Abstract
Background
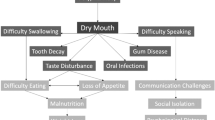
Over three-quarters of the older population take medications that can potentially cause dry mouth. Physicians or pharmacists rarely inform patients about this adverse effect and its potentially severe damage to the teeth, mouth and general health.
Objectives
The objectives of this study were to (1) identify warnings in the literature about dry mouth associated with the most frequently prescribed pharmaceutical products in Canada; and (2) consider how this information might be obtained by physicians, pharmacists and patients.
Methods
Monographs on the 72 most frequently prescribed medications during 2010 were retrieved from the Compendium of Pharmaceuticals and Specialties (CPS, a standard drug information reference for physicians and pharmacists), the National Library of Medicine’s ‘DailyMed’ database, directly from the manufacturers, and from a systematic search of biomedical journals.
Results
The CPS provided monographs for 43 % of the medications, and requests to manufacturers produced the remaining monographs. Mentions of dry mouth were identified in 61 % of the products (43 % amongst CPS monographs; an additional 43 % amongst manufacturers’ monographs; 7 % in the DailyMed database and 7 % from biomedical journals); five medications had contradictory reports in different monographs.
Conclusion
Nearly two-thirds (61 %) of the most commonly prescribed medications can cause dry mouth, yet warnings about this adverse effect and its potentially serious consequences are not readily available to physicians, pharmacists, dentists or patients.
Similar content being viewed by others
References
Shinozaki S, Moriyama M, Hayashida JN, Tanaka A, Maehara T, Ieda S, et al. Close association between oral Candida species and oral mucosal disorders in patients with xerostomia. Oral Dis. 2012;18(7):667–72. doi:10.1111/j.1601-0825.2012.01923.x.
Hopcraft MS, Tan C. Xerostomia: an update for clinicians. Aust Dental J. 2010;55(3):238–44, quiz 353. doi:10.1111/j.1834-7819.2010.01229.x.
Thomson WM, Ikebe K, Tordoff JM, Campbell AJ. Dry mouth and medications. In: MacEntee MI, Muller F, Wyatt CC, editors. Oral healthcare and the frail elder: a clinical perspective. Ames: Wiley-Blackwell Publishing Ltd; 2010. p. 51–71.
Dodds MW, Johnson DA, Yeh CK. Health benefits of saliva: a review. J Dent. 2005;33(3):223–33. doi:10.1016/j.jdent.2004.10.009.
Mese H, Matsuo R. Salivary secretion, taste and hyposalivation. J Oral Rehabil. 2007;34(10):711–23. doi:10.1111/j.1365-2842.2007.01794.x.
Turner MD, Ship JA. Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc. 2007;138(Suppl):15S–20S.
Niedermeier WH, Kramer R. Salivary secretion and denture retention. J Prosthet Dent. 1992;67(2):211–6.
Scully C, Sonis S, Diz PD. Oral mucositis. Oral Dis. 2006;12(3):229–41. doi:10.1111/j.1601-0825.2006.01258.x.
Strömberg E, Hagman-Gustafsson ML, Holmén A, Wårdh I, Gabre P. Oral status, oral hygiene habits and caries risk factors in home-dwelling elderly dependent on moderate or substantial supportive care for daily living. Community Dent Oral Epidemiol. 2012;40(3):221–9. doi:10.1111/j.1600-0528.2011.00653.x.
Awano S, Ansai T, Takata Y, Soh I, Akifusa S, Hamasaki T, et al. Oral health and mortality risk from pneumonia in the elderly. J Dental Res. 2008;87(4):334–9.
Orellana MF, Lagravère MO, Boychuk DG, Major PW, Flores-Mir C. Prevalence of xerostomia in population-based samples: a systematic review. J Public Health Dent. 2006;66(2):152–8.
Kandelman D, Petersen PE, Ueda H. Oral health, general health, and quality of life in older people. Spec Care Dentist. 2008;28(6):224–36. doi:10.1111/j.1754-4505.2008.00045.x.
Nagler RM, Hershkovich O. Age-related changes in unstimulated salivary function and composition and its relations to medications and oral sensorial complaints. Aging Clin Exp Res. 2005;17(5):358–66.
Leal SC, Bittar J, Portugal A, Falcão DP, Faber J, Zanotta P. Medication in elderly people: its influence on salivary pattern, signs and symptoms of dry mouth. Gerodontology. 2010;27(2):129–33. doi:10.1111/j.1741-2358.2009.00293.x.
Nederfors T. Xerostomia and hyposalivation. Adv Dental Res. 2000;14:48–56.
MacEntee MI, Thorne S, Kazanjian A. Conflicting priorities: oral health in long-term care. Spec Care Dentist. 1999;19(4):164–72.
Andersson K, Furhoff AK, Nordenram G, Wårdh I. ‘Oral health is not my department’. Perceptions of elderly patients’ oral health by general medical practitioners in primary health care centres: a qualitative interview study. Scand J Caring Sci. 2007;21(1):126–33. doi:10.1111/j.1471-6712.2007.00446.x.
Jones RN, Masterton R. Determining the value of antimicrobial surveillance programs. Diagn Microbiol Infect Dis. 2001;41(4):171–5.
Erwin ME, Fix AM, Jones RN. Three independent yearly analyses of the spectrum and potency of metronidazole: a multicenter study of 1,108 contemporary anaerobic clinical isolates. Diagn Microbiol Infect Dis. 2001;39(2):129–32.
Ship JA, Nolan NE, Puckett SA. Longitudinal analysis of parotid and submandibular salivary flow rates in healthy, different-aged adults. J Gerontol Ser A Biol Sci Med Sci. 1995;50(5):M285–9.
von Gunten CF. Interventions to manage symptoms at the end of life. J Palliat Med. 2005;8(Suppl 1):S88–94. doi:10.1089/jpm.2005.8.s-88.
Hamilton HJ, Gallagher PF, O’Mahony D. Inappropriate prescribing and adverse drug events in older people. BMC Geriatr. 2009;9:5. doi:10.1186/1471-2318-9-5.
Institute of Medicine. Health IT and patient safety: building safer systems for better care. Washington DC: National Academies Press; Winterstein. Available from: http://site.ebrary.com/lib/ubc/docDetail.action?docID=10557783. Accessed 8 Oct 2013
Patel I, Balkrishnan R. Medication error management around the globe: an overview. Indian J Pharm Sci. 2010;72(5):539–45. doi:10.4103/0250-474X.78518.
Orser B. Reducing medication errors. CMAJ. 2000;162(8):1150–1.
Campeau L. Top Rx drugs of 2010. Pharmacy Practice; 2011. p. 40–6.
Repchinsky C, editor. Compendium of pharmaceuticals and specialties. Ottawa: Canadian Pharmacists Association; 2011.
e-Therapeutics. e-CPS. Canadian Pharmacists Association; 2011. Available from: http://www.e-therapeutics.ca/cps.showMonograph.action.
DailyMed. US National Library of Medicine; 2012. Available from: http://dailymed.nlm.nih.gov/dailymed/about.cfm.
Atkinson JC, Shiroky JB, Macynski A, Fox PC. Effects of furosemide on the oral cavity. Gerodontology. 1989;8(1):23–6.
Hackett D, Parks V, Salinas E, editors. Open-label evaluation of once-daily venlafaxine XR. European College of Neuropsychopharmacology; 1997.
Allgulander C, Hackett D, Salinas E. Venlafaxine extended release (ER) in the treatment of generalised anxiety disorder: twenty-four-week placebo-controlled dose-ranging study. Br J Psychiatry. 2001;179:15–22.
Allard P, Gram L, Timdahl K, Behnke K, Hanson M, Sogaard J. Efficacy and tolerability of venlafaxine in geriatric outpatients with major depression: a double-blind, randomised 6-month comparative trial with citalopram. Int J Geriatr Psychiatry. 2004;19(12):1123–30. doi:10.1002/gps.1190.
Gelenberg AJ, Lydiard RB, Rudolph RL, Aguiar L, Haskins JT, Salinas E. Efficacy of venlafaxine extended-release capsules in nondepressed outpatients with generalized anxiety disorder: a 6-month randomized controlled trial. JAMA. 2000;283(23):3082–8.
Guelfi JD, Ansseau M, Timmerman L, Korsgaard S. Mirtazapine versus venlafaxine in hospitalized severely depressed patients with melancholic features. J Clin Psychopharmacol. 2001;21(4):425–31.
Katzman M. Venlafaxine in the treatment of anxiety disorders. Expert Rev Neurother. 2004;4(3):371–81. doi:10.1586/14737175.4.3.371.
Sindrup SH, Bach FW, Madsen C, Gram LF, Jensen TS. Venlafaxine versus imipramine in painful polyneuropathy: a randomized, controlled trial. Neurology. 2003;60(8):1284–9.
Kulkarni S, Tripathi S, Mehta PD, Lodhi NS, Sengar NPS. Esomeprazole in the treatment of acidic disorder: an overview. Asian J Biochem Pharm Res. 2011;1(2):562–6.
Van Zwieten PA. Centrally acting antihypertensive drugs: present and future. Clin Exp Hypertens. 1999;21(5–6):859–73.
Gallagher L, Naidoo P. Prescription drugs and their effects on swallowing. Dysphagia. 2009;24(2):159–66. doi:10.1007/s00455-008-9187-7.
Baldwin CM, Keam SJ. Rabeprazole: a review of its use in the management of gastric acid-related diseases in adults. Drugs. 2009;69(10):1373–401. doi:10.2165/00003495-200969100-00007.
Dadabhai A, Friedenberg FK. Rabeprazole: a pharmacologic and clinical review for acid-related disorders. Expert Opinion Drug Saf. 2009;8(1):119–26. doi:10.1517/14740330802622892.
Battaglia J, Moss S, Rush J, Kang J, Mendoza R, Leedom L, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective, double-blind, emergency department study. Am J Emerg Med. 1997;15(4):335–40.
Gimbel JS, Brugger A, Zhao W, Verburg KM, Geis GS. Efficacy and tolerability of celecoxib versus hydrocodone/acetaminophen in the treatment of pain after ambulatory orthopedic surgery in adults. Clin Ther. 2001;23(2):228–41.
Reuben SS, Buvanendran A, Kroin JS, Raghunathan K. The analgesic efficacy of celecoxib, pregabalin, and their combination for spinal fusion surgery. Anesth Analg. 2006;103(5):1271–7. doi:10.1213/01.ane.0000237279.08847.2d.
Martin-Piedra MA, Aguilar-Salvatierra A, Herrera D, Gomez-Moreno G. Effectiveness of recent topical sialogogue in the management of drug-induced xerostomia. J Clin Exp Dent. 2011;3(4):e268–73.
Koylan N, Acarturk E, Canberk A, Caglar N, Caglar S, Erdine S, et al. Effect of irbesartan monotherapy compared with ACE inhibitors and calcium-channel blockers on patient compliance in essential hypertension patients: a multicenter, open-labeled, three-armed study. Blood Pressure Suppl. 2005;1:23–31.
Gimbel JS, Richards P, Portenoy RK. Controlled-release oxycodone for pain in diabetic neuropathy: a randomized controlled trial. Neurology. 2003;60(6):927–34.
Ong SB, Lee CT. A double-blind comparison of nomifensine and amitriptyline in the treatment of depression. Acta Psychiatr Scand. 1981;63(3):198–207.
van Ophoven A, Hertle L. Long-term results of amitriptyline treatment for interstitial cystitis. J Urol. 2005;174(5):1837–40.
Penttila J, Syvalahti E, Hinkka S, Kuusela T, Scheinin H. The effects of amitriptyline, citalopram and reboxetine on autonomic nervous system: a randomised placebo-controlled study on healthy volunteers. Psychopharmacology. 2001;154(4):343–9.
Young JP, Coleman A, Lader MH. A controlled comparison of fluoxetine and amitriptyline in depressed out-patients. Br J Psychiatry. 1987;151:337–40.
Kaur H, Hota D, Bhansali A, Dutta P, Bansal D, Chakrabarti A. A comparative evaluation of amitriptyline and duloxetine in painful diabetic neuropathy: a randomized, double-blind, cross-over clinical trial. Diabetes Care. 2011;34(4):818–22. doi:10.2337/dc10-1793.
Joubert PH, Starke DD, Van Reenen O, Venter CP. A comparison of the cardiovascular effects and subjective tolerability of binedaline and amitriptylene in healthy volunteers. Eur J Clin Pharmacol. 1985;27(6):667–70.
Rintala DH, Holmes SA, Courtade D, Fiess RN, Tastard LV, Loubser PG. Comparison of the effectiveness of amitriptyline and gabapentin on chronic neuropathic pain in persons with spinal cord injury. Arch Phys Med Rehabil. 2007;88(12):1547–60. doi:10.1016/j.apmr.2007.07.038.
Watson CP, Vernich L, Chipman M, Reed K. Nortriptyline versus amitriptyline in postherpetic neuralgia: a randomized trial. Neurology. 1998;51(4):1166–71.
Fridrich P, Colvin HP, Zizza A, Wasan AD, Lukanich J, Lirk P, et al. Phase 1A safety assessment of intravenous amitriptyline. J Pain. 2007;8(7):549–55. doi:10.1016/j.jpain.2007.02.433.
Pezzella G, Moslinger-Gehmayr R, Contu A. Treatment of depression in patients with breast cancer: a comparison between paroxetine and amitriptyline. Breast Cancer Res Treatment. 2001;70(1):1–10.
Bulut S, Berilgen MS, Baran A, Tekatas A, Atmaca M, Mungen B. Venlafaxine versus amitriptyline in the prophylactic treatment of migraine: randomized, double-blind, crossover study. Clin Neurol Neurosurg. 2004;107(1):44–8. doi:10.1016/j.clineuro.2004.03.004.
Tanser PH, Campbell LM, Carranza J, Karrash J, Toutouzas P, Watts R. Candesartan cilexetil is not associated with cough in hypertensive patients with enalapril-induced cough. Multicentre Cough Study Group. Am J Hypertens. 2000;13(2):214–8.
Koenig W. Comparison of the efficacy and tolerability of combination tablets containing candesartan cilexetil and hydrochlorothiazide or losartan and hydrochlorothiazide in patients with moderate to severe hypertension: results of the CARLOS-study. Clin Drug Investig. 2000;19(4):239–46.
Arnold LM, Russell IJ, Diri EW, Duan WR, Young JP Jr, Sharma U, et al. A 14-week, randomized, double-blinded, placebo-controlled monotherapy trial of pregabalin in patients with fibromyalgia. J Pain. 2008;9(9):792–805. doi:10.1016/j.jpain.2008.03.013.
Mease PJ, Russell IJ, Arnold LM, Florian H, Young JP Jr, Martin SA, et al. A randomized, double-blind, placebo-controlled, phase III trial of pregabalin in the treatment of patients with fibromyalgia. J Rheumatol. 2008;35(3):502–14.
Semel D, Murphy TK, Zlateva G, Cheung R, Emir B. Evaluation of the safety and efficacy of pregabalin in older patients with neuropathic pain: results from a pooled analysis of 11 clinical studies. BMC Fam Pract. 2010;11:85. doi:10.1186/1471-2296-11-85.
Tzellos TG, Toulis KA, Goulis DG, Papazisis G, Zampeli VA, Vakfari A, et al. Gabapentin and pregabalin in the treatment of fibromyalgia: a systematic review and a meta-analysis. J Clin Pharm Ther. 2010;35(6):639–56. doi:10.1111/j.1365-2710.2009.01144.x.
Marencak J, Cossons NH, Darekar A, Mills IW. Investigation of the clinical efficacy and safety of pregabalin alone or combined with tolterodine in female subjects with idiopathic overactive bladder. Neurourol Urodyn. 2011;30(1):75–82. doi:10.1002/nau.20928.
Crofford LJ, Rowbotham MC, Mease PJ, Russell IJ, Dworkin RH, Corbin AE, et al. Pregabalin for the treatment of fibromyalgia syndrome: results of a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2005;52(4):1264–73. doi:10.1002/art.20983.
Dworkin RH, Corbin AE, Young JP Jr, Sharma U, LaMoreaux L, Bockbrader H, et al. Pregabalin for the treatment of postherpetic neuralgia: a randomized, placebo-controlled trial. Neurology. 2003;60(8):1274–83.
Rickels K, Pollack MH, Feltner DE, Lydiard RB, Zimbroff DL, Bielski RJ, et al. Pregabalin for treatment of generalized anxiety disorder: a 4-week, multicenter, double-blind, placebo-controlled trial of pregabalin and alprazolam. Arch General Psychiatry. 2005;62(9):1022–30. doi:10.1001/archpsyc.62.9.1022.
Mittal M, Pasnoor M, Mummaneni RB, Khan S, McVey A, Saperstein D, et al. Retrospective chart review of duloxetine and pregabalin in the treatment of painful neuropathy. Int J Neurosci. 2011;121(9):521–7. doi:10.3109/00207454.2011.582238.
Zaccara G, Gangemi P, Perucca P, Specchio L. The adverse event profile of pregabalin: a systematic review and meta-analysis of randomized controlled trials. Epilepsia. 2011;52(4):826–36. doi:10.1111/j.1528-1167.2010.02966.x.
Nederfors T, Dahlof C. Effects on salivary flow rate and composition of withdrawal of and re-exposure to the beta 1-selective antagonist metoprolol in a hypertensive patient population. Eur J Oral Sci. 1996;104(3):262–8.
Liberali S. Oral impact of gastro-oesophageal reflux disease: a case report. Aust Dental J. 2008;53(2):176–9. doi:10.1111/j.1834-7819.2008.00029.x.
Dong Z, Wang Z, Yang K, Liu Y, Gao W, Chen W. Tamsulosin versus terazosin for benign prostatic hyperplasia: a systematic review. Syst Biol Reprod Med. 2009;55(4):129–36. doi:10.3109/19396360902833235.
Lee E, Lee C. Clinical comparison of selective and non-selective alpha 1A-adrenoreceptor antagonists in benign prostatic hyperplasia: studies on tamsulosin in a fixed dose and terazosin in increasing doses. Br J Urology. 1997;80(4):606–11.
Hoschl C, Svestka J. Escitalopram for the treatment of major depression and anxiety disorders. Expert Rev Neurother. 2008;8(4):537–52. doi:10.1586/14737175.8.4.537.
Bose A, Li D, Gandhi C. Escitalopram in the acute treatment of depressed patients aged 60 years or older. Am J Geriatr Psychiatry. 2008;16(1):14–20. doi:10.1097/JGP.0b013e3181591c09.
Rabinowitz I, Baruch Y, Barak Y. High-dose escitalopram for the treatment of obsessive-compulsive disorder. Int Clin Psychopharmacol. 2008;23(1):49–53. doi:10.1097/YIC.0b013e3282f0f0c5.
Pigott TA, Prakash A, Arnold LM, Aaronson ST, Mallinckrodt CH, Wohlreich MM. Duloxetine versus escitalopram and placebo: an 8-month, double-blind trial in patients with major depressive disorder. Curr Med Res Opin. 2007;23(6):1303–18. doi:10.1185/030079907X188107.
Nierenberg AA, Greist JH, Mallinckrodt CH, Prakash A, Sambunaris A, Tollefson GD, et al. Duloxetine versus escitalopram and placebo in the treatment of patients with major depressive disorder: onset of antidepressant action, a non-inferiority study. Curr Med Res Opin. 2007;23(2):401–16. doi:10.1185/030079906X167453.
Van Gerwen F, Van der Korst JK, Gribnau FW. Double-blind trial of naproxen and phenylbutazone in ankylosing spondylitis. Ann Rheum Dis. 1978;37(1):85–8.
Gross NJ. Tiotropium bromide. Chest. 2004;126(6):1946–53. doi:10.1378/chest.126.6.1946.
Tonnel AB, Perez T, Grosbois JM, Verkindre C, Bravo ML, Brun M. Effect of tiotropium on health-related quality of life as a primary efficacy endpoint in COPD. Int J Chron Obstruct Pulmon Dis. 2008;3(2):301–10.
Freeman D, Lee A, Price D. Efficacy and safety of tiotropium in COPD patients in primary care: the SPiRiva Usual CarE (SPRUCE) study. Resp Res. 2007;8:45. doi:10.1186/1465-9921-8-45.
Kesten S, Jara M, Wentworth C, Lanes S. Pooled clinical trial analysis of tiotropium safety. Chest. 2006;130(6):1695–703. doi:10.1378/chest.130.6.1695.
Saberi F, O’Donnell DE. The role of tiotropium bromide, a long-acting anticholinergic bronchodilator, in the management of COPD. Treat Resp Med. 2005;4(4):275–81.
Keating GM. Tiotropium bromide inhalation powder: a review of its use in the management of chronic obstructive pulmonary disease. Drugs. 2012;72(2):273–300. doi:10.2165/11208620-000000000-00000.
Koumis T, Samuel S. Tiotropium bromide: a new long-acting bronchodilator for the treatment of chronic obstructive pulmonary disease. Clin Ther. 2005;27(4):377–92. doi:10.1016/j.clinthera.2005.04.006.
Barr RG, Bourbeau J, Camargo CA, Ram FS. Tiotropium for stable chronic obstructive pulmonary disease: a meta-analysis. Thorax. 2006;61(10):854–62. doi:10.1136/thx.2006.063271.
Olin JL. Tiotropium: an inhaled anticholinergic for chronic obstructive pulmonary disease. Am J Health Syst Pharm. 2005;62(12):1263–9.
Vincken W, van Noord JA, Greefhorst AP, Bantje TA, Kesten S, Korducki L, et al. Improved health outcomes in patients with COPD during 1 yr’s treatment with tiotropium. Eur Resp J. 2002;19(2):209–16.
Nardi AE, Freire RC, Mochcovitch MD, Amrein R, Levitan MN, King AL, et al. A randomized, naturalistic, parallel-group study for the long-term treatment of panic disorder with clonazepam or paroxetine. J Clin Psychopharmacol. 2012;32(1):120–6. doi:10.1097/JCP.0b013e31823fe4bd.
Nardi AE, Freire RC, Valenca AM, Amrein R, de Cerqueira AC, Lopes FL, et al. Tapering clonazepam in patients with panic disorder after at least 3 years of treatment. J Clin Psychopharmacol. 2010;30(3):290–3. doi:10.1097/JCP.0b013e3181dcb2f3.
Gremeau-Richard C, Woda A, Navez ML, Attal N, Bouhassira D, Gagnieu MC, et al. Topical clonazepam in stomatodynia: a randomised placebo-controlled study. Pain. 2004;108(1–2):51–7. doi:10.1016/j.pain.2003.12.002.
Aarsland D, Laake K, Larsen JP, Janvin C. Donepezil for cognitive impairment in Parkinson’s disease: a randomised controlled study. J Neurol Neurosurg Psychiatry. 2002;72(6):708–12.
Tonnesen P, Tonstad S, Hjalmarson A, Lebargy F, Van Spiegel PI, Hider A, et al. A multicentre, randomized, double-blind, placebo-controlled, 1-year study of bupropion SR for smoking cessation. J Intern Med. 2003;254(2):184–92.
Semenchuk MR, Sherman S, Davis B. Double-blind, randomized trial of bupropion SR for the treatment of neuropathic pain. Neurology. 2001;57(9):1583–8.
Aubin HJ. Tolerability and safety of sustained-release bupropion in the management of smoking cessation. Drugs. 2002;62(Suppl 2):45–52.
Haggstram FM, Chatkin JM, Sussenbach-Vaz E, Cesari DH, Fam CF, Fritscher CC. A controlled trial of nortriptyline, sustained-release bupropion and placebo for smoking cessation: preliminary results. Pulmon Pharmacol Ther. 2006;19(3):205–9. doi:10.1016/j.pupt.2005.05.003.
Dhillon S, Yang LP, Curran MP. Bupropion: a review of its use in the management of major depressive disorder. Drugs. 2008;68(5):653–89.
Settle EC, Stahl SM, Batey SR, Johnston JA, Ascher JA. Safety profile of sustained-release bupropion in depression: results of three clinical trials. Clin Ther. 1999;21(3):454–63.
Glod CA, Lynch A, Flynn E, Berkowitz C, Baldessarini RJ. Open trial of bupropion SR in adolescent major depression. J Child Adolesc Psychiatr Nurs. 2003;16(3):123–30.
Foley KF, DeSanty KP, Kast RE. Bupropion: pharmacology and therapeutic applications. Expert Rev Neurother. 2006;6(9):1249–65. doi:10.1586/14737175.6.9.1249.
Lenze EJ, Mulsant BH, Shear MK, Dew MA, Miller MD, Pollock BG, et al. Efficacy and tolerability of citalopram in the treatment of late-life anxiety disorders: results from an 8-week randomized, placebo-controlled trial. Am J Psychiatry. 2005;162(1):146–50. doi:10.1176/appi.ajp.162.1.146.
Hellerstein DJ, Batchelder S, Miozzo R, Kreditor D, Hyler S, Gangure D, et al. Citalopram in the treatment of dysthymic disorder. Int Clin Psychopharmacol. 2004;19(3):143–8.
Kyle CJ, Petersen HE, Overo KF. Comparison of the tolerability and efficacy of citalopram and amitriptyline in elderly depressed patients treated in general practice. Depress Anxiety. 1998;8(4):147–53.
Thomsen PH, Ebbesen C, Persson C. Long-term experience with citalopram in the treatment of adolescent OCD. J Am Acad Child Adolesc Psychiatry. 2001;40(8):895–902. doi:10.1097/00004583-200108000-00010.
Gravem A, Amthor KF, Astrup C, Elgen K, Gjessing LR, Gunby B, et al. A double-blind comparison of citalopram (Lu 10–171) and amitriptyline in depressed patients. Acta Psychiatr Scand. 1987;75(5):478–86.
Stip E, Remington GJ, Dursun SM, Reiss JP, Rotstein E, MacEwan GW, et al. A Canadian multicenter trial assessing memory and executive functions in patients with schizophrenia spectrum disorders treated with olanzapine. J Clin Psychopharmacol. 2003;23(4):400–4. doi:10.1097/01.jcp.0000085414.08426.8f.
Lonergan E, Britton AM, Luxenberg J, Wyller T. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;(2):CD005594. doi:10.1002/14651858.CD005594.pub2.
Tollefson GD, Birkett MA, Kiesler GM, Wood AJ. Double-blind comparison of olanzapine versus clozapine in schizophrenic patients clinically eligible for treatment with clozapine. Biol Psychiatry. 2001;49(1):52–63.
McEvoy JP, Lieberman JA, Stroup TS, Davis SM, Meltzer HY, Rosenheck RA, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163(4):600–10. doi:10.1176/appi.ajp.163.4.600.
Lambert M, Holzbach R, Moritz S, Postel N, Krausz M, Naber D. Objective and subjective efficacy as well as tolerability of olanzapine in the acute treatment of 120 patients with schizophrenia spectrum disorders. Int Clin Psychopharmacol. 2003;18(5):251–60. doi:10.1097/01.yic.0000085883.08392.91.
Rendell JM, Gijsman HJ, Keck P, Goodwin GM, Geddes JR. Olanzapine alone or in combination for acute mania. Cochrane Database Syst Rev. 2003;(3):CD004040. doi:10.1002/14651858.CD004040.
Conley RR, Tamminga CA, Bartko JJ, Richardson C, Peszke M, Lingle J, et al. Olanzapine compared with chlorpromazine in treatment-resistant schizophrenia. Am J Psychiatry. 1998;155(7):914–20.
Malone RP, Cater J, Sheikh RM, Choudhury MS, Delaney MA. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. J Am Acad Child Adolesc Psychiatry. 2001;40(8):887–94. doi:10.1097/00004583-200108000-00009.
Hwang JP, Yang CH, Lee TW, Tsai SJ. The efficacy and safety of olanzapine for the treatment of geriatric psychosis. J Clin Psychopharmacol. 2003;23(2):113–8.
Costabile RA, Spevak M. Oral trazodone is not effective therapy for erectile dysfunction: a double-blind, placebo controlled trial. J Urol. 1999;161(6):1819–22.
Al-Yassiri MM, Ankier SI, Bridges PK. A double blind comparison of the efficacy and safety of trazodone and imipramine in endogenous depression. J Affect Disord. 1983;5(4):333–40.
Lance R, Albo M, Costabile RA, Steers WD. Oral trazodone as empirical therapy for erectile dysfunction: a retrospective review. Urology. 1995;46(1):117–20. doi:10.1016/S0090-4295(99)80176-9.
Monteleone P, Gnocchi G, Delrio G. Plasma trazodone concentrations and clinical response in elderly depressed patients: a preliminary study. J Clin Psychopharmacol. 1989;9(4):284–7.
Mihara K, Yasui-Furukori N, Kondo T, Ishida M, Ono S, Ohkubo T, et al. Relationship between plasma concentrations of trazodone and its active metabolite, m-chlorophenylpiperazine, and its clinical effect in depressed patients. Ther Drug Monit. 2002;24(4):563–6.
Fink HA, MacDonald R, Rutks IR, Wilt TJ. Trazodone for erectile dysfunction: a systematic review and meta-analysis. BJU Int. 2003;92(4):441–6.
Davidoff G, Guarracini M, Roth E, Sliwa J, Yarkony G. Trazodone hydrochloride in the treatment of dysesthetic pain in traumatic myelopathy: a randomized, double-blind, placebo-controlled study. Pain. 1987;29(2):151–61.
Elie R, Lavoie G, Bourgouin J, Le Morvan P. Zopiclone versus flurazepam in insomnia: prolonged administration and withdrawal. Int Clin Psychopharmacol. 1990;5(4):279–86.
Noble S, Langtry HD, Lamb HM. Zopiclone. An update of its pharmacology, clinical efficacy and tolerability in the treatment of insomnia. Drugs. 1998;55(2):277–302.
Mullen J, Jibson MD, Sweitzer D. A comparison of the relative safety, efficacy, and tolerability of quetiapine and risperidone in outpatients with schizophrenia and other psychotic disorders: the quetiapine experience with safety and tolerability (QUEST) study. Clin Ther. 2001;23(11):1839–54.
Purdon SE, Malla A, Labelle A, Lit W. Neuropsychological change in patients with schizophrenia after treatment with quetiapine or haloperidol. J Psychiatry Neurosci. 2001;26(2):137–49.
Baldwin CM, Scott LJ. Quetiapine extended release: in schizophrenia. CNS Drugs. 2009;23(3):261–9. doi:10.2165/00023210-200923030-00007.
Srisurapanont M, Disayavanish C, Taimkaew K. Quetiapine for schizophrenia. Cochrane Database Syst Rev. 2000;(3):CD000967. doi:10.1002/14651858.CD000967.
Yatham LN, Paulsson B, Mullen J, Vagero AM. Quetiapine versus placebo in combination with lithium or divalproex for the treatment of bipolar mania. J Clin Psychopharmacol. 2004;24(6):599–606.
Conley RR, Kelly DL, Nelson MW, Richardson CM, Feldman S, Benham R, et al. Risperidone, quetiapine, and fluphenazine in the treatment of patients with therapy-refractory schizophrenia. Clin Neuropharmacol. 2005;28(4):163–8.
Spencer T, Biederman J, Wilens T, Doyle R, Surman C, Prince J, et al. A large, double-blind, randomized clinical trial of methylphenidate in the treatment of adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57(5):456–63. doi:10.1016/j.biopsych.2004.11.043.
Biederman J, Mick E, Surman C, Doyle R, Hammerness P, Harpold T, et al. A randomized, placebo-controlled trial of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2006;59(9):829–35. doi:10.1016/j.biopsych.2005.09.011.
Blockmans D, Persoons P, Van Houdenhove B, Bobbaers H. Does methylphenidate reduce the symptoms of chronic fatigue syndrome? Am J Med. 2006;119(2):167 e23–30. doi:10.1016/j.amjmed.2005.07.047.
Alban JP, Hopson MM, Ly V, Whyte J. Effect of methylphenidate on vital signs and adverse effects in adults with traumatic brain injury. Am J Phys Med Rehabil. 2004;83(2):131–7 (quiz 8–41, 67). doi:10.1097/01.phm.0000112308.68586.1d.
Damestoy N, Collin J, Lalande R. Prescribing psychotropic medication for elderly patients: some physicians’ perspectives. CMAJ. 1999;161(2):143–5.
Feng B, Bell RA, Jerant AF, Kravitz RL. What do doctors say when prescribing medications? An examination of medical recommendations from a communication perspective. Health Commun. 2011;26(3):286–96. doi:10.1080/10410236.2010.550020.
WHO. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003.
Tahaineh LM, Wazaify M, Albsoul-Younes A, Khader Y, Zaidan M. Perceptions, experiences, and expectations of physicians in hospital settings in Jordan regarding the role of the pharmacist. Res Social Adm Pharm. 2009;5(1):63–70. doi:S1551-7411(08)00048-X10.1016/j.sapharm.2008.05.003.
Winterstein AG, Linden S, Lee AE, Fernandez EM, Kimberlin CL. Evaluation of consumer medication information dispensed in retail pharmacies. Arch Intern Med. 2010;170(15):1317–24. doi:170/15/131710.1001/archinternmed.2010.263.
Modig S, Kristensson J, Troein M, Brorsson A, Midlov P. Frail elderly patients’ experiences of information on medication. A qualitative study. BMC Geriatr. 2012;12:46. doi:10.1186/1471-2318-12-46.
Moen J, Bohm A, Tillenius T, Antonov K, Nilsson JL, Ring L. “I don’t know how many of these [medicines] are necessary.”—a focus group study among elderly users of multiple medicines. Patient Educ Couns. 2009;74(2):135–41. doi:10.1016/j.pec.2008.08.019.
Ljungberg C, Lindblad AK, Tully MP. Hospital doctors’ views of factors influencing their prescribing. J Eval Clin Pract. 2007;13(5):765–71. doi:10.1111/j.1365-2753.2006.00751.x.
Jones MI, Greenfield SM, Bradley CP. Prescribing new drugs: qualitative study of influences on consultants and general practitioners. BMJ. 2001;323(7309):378–81.
Greene JA. Pharmaceutical marketing research and the prescribing physician. Ann Intern Med. 2007;146(10):742–8.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi:10.1016/S0140-6736(12)60240-2.
Reason B, Terner M, Moses McKeag A, Tipper B, Webster G. The impact of polypharmacy on the health of Canadian seniors. Fam Pract. 2012;29(4):427–32. doi:10.1093/fampra/cmr124.
Seroquel—quetiapine fumarate immediate-release tablets quetiapine 25, 100, 200 and 300 mg; Product Monograph. Astra Zeneca Canada. Revised June 22, 2011. Available from: http://www.astrazeneca.ca/documents/ProductPortfolio/SEROQUEL_PM_en.pdf.
Therapeutics-Initiative. Is use of quetiapine for sleep evidence-based? Therapeutics Letter 79; 2010. Available from: http://www.ti.ubc.ca/sites/ti.ubc.ca/files/79_0.pdf.
Han PK, Klein WM, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Making. 2011;31(6):828–38. doi:10.1177/0272989X11393976.
Acknowledgments
We are grateful to Dr Alphonse Tran and Jassica Kaur-Sarai for their valuable contributions to this project. No external sources of funding were used to conduct this study or prepare this manuscript. The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nguyen, C.T., MacEntee, M.I., Mintzes, B. et al. Information for Physicians and Pharmacists About Drugs That Might Cause Dry Mouth: A Study of Monographs and Published Literature. Drugs Aging 31, 55–65 (2014). https://doi.org/10.1007/s40266-013-0141-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-013-0141-5