Abstract
Background
Drug-induced torsades de pointes (TdP) and related clinical entities represent a current regulatory and clinical burden.
Objective
As part of the FP7 ARITMO (Arrhythmogenic Potential of Drugs) project, we explored the publicly available US FDA Adverse Event Reporting System (FAERS) database to detect signals of torsadogenicity for antipsychotics (APs).
Methods
Four groups of events in decreasing order of drug-attributable risk were identified: (1) TdP, (2) QT-interval abnormalities, (3) ventricular fibrillation/tachycardia, and (4) sudden cardiac death. The reporting odds ratio (ROR) with 95 % confidence interval (CI) was calculated through a cumulative analysis from group 1 to 4. For groups 1+2, ROR was adjusted for age, gender, and concomitant drugs (e.g., antiarrhythmics) and stratified for AZCERT drugs, lists I and II (http://www.azcert.org, as of June 2011). A potential signal of torsadogenicity was defined if a drug met all the following criteria: (a) four or more cases in group 1+2; (b) significant ROR in group 1+2 that persists through the cumulative approach; (c) significant adjusted ROR for group 1+2 in the stratum without AZCERT drugs; (d) not included in AZCERT lists (as of June 2011).
Results
Over the 7-year period, 37 APs were reported in 4,794 cases of arrhythmia: 140 (group 1), 883 (group 2), 1,651 (group 3), and 2,120 (group 4). Based on our criteria, the following potential signals of torsadogenicity were found: amisulpride (25 cases; adjusted ROR in the stratum without AZCERT drugs = 43.94, 95 % CI 22.82–84.60), cyamemazine (11; 15.48, 6.87–34.91), and olanzapine (189; 7.74, 6.45–9.30).
Conclusions
This pharmacovigilance analysis on the FAERS found 3 potential signals of torsadogenicity for drugs previously unknown for this risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Drug-induced cardiac ventricular arrhythmias represent a major safety concern, both on regulatory and clinical grounds [1, 2]. Torsades de pointes (TdP) is a specific form of ventricular arrhythmia very frequently attributable to drug administration. Together with its surrogate QT prolongation, TdP has caused a variety of drug withdrawals and/or restrictions of use (e.g., haloperidol, sertindole, and astemizole) in past decades, especially for noncardiovascular drugs [3]. In addition, a long list of warnings of TdP risk from regulatory agencies has begun to accrue, resulting in a reduction of therapeutic alternatives in the prescribers’ toolkit. From the clinical standpoint, TdP frequently terminates spontaneously, causing syncope, but can sometimes degenerate into ventricular fibrillation with cardiac arrest and sudden cardiac death (SCD) if not resuscitated [4]. The point at which the physician observes an evolving arrhythmic event (such as TdP) therefore influences how the event will be described and reported. Hence, composite clinical endpoints are needed to fully explore the range of drug-associated TdPs [5]. Moreover, a number of risk factors for TdP occurrence have been identified (e.g., congenital long QT syndrome, heart failure, electrolyte balance impairment, multiple drug therapies) and physicians are requested to prioritize patient safety by selecting the safest therapy among the available options [6].
Although a number of strategies (both clinical and preclinical) have been proposed, the assignment of the proarrhythmic risk of drugs is still far from established, because of the lack of predictive value of each approach [7]. The attempt to provide a torsadogenic score to each drug by knowledge integration of heterogeneous evidence represents the ultimate goal of the ARITMO (Arrhythmogenic Potential of Drugs) project [8]. As part of this consortium, spontaneous reporting systems emerged as a cornerstone for timely detection of signals (previously unknown drug–event associations or increasing the frequency of known adverse drug reactions [ADRs]), which deserve validation and risk quantification through different sources such as healthcare databases. The importance of pharmacovigilance analyses has been clearly underlined by several studies that showed that case report/case series represented the most important source of evidence for drug withdrawals in Europe and the US [9].
Although several postmarketing studies have been conducted to assess the risk of QT prolongation, TdP, ventricular fibrillation, and SCD with non-anti-arrhythmic drugs [10–16], to the best of our knowledge, no pharmacovigilance analyses have systematically addressed the torsadogenic potential of antipsychotics (APs). The interest for this therapeutic class has strongly increased in the past two decades for several reasons: on the one hand, the epidemiological burden of the psychoses and the related innovation in diagnostic procedures for early recognition; on the other hand, the availability of new drugs with possibly better benefit–risk profiles compared with the older, first-generation compounds and the consequent increase in drug consumption throughout all age groups, ethnic groups, and approved indications [17–20]. The rapid changes in the uptake of these drugs require adequate monitoring of actual adverse effects in the population, while spontaneous reporting represents a ready-to-use source of data to be analyzed for an early and timely identification of risks.
In this study, we explored the US FDA Adverse Event Reporting System (FAERS) to detect signals of increased torsadogenic risk for APs. By virtue of its large population coverage (including all US reports and serious/unexpected ADRs from non-US countries) and free availability (providing public access from 2004), the FAERS is an attractive source to explore rare ADRs such as TdP [21, 22].
2 Methods
2.1 Data Source and Processing
Data were obtained from the publicly accessible FAERS database (first quarter of 2004 through fourth quarter of 2010), which is a computerized information system where healthcare professionals and consumers send adverse event reports voluntarily through the MedWatch program [23]. The system includes all serious and unlabelled spontaneous reports from the USA and non-US countries (submission required by manufacturers), and nonserious reports only from the USA [24].
Data submitted to the FAERS database are structured in different files, generating specific tables that are linked to each other by an ‘ISR number’. Each ISR number identifies a case–drug pair and may indicate an initial or a follow-up status of the report. More case–drug pairs can be included in a unique FAERS case, identified by a ‘case number’. The following files/tables were analyzed:
A. DEMO: demographic characteristics (patient ‘age’, ‘gender’, ‘reporter country’, and ‘event date’);
B. DRUG: reported medications with their assigned role code (‘primary suspect drug’, PS; ‘secondary suspect drug’, SS; ‘interacting’, I; ‘concomitant’, C). The analysis was restricted to reports where APs were recorded as suspect or interacting. Information on concomitant drugs was used to identify potential confounders/effect modifiers to adjust or stratify disproportionality analysis (see below).
C. REACTION: ADRs coded by the standardized Medical Dictionary for Regulatory Activities (MedDRA®), the international medical terminology developed under the auspices of the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH). The full list of MedDRA® preferred terms (PTs) used for search strategy is shown as supplementary material in Table S2;
D. OUTCOME: death, life-threatening, hospitalization, or other. This information on the seriousness of the disease was used to identify different subgroups within outcomes of interest (see below).
Data mining of the FAERS requires complex data processing to obtain the final dataset; in particular, an ad hoc drug mapping, duplicate detection and removal as well as management of missing data. These technical issues are described in detail elsewhere [25]. In summary, this mapping approach allowed allocation of a substance name to about 90 % of all records in the entire database. The fraction of missing data varied widely among data files (e.g., 8 % for gender, 34 % for age). In this study, we first imputed missing values in the DEMO file based on the degree of similarity between two records; we then excluded reports with missing information on age and gender, and, finally, performed a de-duplication approach based on the following key field: age, gender, event date, and reporter’s country. This multistep process not only ensures a minimum level of quality of spontaneous reports, but also is warranted to allow adjustment for demographic factors in disproportionality (see below).
2.2 Case Definition and Coding
Because of the heterogeneous nature of drug-induced TdP, composite clinical endpoints are needed to capture as many cases as possible associated with drug exposure [5]. Therefore, a multidisciplinary panel within the ARITMO consortium (i.e., cardiologists, pharmacoepidemiologists, and pharmacovigilance experts) reached consensus on defining four groups of events in decreasing order of drug-attributable risk for TdP. The groups were: (1) TdP; (2) QT interval abnormalities; (3) ventricular fibrillation/tachycardia; and (4) SCD. Within each group, different subgroups were identified based on the seriousness of the outcomes; that is, whether the event caused death or life-threatening events. These groups allow both evaluation of single events per se and combined analyses of groups of events through a cumulative approach (i.e., a single case report of interest can be classified only in one group based on the following order: 1 > 2 > 3 > 4). Details on outcome definition are provided in the supplementary material (Table SI). This case definition was created by building on the already existing standardized MedDRA® query (SMQ), namely TdT-QT prolongation, which is based on a ‘narrow’ strategy (including a core of medical concepts specific for TdP/QT prolongation) and a ‘broad’ search scope (including nonspecific terms such as SCD). As a matter of fact, all PTs of the SMQ were considered, with the addition of new potentially useful terms (e.g., QT-interval shortening [26, 27]). Moreover, the seriousness of the event was analyzed to distinguish different subgroups and remove nonspecific clinical entities such as non-life-threatening syncope with a neurological cause. For a complete list of MedDRA® codes (version 13.0), see supplementary Table SII.
2.3 Data Analysis
First, a case listing was generated with the AP and the number of cases by type of event. Second, we applied the case/noncase disproportionality analysis to the four groups of events; cases were represented by reports of arrhythmias according to PTs of MedDRA® coding, whereas noncases were defined as all other reports (i.e., those without such PTs). Disproportionality analysis was performed by calculating the reporting odds ratio (ROR), with the corresponding 95 % confidence interval (CI). Disproportionality was formally defined when the lower limit of the 95 % CI was >1, with >3 cases [28]. The ROR was first calculated by progressively aggregating the events from 1 to 4 (i.e., cumulative analysis). Second, the disproportionality approach was refined in light of the clinical setting in which TdP usually occurs.
When more than one outcome of interest was listed in a single report (e.g., TdP and QT prolongation), the case was considered once by assigning the priority to the most specific outcome for TdP (i.e., TdP > QT abnormalities > ventricular fibrillation/tachycardia > SCD).
Because the role of other risk factors cannot be disregarded in the genesis of TdP (the multihit hypothesis implying the so-called reduced repolarization reserve [29]), the following approach was carried out. The main known factors influencing association between drug and TdP were taken into account to perform separate univariate regressions: age, gender, use of Class I/III antiarrhythmic drugs as a proxy of already diagnosed arrhythmia (ATC code: C01B), use of drugs with cardiovascular indications (i.e., digitalis, C01A; diuretics, C03; beta blockers, C07; calcium channel blockers, C08; ACE inhibitors/ARBs, C09) as a proxy of heart disease, and use of drugs known for their torsadogenic potential (reference source: lists I and II of the Arizona CERT [30], downloaded in the version available as of June 2011).
The concomitant presence of AZCERT drugs emerged as an effect modifier and was therefore used for stratification, whereas other covariates were regarded as confounding factors and were used to adjust the ROR according to the Mantel–Haenszel method.
A potential signal of torsadogenicity was defined if a drug met all the following criteria:
-
at least 4 cases in group 1+2;
-
significant disproportionality in group 1+2 that persists through the cumulative approach;
-
significant disproportionality in group 1+2 (ROR adjusted for confounders) in the stratum without AZCERT drugs (effect modifier);
-
not included in the AZCERT lists (downloaded in the version available as of June 2011).
As a third step, the ROR was calculated within APs. This means to compare the reporting of a given drug with other agents belonging to the same therapeutic class (e.g., haloperidol versus all other APs). To this end, the analysis was run using a subset of data at the ATC level 3 (N05A). This approach allowed for mitigation of potential bias such as ‘confounding by indication’, which should be considered because patients with psychosis have an increased likelihood of SCD. Restriction of the analysis to the pharmacological class of interest may be considered as a sensitivity analysis and allows for investigation of potential intraclass variations in terms of risk. All the analyses were performed using the statistical package SPSS (version 19.0, IBM SPSS Software, Armonk, NY, USA).
3 Results
3.1 Descriptive Analysis
Over the 7-year period, 2,131,688 spontaneous reports were retrieved after removal of duplicates and multiple records. The outcomes of interest according to case definition (see ‘Methods’ and Table S1) were reported in 62,848 cases (Fig. 1); 5,802 of these reports contained at least one AP drug. Among the considered outcomes, SCD (group 4a) and nonserious ventricular tachycardia (group 3c) were the most frequently reported outcomes, and APs were mentioned in the 8–9 % of these. On the other hand, TdP (group 1) and symptomatic QT abnormalities (group 2a) were less frequently reported outcomes both for the overall FAERS reports (1,770 and 1,075 cases, respectively) and for the AP reports (168 and 241). Notably, APs were reported in 9 % of TdP cases and in 22 % of symptomatic QT abnormalities.
Most of the cases associated with APs occurred in women, especially for group 1 (60 %) and group 2 (56 %). Patients younger than 65 years of age were the most frequently represented: 66, 80, 88, and 83 % of cases (groups 1, 2, 3, and 4, respectively). Physicians submitted 46 % of TdP cases (group 1), 52 % of group 2 cases, and 46 % of the cases in groups 3 and 4, respectively. The USA was the reporter country in 48, 29, 26, and 44 % of the ARITMO cases (groups 1, 2, 3, and 4, respectively).
Table 1 shows the number of cases grouped by outcome for each considered agent. Overall, 37 different APs were reported in cases of cardiac arrhythmia: quetiapine (1,120 cases), clozapine (1,078), and olanzapine (901) were the most frequently reported. By considering only group 1 (TdP), 7 drugs were reported in at least 4 cases with the following ranking: haloperidol (40 cases), ziprasidone (29), quetiapine (25), risperidone (21), olanzapine (8), droperidol (6), and amisulpride (4). By extending the selection of cases to QT abnormalities (group 1 + group 2 outcomes), 20 APs reached 4 cases: olanzapine (189 cases), quetiapine (186), and clozapine (178) were the most frequently reported.
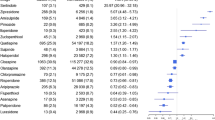
3.2 Disproportionality Analyses
Table 2 provides the results of disproportionality analysis (crude ROR) obtained by combining groups through a progressive cumulative approach (1+2+3+4). Among 37 analyzed APs, 5 drugs showed disproportionality in all steps of the cumulative analysis: amisulpride, droperidol, haloperidol, risperidone, and ziprasidone. At the second step (groups 1+2a), 5 drugs appeared: cyamemazine, levomepromazine, olanzapine, quetiapine, and zuclopentixole; and 7 drugs at the third (groups 1+2): bromperidol, chlorpromazine, chlorprothixene, clozapine, fluphenazine, pimozide, and prothipendyl. Notably, for all APs with significant ROR in group 1 or 2, disproportionality persisted throughout all remaining groups. However, the strength of the ROR, in terms of absolute values, increases from group 1 to 2 and progressively declines when moving from group 2 to 4.
Table 3 shows the results of disproportionality analyses, stratified and adjusted for covariates (see ‘Methods’), performed on 29 APs with cases of TdP/QT abnormalities. Six agents showed disproportion in all different data-mining approaches (both crude, stratified, and adjusted within strata): amisulpride, clozapine, droperidol, haloperidol, risperidone, ziprasidone. For 4 additional APs (chlorpromazine, cyamemazine, olanzapine, and quetiapine), disproportion found by crude ROR persisted only in the stratum without concomitant AZCERT drugs, also after adjustment. Aripiprazole and paliperidone showed significant disproportion only in the stratum without concomitant AZCERT drugs, before and after the adjustment.
Based on previously described criteria (see Table 4), the following potential signals of torsadogenicity were found: amisulpride (25 cases; adjusted ROR in the stratum without AZCERT drugs 43.94, 95 % CI 22.82–84.60), cyamemazine (11; 15.48, 6.87–34.91), and olanzapine (189; 7.74, 6.45–9.30).
When the disproportionality was calculated intraclass (i.e., by considering only reports where at least one AP was recorded, Table 5), a significant disproportion was found through all approaches for only three agents: amisulpride, haloperidol, and ziprasidone. Chlorpromazine, cyamemazine, and olanzapine showed disproportion only in the strata without concomitant AZCERT drugs (before and after adjustment for covariates).
4 Discussion
The FAERS from 2004 up to December 2010 contained case reports of cardiac arrhythmia related to 39 AP agents. Based on our criteria to define potential signals of torsadogenicity, the following APs emerged: amisulpride, cyamemazine, and olanzapine. The case-by-case evaluation of reports (e.g., number of concomitant drugs, information on dechallenge, time to onset, where available) found no elements in causality assessment against this hypothesis. Notably, these agents represent old drugs with different marketing penetration: a high and very widespread use for olanzapine, a lower but considerable consumption in many Countries for amisulpride and a marketing authorization limited to a few countries for cyamemazine (only in France and Portugal). Remarkably, AZCERT lists have been updated after our analysis, and, in fact, only recently have amisulpride and olanzapine been added to AZCERT lists III and II, respectively. Amisulpride is the only AP categorized in this group with ‘conditional risk of TdP’: considering that disproportion persisted in the intraclass analysis, it could also be considered for inclusion in higher risk lists. In our opinion, olanzapine is now included in the appropriate risk category, similar to many other second-generation APs.
Our study should be interpreted with caution, especially in light of inherent limitations affecting spontaneous reporting systems, which cannot be used to provide incidence or to quantify risk due to under-reporting and lack of exposure data, respectively. In the FAERS, data distortion may occur at two levels: individual records (e.g., quality and completeness of the reported information that compromise the causality assessment, duplicates, errors in drug codification, etc.) and the overall sample (e.g., lack of nonserious events for drugs outside the US market, market penetration of drugs). Nonetheless, all technical issues have been considered in this analysis. In addition, several well-known external factors may affect reporting; for example, notoriety bias, the Weber effect, and product age [31–34]. In this respect, with only a few exceptions (aripiprazole, asenapine, and paliperidone), APs have long been in use and therefore the impact of these factors is assumed to be limited.
Notwithstanding the aforementioned limitations, our study found three potential torsadogenic signals that should be taken into account when assessing the risk–benefit profile of APs: the available evidence suggests similar torsadogenic profiles for first- and second-generation agents [35], as well as no significant difference in their effectiveness [36]. Our findings are also in line with a recent pharmacovigilance analysis of the WHO_Vigibase, which revealed no difference in the cardiac safety profile among haloperidol, olanzapine, and quetiapine [37].
Preclinical data on amisulpride, cyamemazine, and olanzapine (mainly in vitro studies on human Ether-à-go-go Related Gene [hERG] blocking potency) showed only minor inhibition of hERG K+ channels compared with haloperidol and thioridazine, and indicate only a low torsadogenic potential in humans [38, 39]. For cyamemazine, similar hERG channel affinities were demonstrated both for the parent compound and the relevant active metabolites [40, 41]. The hERG blocking liability of olanzapine was confirmed to be theoretically low also in the context of pharmacokinetic data such as myocardial distribution [42]. Notably, the occurrence of TdP-related events in amisulpride recipients could be a specific concern of the overdose setting, a clinical scenario carrying increased risk of torsadogenicity [43]. These data together with the lack of dedicated thorough QT studies strengthen the importance of postmarketing surveillance to detect safety issues that may be missed during the premarketing phase because of the imperfect predictivity of in vitro/in vivo studies.
Although no signal was found for more recently marketed APs, aripiprazole and paliperidone deserve appropriate discussion because they are gaining increasing marketing penetration. Aripiprazole, first marketed in 2002 in the USA, is currently recommended for the treatment of schizophrenia, for the treatment of manic or mixed episodes associated with bipolar I disorder, and for preventing the recurrence of mood episodes during longer-term therapy. More recently, aripiprazole has been approved as an adjunctive treatment for major depressive disorder [44]. Moreover, it is considered the safer alternative in patients with risk factors for QT prolongation [45, 46]. A recent meta-analysis also showed a lower impact on QT interval by aripiprazole in comparison with other second-generation APs [47]. By contrast, our analysis found that aripiprazole was reported in 46 cases of TdP/QT abnormalities with significant disproportionality in the two strata without AZCERT drugs, although the intraclass ROR was not significant. This may be easily explained by the fact that the intraclass analysis was performed on a pharmacological class of concern associated with a certain baseline level of proarrhythmic risk, which may bias disproportionality. On the other hand, the relatively high number of cases and the relevant disproportionality may result from channelling of patients at risk (who receive aripiprazole as a safer alternative according to guidelines). Although our data require validation, caution is needed in vulnerable patients: the risk for the patients must be balanced against the benefit achieved in controlling their underlying disease.
Paliperidone is listed in AZCERT list II and its summary of product characteristics describes a mild risk for QT prolongation; in vitro studies showed a high potency of K+-channel blockade, whereas the effect in a dedicated thorough QT study was considered nonsignificant from a regulatory standpoint and noninferior to quetiapine [48–50]. The 11 cases together with disproportionality analysis indicate that uncertainty persists on its torsadogenic risk. It seems appropriate to continue monitoring paliperidone.
No firm conclusion can be drawn from our study regarding asenapine, because of its very recent marketing approval (2009 in the USA).
From a general regulatory viewpoint, the consensus process in case definition resulted in a comprehensive query, which can be utilized by regulators and researchers when investigating the torsadogenic potential of a given drug within a pharmacovigilance database. Although the search strategy carries inherent limitations of spontaneous reports (e.g., the inability to validate cases of SCD through autopsy), the aim of our approach was to increase the sensitivity of signal detection without substantially affecting specificity; that is, to build on the existing rather than replace the current SMQ.
Another important aspect pertains to the cumulative approach in decreasing order of drug-attributable risk for TdP. This approach may be of interest to refine signal detection because disproportion may appear for a single outcome. Notably, all APs with disproportionality in group 1 or 2 maintained significant ROR when groups 3 and 4 were added to the analysis. This indicates a good concordance between more drug-attributable outcomes (TdP and QT abnormalities) and more sensitive ones (ventricular arrhythmia and SCD). In addition, the analysis of groups 3 and 4 may be useful for drugs with uncertain data on TdP; for instance, due to the low number of cases, especially for recent drugs (e.g., asenapine).
Concerning data processing, the analysis restricted to the refined dataset (i.e., reports without missing data, see Supplementary Table SIII) demonstrated that the adopted criteria did not significantly affect results, but ensured a minimum quality standard.
The role of concomitant drugs as effect modifiers/confounders has been carefully addressed and its importance in the drug–event association clearly emerged, as also recently demonstrated by Tatonetti et al. [51] through a data-driven approach.
4.1 Toward a Targeted Pharmacovigilance Approach
Although it is challenging to identify safer molecules within therapeutic classes, several efforts have been made to provide comprehensive lists of drugs with recognized or potential TdP liability [52]. Because of the compelling clinical need, this aspect is starting to be critically considered in pharmacovigilance. For instance, a recent study on Stevens-Johnson syndrome/toxic epidermal necrolysis underlined several drugs with no association, which may be considered as alternative treatment options [53].
Although actual ranking of risk cannot be achieved through spontaneous reports, the extent of consumption and time on the market should also be taken into account when interpreting pharmacovigilance data (targeted pharmacovigilance).
Based on these criteria and our results, three provisional classes of risk could be proposed: APs with a potential torsadogenic risk (i.e., if a significant disproportionality is found for TdP/QT and consistently persists across all analyses, including the intraclass approach); APs with uncertain torsadogenic risk (i.e., no consistency across disproportionality analyses and low use or very recent entry on the market); and APs with a probably lower risk of torsadogenicity (i.e., consistent absence of significant disproportionality across analyses, high use, and long market life). Within the first class, only the following APs can be included: amisulpride, haloperidol, and ziprasidone. No drug used to treat psychosis can be included at the moment in the lower risk class. All other APs should be included in the uncertain class, either because of the inconsistency among disproportionality results or because of the limited marketing penetration.
We believe that, for practical reasons, the AZCERT website represents the most authoritative source of data regarding the risk of drug-induced TdP, especially as rapid screening for physicians. However, this resource appears to adopt a very precautionary attitude in line with the approach of regulators (e.g., moxifloxacin is now reported in List 1 despite being largely used as a comparator in thorough QT studies; citalopram is now included in List 1 after a warning was posted by the European Medicines Agency), thus causing a steady increase in the number of torsadogenic drugs. The website even explicitly mentioned that “The absence of a drug from these lists should not be considered an indication that they are free of risk of QT prolongation or torsades de pointes” [30]. The AZCERT Advisory Board should implement available lists by identifying possible therapeutic alternatives within the main pharmacological classes to be used in patients susceptible to TdP.
5 Conclusion
This pharmacovigilance analysis on the FAERS identified three torsadogenic signals, which were neither mentioned by the 2011 AZCERT classification nor arose from previous literature data: amisulpride, cyamemazine, and olanzapine. Our findings should be considered with caution, because they need to be validated by integrating data from sources of clinical data. In addition, for more recently marketed drugs, which may be channelled to patients at high risk of TdP, careful monitoring should be maintained. As a matter of fact, the imperfect predictivity of in vitro/in vivo assays and thorough QT studies strengthens the role of postmarketing surveillance in early and timely detection of safety signals.
We believe that the proposed strategy to identify signals is of interest for regulators, as a tool to implement routine pharmacovigilance activity in prioritizing safety issues. On the other hand, our findings represent per se a preliminary contribution for clinicians in prescribing or switching between APs, especially in the clinical setting of polypharmacy, where drug–drug interactions may increase the likelihood of TdP occurrence in susceptible patients.
References
Kannankeril P, Roden DM, Darbar D. Drug-induced long QT syndrome. Pharmacol Rev. 2010;62:760–81.
Behr ER, Roden D. Drug-induced arrhythmia: pharmacogenomic prescribing? Eur Heart J. 2013;34:89–95.
De Ponti F, Poluzzi E, Cavalli A, et al. Safety of non-antiarrhythmic drugs that prolong the QT interval or induce torsade de pointes: an overview. Drug Saf. 2002;25:263–86.
Drew BJ, Ackerman MJ, Funk M, et al. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121:1047–60.
Darpo B. Detection and reporting of drug-induced proarrhythmias: room for improvement. Europace. 2007;9 Suppl 4:iv23–36.
Owens RC Jr. QT prolongation with antimicrobial agents: understanding the significance. Drugs. 2004;64:1091–124.
Raschi E, Ceccarini L, De Ponti F, et al. hERG-related drug toxicity and models for predicting hERG liability and QT prolongation. Expert Opin Drug Metab Toxicol. 2009;5:1005–21.
The ARITMO project [online]. http://www.aritmo-project.org (Accessed May 7 2012).
Clarke A, Deeks JJ, Shakir SA. An assessment of the publicly disseminated evidence of safety used in decisions to withdraw medicinal products from the UK and US markets. Drug Saf. 2006;29:175–81.
Ray WA, Meredith S, Thapa PB, et al. Antipsychotics and the risk of sudden cardiac death. Arch Gen Psychiatry. 2001;58:1161–7.
Hennessy S, Bilker WB, Knauss JS, et al. Cardiac arrest and ventricular arrhythmia in patients taking antipsychotic drugs: cohort study using administrative data. BMJ. 2002;325:1070.
Straus SM, Bleumink GS, Dieleman JP, et al. Antipsychotics and the risk of sudden cardiac death. Arch Intern Med. 2004;164:1293–7.
Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294:1934–43.
Jolly K, Gammage MD, Cheng KK, et al. Sudden death in patients receiving drugs tending to prolong the QT interval. Br J Clin Pharmacol. 2009;68:743–51.
Ray WA, Chung CP, Murray KT, et al. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. 2009;360:225–35.
Manu P, Kane JM, Correll CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72:936–41.
Rani F, Murray ML, Byrne PJ, et al. Epidemiologic features of antipsychotic prescribing to children and adolescents in primary care in the United Kingdom. Pediatrics. 2008;121:1002–9.
Verdoux H, Tournier M, Begaud B. Antipsychotic prescribing trends: a review of pharmaco-epidemiological studies. Acta Psychiatr Scand. 2010;121:4–10.
Wittkampf LC, Smeets HM, Knol MJ, et al. Differences in psychotropic drug prescriptions among ethnic groups in the Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2010;45:819–26.
Alexander GC, Gallagher SA, Mascola A, et al. Increasing off-label use of antipsychotic medications in the United States, 1995–2008. Pharmacoepidemiol Drug Saf. 2011;20:177–84.
Poluzzi E, Raschi E, Moretti U, et al. Drug-induced torsades de pointes: data mining of the public version of the FDA Adverse Event Reporting System (AERS). Pharmacoepidemiol Drug Saf. 2009;18:512–8.
Poluzzi E, Raschi E, Motola D, et al. Antimicrobials and the risk of torsades de pointes: the contribution from data mining of the US FDA Adverse Event Reporting System. Drug Saf. 2010;33:303–14.
The FDA Adverse Event Reporting System (FAERS): Latest Quarterly Data Files [online]. http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Surveillance/AdverseDrugEffects/ucm082193.htm (Accessed May 7 2012).
MedWatch: The FDA Safety Information and Adverse Event Reporting Program [online]. http://www.fda.gov/Safety/MedWatch/default.htm (Accessed May 7 2012).
Poluzzi E, Raschi E, Piccinni C, et al. Data mining techniques in pharmacovigilance: analysis of the publicly accessible FDA adverse event reporting system (AERS). In: Karahoca A, editor. Data mining applications in engineering and medicine. Croatia: InTech; 2012. p. 267–301.
Shah RR. Drug-induced QT interval shortening: potential harbinger of proarrhythmia and regulatory perspectives. Br J Pharmacol. 2010;159:58–69.
Raschi E, Poluzzi E, Koci A, et al. QT interval shortening in spontaneous reports submitted to the FDA: the need for consensus. Br J Clin Pharmacol. 2011;72:839–41.
van Puijenbroek EP, Bate A, Leufkens HG, et al. A comparison of measures of disproportionality for signal detection in spontaneous reporting systems for adverse drug reactions. Pharmacoepidemiol Drug Saf. 2002;11:3–10.
Roden DM. Taking the “idio” out of “idiosyncratic”: predicting torsades de pointes. Pacing Clin Electrophysiol. 1998;21:1029–34.
The ArizonaCERT. Center for Education and Research on Therapeutics [online]. http://www.azcert.org/ (Accessed May 7 2012).
Stephenson WP, Hauben M. Data mining for signals in spontaneous reporting databases: proceed with caution. Pharmacoepidemiol Drug Saf. 2007;16:359–65.
Pariente A, Gregoire F, Fourrier-Reglat A, et al. Impact of safety alerts on measures of disproportionality in spontaneous reporting databases: the notoriety bias. Drug Saf. 2007;30:891–8.
Bate A, Evans SJ. Quantitative signal detection using spontaneous ADR reporting. Pharmacoepidemiol Drug Saf. 2009;18:427–36.
Raschi E, Piccinni C, Poluzzi E, et al. The association of pancreatitis with antidiabetic drug use: gaining insight through the FDA pharmacovigilance database. Acta Diabetol (Epub Oct 19 2011).
Nielsen J, Graff C, Kanters JK, et al. Assessing QT interval prolongation and its associated risks with antipsychotics. CNS Drugs. 2011;25:473–90.
Leucht S, Corves C, Arbter D, et al. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet. 2009;373:31–41.
Meyer-Massetti C, Vaerini S, Ratz Bravo AE, et al. Comparative safety of antipsychotics in the WHO pharmacovigilance database: the haloperidol case. Int J Clin Pharm. 2011;33:806–14.
Kongsamut S, Kang J, Chen XL, et al. A comparison of the receptor binding and HERG channel affinities for a series of antipsychotic drugs. Eur J Pharmacol. 2002;450:37–41.
Crumb WJ Jr, Ekins S, Sarazan RD, et al. Effects of antipsychotic drugs on I (to), I (Na), I (sus), I (K1), and hERG: QT prolongation, structure activity relationship, and network analysis. Pharm Res. 2006;23:1133–43.
Crumb W, Llorca PM, Lancon C, et al. Effects of cyamemazine on hERG, INa, ICa, Ito, Isus and IK1 channel currents, and on the QTc interval in guinea pigs. Eur J Pharmacol. 2006;532:270–8.
Crumb W, Benyamina A, Arbus C, et al. Cyamemazine metabolites: effects on human cardiac ion channels in-vitro and on the QTc interval in guinea pigs. J Pharm Pharmacol. 2008;60:1507–13.
Titier K, Canal M, Deridet E, et al. Determination of myocardium to plasma concentration ratios of five antipsychotic drugs: comparison with their ability to induce arrhythmia and sudden death in clinical practice. Toxicol Appl Pharmacol. 2004;199:52–60.
Isbister GK, Balit CR, Macleod D, et al. Amisulpride overdose is frequently associated with QT prolongation and torsades de pointes. J Clin Psychopharmacol. 2010;30:391–5.
Dhillon S. Aripiprazole: a review of its use in the management of mania in adults with bipolar I disorder. Drugs. 2012;72:133–62.
Taylor D, Paton C, Kapur S, editors. The South London and Maudsley NHS Foundation Trust & Oxleas NHS Foundation Trust Prescribing Guidelines. 10th ed. London: Informa Healthcare; 2010.
Belgamwar RB, El-Sayeh HG. Aripiprazole versus placebo for schizophrenia. Cochrane Database Syst Rev. 2011;CD006622.
Chung AK, Chua SE. Effects on prolongation of Bazett’s corrected QT interval of seven second-generation antipsychotics in the treatment of schizophrenia: a meta-analysis. J Psychopharmacol. 2011;25:646–66.
Hough DW, Natarajan J, Vandebosch A, et al. Evaluation of the effect of paliperidone extended release and quetiapine on corrected QT intervals: a randomized, double-blind, placebo-controlled study. Int Clin Psychopharmacol. 2011;26:25–34.
Vigneault P, Kaddar N, Bourgault S, et al. Prolongation of cardiac ventricular repolarization under paliperidone: how and how much? J Cardiovasc Pharmacol. 2011;57:690–5.
Suzuki Y, Fukui N, Watanabe J, et al. QT prolongation of the antipsychotic risperidone is predominantly related to its 9-hydroxy metabolite paliperidone. Hum Psychopharmacol. 2012;27:39–42.
Tatonetti NP, Ye PP, Daneshjou R, et al. Data-driven prediction of drug effects and interactions. Sci Transl Med. 2012;4:125ra31.
De Ponti F, Poluzzi E, Montanaro N. Organising evidence on QT prolongation and occurrence of Torsades de Pointes with non-antiarrhythmic drugs: a call for consensus. Eur J Clin Pharmacol. 2001;57:185–209.
Papay J, Yuen N, Powell G, et al. Spontaneous adverse event reports of Stevens-Johnson syndrome/toxic epidermal necrolysis: detecting associations with medications. Pharmacoepidemiol Drug Saf. 2012;21:289–96.
Acknowledgments
The research leading to these results has received funding from the European Community’s Seventh Framework Programme (FP7/2007-2013) under Grant Agreement No. 241679—the ARITMO project.
MedDRA® trademark is owned by the International Federation of Pharmaceutical Manufacturers & Associations (IFPMA) on behalf of ICH.
Elisabetta Poluzzi and Emanuel Raschi conceived the study; collected, analyzed and interpreted data; drafted and approved the final submitted manuscript.
Ariola Koci collected, analyzed, and interpreted data; revised and approved the final submitted manuscript.
Fabrizio De Ponti conceived the study, made substantive suggestions for data interpretation, revised and approved the final submitted manuscript.
Ugo Moretti, Edoardo Spina, Elijah Behr and Miriam Sturkenboom made substantive suggestions for data interpretation, revised and approved the final submitted manuscript.
Elisabetta Poluzzi, Emanuel Raschi, Ariola Koci, Ugo Moretti, Edoardo Spina, Elijah Behr and Fabrizio De Ponti declare no conflict of interest relevant to the present manuscript.
Miriam Sturkenboom is heading a research unit that holds unconditional research contracts with some pharmaceutical companies (EliLilly, Pfizer, AstraZeneca). None is related to this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Poluzzi, E., Raschi, E., Koci, A. et al. Antipsychotics and Torsadogenic Risk: Signals Emerging from the US FDA Adverse Event Reporting System Database. Drug Saf 36, 467–479 (2013). https://doi.org/10.1007/s40264-013-0032-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-013-0032-z