Abstract
Introduction
Additional risk minimisation measures (aRMMs) may be required to minimise important risks of medicines. aRMMs may be required at the time of authorisation, but may also be introduced or discontinued during the product life cycle as new safety information arises. The aim of this study is to describe post-authorisation introductions of new aRMMs and discontinuations of existing aRMMs for medicines authorised in the European Union (EU).
Methods
We performed a retrospective cohort study that included all new active substances authorised through the EU centralised procedure between January 1st 2006 and December 31st 2017. Data was extracted from European Public Assessment Reports available on the website of the European Medicines Agency (ema.europa.eu). Medicines were followed up from the date of marketing authorisation (MA) until first introduction or discontinuation of aRMMs, excluding Direct Healthcare Professional Communications (DHPCs), withdrawal/suspension/revocation of the MA, or July 1st 2018, when data extraction took place. Descriptive statistics were used to analyse frequency data, and survival analysis was used to calculate 5- and 10-year probability of introduction or discontinuation of aRMMs.
Results
A total of 476 medicines were authorised during the study period. The probability of getting aRMMs after authorisation for products authorised without aRMMs was 3.5% [95% confidence interval (CI) 1.2–5.7] within 5 years after authorisation and 6.9% (95% CI 2.6–11) within 10 years after authorisation. For products authorised with aRMMs, the probability of discontinuation of aRMMs was 0.9% (95% CI 0–2.6) within 5 years and 8.3% (95% CI 0–16.1) within 10 years after authorisation.
Conclusions
We found low probabilities of introduction and discontinuation of aRMMs (excluding DHPCs) during the product life cycle for medicines authorised between 2006 and 2017. The low rate of discontinuation may potentially be due to a lack of robust data on effectiveness of aRMMs. Further research is needed to get more insight into the dynamics of aRMMs during the medicine life cycle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Medicines authorised between 2006 and 2017 without additional risk minimisation measures (aRMMs) have a low probability that aRMMs will be introduced within 5 and 10 years after authorisation, and medicines authorised with aRMMs during that period have a low probability that aRMMs will be discontinued. |
Post-authorisation introduction of aRMMs is most often triggered by new safety information arising from spontaneous reports or clinical trials. |
The role of effectiveness evaluation of aRMMs in the life cycle management of medicines is currently unclear. |
1 Introduction
The European Union Risk Management Plan (EU-RMP) has become an integral tool in the proactive life cycle management of medicinal products and facilitates identification, characterisation, monitoring, and minimisation of risks. The EU-RMP first became a mandatory part of the authorisation dossier of innovative medicinal products authorised in the European Union (EU) in November 2005, and became mandatory for all medicinal products in 2012 [1, 2]. The EU-RMP consists of three key components: the safety specification, the pharmacovigilance plan and the risk minimisation plan [3]. The safety specification describes the safety data available for the medicinal product, with focus on those safety concerns that require further activities post-authorisation. These safety concerns are listed as important identified risks, important potential risks and missing information. The pharmacovigilance plan describes the methods used to monitor and/or further characterise the important risks described in the safety specification. The risk minimisation plan describes the measures to minimise the important risks [3].
Routine risk minimisation measures are in place for all medicinal products, for example, the Summary of Product Characteristics (SPC), Patient Information Leaflet, pack design, and prescription status. However, some medicinal products may be associated with important risks that may not be sufficiently minimised by these routine measures alone. Additional risk minimisation measures (aRMMs) may be needed to ensure that the benefits of these products outweigh their risks. Types of aRMMs include educational materials that provide information to healthcare professionals and/or patients regarding risks on top of the information in the SPC; controlled access, in which prescription or dispensing of a medicinal product is conditional on fulfilling certain criteria (i.e. following a training programme or performing certain diagnostic testing); controlled distribution, in which all stages of the product distribution are tracked; and pregnancy prevention programmes, which may include one or more of the measures described above [3, 4]. aRMMs are conditions to the marketing authorisation (MA) and are therefore listed in annex IID of the MA, “Conditions and restrictions with regard to the safe and effective use of the product”.
A need for aRMMs is assessed at the time of the authorisation. Studies have shown that, between 2006 and 2015, the proportion of products with aRMMs at the time of authorisation ranged from 26 to 42% [5,6,7,8]. However, risk management is an iterative process that is continuously applied throughout the product life cycle. New information regarding risks may become available post-authorisation, requiring introduction of new aRMMs or strengthening of already existing aRMMs. Conversely, new information regarding risks post-authorisation may also allow for the reduction or discontinuation of existing aRMMs. Currently, there are no published data on post-authorisation changes to aRMMs for products authorised in Europe, which translates to an important deficit in our knowledge regarding the life cycle management of medicinal products.
The aim of this study is to describe post-authorisation introductions and discontinuations of aRMMs for medicinal products authorised in the EU.
2 Methods
2.1 Study Design
We performed a retrospective cohort study that included all new active substances authorised through the centralised procedure between January 1st 2006 and December 31st 2017. Medicinal products included in our study were followed up from the date of MA until the first occurrence of an introduction or discontinuation of aRMMs, withdrawal, suspension, or revocation of the MA, or the date of data extraction (July 1st 2018), whichever came first. One or more types of aRMM can be introduced or discontinued simultaneously.
2.2 Data Sources and Setting
We extracted all centrally authorised medicines from the website of the European Medicines Agency (EMA) on www.ema.europa.eu. We excluded non-innovator applications, such as generic applications, as they have an EU-RMP aligned with the reference product. EMA publishes European Public Assessment Reports (EPARs) for all products authorised through the centralised procedure. We extracted data from the following EPARs: the “EPAR—Public assessment report”, the “EPAR—Product information”, and the “EPAR—Procedural steps taken and scientific information after authorisation”. The “EPAR—Public assessment report” is the summary of the initial assessment of the MA application and includes a summary of the RMP at the time of authorisation. The “EPAR—Product information” includes the most up-to-date product information with the annexes of the MA. The “EPAR—Procedural steps taken and scientific information after authorisation” is a log of all variations to the MA, i.e. any changes in the administrative information (such as transfers of the MA), changes in the manufacturing process, and changes in the benefit–risk profile of the product.
2.3 Study Outcomes
Our main outcome was either the first introduction of aRMM(s) for medicines without aRMMs at the time of authorisation or the first discontinuation of at least one of the aRMMs for medicines with aRMMs at the time of authorisation.
We identified products with post-authorisation introduction or discontinuation of aRMMs in two ways to ensure completeness. First, for all products included in the study, the “EPAR—Public assessment report” was reviewed to identify whether aRMMs were in place at the time of MA and the “EPAR—Product information” was reviewed to identify whether aRMMs were in place at the time of data extraction. A discrepancy between these two EPARs was regarded as a change (considered an introduction if the aRMM was not in the initial RMP, but present in annex IID, and a discontinuation if vice versa). Secondly, for all products included in the study, we reviewed the “EPAR—Procedural steps taken and scientific information after authorisation”. All regulatory procedures that included amendments to annex II of the MA were screened to identify whether aRMMs were introduced or discontinued.
We also used the “EPAR—Procedural steps taken and scientific information after authorisation” to identify the regulatory procedure in which the introduction or discontinuation occurred and find the corresponding EPAR.
2.4 Covariates
The following information was extracted from the EPARs for all products included in our study: active substance, Anatomical Therapeutic Chemical (ATC) classification first level, date and type of MA, authorisation status (authorised, suspended, withdrawn), orphan designation (yes/no), aRMMs at the time of MA (yes/no), aRMMs at the time of data extraction (yes/no), and type of aRMMs.
Categorisation of the type of aRMM was based on the current definitions as laid down in the “Good pharmacovigilance practices (GVP)” (module XVI rev 2) guidelines of the EMA, as described in Table 1 [4, 5]. Direct Healthcare Professional Communications (DHPCs) were not included in our study, as these are generally not included in annex IID of the MA and could not be systematically collected from the website of the EMA. One product can have one or more types of aRMM. Educational materials targeting healthcare professionals and educational materials targeting patients and/or caregivers were counted as different categories of aRMMs.
The type of MA was categorised as regular MA, conditional MA, or MA under exceptional circumstances [1, 9].
For products with introduction or discontinuation of aRMMs, we extracted the following information from the EPAR of the corresponding regulatory procedure: the date of the amendment, the risk addressed with aRMMs, categorisation of the risk in the EU-RMP, and the sources of the evidence that formed the basis for the introduction or discontinuation of the aRMM.
Categorisation of risks in the EU-RMP was based on the current definitions as laid down in GVP module V rev 2, i.e. important identified risks, important potential risks, and areas of missing information [3]. We categorised sources of evidence that formed the bases for the variation to the MA as non-clinical studies, clinical trials, observational studies, and spontaneous reports. We also assessed whether aRMMs were imposed on medicines following EU referral procedures, i.e. (urgent) reviews of the benefit–risk balance of a medicine or class of medicines due to quality, safety, or efficacy issues.
2.5 Data Analysis
Descriptive statistics were used to provide frequency data. We used Pearson’s χ2 test or Fisher’s exact test to investigate differences in categorical covariates between products with and without introduction or discontinuation of aRMMs.
To account for the time needed to accumulate sufficient data as justification for an introduction or discontinuation, we calculated the probability of introduction or discontinuation of aRMMs within 5 and 10 years after authorisation, using Kaplan–Meier survival analysis. The cut-offs of 5 and 10 years are of particular interest, since MAs in the EU have initial duration of 5 years, after which the MA may be renewed with unlimited validity following a re-examination of the benefit–risk balance. Additionally, 10 years is the duration of market protection for innovative medicines.
All analyses were conducted using Microsoft Excel and R version 3-6-1.
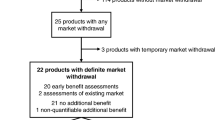
3 Results
We identified 476 medicinal products authorised during the study period (January 2006–December 2017), with a total of 32.514 months of follow-up. The median follow-up time was 60 months (range 8–150). The characteristics of the products included in the study are presented in Table 2. Of the 476 products, 91% were granted regular MA, 4% were granted conditional MA, and 5% were granted MA under exceptional circumstances; 18% were intended for treatment of an orphan disease. Of the 476 products, 27% concerned “Antineoplastic and immunomodulatory agents”, 19% concerned “Antiinfectives for systemic use”, and 12% concerned medicines targeting the “Alimentary tract and metabolism”. aRMMs were required at the time of authorisation for 27% (n = 130) of the products. For all 130 products with aRMMs at the time of authorisation, the aRMMs included the provision of educational materials targeted at healthcare professionals in 94% and at patients in 55%. For 14% (n = 18) of the products with aRMMs, other measures were required in addition to the educational materials. This included two products that had controlled distribution and a pregnancy prevention programme (ambrisentan, pomalidomide) and one product that had controlled access and a pregnancy prevention programme (sitaxentan sodium). At the time of data collection (July 2018), 91% of the products were still authorised, 9% of the products had been withdrawn, and for one product, the MA had been suspended (autologous cultured chondrocytes). Medicines with aRMMs at the time of MA had an orphan designation more often than medicines without aRMMs at the time of MA. There were no other significant differences in product characteristics between medicines authorised without and with aRMMs.
During the study period, aRMMs were introduced for 14 of 346 products authorised without aRMMs. All 14 aRMMs introduced post-authorisation included the provision of educational materials, which were aimed at healthcare professionals in 12 products (86%) and at patients or caregivers in seven (50%). For two products [gadoversetamide and split influenza virus inactivated, containing antigen equivalent to A/California/07/2009 (H1N1)-derived strain used NYMC X-179A], controlled distribution systems were introduced in addition to the educational materials. Among the 14 medicines for which aRMMs were introduced post-authorisation, one (antithrombin alfa) was authorised under exceptional circumstances and one (velaglucerase alfa) was intended for the treatment of an orphan disease. For the 14 medicines where aRMMs were introduced post-authorisation, five (36%) targeted “Blood and blood forming organs”, three (21%) were “Antiinfectives for systemic use”, and two (14%) targeted the “Musculoskeletal system”. The remaining four belonged to the ATC groups “Alimentary tract and metabolism”, “Antineoplastic and immunomodulatory agents”, “Nervous system”, and “Various”. Of the 14 medicines with introduction of aRMMs post-authorisation, 11 were still authorised and three [gadoversetamide, ferumoxytol, and split influenza virus inactivated, containing antigen equivalent to A/California/07/2009 (H1N1)-derived strain used NYMC X-179A] were voluntarily withdrawn from the market at the time of data collection (July 2018) (Table 2).
aRMMs were discontinued for four of 130 medicines authorised with aRMMs during the study period. The products for which aRMMs were discontinued post-authorisation all had regular MA, and none had an orphan designation. The four medicines for which aRMMs were discontinued post-authorisation belonged to the ATC groups “Blood and blood forming organs”, “Antiinfectives for systemic use”, “Respiratory system”, and “Various”. All aRMMs were discontinued for these four products. The discontinued aRMMs involved educational materials targeted at healthcare professionals for all four medicines and educational materials targeted at patients/caregivers for two medicines. All four medicines for which aRMMs were discontinued post-authorisation were still authorised at the time of data collection (Table 2).
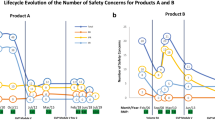
The median follow-up time for medicines for which aRMMs were introduced post-authorisation was 43 months (range 17–137 months), and the median follow-up time for medicines for which aRMMs were discontinued was 90 months (range 25–96 months) (Table 2). The probability of introduction of aRMMs post-authorisation for medicines without aRMM at authorisation was 3.5% [95% confidence interval (CI) 1.2–5.7] within 5 years after authorisation and 6.9% (95% CI 2.6–11) within 10 years after authorisation. For medicines with aRMMs at authorisation, the probability of discontinuation of aRMMs was 0.9% (95% CI 0–2.6) within 5 years and 8.3% (95% CI 0–16.1) within 10 years after authorisation (Figs. 1 and 2).
Table 3 describes the safety concerns and sources of evidence for the medicines for which aRMMs were introduced or discontinued. The aRMMs of the 14 products introduced post-authorisation addressed 21 safety concerns (median 1, range 1–3), of which 57% involved important identified risks, 38% important potential risks, and 5% missing information. The data sources that triggered the introduction of aRMMs post-authorisation concerned spontaneous reports (64%), post-authorisation clinical trials (50%), observational studies (21%), and non-clinical studies (14%). These percentages do not add up to 100% since multiple sources of evidence could form the basis for the introduction of aRMMs post-authorisation. aRMMs were imposed on gadoversetamide following an EU review of the benefit–risk balance (referral) of gadolinium-containing contrast agents in light of the risk of nephrogenic systemic fibrosis.
The aRMMs of the four products that were discontinued post-authorisation addressed ten safety concerns (median 2, range 1–5), of which 40% involved important identified risks, 40% important potential risks, and 20% missing information. For the discontinuation of aRMMs, the sources of evidence were a non-clinical study (25%) and an observational study (25%). The observational study was a multi-database drug-utilisation study for indacaterol maleate, which was authorised only for use in chronic obstructive pulmonary disease, and had aRMMs to reduce the risks associated with off-label use in asthma; the authors concluded that there was little to no off-label use of indacaterol in the EU [10]. The data sources could not be identified in two products (50%).
4 Discussion
The aim of our study was to describe discontinuations and introductions of aRMMs post-authorisation for centrally authorised medicinal products in the EU. We assessed the probability of post-authorisation introduction or discontinuation of aRMMs, rather than proportions, to account for the time required to accumulate sufficient data as justification for an introduction or discontinuation. During the study period, the probability of post-authorisation introduction of aRMMs was 3.5% (95% CI 1.2–5.7) within 5 years and 6.9% (95% CI 2.6–11) within 10 years after authorisation, while the probability of discontinuation of aRMMs was 0.9% (95% CI 0–2.6) within 5 years and 8.3% (95% CI 0–16.1) within 10 years after authorisation.
The probability of introduction of aRMMs within 5 and 10 years in our study is low. Besides introduction of aRMMs, regulatory action for safety issues emerging post-authorisation may include further investigation/monitoring, changes to routine risk minimisation measures, or suspension/revocation of the MA. Studies have shown that the vast majority of important post-authorisation safety issues are either investigated further or monitored, or are sufficiently minimised through routine risk minimisation measures [11]. Moreover, the probability of introduction of aRMMs within 5 and 10 years post-authorisation found in our study is lower than the probability of safety-related DHPC post-authorisation in a study that investigated whether the probability of DHPCs increased with increasing level of innovation of medicines [12]. DHPCs are listed as a type of aRMM in GVP module XVI rev 2, but differ from the aRMMs investigated in our study due to their one-off mode of action and broader scope of use. Between 1 January 1999 and 1 January 2009, 157 DHPCs were sent out for 112 different active substances available in the Netherlands, and 131 DHPCs were issued between 1 January 2010 and 31 December 2014 in the UK. [13, 14].
Spontaneous reports and clinical trials were the most frequent triggers for introduction of post-authorisation aRMMs in our study. These findings are comparable with results of other studies, in which spontaneous reports and post-marketing clinical trials are the most frequent sources of new safety information post-authorisation. aRMMs were imposed on one medicine in our study (gadoversetamide) following a review of the benefit–risk balance of gadolinium-containing contrast agents, i.e. a referral procedure. Although several referrals were conducted and concluded during the study period, these concerned medicines approved before our study period (such as vitamin A derivatives) or medicines not approved centrally (such as sodium valproate). In addition, some referrals did not lead to imposition of aRMMs, such as both referrals concerning sodium glucose co-transporter 2 inhibitors.
The probability of discontinuation observed in our study is low compared to the discontinuation rates reported in literature for the United States Food and Drug Administration’s (FDA) Risk Evaluation and Mitigation Strategies (REMS). Studies have reported discontinuation rates of REMS between 57 and 75%, with an average time to REMS discontinuation of 1.7 years [15,16,17]. Median time to discontinuation of aRMMs in our study was 7.5 years. However, when comparing discontinuation rates of aRMMs in the EU and REMS in the USA, some key factors should be considered. First and most importantly, medication guides (paper handouts which may help patients avoid serious risks) were considered a REMS until November 2011, when the FDA released new guidance clarifying that medication guides may not always be a REMS [18]. In one study, almost all the discontinued REMS consisted of only a medication guide [15]. The high reported rate of REMS discontinuation may be partly explained by re-evaluation of these medication guide–only REMS. Second, the high discontinuation rates reported for REMS included multiple product-specific REMS programmes for both innovator and non-innovator medicines with the same active substances and REMS programmes for non-innovator medicinal products containing active substances with a long history of use. To avoid multiple counting of aRMMs, we excluded non-innovator medicines from our study, as they are expected to follow the RMP of the reference innovator medicine. The discontinuation rate of REMS as reported in the literature is therefore not directly comparable to the discontinuation rate of aRMMs in our study. Different conclusions regarding safety between different regulators have been shown to lead to differences in frequency, timing, and content of safety communications both within the EU and between the USA, Canada, and the UK [14, 19]. This may also impact the decision to require or discontinue either aRMMs or REMS. Lastly, REMS requirements include mandatory assessment of the effectiveness of the measures after 18 months, 3 years, and 7 years. In contrast, timelines for evaluation of effectiveness of aRMMs are determined on a case-by-case basis, although GVP module XVI rev 2 provides guidance on time points of particular interest, namely 1 year after implementation and 5 years after MA [4].
Evaluation of the effectiveness of risk minimisation programmes became mandatory with amendments to the EU’s pharmaceutical legislation in 2012, with updated guidelines highlighting the importance of evaluation of effectiveness of aRMMs [1]. Studies have found that effectiveness of aRMMs is evaluated through routine pharmacovigilance for more than half of the products with aRMMs [7, 20]. Recent reviews of studies evaluating the effectiveness of product-specific risk minimisation measures have shown heterogeneous methodology and mixed study outcomes [21,22,23]. In one review of effectiveness evaluation studies, the outcome of effectiveness evaluations led to discontinuation of the aRMMs under investigation in 9% of effectiveness evaluation studies. Further action such as updates to the content or improved distribution or follow-up assessment was required following half of the evaluations, and the evaluation did not lead to any changes in the remaining 40% [24]. However, these reviews concerned effectiveness evaluations in a subset of medicines (those intended for chronic treatment) or have been conducted using data available in the EU PAS register [21,22,23,24]. They may not provide an exhaustive overview of all effectiveness studies performed in the EU, since registration in the EU PAS register is only mandatory for studies imposed on the MA or studies that are a specific obligation to the MA—effectiveness evaluation studies rarely fall in these categories [25]. In our study, effectiveness evaluation was the trigger for only one discontinuation (Hirobriz breezhaler). This effectiveness evaluation study was not registered in the EU PAS register.
Notably, GVP module V was updated in 2017 to emphasise that aRMMs may be discontinued when no longer considered necessary; thus, we expect the probability of discontinuation of aRMMs to rise in the coming years [3].
Our study has limitations. First, we did not include DHPCs in our study as they differ substantially from the other aRMM modalities due their non-recurring nature and broader scope of use. Importantly, DHPCs are the only type of aRMM that are not recorded in annex IID of the MA, and information on issued DHPCs is not systematically reflected on the EMA website. Although several national competent authorities publish DHPCs on their websites, studies have shown inconsistencies between national competent authorities with regard to dissemination and content of DHPCs [19].
Second, our study included only centrally authorised products in the EU. However, due to the mandatory scope of the central procedure, the majority of new active substances approved during the study period is expected to be included in our study [1]. In addition, the vast majority (80–98%) of medicines approved through national, mutual recognition and decentralised procedures concern non-innovator applications such as generics: in 2018, 80–98% of the applications submitted to the Coordination Group for Mutual Recognition and Decentralised Procedures over the year 2018 concerned non-innovator applications. We excluded non-innovator products as their EU-RMP should be in line with the EU-RMP of the reference product.
Third, our study was conducted with publicly available data. The structure and quality of the EPARs, in particular the “EPAR—Public Assessment Report”, evolved over time to include more information in a standardised manner. Particularly for the first part of the study period, identifying aRMMs at the time of MA could be challenging, leading us to develop the two-step approach we used in this study. Although there is residual potential for misclassification, for instance, if the content of the EPARs is not updated correctly, this probability is considered to be small.
5 Conclusion
We found low probabilities of introduction and discontinuation of aRMMs (excluding DHPCs) during the product life cycle for medicines authorised between 2006 and 2017. The low probability of discontinuation may be due to lack of robust data on effectiveness of aRMMs. Further research is needed to get more insight into the dynamics of aRMMs during the medicine life cycle.
References
Regulation (EC) No 726/2004 of the European Parliament and of the Council of March 2004 laying down Community procedures for the authorisation and supervision of medicinal products for human and veterinary use and establishing a European Medicines Agency.
Directive 2001/83/EC of the European Parliament and of the Council of 6 November 2001 on the Community code relating to medicinal products for human use.
Guideline on good pharmacovigilance practices (GVP): module V—risk management systems (Rev 2). 2017.
Guideline on good pharmacovigilance practices (GVP): module XVI—risk minimisation measures: selection of tools and effectiveness indicators (Rev 2). 2017.
Francisca RDC, Zomerdijk IM, Sturkenboom MCJM, Straus SMJM. Measuring the impact of the 2012 European pharmacovigilance legislation on additional risk minimization measures. Expert Opin Drug Saf. 2018;17(10):975–82.
Keddie S. A descriptive study of additional risk minimization measures included in risk management plans reviewed by the United Kingdom regulatory authority. Pharm Med. 2013;27(1):25–34.
Rubino A, Artime E. A descriptive review of additional risk minimisation measures applied to EU centrally authorised medicines 2006–2015. Expert Opin Drug Saf. 2017;16(8):877–84.
Zomerdijk IM, Sayed-Tabatabaei FA, Trifiro G, Blackburn SC, Sturkenboom MC, Straus SM. Risk minimization activities of centrally authorized products in the EU: a descriptive study. Drug Saf. 2012;35(4):299–314.
Commission Regulation (EC) No 507/2006 of 29 March 2006 on the conditional marketing authorisation for medicinal products for human use falling within the scope of Regulation (EC) No 726/2004 of the European Parliament and of the Council.
Rebordosa C, Houben E, Laugesen K, Bothner U, Montonen J, Aguado J, et al. No evidence of off-label use of olodaterol and indacaterol in Denmark, France, and the Netherlands: a drug utilization study. Sci Rep. 2020;10(1):586.
Potts J, Genov G, Segec A, Raine J, Straus S, Arlett P. Improving the safety of medicines in the EU: from signals to action. Clin Pharmacol Ther. 2019;107:521–9.
Mol PGM, Arnardottir AH, Motola D, Vrijlandt PJ, Duijnhoven RG, Haaijer-Ruskamp FM, et al. Post-approval safety issues with innovative drugs: a European cohort study. Drug Saf. 2013;36(11):1105–15.
Mol PGM, Straus SMJM, Piening S, de Vries JTN, de Graeff PA, Haaijer-Ruskamp FMJDS. A decade of safety-related regulatory action in the Netherlands. Drug Saf. 2010;33(6):463–74.
Bjerre LM, Parlow S, De Launay D, Hogel M, Black CD, Mattison DR, et al. Comparative, cross-sectional study of the format, content and timing of medication safety letters issued in Canada, the USA and the UK. BMJ Open. 2018;8(10):e020150.
Slomiany M, Bitar R, Kruse S, Jeffers S, Berkowitz K, Hassan M. Drug safety and the cost of monitoring: the role of REMS in risk management. Ther Innov Regul Sci. 2015;49(4):514–23.
Johnson NA, Priefer R. Assessment of the approved risk evaluation and mitigation strategy programs for new drug applications and biologics licensing applications. Regul Toxicol Pharmacol. 2019;101:53–6.
Rodriguez-Monguio R, Spielberger K, Seoane-Vazquez E. Examination of risk evaluation and mitigation strategies and drug safety in the US. Res Soc Adm Pharm. 2014;10(1):232–8.
Wu J, Juhaeri J. The US food and drug administration's risk evaluation and mitigation strategy (REMS) Program—current status and future direction. Clin Ther. 2016;38(12):2526–32.
Zeitoun JD, Lefèvre JH, Downing N, Bergeron H, Ross JS. Inconsistencies among European Union pharmaceutical regulator safety communications: a cross-country comparison. PLoS ONE. 2014;9(10):e109100.
Gridchyna I, Cloutier AM, Nkeng L, Craig C, Frise S, Moride Y. Methodological gaps in the assessment of risk minimization interventions: a systematic review. Pharmacoepidemiol Drug Saf. 2014;23(6):572–9.
Mazzaglia G, Straus SMJ, Arlett P, da Silva D, Janssen H, Raine J, et al. Study design and evaluation of risk minimization measures: a review of studies submitted to the European Medicines Agency for cardiovascular, endocrinology, and metabolic drugs. Drug Saf. 2017;41:1–12.
Vora P, Artime E, Soriano-Gabarró M, Qizilbash N, Singh V, Asiimwe A. A review of studies evaluating the effectiveness of risk minimisation measures in Europe using the European Union electronic Register of Post-Authorization Studies. Pharmacoepidemiol Drug Saf. 2018;27(7):695–706.
Farcas A, Huruba M, Mogosan C. Study design, process and outcome indicators of post-authorization studies aimed at evaluating the effectiveness of risk minimization measures in the EU PAS Register. Br J Clin Pharmacol. 2019;85(3):476–91.
Artime E, Qizilbash N, Garrido-Estepa M, Vora P, Soriano-Gabarró M, Asiimwe A, et al. Are risk minimization measures for approved drugs in Europe effective? A systematic review. Expert Opin Drug Saf. 2019;18(5):443–54.
Guideline on good pharmacovigilance practices (GVP): module VIII—post-authorisation safety studies (rev 3). 2017.
Acknowledgements
The authors would like to thank Dr. Fakhredin Sayed Tabatabaei and Dr. Liana Gross-Martirosyan for their input.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this study.
Conflict of interest
The authors report no conflicts of interests in relation to this study. MS has led research projects (through organisations) for PASS studies from Servier, GSK, and Novartis, none related to this study.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
R statistical software and the packages utilised in this study are freely available from cran.r-project.org. Custom code is available from the corresponding author on reasonable request.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by RF, EB, and CH. The first draft of the manuscript was written by RF, and all authors commented on this and/or later versions of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Francisca, R.D.C., Baba, E., Hoeve, C.E. et al. Introduction or Discontinuation of Additional Risk Minimisation Measures During the Life Cycle of Medicines in Europe. Drug Saf 44, 63–72 (2021). https://doi.org/10.1007/s40264-020-00993-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-020-00993-6