Abstract
Background
Generalized convulsive status epilepticus (GCSE) is a medical emergency associated with high morbidity and mortality that requires prompt medical intervention. Topiramate (TPM) is an antiepileptic drug effective against a broad spectrum of seizure types, and has been proposed as a possible therapeutic option for super-refractory status epilepticus (SRSE), the most severe form of GCSE.
Aim
This review aimed to evaluate the role of TPM in GCSE, including SRSE.
Methods
MEDLINE, CENTRAL, ClinicalTrials.gov, LILACS, Google Scholar, and Opengrey.eu were systematically searched. We compared: (1) patients who did and who did not receive TPM as their last drug; (2) patients receiving TPM as the last drug and achieving SE control and patients receiving TPM as the last drug but without termination of SE.
Results
The literature search yielded 1164 results, with individual data available for 35 patients (six with SRSE) from four studies. SE was controlled in 68.6% of patients receiving TPM either as the last drug (20) or not (15), and in 14 of the 20 patients receiving TPM as the last drug (70%). Only six patients received TPM for SRSE; in five of them, TPM was administered as the last drug with resolution of SE in four. When comparing patients who did and did not receive TPM as the last drug, no statistically significant difference was found for any of the variables considered; similarly, no difference was found comparing patients receiving TPM as the last drug and achieving SE control with those receiving TPM as the last drug but without termination of SE.
Conclusions
The lack of a statistically significant difference is likely to be due to the small sample size. In only a few patients was TPM used for SRSE. There is an unmet need for high-quality studies to evaluate the role of TPM in GCSE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In this individual patient data analysis, the first to be conducted in status epilepticus (SE), we did not find any variable associated with a likely response to topiramate (TPM). However, considering the relatively small number of patients analyzed, the lack of a statistically significant difference may be due to statistical error type II. |
The number of patients with super-refractory status epilepticus (SRSE) treated to date with TPM is probably much lower than commonly reported and is definitely too small to draw any conclusion about its definite role in the treatment of this condition. |
There is still an unmet need for high-quality observational and interventional studies to evaluate the role of TPM in SE, including SRSE. |
1 Introduction
Status epilepticus (SE) is defined as “a condition resulting either from the failure of the mechanisms responsible for seizure termination or from the initiation of mechanisms, which lead to abnormally prolonged seizures” [1]. This condition represents a neurological and medical emergency with an estimated crude incidence of 10–41/100,000 patients per year, an age-standardized incidence ranging from 4.61/100,000 [2] to 18.3/100,000 [3], and an overall mortality of 20% [4–6]. SE carries a high risk of long-term consequences including death and, as such, it needs to be promptly recognized and adequately treated.
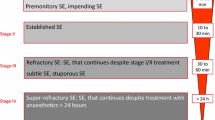
Generalized convulsive (tonic–clonic) SE (GCSE) is currently defined as a generalized tonic–clonic seizure lasting more than 5 min [1]. The treatment of GCSE usually follows a stepwise approach, with initial administration of benzodiazepines followed by intravenous antiepileptic drugs (AEDs) if seizure activity continues [5, 6]. After failure of first- and second-line treatments, a more aggressive approach consisting of anesthetics (propofol, pentobarbital, thiopentone, midazolam, or ketamine) is required [5, 6]. However, SE may continue or recur 24 h or more after the onset of anesthetic therapy, or may recur on reduction or withdrawal of anesthesia; this condition, which is associated with a mortality of 35% [7], has been termed “super-refractory status epilepticus” (SRSE) [8]. The prognosis of SE strongly depends on its duration, etiology, and intrinsic severity [9, 10]. However, data on these prognostic factors are usually lacking in trials assessing the efficacy of treatments for SE [11, 12].
Topiramate (TPM) is an AED that is effective against a broad spectrum of seizure types, possibly reflecting its multiple mechanisms of action. Topiramate has good oral bioavailability, linear kinetics, low protein binding, and no active metabolites [13]. In critically ill patients, TPM can be titrated relatively quickly and has been listed among possible therapeutic options for SRSE [7].
The aim of this systematic review with individual patient data analysis was to evaluate the role of topiramate (TPM) in GCSE, including SRSE.
2 Methods
A comprehensive review of the available literature was performed to minimize publication bias. We systematically searched MEDLINE, CENTRAL, LILACS, ClinicalTrials.gov, Google Scholar, and Opengrey.eu to identify studies assessing the role of TPM in the treatment of adult cases of GCSE and reporting individual patient data. Search strategies are reported in the Supplementary Material. Cases of post-anoxic SE and other subtypes of SE were excluded. Similarly, studies conducted in pediatric populations (<16 years of age) were excluded. To minimize the risk of selective outcome reporting we also excluded single case reports. There were no language restrictions. All searches were conducted on 10 October 2016.
Retrieved articles were independently evaluated for inclusion by two review authors; any disagreement was resolved through discussion.
The following individual patient data were collected: age, gender, weight, previous history of seizures, etiology (acute symptomatic, remote symptomatic, progressive symptomatic, epilepsy, unknown/not specified), EEG features, degree of impairment of consciousness, status epilepticus severity score (STESS) or Epidemiology-based Mortality score in SE (EMSE), number of AEDs at admission, number of AEDs prior to TPM administration, route of TPM administration, loading dose of TPM, maintenance dose of TPM, maximum daily dose of TPM, time from SE to TPM administration, time from TPM administration to response, control of SE (yes/no), need for intubation (yes/no), death (yes/no), TPM used as last AED (yes/no), name and order of AEDs used to treat SE.
Data were summarized using percentages, median, range, or mean and standard deviation, whichever was appropriate. Because TPM was not the last AED administered to all patients prior to termination of SE, we compared patients who received TPM as the last drug and those who did not. This comparison was performed to analyze whether there was any difference between the two groups that might help to identify some variables predicting a likely response to TPM. We also compared patients receiving TPM as the last drug and achieving SE control to patients receiving TPM as the last drug but without termination of SE.
Comparisons were conducted by analyzing variables such as: age, gender, previous history of seizures, etiology, number of AEDs prior to TPM, maximum daily dose of TPM, patients with SE controlled, number of deaths, and patients with TPM used as the last AED. Differences between groups were calculated using the Mann–Whitney U test, Chi-squared test, and Fisher’s exact test. A p value of <0.05 was considered statistically significant. A Bonferroni correction was applied to correct for multiple testing.
3 Results
The literature search yielded 1164 articles (MEDLINE: 119; ClinicalTrials.gov: 1; CENTRAL: 4; Opengrey.eu: 0; LILACS: 0; Google Scholar: 1040). After reading the full text, 15 articles initially considered for possible inclusion were eventually excluded (Fig. 1). Excluded articles with reasons for exclusion and number of patients receiving TPM for each excluded study are reported in the Supplementary Material. Individual patient data were available for 35 patients with GCSE (six of whom with SRSE) from four studies [14–17]. The studies from which individual patient data were extracted adopted retrospective [14, 15, 17] and prospective [16] designs.
Individual patient data extracted are reported in the Supplementary Material. Details on clinical features, treatment, and outcomes of patients and results of statistical analyses are reported in Tables 1, 2 and 3.
Despite our primary intention, it was impossible to analyze all variables initially considered because of lack of information for some of them. Hence, only the following data were analyzed: age, gender, previous history of seizures, etiology (acute symptomatic, remote symptomatic, progressive, epilepsy, unknown/not specified), number of AEDs prior to TPM administration, maximum daily dosage of TPM, control of SE (yes/no), death (yes/no), TPM used as last AED (yes/no), order of AEDs used to treat SE.
Thirty-five patients with GCSE (median age: 40 years; range: 16–92; 46% women) were included. In most cases (69%), the etiology underlying GCSE was acute symptomatic. In the majority of cases (69%), TPM was used as third-line AED to control SE. Among the 35 patients receiving TPM either as the last drugs (n = 20) or not (n = 15), SE was controlled in 69%. In six out of 35 patients (17%), TPM was used to control SE, which persisted after first-line and second-line treatments (benzodiazepine followed by AED) and despite the use of anesthetics (SRSE); in five out of these six cases, TPM was administered as the last drug, with a resolution of SE in four cases.
TPM was administered as the last drug in 57% of patients (20/35), leading to SE control in 14/20 (70%) cases.
No statistically significant difference was found for any of the variables considered when we compared patients who received TPM as the last drug to those who did not. The only difference was in the proportion of women, which was higher in those receiving TPM as the last drug (65 vs. 20%; p = 0.016); however, the statistical significance was lost after applying the Bonferroni correction for multiple comparisons (p > 0.05). Similarly, no difference was found comparing patients receiving TPM as the last drug and achieving SE control with those receiving TPM as the last drug but without termination of SE.
4 Discussion
This is the first attempt in the literature to perform an individual patient data analysis in SE. Rather than extracting aggregate data from published studies, individual patient data analyses are carried out using the original research data reported in primary studies or provided by the researchers responsible for each study. Individual patient data can then be re-analyzed and combined, if appropriate, into meta-analyses. Individual patient data analyses have the potential to answer questions not posed by individual studies or conventional meta-analyses, as they can improve data quality and the type of analyses, producing more reliable results [18]. As such, individual patient data analyses are considered the gold standard of review. However, as for conventional meta-analyses, their validity depends on the quality of the individual patient data obtained from primary studies.
The use of individual patient data analyses has been particularly advocated for the assessment of the efficacy of treatments for SE, a condition where several confounding factors are usually not adequately reported and analyzed with potential effect on the overall results [11, 19]. In this scenario, individual patient data analyses may enable the conduction of subgroup analyses not conducted by the original researchers, taking into account relevant prognostic aspects such as etiology and seizure type [19]. However, in order for these individual patient data analyses to be reliable, it is necessary that the data being analyzed are unbiased and complete for the variable(s) of interest.
Results of case reports including data on TPM in SE are likely to be affected by selective outcome reporting bias and positive-results publication bias, as favorable results have a higher chance of being reported and published. For this reason, data from case reports were not included in the present review and analyses. Individual patient data were extracted either from retrospective [14, 15, 17] or prospective [16] trials. In all these studies the potential risk for selective outcome reporting seems low, at least according to the details provided in the methods section of the published reports. Whether results obtained from these studies actually provide a reliable picture, however, remains unclear, as it is impossible to verify and quantify the existence and the amount of unpublished studies where TPM proved of limited utility in the treatment of SE. However, despite searching multiple databases to identify bibliographical references for gray literature, we were not able to retrieve additional studies.
Hence, it is difficult to understand whether individual patient data included and analyzed in the present review reflect the prognosis of an unbiased patient population treated with TPM for SE. In other terms, it is unclear whether the individual patient data collected and analyzed in our review are truly representative of patients treated with TPM for SE in terms of clinical and prognostic features.
However, even if the results had been obtained from unbiased sources, it would have been impossible to analyze the role of some prognostic factors such as duration of SE and its intrinsic severity (e.g., assessed with STESS, or EMSE), because of a lack of information on these variables.
Among the 35 patients receiving TPM either as the last drug or not, SE was controlled in 69%. Conversely, SE was terminated in 14 of 20 patients receiving TPM as the last drug (70%). We considered these patients receiving TPM as the last drug and achieving SE control as subjects in whom TPM was possibly/probably successful. However, it was impossible to adequately evaluate the definite efficacy of TPM because not all studies provided information on the time delay between TPM administration and SE resolution. Furthermore, not all studies specified whether modification of concomitant treatments were made in these patients.
No statistically significant difference was found when comparing patients who received TPM as the last drug for any of the variables considered and those who did not. Similarly, no difference was found comparing patients receiving TPM as the last drug and achieving SE control with those receiving TPM as the last drug but without termination of SE. The higher proportion of women found to have received TPM as the last drug was a false-positive result due to multiple comparisons, as the statistical significance was lost after applying the Bonferroni correction. Hence, we were unable to detect any variable associated with a likely response to TPM. However, considering the relatively small number of patients analyzed, the lack of a statistically significant difference may be likely due to statistical error type II.
Interestingly, in most cases TPM was used as second- (11%) or third-line (69%) AED to control SE. This finding is unexpected, as TPM is not recommended by any guidelines as treatment for SE persisting despite failure of first- and second-line treatments [20–24]. The use of TPM has been suggested as an option for SRSE, i.e., SE continuing or recurring 24 h or more after the onset of anesthetic therapy, or recurring on the reduction or withdrawal of anesthesia [7]. However, in the present review, only six patients (17%) received TPM for SRSE; in five of these cases, TPM was administered as the last drug with resolution of SE in four cases.
In the literature, after excluding case reports, there is only one study (not included in the present review as it did not provide individual patient data) specifically assessing the role of TPM in SRSE in adults [25], whereas one study has evaluated TPM in SE continuing despite two adequately dosed AEDs (i.e. “refractory SE”) [26]. In the SRSE study, among the 28 patients receiving TPM as the last drug and discontinuing intravenous anesthetics with no additional AEDs administered, cumulative cessation of RSE in patients was 4/35 (11%) at 1 day, 10/35 (29%) at 2 days, and 14/35 (40%) at 3 days [25]. This retrospective study represents the largest reported group of patients with SRSE treated with TPM and suggests that TPM might be useful in the treatment of this serious condition in adult patients.
In their review, Ferlisi and Shorvon reported that the published outcome of TPM in SRSE is “restricted to 60 cases (in 10 reports) treated with topiramate” [8]. However, a careful analysis of the data available in the literature indicates that the number of patients with SRSE treated to date with TPM is probably much lower than the reported figure, even after including pediatric patients [27]. This is due to the fact that studies conducted in “refractory SE” have high clinical heterogeneity, as they include both patients with SRSE and patients with SE refractory to first- and second-line treatments but not receiving anesthetics [15–17, 26, 28]. Hence, the number of patients treated with TPM for SRSE is certainly too small to draw any conclusion about its definite role in the treatment of this condition.
The lack of information on TPM in SE can also be attributed to the fact that, even when TPM is widely used, single outcomes are usually not reported. For instance, in a recent retrospective study, TPM was found to be used in 47 out of 341 patients (14%) [29], whereas in a 6-year cohort study TPM was administered as a third-line drug in 34 out of 171 patients (20%) [30]. These are just two examples of the wide use of TPM in clinical practice. However, the fact that none of them reported details on outcomes in subjects receiving TPM further highlights the need for studies reporting individual patient data.
5 Conclusions
No statistically significant difference was found for any of the variables considered when we compared patients who received TPM as the last drug to those who did not. Similarly, no difference was found comparing patients receiving TPM as the last drug and achieving SE control with those receiving TPM as the last drug but without termination of SE. As the present review demonstrates, despite their potential to answer questions not posed by individual studies or conventional meta-analyses, individual patient data analyses can do little if information has been obtained by biased studies or if data are incomplete. There is still an unmet need for high-quality observational and interventional studies to evaluate the role of TPM in SE, including SRSE. Several areas require attention in future research in the treatment of SE: investigators should use uniform definitions of SE and report results using clear and uniform methods to facilitate meta-analysis [11, 12]. Providing individual patient data is crucial, as they may be used to perform more detailed and informative analyses to assess the role of confounders.
References
Trinka E, Cock H, Hesdorffer D, Rossetti AO, Scheffer IE, Shinnar S, Shorvon S, Lowenstein DH. A definition and classification of status epilepticus: report of the ILAE task force on classification of status epilepticus. Epilepsia. 2015;56:1515–23.
Ong CT, Wong YS, Sung SF, Wu CS, Hsu YC, Su YH, et al. Underestimated rate of status epilepticus according to the traditional definition of status epilepticus. Sci World J. 2015;2015:801834.
Hesdorffer DC, Logroscino G, Cascino G, Annegers JF, Hauser WA. Incidence of status epilepticus in Rochester, Minnesota, 1965–1984. Neurology. 1998;50:735–41.
Rosenow F, Hamer HM, Knake S. The epidemiology of convulsive and nonconvulsive status epilepticus. Epilepsia. 2007;48(Suppl 8):82–4.
Trinka E, Höfler J, Leitinger M, Brigo F. Pharmacotherapy for status epilepticus. Drugs. 2015;75:1499–521.
Trinka E, Höfler J, Leitinger M, Rohracher A, Kalss G, Brigo F. Pharmacologic treatment of status epilepticus. Expert Opin Pharmacother. 2016;17:513–34.
Ferlisi M, Shorvon S. The outcome of therapies in refractory and super-refractory convulsive status epilepticus and recommendations for therapy. Brain. 2012;135:2314–28.
Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011;134:2802–18.
Rossetti AO, Alvarez V, Januel JM, Burnand B. Treatment deviating from guidelines does not influence status epilepticus prognosis. J Neurol. 2013;260:421–8.
Leitinger M, Kalss G, Rohracher A, Pilz G, Novak H, Höfler J, Deak I, Kuchukhidze G, Dobesberger J, Wakonig A, Trinka E. Predicting outcome of status epilepticus. Epilepsy Behav. 2015;49:126–30.
Brigo F, Storti M, Del Felice A, Fiaschi A, Bongiovanni LG. IV Valproate in generalized convulsive status epilepticus: a systematic review. Eur J Neurol. 2012;19:1180–91.
Prasad M, Krishnan PR, Sequeira R, Al-Roomi K. Anticonvulsant therapy for status epilepticus. Cochrane Database Syst Rev. 2014;9:CD003723.
Shank RP, Gardocki JF, Streeter AJ, Maryanoff BE. An overview of the preclinical aspects of topiramate: pharmacology, pharmacokinetics, and mechanism of action. Epilepsia. 2000;41(Suppl 1):S3–9.
Kim W, Kwon SY, Cho AH, Lim SC, Kim YI, Shon YM. Effectiveness of topiramate in medically complicated patients with status epilepticus or acute refractory seizures. J Epilepsy Res. 2011;1:52–6.
Hottinger A, Sutter R, Marsch S, Rüegg S. Topiramate as an adjunctive treatment in patients with refractory status epilepticus: an observational cohort study. CNS Drugs. 2012;26:761–72.
Asadi-Pooya AA, Jahromi MJ, Izadi S, Emami Y. Treatment of refractory generalized convulsive status epilepticus with enteral topiramate in resource limited settings. Seizure. 2015;24:114–7.
Stojanova V, Rossetti AO. Oral topiramate as an add-on treatment for refractory status epilepticus. Acta Neurol Scand. 2012;125:e7–11.
Stewart LA, Tierney JF. To IPD or not to IPD? Advantages and disadvantages of systematic reviews using individual patient data. Eval Health Prof. 2002;25:76–97.
Brigo F, Nardone R, Tezzon F, Trinka E. Nonintravenous midazolam versus intravenous or rectal diazepam for the treatment of early status epilepticus: a systematic review with meta-analysis. Epilepsy Behav. 2015;49:325–36.
Minicucci F, Muscas G, Perucca E, Capovilla G, Vigevano F, Tinuper P. Treatment of status epilepticus in adults: guidelines of the Italian League against Epilepsy. Epilepsia. 2006;47(Suppl 5):9–15.
Shorvon S, Baulac M, Cross H, Trinka E, Walker M, TaskForce on Status Epilepticus of the ILAE Commission for European Affairs. The drug treatment of status epilepticus in Europe: consensus document from a workshop at the first London Colloquium on Status Epilepticus. Epilepsia. 2008;49:1277–85.
Meierkord H, Boon P, Engelsen B, Göcke K, Shorvon S, Tinuper P, Holtkamp M, European Federation of Neurological Societies. EFNS guideline on the management of status epilepticus in adults. Eur J Neurol. 2010;17:348–55.
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, Laroche SM, Riviello JJ, Jr., Shutter L, Sperling MR, Treiman DM, Vespa PM, Neurocritical Care Society Status Epilepticus Guideline Writing Committee. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17:3–23.
Glauser T, Shinnar S, Gloss D, Alldredge B, Arya R, Bainbridge J, Bare M, Bleck T, Dodson WE, Garrity L, Jagoda A, Lowenstein D, Pellock J, Riviello J, Sloan E, Treiman DM. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the guideline committee of the american epilepsy society. Epilepsy Curr. 2016;16:48–61.
Synowiec AS, Yandora KA, Yenugadhati V, Valeriano JP, Schramke CJ, Kelly KM. The efficacy of topiramate in adult refractory status epilepticus: experience of a tertiary care center. Epilepsy Res. 2012;98:232–7.
Madžar D, Kuramatsu JB, Gerner ST, Huttner HB. Assessing the value of topiramate in refractory status epilepticus. Seizure. 2016;38:7–10.
Akyildiz BN, Kumandaş S. Treatment of pediatric refractory status epilepticus with topiramate. Childs Nerv Syst. 2011;27:1425–30.
Towne AR, Garnett LK, Waterhouse EJ, Morton LD, DeLorenzo RJ. The use of topiramate in refractory status epilepticus. Neurology. 2003;60:332–4.
Kortland LM, Alfter A, Bähr O, Carl B, Dodel R, Freiman TM, Hubert K, Jahnke K, Knake S, von Podewils F, Reese JP, Runge U, Senft C, Steinmetz H, Rosenow F, Strzelczyk A. Costs and cost-driving factors for acute treatment of adults with status epilepticus: a multicenter cohort study from Germany. Epilepsia. 2016. doi:10.1111/epi.13584.
Sutter R, Marsch S, Fuhr P, Kaplan PW, Rüegg S. Anesthetic drugs in status epilepticus: risk or rescue? A 6-year cohort study. Neurology. 2014;82:656–64.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study received no funding.
Conflict of interest
Dr. Francesco Brigo received speakers´ honoraria from Eisai and UCB Pharma. Prof. Eugen Trinka has acted as a paid consultant to Bial, Biogen Idec, Eisai, Ever Neuropharma, Medtronics, Takeda, Upsher-Smith, and UCB; has received speakers’ honoraria from Bial, Boehringer, Eisai, GL Lannacher, and UCB Pharma; and has received research funding from Biogen Idec, Merck, Novartis, Red Bull, UCB Pharma, the European Union, FWF (Österreichischer Fond zur Wissenschaftsförderung), and Bundesministerium für Wissenschaft und Forschung. Dr. Raffaele Nardone, Dr. Stanley C. Igwe, and Dr. Nicola Luigi Bragazzi report no conflicts of interest relevant to this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Brigo, F., Bragazzi, N.L., Igwe, S.C. et al. Topiramate in the Treatment of Generalized Convulsive Status Epilepticus in Adults: A Systematic Review with Individual Patient Data Analysis. Drugs 77, 67–74 (2017). https://doi.org/10.1007/s40265-016-0672-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-016-0672-2