Abstract
Background
The use of proton pump inhibitors (PPIs) in older adults is high, often inappropriate, and may cause harm. Deprescribing is defined as the reduction, withdrawal, or discontinuation of inappropriate medication.
Objective
We conducted a systematic review to determine the effectiveness of interventions to deprescribe inappropriate PPIs in older adults.
Methods
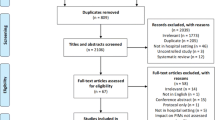
We searched MEDLINE, PubMed, Embase, the Cochrane Library, ProQuest Dissertations and Theses Global, and Google from inception to January 2017 for randomized and non-randomized studies describing the outcomes of interventions to deprescribe inappropriate PPIs in older adults (mean or median age of ≥65 years). Where available, clinically relevant outcomes were also assessed.
Results
We included 21 articles in our review. Six studies demonstrated effective interventions, 11 were inconclusive, and four were ineffective. Effective interventions included a population-wide education and promotion strategy, academic detailing for general practitioners, and inpatient geriatrician-led deprescribing. Methodological issues limited the interpretation of several studies. Standardization in outcome reporting was lacking, and clinical outcome data were absent. A comparison of intervention effectiveness was not possible because of their heterogeneity, which precluded a meta-analysis.
Conclusion
The limited available evidence suggests that some strategies are more successful than others in effectively deprescribing inappropriate PPIs in older adults. However, whether PPI deprescribing translates into better clinical outcomes remains unclear.

Similar content being viewed by others
References
Fox RK, Muniraj T. Pharmacologic therapies in gastrointestinal diseases. Med Clin N Am. 2016;100:827–50.
Poynard T, Lemaire M, Agostini H. Meta-analysis of randomized clinical trials comparing lansoprazole with ranitidine or famotidine in the treatment of acute duodenal ulcer. Eur J Gastroenterol Hepatol. 1995;7:661–5.
Chan WH, Khin LW, Chung YFA, Goh YC, Ong HS, Wong WK. Randomized controlled trial of standard versus high-dose intravenous omeprazole after endoscopic therapy in high-risk patients with acute peptic ulcer bleeding. Br J Surg. 2011;98:640–4.
Sigterman KE, van Pinxteren B, Bonis PA, Lau J, Numans ME. Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux disease-like symptoms and endoscopy negative reflux disease. Cochrane Database Syst Rev. 2013;(5):CD002095.
Swarbrick ET, Gough AL, Foster CS, Christian J, Garrett AD, Langworthy CH. Prevention of recurrence of oesophageal stricture, a comparison of lansoprazole and high-dose ranitidine. Eur J Gastroenterol Hepatol. 1996;8:431–8.
PBS Information Management Section Pharmaceutical Policy Branch. Expenditure and prescriptions twelve months to 30 June 2014. Canberra: Australian Government; 2014.
PBS Information Management Section Pharmaceutical Policy Branch. Expenditure and prescriptions twelve months to 30 June 2015. Canberra: Australian Government; 2015.
Othman F, Card TR, Crooks CJ. Proton pump inhibitor prescribing patterns in the UK: a primary care database study. Pharmacoepidemiol Drug Saf. 2016;25:1079–87.
Pottegard A, Broe A, Hallas J, de Muckadell OBS, Lassen AT, Lodrup AB. Use of proton-pump inhibitors among adults: a Danish nationwide drug utilization study. Therap Adv Gastroenterol. 2016;9:671–8.
Wallerstedt SM, Fastbom J, Linke J, Vitols S. Long-term use of proton pump inhibitors and prevalence of disease- and drug-related reasons for gastroprotection-a cross-sectional population-based study. Pharmacoepidemiol Drug Saf. 2016;6:188–91.
Gastrointestinal (version 6). eTG Complet [internet]. Melbourne: Therapeutic Guidelines Limited; 2016.
Boghossian TA, Rashid Farah J, Welch V, Rojas-Fernandez C, Moayyedi P, Pottie K, et al. Deprescribing versus continuation of chronic proton pump inhibitor use in adults (Protocol). Cochrane Database Syst Rev. 2015;(11):CD011969. doi:10.1002/14651858.CD011969.
Gastroenterological Society of Australia. Gastro-oesophageal reflux disease in adults. 5th ed. Mulgrave: Digestive Health Foundation; 2011.
National Institute for Health and Care Excellence. Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management. London: NICE; 2014.
Gadzhanova SV, Roughead EE, Mackson JM. Initiation and duration of proton pump inhibitors in the Australian veteran population. Intern Med J. 2012;42:e68–73.
Heidelbaugh JJ, Kim AH, Chang R, Walker PC. Overutilization of proton-pump inhibitors: what the clinician needs to know. Ther Adv Gastroenterol. 2012;5:219–32.
Ahrens D, Chenot J-F, Behrens G, Grimmsmann T, Kochen MM. Appropriateness of treatment recommendations for PPI in hospital discharge letters. Eur J Clin Pharmacol. 2010;66:1265–71.
Anderson K, Stowasser D, Freeman C, Scott I. Prescriber barriers and enablers to minimising potentially inappropriate medications in adults: a systematic review and thematic synthesis. BMJ Open. 2014;4:e006544.
Schoenfeld AJ, Grady D. Adverse effects associated with proton pump inhibitors. JAMA Intern Med. 2016;176:172–4.
Masclee GMC, Sturkenboom MCJM, Kuipers EJ. A benefit-risk assessment of the use of proton pump inhibitors in the elderly. Drugs Aging. 2014;31:263–82.
Gomm W, von Holt K, Thomé F, Broich K, Maier W, Fink A, et al. Association of proton pump inhibitors with risk of dementia: a pharmacoepidemiological claims data analysis. JAMA Neurol. 2016;73:410–6.
Alhawassi T, Bajorek B, Krass I, Pont LG. A systematic review of the prevalence and risk factors for adverse drug reactions in the elderly in the acute care setting. Clin Interv Aging. 2014;9:2079–86.
Maggio M, Corsonello A, Ceda G, Cattabiani C, Lauretani F, Butto V, et al. Proton pump inhibitors and risk of 1-year mortality and rehospitalization in older patients discharged from acute care hospitals. J Am Med Assoc Intern Med. 2013;173:518–23.
Juurlink DN, Gomes T, Ko DT, Szmitko PE, Austin PC, Tu JV, et al. A population-based study of the drug interaction between proton pump inhibitors and clopidogrel. Can Med Assoc J. 2009;180:713–8.
Bhatt DL, Cryer BL, Contant CF, Cohen M, Lanas A, Schnitzer TJ, et al. Clopidogrel with or without omeprazole in coronary artery disease. N Engl J Med. 2010;363:1909–17.
Yepuri G, Sukhovershin R, Nazari-Shafti TZ, Petrascheck M, Ghebre YT, Cooke JP. Proton pump inhibitors accelerate endothelial senescence. Circ Res. 2016;118:e36–42.
Reeve E, Gnjidic D, Long J, Hilmer S. A systematic review of the emerging definition of ‘deprescribing’ with network analysis: implications for future research and clinical practice. Br J Clin Pharmacol. 2015;80:1254–68.
Haastrup P, Paulsen MS, Begtrup LM, Hansen JM, Jarbøl DE. Strategies for discontinuation of proton pump inhibitors: a systematic review. Fam Pract. 2014;31:625–30.
Lødrup AB, Reimer C, Bytzer P. Systematic review: symptoms of rebound acid hypersecretion following proton pump inhibitor treatment. Scand J Gastroenterol. 2013;48:515–22.
Farrell B, Tsang C, Raman-Wilms L, Irving H, Conklin J, Pottie K. What are priorities for deprescribing for elderly patients? Capturing the voice of practitioners: a modified delphi process. PLoS One. 2015;10:e0122246.
Reeve E, To J, Hendrix I, Shakib S, Roberts MS, Wiese MD. Patient barriers to and enablers of deprescribing: a systematic review. Drugs Aging. 2013;30:793–807.
Higgins JP, Altman DG, Sterne JA, editors. Chapter 8: assessing risk of bias in included studies. In: Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration; 2011.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84.
Atkins R, Smith L. Impact of pharmacy intervention on the use of proton-pump inhibitors in the hospital setting. Consult Pharm. 2013;28:786–92.
Batuwitage BT, Kingham JGC, Morgan NE, Bartlett RL. Inappropriate prescribing of proton pump inhibitors in primary care. Postgrad Med J. 2007;83:66–8.
Hamzat H, Sun H, Ford JC, Macleod J, Soiza RL, Mangoni AA. Inappropriate prescribing of proton pump inhibitors in older patients: effects of an educational strategy. Drugs Aging. 2012;29:681–90.
Lampen-Smith A, Young J, O’Rourke MA, Balram A, Inns S. Blinded randomised controlled study of the effect of a discharge communication template on proton pump inhibitor prescribing. N Z Med J. 2012;125:30–6.
Pratt NL, Kalisch Ellett LM, Sluggett JK, Gadzhanova SV, Ramsay EN, Kerr M, et al. Use of proton pump inhibitors among older Australians: national quality improvement programmes have led to sustained practice change. Int J Qual Health Care. 2016. doi:10.1093/intqhc/mzw138.
Reeve E, Andrews JM, Wiese MD, Hendrix I, Roberts MS, Shakib S. Feasibility of a patient-centered deprescribing process to reduce inappropriate use of proton pump inhibitors. Ann Pharmacother. 2015;49:29–38.
Roughead EE, Kalisch Ellett LM, Ramsay EN, Pratt NL, Barratt JD, LeBlanc VT, et al. Bridging evidence-practice gaps: improving use of medicines in elderly Australian veterans. BMC Health Serv Res. 2013;13:514.
Brulhart MI, Wermeille JP. Multidisciplinary medication review: evaluation of a pharmaceutical care model for nursing homes. Int J Clin Pharm. 2011;33:549–57.
Clyne B, Smith SM, Hughes CM, Boland F, Bradley MC, Cooper JA, et al. Effectiveness of a multifaceted intervention for potentially inappropriate prescribing in older patients in primary care: a cluster-randomized controlled trial (OPTI-SCRIPT Study). Ann Fam Med. 2015;13:545–53.
Clyne B, Smith SM, Hughes CM, Boland F, Cooper JA, Fahey T, et al. Sustained effectiveness of a multifaceted intervention to reduce potentially inappropriate prescribing in older patients in primary care (OPTI-SCRIPT study). Implement Sci. 2016;11:79.
Frely A, Chazard E, Pansu A, Beuscart JB, Puisieux F. Impact of acute geriatric care in elderly patients according to the Screening Tool of Older Persons’ Prescriptions/Screening Tool to Alert doctors to Right Treatment criteria in northern France. Geriatr Gerontol Int. 2016;16:272–8.
Garfinkel D, Mangin D. Feasibility study of a systematic approach for discontinuation of multiple medications in older adults: addressing polypharmacy. Arch Intern Med. 2010;170:1648–54.
Khunti K, Kinsella B. Effect of systematic review of medication by general practitioner on drug consumption among nursing-home residents. Age Ageing. 2000;29:451–3.
Lang PO, Vogt-Ferrier N, Hasso Y, Le Saint L, Drame M, Zekry D, et al. Interdisciplinary geriatric and psychiatric care reduces potentially inappropriate prescribing in the hospital: interventional study in 150 acutely ill elderly patients with mental and somatic comorbid conditions. J Am Med Dir Assoc. 2012;13:406.e1–7.
Michalek C, Wehling M, Schlitzer J, Frohnhofen H. Effects of ‘Fit fOR The Aged’ (FORTA) on pharmacotherapy and clinical endpoints–a pilot randomized controlled study. Eur J Clin Pharmacol. 2014;70:1261–7.
Mudge A, Radnedge K, Kasper K, Mullins R, Rofail S, Adsett J, et al. Effects of a pilot multidisciplinary clinic for frequent attending elderly patients on deprescribing. Aust Health Rev. 2016;40:86–91.
Mulvogue K, Roberts JA, Coombes I, Cottrell N, Kanagarajah S, Smith A. The effect of pharmacists on ward rounds measured by the STOPP/START tool in a specialized geriatric unit. J Clin Pharm Ther. 2016. doi:10.1111/jcpt.12489.
Potter K, Flicker L, Page A, Etherton-Beer C. Deprescribing in frail older people: a randomised controlled trial. PLoS One. 2016;11:e0149984.
Teichert M, Luijben SN, Wereldsma A, Schalk T, Janssen J, Wensing M, et al. Implementation of medication reviews in community pharmacies and their effect on potentially inappropriate drug use in elderly patients. Int J Clin Pharm. 2013;35:719–26.
Urfer M, Elzi L, Dell-Kuster S, Bassetti S. Intervention to improve appropriate prescribing and reduce polypharmacy in elderly patients admitted to an internal medicine unit. PLoS One. 2016;11:e0166359.
Wehling M, Burkhardt H, Kuhn-Thiel A, Pazan F, Throm C, Weiss C, et al. VALFORTA: a randomised trial to validate the FORTA (Fit fOR The Aged) classification. Age Ageing. 2016;45:262–7.
Acknowledgements
The authors acknowledge Raechel Damarell (Medical Librarian, Flinders University) for her assistance in the design of our search strategy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was used in the preparation of this manuscript
Conflict of interest
TW, IH, TT, and AM have no conflicts of interest in relation to this manuscript.
Additional information
The original version of this article was revised: Author affiliation was incorrectly published in the original version and it has been updated.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wilsdon, T.D., Hendrix, I., Thynne, T.R.J. et al. Effectiveness of Interventions to Deprescribe Inappropriate Proton Pump Inhibitors in Older Adults. Drugs Aging 34, 265–287 (2017). https://doi.org/10.1007/s40266-017-0442-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-017-0442-1