Abstract
Estetrol/drospirenone is a combined oral contraceptive (COC) with a plant-synthesised foetal oestrogen (estetrol) and a well-established progestin (drospirenone). In preclinical models, estetrol has lower binding affinity for the oestrogen receptor-α (ER-α) in contrast to estradiol and has antagonistic properties against membrane ER-α in several tissues, including the breast, while retaining agonistic activity on receptors located in the nucleus. The low oestrogenicity of estetrol may potentially contribute to reduced thrombotic risk. Estetrol/drospirenone was an effective contraceptive in phase II and III clinical trials, with regular and predictable bleeding cycles maintained in the majority of women. Estetrol/drospirenone was generally well-tolerated with metrorrhagia reported as the most common treatment-related adverse event, which is consistent with other COCs. Cases of migraines with aura (or severe migraines), deep vein thrombosis, hyperkalaemia and depression were rarely reported during the phase III trials. Overall, estetrol/drospirenone is an effective and generally well-tolerated COC, with a potentially reduced risk of thrombosis.
Plain Language Summary
In 2019, an estimated 44% of women aged 15–49 years worldwide used modern contraception methods, and in these women using modern methods, 18% used an oral contraceptive. Estetrol/drospirenone is a combined oral contraceptive (COC) which uses estetrol, a plant-synthesised oestrogen naturally produced by the human foetal liver during pregnancy, in combination with drospirenone, a well-known progestin. Combined, these hormones suppress ovulation, which constitutes their primary mode of action in preventing pregnancy. As estetrol has weaker oestrogen-related effects, it may potentially reduce the risk for blood clots. Estetrol/drospirenone was an effective contraceptive in clinical trials, and most women had regular and predictable bleeding cycles. Metrorrhagia (i.e. abnormal bleeding) was the most commonly reported treatment-related adverse effect; however, this is a common issue with hormonal contraceptives. Cases of severe migraine headaches, deep vein thrombosis, high potassium levels or depression were rarely reported during clinical trials. Estetrol/drospirenone is an effective oral contraceptive, which may offer a contraceptive option with a lower risk for blood clots. However, further research is required to confirm the reduced risk of clotting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Digital Features for this Adis Drug Evaluation can be found at https://doi.org/10.6084/m9.figshare.19768738. |
Combined oral contraceptive with estetrol, a natural foetal oestrogen, and drospirenone, a progestin |
Estetrol has lower oestrogenicity than estradiol; thus estetrol may potentially reduce thrombotic risk |
Effective contraceptive with predictable bleeding cycles in a majority of women |
Generally well-tolerated with metrorrhagia being the most common treatment-related adverse event |
1 Introduction
In 2019, there were an estimated 842 million women (44% of 1.9 billion women) aged 15–49 years worldwide who used modern contraceptive methods, and of these women, 151 million (18%) used oral contraceptives [1]. The number of women using oral contraceptives increased from 97 million to 151 million between 1994 and 2019, with the prevalence of use rising in most geographical regions. Oral contraceptives were the most commonly used contraception method in Europe and North America, Oceania and Northern Africa and Western Asia [1].
Combined oral contraceptives (COC), which are a subset of combined hormonal contraceptives (CHC), typically contain an oestrogen and a progestin [2]. Progestins suppress the release of gonadotropin-releasing hormone from the hypothalamus, which prevents the secretion of luteinizing hormone from the pituitary, and subsequently, inhibits ovulation. Furthermore, by thickening the cervical mucus, progestins inhibit the movement and survival of sperm and prevent their travel to the fallopian tubes. Oestrogens complement the contraceptive action of progestins, as they prevent the release of gonadotropins and follicle-stimulating hormone to suppress the development of a dominant follicle [2]. As the efficacy of COCs has been excellent since the first available COC, the search for safer alternatives has been the goal of COC development [3]. A rare, but serious, adverse reaction with COCs is thrombotic events, including deep vein thrombosis (DVT), which are attributed to an increase in haemostatic activity caused by oestrogens [2].
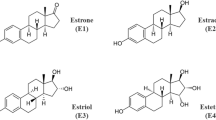
Estetrol/drospirenone (Nextstellis® in the USA and Drovelis® or Lydisilka® in the EU) is a once-daily, single-tablet COC; estetrol is a previously unutilised oestrogen [4] and drospirenone is a progestin which has been utilised in other hormonal contraceptives [5]. Estetrol is naturally produced by the foetal liver during pregnancy, but may be manufactured from plant-based sources [6]. Recently, estetrol has been investigated for potential safety benefits, including a reduced impact on coagulation [7, 8]. Estetrol/drospirenone is approved as an oral contraceptive in several countries, including the USA and those in Europe. This article summarises the pharmacological properties, therapeutic efficacy and tolerability of estetrol/drospirenone in contraception as approved in Europe and the USA.
2 Pharmacodynamic Properties of Estetrol/Drospirenone
The primary mechanism of contraception with estetrol and drospirenone is the inhibition of ovulation (Table 1). In a phase II trial, Hoogland scores were utilised to assess the suppression of ovarian function in women receiving estetrol (as monohydrate)/drospirenone 15 mg/3 mg or ethinylestradiol/drospirenone 20 μg/3 mg [9]. Ovulation was inhibited in all estetrol/drospirenone recipients in cycles 1–3, whereas three ovulation events were observed in two ethinylestradiol/drospirenone recipients (Table 1). No ovarian activity was reported in 85.0% of estetrol/drospirenone recipients and 82.9% of ethinylestradiol/drospirenone recipients in cycle 1, and 65.8% and 83.8% in cycle 3, respectively. The lower proportion of estetrol/drospirenone recipients with the absence of ovarian activity in cycle 3 may be attributed to reduced pituitary suppression in comparison with ethinylestradiol/drospirenone. Endometrial thickness was similar between both treatment arms and the thickness was generally constant throughout cycles 1 and 3. The mean time to restoration of ovulation was 15.5 days and 18.1 days following discontinuation of estetrol/drospirenone and ethinylestradiol/drospirenone, respectively [9]. Additionally, in a phase II dose-finding trial, ovulation was inhibited in all estetrol/drospirenone recipients (Table 1) [10].
The key pharmacodynamic effects of estetrol/drospirenone are summarized in Table 1. Estetrol or estetrol/drospirenone had minimal effects on carbohydrate and lipid metabolism [11], with a limited effect on haemostasis parameters [8, 12] and a neutral risk for breast cancer (at therapeutic concentrations) [13]. Estetrol/drospirenone does not prolong QT interval to a clinically relevant extent [14]. As the pharmacodynamic properties of drospirenone, including its antimineralocorticoid properties and the potential for hyperkalaemia, have been reviewed previously [5], the remainder of this section will primarily discuss the pharmacodynamic properties of estetrol.
Estetrol demonstrated similarities and differences in oestrogen receptor (ER) activity in comparison with estradiol (Table 1). Estetrol and estradiol have similar binding characteristics on ER-α and are both agonists for ERs located within the nucleus [15]. However, estetrol is a partial antagonist against ER-α expressed in cell membranes, which abrogates membrane-initiated steroid signalling (MISS)-related effects, including effects on endothelial nitric oxide synthase, endothelial healing and MISS-related signalling in a breast cancer cell line [15]. Additionally, estetrol was less potent and had a lower binding affinity than estradiol for ER-α (Table 1) [15, 16]. The reduced oestrogenicity of estetrol in comparison with other oestrogens may account for the lower thrombotic potential of estetrol, which was demonstrated by its reduced effects on endogenous thrombin potential (ETP)-based activated protein C sensitivity resistance (APCr) and other coagulation factors (Table 1) [8, 12].
3 Pharmacokinetic Properties of Estetrol/Drospirenone
The pharmacokinetics of estetrol/drospirenone are dose-proportional between 15–75 mg for estetrol and 1–10 mg for drospirenone [14]. The median times to maximum plasma concentration (Tmax) of estetrol and drospirenone are 0.5 h and 1.0 h, respectively. With multiple administrations of estetrol/drospirenone, steady state occurs after 4 and 10 days for estetrol and drospirenone, with an accumulation ratio of 1.6 and 2.3, respectively. Relative to fasting, when estetrol/drospirenone is taken with a high-fat meal, the geometric means of the ratios in the maximum plasma concentration (Cmax) for estetrol and drospirenone are 0.51 and 0.75; the geometric means of the ratios in the area under the concentration-time curve (AUC) from time zero to infinity are 1.01 and 1.08 [14]. The proportion of plasma protein binding was 46–50% for estetrol and 95–97% for drospirenone, with the latter binding primarily to plasma albumin [14, 17]; neither estetrol nor drospirenone bind to sex hormone binding globulin [17]. The half-lives of estetrol and drospirenone are 24–27 h and 34 h, respectively [14, 17], with the former affected by enterohepatic recycling [14]. Estetrol primarily undergoes phase 2 metabolism resulting in the formation of inactive glucuronide and sulfate conjugates; UDP-glucuronosyltransferase 2B7 is the main enzyme isoform that is responsible for the formation of glucuronide conjugates [14, 17] and oestrogen sulfotransferase (SULT1E1) for the production of sulfate conjugates [17]. Drospirenone is metabolised by cytochrome P450 (CYP) 3A4 and is predominantly present in the plasma as the acid form or as a metabolite formed by reduction and subsequent sulfation [14, 17]. Approximately 69% of the estetrol dose is excreted into the urine (0% as unchanged drug [14]) and 22% of the dose into the faeces (100% as unchanged drug [14]) [14, 17]; 38% and 44% of the drospirenone dose is excreted into the urine and faeces, respectively [14].
Concomitant administration of rifampicin (a CYP3A4 inducer) with ethinylestradiol/drospirenone 20 µg/3 mg resulted in a decrease in the 24 h AUC (AUC24) of drospirenone by 30% with a low rifampin dose and 86% with a high rifampin dose [14]. Conversely, concomitant administration of ketoconazole (a CYP3A4 inhibitor) with ethinylestradiol/drospirenone 20 µg/3 mg increased the AUC24 and Cmax of drospirenone by 2.68-fold and 1.97-fold. Oestrogens are known to decrease plasma concentrations of lamotrigine, which is attributed to the induction of lamotrigine glucuronidation. However, no specific data are available regarding the impact of estetrol on lamotrigine exposure [14]. Concomitant use of antiviral drugs for the treatment of human immunodeficiency virus or hepatitis C virus infections may increase or decrease plasma concentrations of oestrogens and progestogens to a clinically relevant extent [17].
The effect of hepatic impairment or chronic kidney disease on estetrol pharmacokinetics are unknown, however, drospirenone pharmacokinetics are affected by these conditions [14, 17]. In women with moderate hepatic impairment, the exposure to drospirenone is 3-fold higher than in those with normal hepatic function; the effects of severe hepatic impairment on drospirenone are unknown. The mean serum concentration of drospirenone is 37% higher in women with a creatinine clearance (CLcr) of 30–49 mL/min who are on a low-potassium diet and potassium-sparing drugs, in comparison with women with a normal CLcr. No clinically significant differences in drospirenone pharmacokinetics are reported in women with a CLcr of 50–79 mL/min [14].
4 Contraceptive Efficacy of Estetrol/Drospirenone
In an open-label, randomized, phase II trial (FIESTA) evaluating estetrol 15 or 20 mg, combined with drospirenone 3 mg or levonorgestrel 150 µg, estetrol/drospirenone 15 mg/3 mg provided the most favourable bleeding pattern and cycle control [18]. Consequently, the efficacy of this regimen was evaluated in two similarly designed multi-national, single-arm, open-label phase III trials [E4 FREEDOM] (Fig. 1) [19, 20]. The E4 FREEDOM trials were conducted in the USA/Canada [19] and Europe/Russia [20]. Eligible patients were heterosexually active women aged 16–50 years in the USA/Canada study and 18–50 years in the Europe/Russia study, with a body mass index (BMI) of ≤ 35 kg/m2 who were willing to use estetrol/drospirenone as the only or primary method of contraception for 13 cycles (12 months) [19, 20]. Women were required to have a regular menstrual cycle when not using a hormonal treatment and a negative pregnancy test prior to initiating contraception. Switching immediately from other contraceptives to estetrol/drospirenone was permitted, with the exception of injectable formulations that required a washout period prior to initiating contraception with estetrol/drospirenone. Key exclusion criteria were consistent with World Health Organization (WHO) contraindications to COC use, including cardiovascular, thromboembolic or cerebrovascular conditions (e.g. hypertension defined as ≥ 140/90 mmHg) and nicotine smokers aged ≥ 35 years [19, 20].
Trial design of single arm, open-label phase III E4 FREEDOM trials in women [19, 20]. Efficacy results are reported in the animated figure (available online). At-risk cycles were cycles where participants self-reported study treatment intake, sexual intercourse and no additional contraception. Modified at-risk cycles included all cycles where no additional contraception was used, irrespective of sexual activity during the cycle. WHO World Health Organization
Supplementary file1 (MP4 8230 KB)
The E4 FREEDOM trial participants received contraception in 28-day cycles for 13 cycles (12 months), with each cycle consisting of 24 days of active treatment with estetrol/drospirenone 15 mg/3 mg and 4 days of placebo once daily [19, 20]. The intake of study treatment, sexual activity, use of other contraceptives and vaginal bleeding or spotting events were recorded by trial participants [19, 20].
The primary efficacy endpoint in both E4 FREEDOM trials was the Pearl Index (PI), which was defined as the number of on-treatment pregnancies per 100 women-years of exposure calculated in at-risk cycles [19, 20]. On-treatment was defined as any reported or confirmed pregnancy with an estimated date of conception up to 7 days (US FDA definition) [19] or 2 days (EMA definition) [20] after the last intake of study treatment. At-risk treatment cycles were defined as cycles where participants self-reported study treatment intake (empty study drug packets were returned to investigators during the Europe/Russia study [20]), sexual intercourse and no additional contraception [19, 20]. In the Europe/Russia study, the PI was also calculated in modified at-risk cycles (EMA definition), which included all cycles where no additional contraception was used, irrespective of sexual activity during the cycle [20]. The PI was calculated in women aged 16–35 years in the USA/Canada study [19] and 18–35 years in the Europe/Russia study [20]. A key secondary endpoint was method-failure PI; a pregnancy was considered a ‘method failure’ when it occurred with reported correct study medication intake while excluded medications or supplements were not taken [19, 20].
In the primary efficacy population, the mean age was 25.8 and 25.0 years in the USA/Canada and Europe/Russia studies. The mean BMI was 25.8 and 22.9 kg/m2 in the USA/Canada and Europe/Russia studies, with 22.5% and 5.5% of women in the respective studies having a BMI of ≥ 30 kg/m2. In the USA/Canada study, 70.1% of women were white, 19.5% were black, 4.8% were Asian and 5.5% were of other races; in the Europe/Russia study, 98.6% of women were white. The proportion of nulliparous women in the USA/Canada and Europe/Russia studies was 67.7% and 78.9%, respectively [19, 20].
Estetrol/drospirenone was an effective oral contraceptive in both E4 FREEDOM trials [19, 20]. The overall PI was 2.65 in the USA/Canada study and 0.47 in the Europe/Russia study (Table 2; primary endpoint) with the PI for modified at-risk cycles in the Europe/Russia study being 0.44 (Table 2). These results are supported by method-failure PI in both regions (1.43 and 0.29, respectively). In a pooled analysis of 3027 women aged 16–35 years across both trials, the overall PI was 1.52 (95% CI 1.04–2.16) [21]. In addition, in the full trial population aged 18–50 years in the Europe/Russia study, the overall and method-failure PIs were 0.41 and 0.25 for at-risk cycles, and 0.38 and 0.23 for modified at-risk cycles [20].
In the primary efficacy population, overall and method-failure cumulative 13-cycle life-table pregnancy rates were 2.06% (95% CI 1.40–3.04%) and 1.18% (95% CI 0.69–2.01%) in the USA/Canada study [19], and 0.45% (95% CI 0.19–1.09%) and 0.28% (95% CI 0.09–0.86%) in the Europe/Russia study [20]. In the overall population of women aged 18–50 years in the Europe/Russia study, the overall and method-failure pregnancy rates were 0.39% (95% CI 0.16–0.94%) and 0.24% (95% CI 0.08–0.74%), respectively [20].
In the USA/Canada study, independent risk factors for on-treatment pregnancy in estetrol/drospirenone recipients were age (16–25 vs 26–35 years; HR 2.41, 95% CI 1.05–5.54), race (black vs white; HR 3.14, 95% CI 1.32–7.45), parity (parous vs nulliparous; HR 4.15, 95% CI 1.65–10.46) and compliance (< 99% vs ≥ 99%; HR 3.17, 95% CI 1.45–6.93) [19]. BMI, prior hormonal contraceptive use and smoking status were not identified as risk factors for on-treatment pregnancy [19]. However, a trend of decreasing efficacy with increasing BMI was observed during the study [14]. Subgroup analyses were not possible in the Europe/Russia study, as only five on-treatment pregnancies were reported [20].
Regular vaginal bleeding and spotting cycles were maintained during contraception with estetrol/drospirenone in most women [19, 20]. In both trials, clear cyclical patterns of bleeding were observed during the placebo phase of the 28-day treatment cycles and the median duration of scheduled bleeding and/or spotting was 4–5 days. In a pooled analysis of both trials, 87.2–90.4% of women had scheduled bleeding/spotting events across all cycles. The frequency of unscheduled bleeding or spotting events was 27.1% in cycle 1, which from cycle 5 onwards, decreased to < 17.5% [22]. In the USA/Canada study, the proportion of women who reported the absence of scheduled bleeding was highest at cycle 3 (18.0%), which decreased to 13.3% at cycle 12 [19]. In the Europe/Russia study, ≤ 10% of estetrol/drospirenone recipients reported the absence of scheduled bleeding across all treatment cycles [20]. Age, BMI and hormonal contraceptive use 3 months prior to enrolment did not appear to affect bleeding patterns in women enrolled in the Europe/Russia study [23].
In the phase II FIESTA trial, estetrol/drospirenone 15 mg/3 mg was similar to estradiol valerate/dienogest with respect to user satisfaction, acceptability and bodyweight control [24]. Overall satisfaction was assessed using combined data from cycles 1–4 and 6 as an aggregate of the following domains; general feeling, mood, sexual life, premenstrual complaints and overall effect. The odds ratio for overall satisfaction with estetrol/drospirenone 15 mg/3 mg versus estradiol valerate/dienogest was 0.69 (95% CI 0.39–1.25). At cycle 6, the proportion of women who were reported to be satisfied or very satisfied with the study drug were 73.1% versus 67.6%, respectively. The proportion of women who gained or lost ≥ 2 kg of body weight by cycle 6 were generally similar across the estetrol/drospirenone 15 mg/3 mg and estradiol valerate/dienogest treatment arms [24].
5 Tolerability of Estetrol/Drospirenone
Contraception with estetrol/drospirenone was generally well-tolerated in the E4 FREEDOM trials (Sect. 4) [19, 20]. Treatment-emergent adverse events (AEs) were reported in 53.8% of 1864 women in the USA/Canada study [19] and 50.5% of 1553 women in the Europe/Russia study [20], with headache being the most common in both trials (incidence 5.0% and 7.7%, respectively) [19, 20]. Treatment-related AEs were reported in 28.9% of women in the USA/Canada study [19] and 28.5% in the Europe/Russia study [20]. The most commonly (incidence ≥ 3%) reported treatment-related AEs in the USA/Canada study were metrorrhagia (4.4%) and headache (3.5%) [19], and in the Europe/Russia study were metrorrhagia (5.0%), vaginal haemorrhage (4.3%) and acne (3.8%) [20]. The most common (incidence ≥ 0.5%) treatment-related AEs leading to treatment discontinuation were metrorrhagia (0.9%), menorrhagia (0.8%), vaginal haemorrhage (0.5%) and weight increase (0.5%) in the USA/Canada study [19]; in the Europe/Russia study, metrorrhagia (1.5%), acne (1.3%), vaginal haemorrhage (1.0%), decreased libido (0.8%), altered mood (0.5%) and mood swings (0.5%) were the most common [20].
In a pooled analysis of 3417 women from both E4 FREEDOM trials, the most common treatment-related AEs were metrorrhagia (4.7%), acne (3.3%) and headache (3.2%) [21]. Three (0.1%) serious treatment-related AEs were reported, including worsening depression, ectopic pregnancy and venous thromboembolism (VTE); treatment was discontinued following ectopic pregnancy and venous thromboembolism [21].
As with other hormonal contraceptives in general, cardiovascular events (e.g. thromboembolic disorders), migraines and depression have been reported with estetrol/drospirenone in E4 FREEDOM trials (n = 3632 [14]) [14, 17]. Across both trials, one thromboembolic event was reported, which was a case of VTE in a woman with a history of hormonal contraceptive use aged 32 years in her fourth treatment cycle [20]. The VTE event resolved without sequelae following antithrombotic treatment and discontinuation of estetrol/drospirenone [20]. Potential risk factors for VTEs include obesity, family history of VTE, prolonged immobilisation [14, 17], the presence of other medical conditions (e.g. cancer, systemic lupus erythematosus, haemolytic uraemic syndrome, chronic inflammatory bowel disease or sickle cell disease), increasing age [17] and smoking [14]. As migraine with aura is associated with an increased risk of stroke, estetrol/drospirenone was discontinued in six women (0.17%) due to new onset of migraines with aura and in two women (0.05%) due to severe migraines. Depression was reported in 36 women (1.7%), leading to treatment discontinuation in 9 women (0.3%) during the USA/Canada study [14]; the incidence of depression (treatment-related or any event) in the Europe/Russia study was not reported as the incidence was < 2% [20]. Hyperkalaemia, which may occur due to the anti-mineralocorticoid properties of drospirenone, was reported in seven women across both trials, with one woman discontinuing treatment [14]. Most cases of hyperkalaemia were mild in severity or transient in nature [14].
6 Dosage and Administration of Estetrol/Drospirenone
In the USA and the EU, the recommended dosage of estetrol/drospirenone for contraception is one oral tablet taken once daily in 28-day cycles at the same time every day [14, 17]. Each cycle consists of 24 active tablets, each containing 14.2 mg estetrol (equivalent to 15 mg estetrol monohydrate) and 3 mg drospirenone, and four inert tablets. Alternative methods of contraception, such as barrier methods [17] or non-hormonal contraception [14], are recommended in women who miss taking an active tablet by ≥ 24 h (in the EU [17]) or if two active tablets are missed (in the USA [14]); missed doses may be taken immediately, even if two doses are taken on the same day. Seven days of uninterrupted active treatment are required to restore contraceptive effect [14, 17].
As with other hormonal contraceptives, contraception with estetrol/drospirenone is associated with warnings, precautions and contraindications in the USA and the EU (e.g. for patients with concomitant cardiovascular disease, thrombogenic conditions, hyperkalemia, hormonally-sensitive malignancies, hepatic disease, diabetes or migraines) [14, 17]. In the USA, the contraindication of estetrol/drospirenone in women over the age of 35 who smoke, due to the increased risk of serious cardiovascular events, is reported as a boxed warning [14]. Similar contraindications are included in the EU prescribing information [17], and have been reported with other COCs [14, 17]. Consult local prescribing information for details regarding warnings, precautions, contraindications and administration.
7 Place of Estetrol/Drospirenone in Contraception
Estetrol/drospirenone is a COC, which is a potential contraceptive option available to women. Current guidelines from the WHO [25], Centers for Disease Control and Prevention (CDC) [26] and Faculty of Sexual and Reproductive Healthcare (FSRH) [27] are yet to be updated to include specific recommendations on the use of estetrol/drospirenone; recommendations regarding the use of COCs [25] and CHCs [26, 27] are available. The guidelines are generally congruent and recommend the method of contraception be tailored to the medical circumstances and desires of each patient [25,26,27]. With respect to efficacy, COCs and CHCs with a real-world first-year failure rate of 7–9% are less efficacious than methods that do not rely on high patient adherence such as hormonal implants, copper or levonorgestrel intrauterine devices and male or female sterilisation (all having a first-year failure rate < 1%), but are more efficacious than male or female condoms, spermicide, fertility awareness methods and withdrawal (all having a first-year failure rate ≥ 13%). COCs and CHCs are generally as effective as progesterone-only pills or other non-orally administered CHCs including dermal patches, hormonal injections and vaginal rings (2–9%) [25,26,27].
Across all three guidelines, COCs and CHCs are either contraindicated or the risks outweighs the benefits in women who recently gave birth, need prolonged immobilisation (e.g. due to major surgery) or are aged ≥ 35 years and smoke [25,26,27]. COCs and CHCs are also not recommended for women with concomitant active breast cancer, migraines with aura, thrombogenic conditions, high blood pressure (≥ 140/90 mmHg), cardiovascular disease (e.g. myocardial infarction), advanced diabetes, serious hepatic disease (including gallbladder disease) or systemic lupus erythematosus. COCs and CHCs are generally not recommended in women who are taking enzyme-inducing drugs (e.g. rifampicin or rifabutin) due to the potential for reduced contraceptive efficacy [25,26,27].
The pituitary-ovarian axis and ovulation was suppressed in healthy women receiving estetrol/drospirenone (Sect. 2). Ovulation was inhibited in all estetrol/drospirenone recipients, with more than half of the recipients demonstrating an absence of ovarian function [9]. The endometrial thickness in estetrol/drospirenone recipients did not change during treatment cycles and the thickness was consistent with ethinylestradiol/drospirenone recipients [9].
Estetrol/drospirenone was an effective contraceptive in the E4 FREEDOM clinical trials (Sect. 4). In the phase III USA/Canada study, the PI was 2.65 in women aged 16–35 years, which is consistent with other contemporary oestrogen/progestin-based contraceptives [19]; the PI was 2.6 in a trial with ethinylestradiol/norethindrone acetate 10 µg/1 mg (an oral COC) [28] and 2.98 in a trial with ethinylestradiol/segesterone acetate 13 µg/150 µg (a vaginal CHC) [29]. In the phase III Europe/Russia study, the PI was 0.47 in women aged 18–35 years during at-risk cycles and 0.44 in modified at-risk cycles (EMA definition). Additionally, the EMA required precision in the PI was met [20]. Consistent with observations that have been made previously with other cross-continental COC trials, the difference in the PI across the E4 FREEDOM clinical trials may be attributed to socio-cultural effects, which is associated with decreased treatment adherence and efficacy [4, 30]. Secondary analyses including method failure PIs and cumulative life-table pregnancy rates in both trials also supported the efficacy of estetrol/drospirenone [19, 20]. In the North American population, gravidity, compliance, race, and age were independent risk factors for pregnancy, with compliance being the only potentially modifiable risk factor. The association between race and lower efficacy may be attributed to unmeasured factors, such as socioeconomic factors and other social factors or disparities in hormone metabolism due to genetic differences [19]. Satisfactory bleeding cycle control with clear cyclic bleeding patterns was maintained in the majority of women during the E4 FREEDOM trials (Sect. 4).
Estetrol/drospirenone was generally well-tolerated in phase III clinical trials (Sect. 5). Metrorrhagia was the most common treatment-related AE in both phase III trials, which was also the most common treatment-related AE leading to treatment discontinuation [19, 20]. The occurrence of irregular bleeding with estetrol/drospirenone is consistent with COCs or CHCs in general [25,26,27]. Headache and acne were also among the most common treatment-related AEs [19,20,21]. However, the incidence of these were ≤ 5% in either trial [19, 20]. Cases of migraines with aura (or severe migraines), thromboembolic events (one reported case of VTE [20]), hyperkalaemia and depression were minimally reported during the trials (Sect. 5) [14].
Estetrol/drospirenone has lower oestrogenicity than ethinylestradiol-based COCs (Sect. 2). This favourable pharmacodynamic feature may be associated with reduced thrombotic risk and improved HDL profile in clinical trials (Table 1). Estetrol reduced breast cancer risk in animal models at therapeutic concentrations and prevented MISS-related signalling in a breast cancer cell line (Table 1). As the absolute risk of DVT is low, 5–10 years are typically required to determine the DVT risk with COCs [7], and CHC-related regulatory warnings are included in the prescribing information for estetrol/drospirenone (Sect. 6). Although the limited effect of estetrol on the growth of breast cancer or epithelial cells may be beneficial to the safety profile of estetrol/drospirenone, these data are currently in animal models [13, 31]. Additional postmarketing experience will be valuable in determining the thrombotic risk with estetrol/drospirenone.
In conclusion, estetrol/drospirenone is an effective and generally well-tolerated COC, which expands the number of options available for contraception, with a potentially reduced risk of thrombotic events.
Data Selection Estetrol/Drosperinone: 146 records identified
Duplicates removed | 34 |
Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomized trial) | 58 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase I/II trials) | 22 |
Cited efficacy/tolerability articles | 8 |
Cited articles not efficacy/tolerability | 24 |
Search Strategy: EMBASE, MEDLINE and PubMed from 1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were Estetrol, drosperinone, Nextsellis, Lydisilka, combined oral contraceptive, COC. Records were limited to those in English language. Searches last updated 9 Jun 2022 | |
Change history
09 August 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40265-022-01760-w
References
United Nations, Department of Economic and Social Affairs, Population Division. Contraceptive use by method 2019: data booklet (ST/ESA/SER.A/435). 2019.
Teal S, Edelman A. Contraception selection, effectiveness, and adverse effects. JAMA. 2021;326(24):2507–18.
Bastianelli C, Farris M, Rosato E, et al. Pharmacodynamics of combined estrogen-progestin oral contraceptives 3. Inhibition of ovulation. Expert Rev Clin Pharmacol. 2018;11(11):1085–98.
Mawet M, Gaspard U, Foidart JM. Estetrol as estrogen in a combined oral contraceptive, from the first in-human study to the contraceptive efficacy. Eur Gynecol Obstet. 2021;3(1):3–21.
Motivala A, Pitt B. Drospirenone for oral contraception and hormone replacement therapy. Drugs. 2007;67(5):647–55.
National Library of Medicine. Estetrol compound summary. 2022. https://pubchem.ncbi.nlm.nih.gov/. Accessed 9 June 2022.
Foidart JM, Gaspard U, Pequeux C, et al. Unique vascular benefits of estetrol, a native fetal estrogen with specific actions in tissues (NEST). In: Brinton R, Genazzani A, Simoncini T, Stevenson J (eds) Sex steroids' effects on brain, heart and vessels ISGE series. Springer, Cham 2019; Chapter 12:169–95.
Douxfils J, Klipping C, Duijkers I, et al. Evaluation of the effect of a new oral contraceptive containing estetrol and drospirenone on hemostasis parameters. Contraception. 2020;102(6):396–402.
Duijkers I, Klipping C, Kinet V, et al. Effects of an oral contraceptive containing estetrol and drospirenone on ovarian function. Contraception. 2021;103(6):386–93.
Duijkers IJ, Klipping C, Zimmerman Y, et al. Inhibition of ovulation by administration of estetrol in combination with drospirenone or levonorgestrel: results of a phase II dose-finding pilot study. Eur J Contracept Reprod Health Care. 2015;20(6):476–89.
Klipping C, Duijkers I, Mawet M, et al. Endocrine and metabolic effects of an oral contraceptive containing estetrol and drospirenone. Contraception. 2021;103(4):213–21.
Kluft C, Zimmerman Y, Mawet M, et al. Reduced hemostatic effects with drospirenone-based oral contraceptives containing estetrol vs. ethinyl estradiol. Contraception. 2017;95(2):140–7.
Gallez A, Blacher S, Maquoi E, et al. Estetrol combined to progestogen for menopause or contraception indication is neutral on breast cancer. Cancers (Basel). 2021;13(2486):1–23.
Mayne Pharma. Nextstellis (estetrol/drospirenone) tablets: US prescribing information. 2021. https://dailymed.nlm.nih.gov/. Accessed 9 Jun 2022.
Abot A, Fontaine C, Buscato M, et al. The uterine and vascular actions of estetrol delineate a distinctive profile of estrogen receptor alpha modulation, uncoupling nuclear and membrane activation. EMBO Mol Med. 2014;6(10):1328–46.
European Medicines Agency. Lydisilka (estetrol/drospirenone) tablets: EU assessment report. 2021. https://www.ema.europa.eu/. Accessed 9 Jun 2022.
European Medicines Agency. Lydisilka (estetrol/drospirenone) tablets: EU summary of product characteristics. 2022. https://www.ema.europa.eu/. Accessed 9 Jun 2022.
Apter D, Zimmerman Y, Beekman L, et al. Bleeding pattern and cycle control with estetrol-containing combined oral contraceptives: results from a phase II, randomised, dose-finding study (FIESTA). Contraception. 2016;94(4):366–73.
Creinin MD, Westhoff CL, Bouchard C, et al. Estetrol–drospirenone combination oral contraceptive: North American phase 3 efficacy and safety results. Contraception. 2021;104(3):222–8.
Gemzell-Danielsson K, Apter D, Zatik J, et al. Estetrol–drospirenone combination oral contraceptive: a clinical study of contraceptive efficacy, bleeding pattern and safety in Europe and Russia. BJOG. 2022;129(1):63–71.
Jensen JT, Kaunitz AM, Chen MJ, et al. Pooled phase-3 analysis of efficacy and safety of estetrol/drospirenone combined oral contraceptive [abstract no. P0638]. Int J Gynaecol Obstet. 2021;155(Suppl. 2):386.
Kaunitz AM, Achilles SL, Jost M, et al. Bleeding patterns with use of an oral contraceptive containing estetrol and drospirenone: pooled analysis of phase-3 clinical trials [abstract no. P48]. Contraception. 2021;104(4):463.
Gemzell-Danielsson K, Apter D, Jost M, et al. Bleeding patterns with estetrol/drospirenone oral contraceptive by age, obesity status, and recent hormonal contraceptive use [abstract no. OP04]. Eur Gynecol Obstet. 2021;3(Suppl. 1):82.
Apter D, Zimmerman Y, Beekman L, et al. Estetrol combined with drospirenone: an oral contraceptive with high acceptability, user satisfaction, well-being and favourable body weight control. Eur J Contracept Reprod Health Care. 2017;22(4):260–7.
World Health Organization and Johns Hopkins Bloomberg School of Public Health. Center for Communication Programs. Family planning: a global handbook for providers: evidence-based guidance developed through worldwide collaboration, 3rd ed. (2018).
Centers for Disease Control and Prevention. US selected practice recommendations (US SPR) for contraceptive use, 2016. 2022. https://www.cdc.gov/. Accessed 9 Jun 2022.
Faculty of Sexual and Reproductive Healthcare. FSRH clinical guideline: combined hormonal contraception. 2020. https://www.fsrh.org/. Accessed 9 Jun 2022.
Archer DF, Nakajima ST, Sawyer AT, et al. Norethindrone acetate 10 milligram and ethinyl estradiol 1.0 micrograms as an ultra low-dose oral contraceptive. Obstet Gynecol. 2013;122(3):601–7.
Archer DF, Merkatz RB, Bahamondes L, et al. Efficacy of the 1-year (13-cycle) segesterone acetate and ethinylestradiol contraceptive vaginal system: results of two multicentre, open-label, single-arm, phase 3 trials. Lancet Glob Health. 2019;7(8):e1054–64.
Gerlinger C, Trussell J, Mellinger U, et al. Different Pearl Indices in studies of hormonal contraceptives in the United States: impact of study population. Contraception. 2014;90(2):142–6.
Gerard C, Blacher S, Communal L, et al. Estetrol is a weak estrogen antagonizing estradiol-dependent mammary gland proliferation. J Endocrinol. 2015;224(1):85–95.
Visser M, Foidart JM, Coelingh Bennink HJT. In vitro effects of estetrol on receptor binding, drug targets and human liver cell metabolism. Climacteric. 2008;11(Suppl. 1):64–8.
Acknowledgments
During the peer review process, the manufacturer of estetrol/drospirenone was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and Conflict of interest
Arnold Lee and Yahiya Y. Syed are salaried employees of Adis International Ltd/Springer Nature, and declare no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent to publish, Availability of data and material, Code availability
Not applicable.
Additional information
The original article has been revised due to retrospective open choice order.
The manuscript was reviewed by: C. Di Carlo, Department of Neurosciences and Reproductive Sciences, University of Naples Federico II, Naples, Italy; L. P. Shulman, Department of Obstetrics and Gynecology, Feinberg School of Medicine of Northwestern University, Chicago, IL, USA.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lee, A., Syed, Y.Y. Estetrol/Drospirenone: A Review in Oral Contraception. Drugs 82, 1117–1125 (2022). https://doi.org/10.1007/s40265-022-01738-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-022-01738-8