Abstract
Introduction
Investigations have highlighted the lack of evidence regarding the likelihood of congenital malformations following exposure to antipsychotic drugs during pregnancy. To gain further knowledge regarding their safety, we evaluated signals of congenital malformations with antipsychotics using VigiBase®, the World Health Organization (WHO) Global Individual Case Safety Report (ICSR) database.
Method
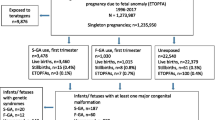
A case/non-case study was conducted in VigiBase® between 1967 and 2014. Signals of disproportionate reporting (SDRs) were detected using the proportional reporting ratio (PRR), which defines SDRs as drug-report associations with a PRR ≥2, Chi square ≥4, and number of cases ≥3. SDR detection for antipsychotics was performed for congenital malformations after removing all reports related to drug competitors and reports of movement disorders from the database.
Results
After removing reports related to drug competitors (antiepileptics, antidepressants, antivirals) and movement disorders, three signals were revealed: ‘palate disorders congenital’ (PRR 2.1, 95 % CI 1.6–2.9, Chi square = 30; n = 41), ‘oesophageal disorders congenital’ (PRR 2.5, 95 % CI 1.3–4.7, Chi square = 11; n = 10) and ‘anorectal disorders congenital’ (PRR 3.0, 95 % CI 1.6–5.6, Chi square = 13; n = 11). Among antipsychotics, phenothiazines with a piperazine side-chain, risperidone and aripiprazole appeared to be more suspect.
Conclusion
Confirming a first signal from spontaneous reporting data, three SDRs for antipsychotics and gastrointestinal congenital abnormalities were unmasked in VigiBase®. This signal should be further explored by ad hoc pharmacoepidemiologic studies in order to assess whether it is relevant for prescription and public health.

Similar content being viewed by others
References
Abel K. Review: teratogenicity of first- and second-generation antipsychotics in pregnancy is unclear. Evid Based Ment Health. 2011;14:31.
Einarson A, Einarson TR. Maternal use of antipsychotics in early pregnancy: little evidence of increased risk of congenital malformations. Evid Based Ment Health. 2009;12:29.
Gentile S. Antipsychotic therapy during early and late pregnancy. A systematic review. Schizophr Bull. 2010;36:518–44.
Oyebode F, Rastogi A, Berrisford G, Coccia F. Psychotropics in pregnancy: safety and other considerations. Pharmacol Ther. 2012;135:71–7.
Cohen LS, Viguera AC, McInerney KA, Freeman MP, Sosinsky AZ, Moustafa D, et al. Reproductive safety of second-generation antipsychotics: current data from the Massachusetts General Hospital National Pregnancy Registry for Atypical Antipsychotics. Am J Psychiatry. 2015. doi:10.1176/appi.ajp.2015.15040506.
Webb RT, Howard L, Abel KM. Antipsychotic drugs for non-affective psychosis during pregnancy and postpartum. Cochrane Database Syst Rev. 2004;2:CD004411.
Galbally M, Snellen M, Power J. Antipsychotic drugs in pregnancy: a review of their maternal and fetal effects. Ther Adv Drug Saf. 2014;5:100–9.
Newport DJ, Calamaras MR, DeVane CL, Donovan J, Beach AJ, Winn S, et al. Atypical antipsychotic administration during late pregnancy: placental passage and obstetrical outcomes. Am J Psychiatry. 2007;164:1214–20.
Gilman AG, et al. Goodman and Gilman’s the pharmacological basis of therapeutics. New York: McGraw-Hill; 2011.
Johnson KC, LaPrairie JL, Brennan PA, Stowe ZN, Newport DJ. Prenatal antipsychotic exposure and neuromotor performance during infancy. Arch Gen Psychiatry. 2012;69:787–94.
Alexander GC, Gallagher SA, Mascola A, Moloney RM, Stafford RS. Increasing off-label use of antipsychotic medications in the United States, 1995–2008. Pharmacoepidemiol Drug Saf. 2011;20:177–84.
Epstein RA, Bobo WV, Shelton RC, Arbogast PG, Morrow JA, Wang W, et al. Increasing use of atypical antipsychotics and anticonvulsants during pregnancy. Pharmacoepidemiol Drug Saf. 2013;22:794–801.
Verdoux H, Tournier M, Bégaud B. Antipsychotic prescribing trends: a review of pharmaco-epidemiological studies. Acta Psychiatr Scand. 2010;121:4–10.
Toh S, Li Q, Cheetham TC, Cooper WO, Davis RL, Dublin S, et al. Prevalence and trends in the use of antipsychotic medications during pregnancy in the US, 2001–2007: a population-based study of 585,615 deliveries. Arch Womens Ment Health. 2013;16:149–57.
Meyboom RH, Lindquist M, Flygare AK, Biriell C, Edwards IR. The value of reporting therapeutic ineffectiveness as an adverse drug reaction. Drug Saf. 2000;23:95–9.
Roberto G, Piccinni C, D’Alessandro R, Poluzzi E. Triptans and serious adverse vascular events: data mining of the FDA Adverse Event Reporting System database. Cephalalgia Int J Headache. 2014;34:5–13.
Montastruc J-L, Sommet A, Bagheri H, Lapeyre-Mestre M. Benefits and strengths of the disproportionality analysis for identification of adverse drug reactions in a pharmacovigilance database. Br J Clin Pharmacol. 2011;72:905–8.
Rothman KJ, Lanes S, Sacks ST. The reporting odds ratio and its advantages over the proportional reporting ratio. Pharmacoepidemiol Drug Saf. 2004;13:519–23.
Edwards IR, Biriell C. Harmonisation in pharmacovigilance. Drug Saf. 1994;10:93–102.
Salvo F, Leborgne F, Thiessard F, Moore N, Bégaud B, Pariente A. A potential event-competition bias in safety signal detection: results from a spontaneous reporting research database in France. Drug Saf. 2013;36:565–72.
Wang H, Hochberg AM, Pearson RK, Hauben M. An experimental investigation of masking in the US FDA adverse event reporting system database. Drug Saf. 2010;33:1117–33.
Pariente A, Avillach P, Salvo F, Thiessard F, Miremont-Salamé G, Fourrier-Reglat A, et al. Effect of competition bias in safety signal generation: analysis of a research database of spontaneous reports in France. Drug Saf. 2012;35:855–64.
Lindquist M. VigiBase, the WHO Global ICSR Database System: basic facts. Drug Inf J. 2008;42:409–19.
Uppsala Monitoring Centre. http://www.who-umc.org/DynPage.aspx?id=97218&mn1=7347&mn2=7252. Accessed 12 May 2015.
Bate A, Evans SJW. Quantitative signal detection using spontaneous ADR reporting. Pharmacoepidemiol Drug Saf. 2009;18:427–36.
Arnaud M, Salvo F, Ahmed I, Robinson P, Moore N, Bégaud B, et al. A method for the minimization of competition bias in signal detection from spontaneous reporting databases. Drug Saf. 2016;39:251–60.
Pearson RK, Hauben M, Goldsmith DI, Gould AL, Madigan D, O’Hara DJ, et al. Influence of the MedDRA hierarchy on pharmacovigilance data mining results. Int J Med Inf. 2009;78:e97–103.
Druga A, Nyitray M, Szaszovszky E. Experimental teratogenicity of structurally similar compounds with or without piperazine-ring: a preliminary report. Pol J Pharmacol Pharm. 1980;32:199–204.
Bertelli A, Polani PE, Spector R, Seller MJ, Tuchmann-Duplessis H, Mercier-Parot L. Effect of a neuroleptic, haloperidol, on the gestation and prenatal development of rodents. Results of 3 groups of experiments [in French]. Arzneimittelforschung. 1968;18:1420–4.
Rodríguez GMD, Friman PM. Teratogenic effect of trifluoperazine in rats and mice. Acta Biol Hung. 1985;36:233–7.
Walker BE, Patterson A. Induction of cleft palate in mice by tranquilizers and barbiturates. Teratology. 1974;10:159–63.
Ho CK, Kaufman RL, McAlister WH. Congenital malformations. Cleft palate, congenital heart disease, absent tibiae, and polydactyly. Am J Dis Child. 1960;1975(129):714–6.
Peitl MV, Petrić D, Peitl V. Ziprasidone as a possible cause of cleft palate in a newborn. Psychiatr Danub. 2010;22:117–9.
Puhó EH, Szunyogh M, Métneki J, Czeizel AE. Drug treatment during pregnancy and isolated orofacial clefts in hungary. Cleft Palate-Craniofacial J. 2007;44:194–202.
Reis M, Källén B. Maternal use of antipsychotics in early pregnancy and delivery outcome. J Clin Psychopharmacol. 2008;28:279–88.
Sadowski A, Todorow M, Yazdani Brojeni P, Koren G, Nulman I. Pregnancy outcomes following maternal exposure to second-generation antipsychotics given with other psychotropic drugs: a cohort study. BMJ Open. 2013;3:e003062. doi:10.1136/bmjopen-2013-003062.
Rumeau-Rouquette C, Goujard J, Huel G. Possible teratogenic effect of phenothiazines in human beings. Teratology. 1977;15:57–64.
Habermann F, Fritzsche J, Fuhlbrück F, Wacker E, Allignol A, Weber-Schoendorfer C, et al. Atypical antipsychotic drugs and pregnancy outcome: a prospective, cohort study. J Clin Psychopharmacol. 2013;33:453–62.
Slone D, Siskind V, Heinonen OP, Monson RR, Kaufman DW, Shapiro S. Antenatal exposure to the phenothiazines in relation to congenital malformations, perinatal mortality rate, birth weight, and intelligence quotient score. Am J Obstet Gynecol. 1977;128:486–8.
McKenna K, Koren G, Tetelbaum M, Wilton L, Shakir S, Diav-Citrin O, et al. Pregnancy outcome of women using atypical antipsychotic drugs: a prospective comparative study. J Clin Psychiatry. 2005;66:444–9 (quiz 546).
Coughlin CG, Blackwell KA, Bartley C, Hay M, Yonkers KA, Bloch MH. Obstetric and neonatal outcomes after antipsychotic medication exposure in pregnancy. Obstet Gynecol. 2015;125:1224–35.
Montastruc J-L, Sommet A, Lacroix I, Olivier P, Durrieu G, Damase-Michel C, et al. Pharmacovigilance for evaluating adverse drug reactions: value, organization, and methods. Joint Bone Spine. 2006;73:629–32.
Weber J. Epidemiology of adverse reactions to nonsteroidal antiinflammatory drugs. In: Rainsford KD, editor. Advances in inflammation. New York: Raven Press; 1984. p. 1–7.
Hartnell NR, Wilson JP. Replication of the Weber effect using postmarketing adverse event reports voluntarily submitted to the United States Food and Drug Administration. Pharmacotherapy. 2004;24:743–9.
Blomberg S. Influence of maternal distress during pregnancy on fetal malformations. Acta Psychiatr Scand. 1980;62:315–30.
Gladston S, Clarke DJ. Clozapine treatment of psychosis associated with velo-cardio-facial syndrome: benefits and risks. J Intellect Disabil Res. 2005;49:567–70.
Damase-Michel C, Lacroix I, Hurault-Delarue C, Beau A-B, Montastruc J-L, les partenaires d’EFEMERIS. Drug in pregnancy: studies in the French database EFEMERIS [in French]. Thérapie. 2014;69:91–100.
Patadia VK, Schuemie MJ, Coloma P, Herings R, van der Lei J, Straus S, et al. Evaluating performance of electronic healthcare records and spontaneous reporting data in drug safety signal detection. Int J Clin Pharm. 2015;37:94–104.
Mitchell AA. Systematic identification of drugs that cause birth defects: a new opportunity. N Engl J Med. 2003;349:2556–9.
Acknowledgments
The authors would like to thank the UMC, which provided and gave permission to use the data analysed in the present study.
The authors are indebted to the National Pharmacovigilance Centres that contributed data. The opinions and conclusions in this study are not necessarily those of the various centres or the WHO.
The authors gratefully acknowledge Mrs Christine Damase-Michel and Mrs Isabelle Lacroix for their advice and corrections. The authors also thank Mr Ray Cooke for revising the English.
Authors’ contributions
François Montastruc, Bernard Bégaud and Antoine Pariente participated in the study design and planning; François Montastruc, Francesco Salvo, Mickaël Arnaud, Bernard Bégaud and Antoine Pariente took part in the acquisition, analysis and interpretation of the data; François Montastruc, Bernard Bégaud and Antoine Pariente drafted the manuscript; and Francesco Salvo, Mickaël Arnaud, Bernard Bégaud and Antoine Pariente critically revised the manuscript for important intellectual content. All authors approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No specific funding was received for this study.
Conflicts of interest
François Montastruc, Francesco Salvo, Mickaël Arnaud, Bernard Bégaud and Antoine Pariente have no conflicts of interest that are directly relevant to the content of this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Montastruc, F., Salvo, F., Arnaud, M. et al. Signal of Gastrointestinal Congenital Malformations with Antipsychotics After Minimising Competition Bias: A Disproportionality Analysis Using Data from Vigibase® . Drug Saf 39, 689–696 (2016). https://doi.org/10.1007/s40264-016-0413-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-016-0413-1