trial. J Am Geriatr Soc. 2007;55:658–65.
Van der Linden L, Decoutere L, Walgraeve K, et al. Combined use of the Rationalization of home medication by an Adjusted STOPP in older Patients (RASP) list and a pharmacist-led medication review in very old inpatients: impact on quality of prescribing and clinical outcome. Drugs Aging. 2017;34:123–33.
Institute of Medicine (US) Committee on Standards for Systematic Reviews of Comparative Effectiveness Research; Eden J, Levit L, Berg A, et al., editors. Finding what works in health care: standards for systematic reviews. Washington, DC: National Academies Press (US); 2011. https://doi.org/10.17226/13059. https://www.ncbi.nlm.nih.gov/books/NBK209518/. Accessed 23 Sept 2019.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65–94.
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Beer C, Loh PK, Peng YG, Potter K, Millar A. A pilot randomized controlled trial of deprescribing. Ther Adv Drug Saf. 2011;2:37–43.
Bergh S, Selbæk G, Engedal K. Discontinuation of antidepressants in people with dementia and neuropsychiatric symptoms (DESEP study): double blind, randomised, parallel group, placebo controlled trial. BMJ. 2012;344:e1566.
Bourgeois J, Elseviers MM, Van Bortel L, Petrovic M, Vander Stichele RH. Feasibility of discontinuing chronic benzodiazepine use in nursing home residents: a pilot study. Eur J Clin Pharmacol. 2014;70(10):1251–60.
Kutner JS, Blatchford PJ, Taylor DH Jr, et al. Safety and benefit of discontinuing statin therapy in the setting of advanced, life-limiting illness: a randomized clinical trial. JAMA Intern Med. 2015;175:691–700.
Lopez-Peig C, Mundet X, Casabella B, del Val JL, Lacasta D, Diogene E. Analysis of benzodiazepine withdrawal program managed by primary care nurses in Spain. BMC Res Notes. 2012;5:684.
Moonen JE, Foster-Dingley JC, de Ruijter W, et al. Effect of discontinuation of antihypertensive treatment in elderly people on cognitive functioning—the DANTE Study Leiden: a randomized clinical trial. JAMA Intern Med. 2015;175:1622–30.
Polinder S, Boyé ND, Mattace-Raso FU, et al. Cost-utility of medication withdrawal in older fallers: results from the Improving Medication Prescribing to reduce Risk Of FALLs (IMPROveFALL) trial. BMC Geriatr. 2016;16:179.
Potter K, Flicker L, Page A, Etherton-Beer C. Deprescribing in frail older people: a randomised controlled trial. PLoS One. 2016;11:e0149984.
Sakakibara M, Igarashi A, Takase Y, Kamei H, Nabeshima T. Effects of prescription drug reduction on quality of life in community-dwelling patients with dementia. J Pharm Pharm Sci. 2015;18:705–12.
Ulfvarson J, Adami J, Wredling R, Kjellman B, Reilly M, von Bahr C. Controlled withdrawal of selective serotonin reuptake inhibitor drugs in elderly patients in nursing homes with no indication of depression. Eur J Clin Pharmacol. 2003;59:735–40.
Boyé ND, van der Velde N, de Vries OJ, et al. Effectiveness of medication withdrawal in older fallers: results from the Improving Medication Prescribing to reduce Risk Of FALLs (IMPROveFALL) trial. Age Ageing. 2017;46:142–6.
Garfinkel D, Zur-Gil S, Ben-Israel J. The war against polypharmacy: a new cost-effective geriatric-palliative approach for improving drug therapy in disabled elderly people. Isr Med Assoc J. 2007;9:430–4.
Jondeau G, Neuder Y, Eicher JC, et al. B-CONVINCED: beta-blocker CONtinuation vs. INterruption in patients with Congestive heart failure hospitalizED for a decompensation episode. Eur Heart J. 2009;30:2186–92.
Cantril H. The pattern of human concerns. New Brunswick: Rutgers University Press; 1965.
Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–43.
Cohen SR, Mount BM, Strobel MG, Bui F. The McGill Quality of Life Questionnaire: a measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliat Med. 1995;9:207–19.
Torisson G, Stavenow L, Minthon L, Londos E. Reliability, validity and clinical correlates of the Quality of Life in Alzheimer’s disease (QoL-AD) scale in medical inpatients. Health Qual Life Outcomes. 2016;14:90.
Hagell P, Westergren A, Årestedt K. Beware of the origin of numbers: standard scoring of the SF-12 and SF-36 summary measures distorts measurement and score interpretations. Res Nurs Health. 2017;40:378–86.
Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:2050312116671725. https://doi.org/10.1177/2050312116671725.
Dills H, Shah K, Messinger-Rapport B, Bradford K, Syed Q. Deprescribing medications for chronic diseases management in primary care settings: a systematic review of randomized controlled trials. J Am Med Dir Assoc. 2018;19(923–935):e2.
Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in the elderly. Expert Opin Drug Saf. 2014;13(1):57–65.
Bain KT, Holmes HM, Beers MH, Maio V, Handler SM, Pauker SG. Discontinuing medications: a novel approach for revising the prescribing stage of the medication-use process. J Am Geriatr Soc. 2008;56(10):1946–52.
Lee M, Saver JL, Wu YL, et al. Utilization of statins beyond the initial period after stroke and 1-year risk of recurrent stroke. J Am Heart Assoc. 2017;6:e005658.
Reeve E, Wolff JL, Skehan M, Bayliss EA, Hilmer SN, Boyd CM. Assessment of attitudes towards deprescribing in older Medicare beneficiaries in the United States. JAMA Intern Med. 2018;178:1673–80.
Kuntz J, Kouch L, Christian D, Peterson PL, Gruss I. Barriers and facilitators to the deprescribing of nonbenzodiazepine sedative medications among older adults. Perm J. 2018;22:17–157.
Dou C, Rebane J, Bardal S. Intervention to improve benzodiazepine tapering success in the elderly: a systematic review. Aging Ment Health. 2018;16:1–6.
Payakachat N, Ali MM, Tilford JM. Can the EQ-5D detect meaningful change? A systematic review. Pharmacoeconomics. 2015;33:1137–54.
Glasziou P, Alexander J, Beller E, Clarke P. Which health-related quality of life score? A comparison of alternative utility measures in patients with type 2 diabetes in the ADVANCE trial. Health Qual Life Outcomes. 2007;5:21.
Tseng HM, Lee CH, Chen YJ, Hsu HH, Huang LY, Huang JL. Developing a measure of medication-related quality of life for people with polypharmacy. Qual Life Res. 2016;25:1295–302.
Thompson W, Reeve E, Moriarty F, et al. Deprescribing: future directions for research. Res Social Adm Pharm. 2019;15:801–5.
Mohammed MA, Moles RJ, Chen TF. Pharmaceutical care and health related quality of life outcomes over the past 25 years: have we measured dimensions that really matter? Int J Clin Pharm. 2018;40:3–14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jennifer A. Pruskowski, Carolyn T. Thorpe, Michele Klein-Fedyshin, and Steven M. Handler declare that they have no conflicts of interest. Sydney Springer’s work on this project was supported by the Department of Veterans Affairs, Office of Academic Affairs Fellowship in Medicare Safety & Pharmacy Outcomes. The views expressed are those of the authors and do not represent the views of the Department of Veterans Affairs.
Funding
The authors received no funding support for this work or to assist in the preparation of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pruskowski, J.A., Springer, S., Thorpe, C.T. et al. Does Deprescribing Improve Quality of Life? A Systematic Review of the Literature. Drugs Aging 36, 1097–1110 (2019). https://doi.org/10.1007/s40266-019-00717-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00717-1