Abstract
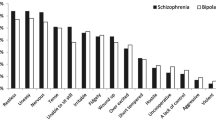
Psychomotor agitation is often associated with aggression. It is important to identify agitation early and achieve results quickly in order to prevent aggressive behavior. Strategies may include verbal de-escalation techniques, reduced stimulation, medications, or a combination of approaches. Historically, pharmacological treatments for agitation have been delivered using oral and intramuscular formulations. Although the types of medication available have not changed dramatically, different formulations have been developed recently to aid in treating this difficult condition. This paper will detail some of the newer, more novel formulations used to deliver medications to treat agitation. Formulations to be described include orally disintegrating tablets, sublingual, buccal and intranasal forms, as well as an inhalation form. Each form has a unique purpose and will aid in treatment of different populations at different levels of agitation. Of note, of the medication formulations to be discussed, only inhaled loxapine is FDA approved for acute agitation in schizophrenia and bipolar disorder and no medications are approved for ‘agitation’ outside of a specific disease state. The orally disintegrating tablets of olanzapine, risperidone, and aripiprazole are swallowed and enter the circulation via the portal system. They do not have a more rapid onset of action than the standard oral tablets but are useful for patients that might otherwise divert the medication. The sublingual, buccal and intranasal formulations include asenapine and midazolam. Absorption by this route is more rapid and avoids first-pass metabolism. Finally, inhaled loxapine enters the alveoli and appears quickly in the arterial circulation. All of these novel formulations require at least some cooperation but have the potential to prevent escalation and improve the experience of patients and could be considered when negotiation is possible.

Similar content being viewed by others
References
Holloman GH Jr, Zeller SL. Overview of project BETA: best practices in evaluation and treatment of agitation. West J Emerg Med. 2011;13:1–2.
Nordstrom K, Zun LS, Wilson MP, et al. Medical evaluation and triage of the agitated patient: consensus statement of the American Association for Emergency Psychiatry Project BETA Medical Evaluation Workgroup. West J Emerg Med. 2012;13(1):3–10.
Lindenmayer JP. The pathophysiology of agitation. J Clin Psychiatry. 2000;61(Suppl. 14):5–10.
Damsa C, Ikelheimer D, Adam E, et al. Heisenberg in the ER: observation appears to reduce involuntary intramuscular injections in a psychiatric emergency service. Gen Hosp Psychiatry. 2006;28(5):431–3.
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–76.
Richmond JS, Berlin JS, Fishkind AB, et al. Verbal de-escalation of the agitated patient: consensus statement of the American Association for Emergency Psychiatry Project BETA De-escalation Workgroup. West J Emerg Med. 2012;13(1):17–25.
Wilson MP, Pepper D, Currier GW, et al. The psychopharmacology of agitation: consensus statement of the American Association for Emergency Psychiatry Project BETA Psychopharmacology Workgroup. West J Emerg Med. 2012;13(1):26–34.
American Society of Health-System Pharmacists. Introduction to Pharmacokinetics and Pharmacodynamics [online]. http://www.ashp.org/DocLibrary/Bookstore/P2418-Chapter1.aspx.
Leucht S, Komossa K, Rummel-Kluge C, et al. A meta-analysis of head-to-head comparisons of second-generation antipsychotics in the treatment of schizophrenia. Am J Psychiatry. 2009;166(2):152–63.
Robinson DG, Woerner MG, Napolitano B, et al. Randomized comparison of olanzapine versus risperidone for the treatment of first-episode schizophrenia: 4-month outcomes. Am J Psychiatry. 2006;163(12):2096–102.
McEvoy JP, Lieberman JA, Perkins DO, et al. Efficacy and tolerability of olanzapine, quetiapine, and risperidone in the treatment of early psychosis: a randomized, double-blind 52-week comparison. Am J Psychiatry. 2007;164(7):1050–60.
Marder SR, McQuade RD, Stock E, et al. Aripiprazole in the treatment of schizophrenia: safety and tolerability in short-term, placebo-controlled trials. Schizophr Res. 2003;61(2–3):123–36.
Potkin SG, Saha AR, Kujawa MJ, et al. Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry. 2003;60(7):681–90.
Tohen M, Sanger TM, McElroy SL, et al. Olanzapine versus placebo in the treatment of acute mania. Am J Psychiatry. 1999;156(6):702–9.
Tohen M, Calbrese JR, Sachs GS, et al. Randomized, placebo-controlled trial of olanzapine as maintenance therapy in patients with bipolar I disorder responding to acute treatment with olanzapine. Am J Psychiatry. 2006;163(2):247–56.
Perlis RH, Baker RW, Zarate CA Jr, et al. Olanzapine versus risperidone in the treatment of manic or mixed States in bipolar I disorder: a randomized, double-blind trial. J Clin Psychiatry. 2006;67(11):1747–53.
Lieberman JA, Tollefson G, Tohen M, et al. Comparative efficacy and safety of atypical and conventional antipsychotic drugs in first-episode psychosis: a randomized, double-blind trial of olanzapine versus haloperidol. Am J Psychiatry. 2003;160(8):1396–404.
Package Insert for Zyprexa. http://pi.lilly.com/us/zyprexa-pi.pdf.
Montgomery W, Treuer T, Karagianis J, et al. Orally disintegrating olanzapine review: effectiveness, patient preference, adherence, and other properties. Patient Preference Adherence. 2012;6:109–25.
Bettinger TL, Mendelson SC, Dorson PG, Crismon ML. Olanzapine-induced glucose dysregulation. Ann Pharmacother. 2000;34:865–7.
Fertig MK, Brooks VG, Shelton PS. Hyperglycemia associated with olanzapine. J Clin Psychiatry. 1998;59:687–9.
Gatta B, Rigalleau V, Gin H. Diabetic ketoacidosis with olanzapine treatment. Diabetes Care. 1999;22:1002–3.
Goldstein LE, Sporn J, Brown S, Kim H, Finkelstein J, Gaffey GK, Sachs G, Stern TA. New-onset diabetes mellitus and diabetic ketoacidosis associated with olanzapine treatment. Psychosomatics. 1999;40:438–43.
Melkersson KI, Hulting AL, Brismar KE. Elevated levels of insulin, leptin, and blood lipids in olanzapine-treated patients with schizophrenia or related psychoses. J Clin Psychiatry. 2000;61:742–9.
Lindenmayer J-P, Nathan A, Smith RC. Hyperglycemia associated with the use of atypical antipsychotics. J Clin Psychiatry. 2001;62(Suppl. 23):30–8.
Osser DN, Najarian DM, Dufresne RL. Olanzapine increases weight and serum triglyceride levels. J Clin Psychiatry. 1999;60:767–70.
Karagianis J, Grossman L, Landry J, et al. A randomized controlled trial of the effect of sublingual orally disintegrating olanzapine versus oral olanzapine on body mass index: the PLATYPUS study. Schizophr Res. 2009;113(1):41–8.
Bobo WV, Epstein RA, Shelton RC. Effects of orally disintegrating vs regular olanzapine tablets on body weight, eating behavior, glycemic and lipid indices, and gastrointestinal hormones: a randomized, open comparison in outpatients with bipolar depression. Ann Clin Psychiatry. 2011;23(3):193–201.
Chue P, Jones B, Taylor CC, Dickson R. Dissolution profile, tolerability, and acceptability of the orally disintegrating olanzapine tablet in patients with schizophrenia. Can J Psychiatry. 2002;47(8):771–4.
Seager H. Drug-delivery products and the Zydis fast-dissolving dosage form. J Pharm Pharmacol. 1998;50(4):375–82.
Hori H, Ueda N, Yoshimura R, et al. Olanzapine orally disintegrating tablets (Zyprexa Zydis) rapidly improved excitement components in the acute phase of first-episode schizophrenic patients: an open-label prospective study. World J Biol Psychiatry. 2009;10(4 Pt 3):741–5.
Kinon BJ, Hill AL, Liu H, Kollack-Walker S. Olanzapine orally disintegrating tablets in the treatment of acutely ill non-compliant patients with schizophrenia. Int J Neuropsychopharmacol. 2003;6(2):97–102.
Hirschfeld RMA, Keck PE, Kramer M, et al. Rapid antimanic effect of risperidone monotherapy: a 3-week multicenter, double-blind, placebo-controlled trial. Am J Psychiatry. 2004;161(6):1057–65.
Khanna S, Vieta E, Lyons B, et al. Risperidone in the treatment of acute mania: double-blind, placebo-controlled study. Br J Psychiatry. 2005;187:229–34.
Perlis RH, Wlege JA, Vornik LA, et al. Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2006;67(4):509–16.
Schooler N, Rabinowitz J, Davidson M, et al. Risperidone and haloperidol in first-episode psychosis: a long-term randomized trial. Am J Psychiatry. 2005;162(5):947–53.
Wang CY, Xiang YT, Cai ZJ, et al. Risperidone maintenance treatment in schizophrenia: a randomized, controlled trial. Am J Psychiatry. 2010;167(6):676–85.
Subotnik KL, Nuechterlein KH, Ventura J, et al. Risperidone nonadherence and return of positive symptoms in the early course of schizophrenia. Am J Psychiatry. 2011;168(3):286–92.
Pandina G, Kushner S, Karcher K, Haas M. An open-label, multicenter evaluation of the long-term safety and efficacy of risperidone in adolescents with schizophrenia. Child Adolesc Psychiatry Ment Health. 2012;6(1):23.
Komossa K, Rummel-Kluge C, Schwarz S, et al. Risperidone versus other atypical antipsychotics for schizophrenia. Cochrane Database Syst Rev. 2011; 19(1):CD006626.
van Schaick EA, Lechat P, Remmerie BMM, et al. Pharmacokinetic comparison of fast-disintegrating and conventional tablet formulations of risperidone in healthy volunteers. Clin Therapeutic. 2003;25(6):1687–99.
Thyssen A, Remmerie B, D’Hoore P, et al. Rapidly disintegrating risperidone in subjects with schizophrenia or schizoaffective disorder: a summary of ten phase I clinical trials assessing taste, tablet disintegration time, bioequivalence, and tolerability. Clin Therapeutic. 2007;29(2):290–304.
Normann C, Schmaub M, Bakri N, et al. Initial treatment of severe acute psychosis with fast orally disintegrating risperidone tablets. Pharmacopsychiatry. 2006;39:209–12.
Package Insert for Abilify. http://www.abilify.com/pdf/pi.aspx.
DeBoer AG, De Leede LG, Breimer DD. Drug absorption by sublingual and rectal routes. Br J Anaesth. 1984;56:69–82.
McIntyre RS. Asenapine: a review of acute and extension phase data in bipolar disorder. CNS Neurosci Ther. 2011;17(6):645–8.
Saphris (asenapine) package insert. Kenilworth: Schering-Plough (Merck & Co., Inc.). 2009.
Citrome L. Asenapine for schizophrenia and bipolar disorder: a review of the efficacy and safety profile for this newly approved sublingually absorbed second-generation antipsychotic. Int J Clin Pract. 2009;63(12):1762–84.
McIntyre RS, Cohen M, Zhao J, et al. A 3-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord. 2009;11(7):673–86.
Henry JM, Fuller MA. Asenapine: a new antipsychotic option. J Pharm Pract. 2011;24(5):447–51.
Weber J, McCormack PL. Asenapine. CNS Drugs. 2009;23(9):781–92.
Gerrits M, de Greef R, Peeters P. Effect of absorption site on the pharmacokinetics of sublingual asenapine in healthy male subjects. Biopharm Drug Dispos. 2010;31(5–6):351–7.
Dubovsky SL, Frobose C, Phiri P, et al. Short-term safety and pharmacokinetic profile of asenapine in older patients with psychosis. Int J Geriatr Psychiatry. 2012;27(5):472–82.
Package insert for Saphris: http://www.merck.com/product/usa/pi_circulars/s/saphris/saphris_pi.pdf.
Reeves JG, Fragen RJ, Vinik R, Greenblatt DJ. Midazolam: pharmacology and uses. Anesthesiol. 1985;62:310–24.
Smith MT, Eadie MJ, Brophy TO. The pharmacokinetics of midazolam in man. Eur J Clin Pharmacol. 1981;19:271–8.
Allonen H, Ziegler G, Klotz U. Midazolam kinetics. Clin Pharmacol Ther. 1981;30:653.
Kogan A, Katz J, Efrat R, Eidelman LA. Premedication with midazolam in young children: a comparison of four routes of administration. Paediatr Anaesth. 2002;12(8):685–9.
Du Cailar J, Holzer J, Jullien Y, Passeron D. Hypnotic efficacy of midazolam in pre-surgical patients: a dose-finding study. Br J Clin Pharmacol. 1983;16(Suppl. 1):129–32.
Beck H, Salom M, Holzer J. Midazolam dosage studies in institutionalized geriatric patients. Br J Clin Pharmacol. 1983;16(Suppl. 1):133–7.
Khanderia U, Pandit SK. Use of midazolam hydrochloride in anesthesia. Clin Pharm. 1987;6(7):533–47.
Schläppi B. Safety aspects of midazolam. Br J Clin Pharmacol. 1983;16(Suppl. 1):37–41.
Popoviciu L, Corfariu O. Efficacy and safety of midazolam in the treatment of night terrors in children. Br J Clin Pharmacol. 1983;16(Suppl. 1):97–102.
Rivera R, Segnini M, Baltodano A, Pérez V. Midazolam in the treatment of status epilepticus in children. Crit Care Med. 1993;21(7):991–4.
Lachnit KS, Proszowski E, Rieder L. Midazolam in the treatment of sleep disorders in geriatric patients. Br J Clin Pharmacol. 1983;16(Suppl. 1):173–7.
McDonough JH, Van Shura KE, LaMont JC, et al. Comparison of the intramuscular, intranasal or sublingual routes of midazolam administration for the control of soman-induced seizures. Basic Clin Pharmacol Toxicol. 2009;104(1):27–34.
Layangool T, Sangtawesin C, Kirawittaya T, et al. A comparison of oral chloral hydrate and sublingual midazolam sedation for echocardiogram in children. J Med Assoc Thai. 2008;91(Suppl. 3):45–52.
Scott RC, Besag FMC, Boyd SG, et al. Buccal absorption of midazolam: pharmacokinetic and EEG pharmacodynamics. Epilepsia. 1998;39(3):290–4.
Schwagmeier R, Alincic S, Striebel HW. Midazolam pharmacokinetics following intravenous and buccal administration. Br J Clin Pharmacol. 1998;46(3):203–6.
Karl HW, Rosenberger JL, Larach MG, Ruffle JM. Transmucosal administration of midazolam for premedication of pediatric patients: comparison of the nasal and sublingual routes. Anesthesiol. 1993;78(5):885–91.
Wilton NCT, Leigh J, Rosen DR, Pandit UA. Preanesthetic sedation of preschool children using intranasal midazolam. Anesthesiol. 1988;69:972–5.
Walberg EJ, Wills RJ, Eckhert J. Plasma concentrations of midazolam in children following intranasal administration. Anesthesiol. 1991;74:233–5.
Zedie N, Amory D, Wagner BHJ, O’Hara DA. Comparison of intranasal midazolam and sufentanil premedication in pediatric outpatients. Clin Pharmacol Ther. 1996;59:341–8.
Wermeling DP, Record KA, Kelly TH, et al. Pharmacokinetics and pharmacodynamics of a new intranasal midazolam formulation in healthy volunteers. Anesth Analg. 2006;103:344–9.
Chakrabarti A, Bagnall AM, Chue P, et al. Loxapine for schizophrenia. Cochrane Database for Systematic Reviews. Cochrane Library. Issue 1 (2007).
Goldschmidt TJ, Burch EA. Use of loxapine to treat a patient with psychotic depression. Am J Psychiatry. 1982;139:946–7.
Vanelle JM, Olie JP, Levy-Soussan P. New antipsychotics in schizophrenia: the French experience. Acta Psychiatr Scand Suppl. 1994;380:59–63.
Singh AN, Barlas C, Singh S, Franks P, Mishra RK. A neurochemical basis for the antipsychotic activity of loxapine: interactions with dopamine D1, D2, D4 and serotonin 5-HT2 receptor subtypes. J Psychiatry Neurosci. 1996;21(1):29–35.
Fruensgaard K, Wollenberg J, Hansen KM, Fensbo C, Sihm F. Loxapine versus perphenazine in psychotic patients: a double-blind, randomized, multicenter trial. Curr Med Res Opin. 1978;5(8):601–7.
Simpson GM, Cuculic Z. A double-blind comparison of loxapine succinate and trifluoperazine in newly admitted schizophrenic patients. J Clin Pharmacol. 1976;16:60–5.
Rabinowitz JD, Wensley M, Lloyd P, et al. Fast onset medications through thermally generated aerosols. J Pharmacol Exp Ther. 2004;309(2):769–75.
Rabinowitz JD, Lloyd PM, Munzar P, et al. Ultra-fast absorption of amorphous pure drug aerosols via deep lung inhalation. J Pharm Sci. 2006;95(11):2438–51.
Dinh KV, Myers DJ, Noymer PD, Cassella JV. In vitro aerosol deposition in the oropharyngeal region for Staccato loxapine. J Aerosol Med Pulm Drug Deliv. 2010;23(4):253–60.
Spyker DA, Munzar P, Cassella JV. Pharmacokinetics of loxapine following inhalation of a thermally generated aerosol in healthy volunteers. J Clin Pharmacol. 2010;50(2):169–79.
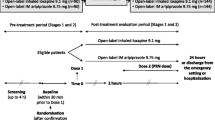
Allen MH, Feifel DA, Lesem MD, Zimbroff DL, Ross R, Spyker DA, Cassella JV. Efficacy and safety of loxapine for inhalation in the treatment of acute agitation in patients with schizophrenia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72(10):1313–21.
Lesem MD, Tran-Johnson TK, Riesenberg RA, et al. Rapid acute treatment of agitation in individuals with schizophrenia: multicenter, randomized, placebo-controlled study of inhaled loxapine. Br J Psychiatry. 2011;198(1):51–8.
Kwentus J, Riesenberg RA, Marandi M, et al. Rapid acute treatment of agitation in patients with bipolar I disorder: a multicenter, randomized, placebo-controlled clinical trial with inhaled loxapine. Bipolar Disord. 2012;14:31–40.
Adasuve REMS Information. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/.
Allen MH, Currier GW, Carpenter D, Ross R, Docherty JP. Expert consensus guideline series: treatment of behavioral emergencies 2005. J Psychiatr Pract. 2005;11(Suppl. 1):1–108.
Pharmacokinetic definitions sources: medical dictionary/MedLine Plus © 2013, Merriam-Webster, Incorporated; Gale Encyclopedia of Medicine © 2008, The Gale Group, Inc.; McGraw-Hill Concise Dictionary of Modern Medicine© 2002, The McGraw-Hill Companies, Inc.
Acknowledgments
Drs. Nordstrom and Allen were supported in part by the VISN 19 Mental Illness Research, Education and Clinical Center. This work does not necessarily represent the views of the Department of Veterans Affairs or the United States Government. Dr. Nordstrom has participated in an advisory board for Alexza Pharmaceuticals. Dr. Allen had or has relationships with: Alexza Pharmaceuticals, Sunovion Pharmaceuticals, Dainippon Sumitomo Pharma Japan, inVentiv Health, and Bracket.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nordstrom, K., Allen, M.H. Alternative Delivery Systems for Agents to Treat Acute Agitation: Progress to Date. Drugs 73, 1783–1792 (2013). https://doi.org/10.1007/s40265-013-0130-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-013-0130-3