Abstract
Introduction
The rapidly expanding size of the Food and Drug Administration’s (FDA) Adverse Event Reporting System database requires modernized pharmacovigilance practices. Techniques to systematically identify high utility individual case safety reports (ICSRs) will support safety signal management.
Objectives
The aim of this study was to develop and validate a model predictive of an ICSR’s pharmacovigilance utility (PVU).
Methods
PVU was operationalized as an ICSR’s inclusion in an FDA-authored pharmacovigilance review’s case series supporting a recommendation to modify product labeling. Multivariable logistic regression models were used to examine the association between PVU and ICSR features. The best performing model was selected for bootstrapping validation. As a sensitivity analysis, we evaluated the model’s performance across subgroups of safety issues.
Results
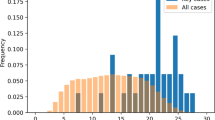
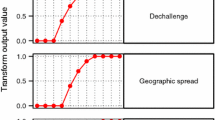
We identified 10,381 ICSRs evaluated in 69 pharmacovigilance reviews, of which 2115 ICSRs were included in a case series. The strongest predictors of ICSR inclusion were reporting of a designated medical event (odds ratio (OR) 1.93, 95% CI 1.54–2.43) and positive dechallenge (OR 1.67, 95% CI 1.50–1.87). The strongest predictors of ICSR exclusion were death reported as the only outcome (OR 2.72, 95% CI 1.76–4.35), more than three suspect products (OR 2.69, 95% CI 2.23–3.24), and > 15 preferred terms reported (OR 2.69, 95% CI 1.90–3.82). The validated model showed modest discriminative ability (C-statistic of 0.71). Our sensitivity analysis demonstrated heterogeneity in model performance by safety issue (C-statistic range 0.58–0.74).
Conclusions
Our model demonstrated the feasibility of developing a tool predictive of ICSR utility. The model’s modest discriminative ability highlights opportunities for further enhancement and suggests algorithms tailored to safety issues may be beneficial.


Similar content being viewed by others
Notes
Serious outcomes are defined by US regulations (CFRs 314.80, 600.80) and include death, life-threatening, hospitalization, disability, congenital anomaly, and other serious outcomes.
Expedited and non-expedited ICSRs are reports that pharmaceutical manufacturers are required to submit by regulation (CFRs 314.80, 600.80).
References
Lester J, Neyarapally GA, Lipowski E, Graham CF, Hall M, Dal Pan G. Evaluation of FDA safety-related drug label changes in 2010. Pharmacoepidemiol Drug Saf. 2013;22(3):302–5.
Ishiguro C, Hall M, Neyarapally GA, Dal Pan G. Post-market drug safety evidence sources: an analysis of FDA drug safety communications. Pharmacoepidemiol Drug Saf. 2012;21(10):1134–6.
FDA Adverse Event Reporting System (FAERS) Public Dashboard. https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Surveillance/AdverseDrugEffects/ucm070093.htm. Accessed 6 Dec 2019.
Duggirala, HJ, Tonning JM, Smith E, Bright RA, Baker JD, Ball R, et al. Data mining at FDA. http://www.fda.gov/downloads/ScienceResearch/DataMiningatFDA/UCM443675.pdf. Accessed 28 Nov 2019.
Bergvall T, Noren GN, Lindquist M. vigiGrade: a tool to identify well-documented individual case reports and highlight systematic data quality issues. Drug Saf. 2014;37(1):65–77.
Guidance for Industry. Good Pharmacovigilance Practices and Pharmacoepidemiologic Assessment, US Food and Drug Administration; 2005. http://www.fda.gov/downloads/regulatoryinformation/guidances/ucm126834.pdf. Accessed 28 Nov 2019.
FDA Drug Safety Guidances. https://www.fda.gov/drugs/guidance-compliance-regulatory-information/guidances-drugs. Accessed 28 Nov 2019.
Moore TJ, Furberg CD, Mattison DR, Cohen MR. Completeness of serious adverse drug event reports received by the US Food and Drug Administration in 2014. Pharmacoepidemiol Drug Saf. 2016;25(6):713–8.
Oosterhuis I, Rolfes L, Ekhart C, Muller-Hansma A, Harmark L. First experiences with a tool to measure the level of clinical information present in adverse drug reaction reports. Expert Opin Drug Saf. 2018;17(2):111–5.
Han L, Ball R, Pamer CA, Altman RB, Proestel S. Development of an automated assessment tool for MedWatch reports in the FDA adverse event reporting system. J Am Med Inform Assoc. 2017;24(5):913–20.
CIOMS Working Group VIII. Practical aspects of signal detection in pharmacovigilance. Geneva: Report of CIOMS Working Group VIII; 2010.
Pinnow E, Amr S, Bentzen SM, Brajovic S, Hungerford L, St George DM, et al. Postmarket safety outcomes for new molecular entity (NME) drugs approved by the food and drug administration between 2002 and 2014. Clin Pharmacol Ther. 2018;104(2):390–400.
Efron B. Estimating the error rate of a prediction rule: improvement on cross-validation. J Am Stat Assoc. 1983;78:316–31.
Steyerberg EW, Harrell FE Jr, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol. 2001;54(8):774–81.
Postmarketing reporting of adverse drug experiences. 21 CFR 314.80.
Gummin DD, Mowry JB, Spyker DA, Brooks DE, Fraser MO, Banner W. 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clin Toxicol (Phila). 2017;55(10):1072–252.
Wunnava S, Qin X, Kakar T, Socrates V, Wallace A, Rundensteiner E. Towards transforming FDA adverse event narratives into actionable structured data for improved pharmacovigilance. In: 2017 Proceedings of the symposium on applied computing, pp 777–782. https://doi.org/10.1145/3019612.3022875.
Schotland P, Racz R, Jackson D, Levin R, Strauss DG, Burkhart K. Target-adverse event profiles to augment pharmacovigilance: a pilot study with six new molecular entities. CPT Pharmacomet Syst Pharmacol. 2018;7(12):809–17.
Caster O, Juhlin K, Watson S, Noren GN. Improved statistical signal detection in pharmacovigilance by combining multiple strength-of-evidence aspects in vigiRank. Drug Saf. 2014;37(8):617–28.
Scholl JHG, van Hunsel F, Hak E, van Puijenbroek EP. A prediction model-based algorithm for computer-assisted database screening of adverse drug reactions in the Netherlands. Pharmacoepidemiol Drug Saf. 2018;27(2):199–205.
Caster O, Sandberg L, Bergvall T, Watson S, Noren GN. vigiRank for statistical signal detection in pharmacovigilance: first results from prospective real-world use. Pharmacoepidemiol Drug Saf. 2017;26(8):1006–10.
Dal Pan GJ. Ongoing challenges in pharmacovigilance. Drug Saf. 2014;37(1):1–8.
PRAC Strategy on Measuring the Impact of Pharmacovigilance Activities. European Medicines Agency. November 30, 2017. http://www.ema.europa.eu/docs/en_GB/document_library/Other/2016/01/WC500199756.pdf. Accessed 18 Apr 2018.
Meyboom RH, Hekster YA, Egberts AC, Gribnau FW, Edwards IR. Causal or casual? The role of causality assessment in pharmacovigilance. Drug Saf. 1997;17(6):374–89.
Agbabiaka TB, Savovic J, Ernst E. Methods for causality assessment of adverse drug reactions: a systematic review. Drug Saf. 2008;31(1):21–37.
Noren GN. The power of the case narrative—can it be brought to bear on duplicate detection? Drug Saf. 2017;40(7):543–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was used for the preparation of this manuscript.
Conflict of interest
Monica A. Muñoz, Gerald J. Dal Pan, Jenny Wei, Chris Delcher, Hong Xiao, Cindy M. Kortepeter, and Almut G. Winterstein declare that they have no conflict of interest.
Ethical approval
This study was approved by both the US FDA and University of Florida’s Institutional Review and Boards.
Additional information
The views expressed are those of the authors and do not necessarily represent the position of, nor imply endorsement from, the US Food and Drug Administration or the US Government.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Muñoz, M.A., Dal Pan, G.J., Wei, YJ.J. et al. Towards Automating Adverse Event Review: A Prediction Model for Case Report Utility. Drug Saf 43, 329–338 (2020). https://doi.org/10.1007/s40264-019-00897-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-019-00897-0