Abstract
Background and objective
Attention-deficit/hyperactivity disorder is a neurodevelopmental disorder that typically begins in childhood and often persists into adulthood. Recent phase III trials have demonstrated the efficacy and safety of viloxazine extended-release capsules (viloxazine ER; Qelbree®) in pediatrics (6–17 years of age). The aim of this study was to evaluate the efficacy and safety of viloxazine ER in adults with attention-deficit/hyperactivity disorder.
Methods
This was a phase III, randomized, double-blind, placebo-controlled, two-arm trial in adults (18–65 years of age) with attention-deficit/hyperactivity disorder. Eligible subjects were randomized 1:1 to viloxazine ER (flexible dose of 200–600 mg/day) or matched placebo. The primary efficacy endpoint was the change from baseline at end of study (week 6) in the Adult ADHD Investigator Symptom Rating Scale (AISRS) total score. The key secondary endpoint was the change from baseline at end of study in the Clinical Global Impressions-Severity of Illness (CGI-S) score. Additional secondary outcome measures included the AISRS Inattention and Hyperactivity/Impulsivity subscales, the Behavior Rating Inventory of Executive Function-Adult (BRIEF-A), the Generalized Anxiety Disorder-7 Item (GAD-7), and the Clinical Global Impressions-Improvement (CGI-I); each was analyzed at end of study. Responder rates on CGI scales and the AISRS were also assessed.
Results
A total of 374 subjects were randomized. At end of study, the mean viloxazine ER dose was 504 mg. The reduction in the change from baseline at end of study AISRS total score (least-square means ± standard error) was significantly greater in subjects treated with viloxazine ER (−15.5 ± 0.91) compared with placebo (−11.7 ± 0.90), p = 0.0040. The reduction in the CGI-S score was also significantly greater in subjects treated with viloxazine ER (−1.4 ± 0.10) compared with placebo (−1.0 ± 0.10), p = 0.0023. The viloxazine ER group demonstrated significantly greater improvements in the AISRS Inattention (p = 0.0015) and Hyperactivity/Impulsivity (p = 0.0380) subscales, the CGI-I (p = 0.0076), and the BRIEF-A Global Executive Composite (p = 0.0468) and Metacognition Index (p = 0.0100). Analysis of categorical secondary endpoints revealed that the viloxazine ER group had a significantly higher AISRS 30% response rate compared with placebo (p = 0.0395); all other comparisons were not significant. Many treatment effects (including the primary and key secondary endpoints) were significant by week 2. The most common treatment-related adverse events that occurred in ≥5% of subjects receiving viloxazine ER were insomnia (14.8%), fatigue (11.6%), nausea (10.1%), decreased appetite (10.1%), dry mouth (9.0%), and headache (9.0%). Viloxazine ER was well tolerated, with a 9.0% discontinuation rate due to adverse events compared with 4.9% in the placebo group.
Conclusions
Treatment with viloxazine ER resulted in a statistically significant improvement in primary and key secondary endpoints, indicating improvements in attention-deficit/hyperactivity disorder symptomology, executive function, and overall clinical illness severity in adults. Viloxazine ER was well tolerated at the tested doses in adults with attention-deficit/hyperactivity disorder.
Clinical Trial Registration
Clinicaltrials.gov identifier: NCT04016779.
Plain Language Summary
Attention-deficit/hyperactivity disorder (ADHD) is a condition characterized by inattention (difficulty maintaining focus), and/or impulsiveness/hyperactivity. In 2021, a nonstimulant medication called viloxazine ER (brand name: Qelbree®) received US FDA-approval for ADHD in children and adolescents (aged 6 to 17 years), based on efficacy and safety demonstrated in clinical trials. Here we present results of a phase 3, randomized, double-blind, placebo-controlled, clinical trial that enrolled 374 adults with ADHD. In this trial, half the patients received viloxazine ER, and half received placebo (identical capsule without active ingredient). Medication doses ranged from 200–600 mg/day, based on symptom response and presence of side effects. To reduce bias, patients and investigators did not know which medication the patient was receiving. The primary measure of efficacy was the Adult ADHD Investigator Symptom Rating Scale (AISRS), a standardized questionnaire rating presence and severity of patient-reported ADHD symptoms. At the end of the 6-week trial, participants receiving viloxazine ER showed greater improvement in ADHD symptoms according to AISRS than those receiving placebo. Improvement was seen in both the Inattentive and Impulsive/Hyperactive components of ADHD and in other study measures, including a measure of behaviors called Executive Function. Viloxazine ER was generally safe and well-tolerated in the trial. The most common side effects were insomnia (14.8%), fatigue (11.6%), and nausea (10.1%). Overall, 9.0% of patients receiving viloxazine and 5% receiving placebo left the trial because of side effects. Due to these positive results, the US FDA recently approved viloxazine ER to treat adults with ADHD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Viloxazine extended release capsules (Qelbree®) is a novel nonstimulant that is US FDA approved for the treatment of attention-deficit/hyperactivity disorder (ADHD) in patients 6 years of age and older based on positive results from three pediatric pivotal phase III trials and one adult phase III trial, which is presented here. |
In this phase III trial, adults with ADHD treated with viloxazine extended release (200–600 mg/day) exhibited a significantly greater improvement in ADHD symptoms compared with placebo evaluated using the Adult ADHD Investigator Symptom Rating Scale. |
Viloxazine extended release was generally safe and well tolerated. |
1 Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder that typically begins in childhood, and persists into adulthood [1]; by one estimate, 90% of children with ADHD experience symptoms into adulthood [2]. The clinical presentation of ADHD core symptoms (i.e., inattention, impulsivity, and/or hyperactivity) typically changes over the lifespan [3,4,5,6]. While inattention may remain persistent, overt signs of hyperactivity may instead manifest as an internal restlessness, difficulty remaining still or seated, or an inability to relax [3,4,5,6]. Similarly, impulsivity may present as impatience, emotional lability, or inappropriate risk taking [3,4,5,6]. Consequently, diagnostic criteria have been updated in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) to be more inclusive of the symptoms and impairments that characterize ADHD in adulthood [1, 7]. Although ADHD was originally thought to remit in adolescence, it is now understood to persist into adulthood, with symptoms fluctuating over time. A recent long-term prospective study found that 64% of children, followed for 2–16 years, experienced periods of remission and recurrence into young adulthood [2]. These data suggest that, even if a patient’s ADHD appears to remit, there is a high likelihood of recurrence over time.
The prevalence of ADHD in adults has been estimated at 2.5–5.0% [8,9,10], with a contemporary meta-analysis indicating an even higher prevalence of 7% worldwide [11], making it among the most common adult psychiatric disorders [12,13,14]. The burden of illness associated with ADHD in adulthood affects multiple areas of a person’s life, and may result in lower educational and financial achievements, reduced job performance, greater social isolation, and overall decreased quality of life [15]. Adults with ADHD have shown lower self-esteem [16], greater sleep disturbances [17], and an increased risk of mortality [18, 19] and comorbidities such as depression, anxiety, and substance use disorders compared with non-ADHD adults [20, 21]. Accordingly, the cumulative negative consequences of living with ADHD in adulthood can substantially impact an individual’s social, emotional, educational, professional, and economic well-being. Fortunately, adults receiving treatment for ADHD experience meaningful improvements across a variety of functional measures, including academic, antisocial behavior, obesity, occupation, self-esteem, and social function outcomes [22, 23], positive effects that have been corroborated in a recent network meta-analytical report [24].
An extended-release capsule formulation of viloxazine (viloxazine ER; Qelbree®) was approved in April 2021 by the US Food and Drug Administration for the treatment of ADHD in children and adolescents (ages 6–17 years). The therapeutic effects of this novel nonstimulant medication are thought to be owing to its action as a norepinephrine reuptake inhibitor; however, contemporary preclinical studies indicate that it may also act on serotonergic signaling in the brain, though the translational effect in humans remains to be fully elucidated [25, 26]. In three phase III, randomized, placebo-controlled clinical trials in children [27, 28] and adolescents [29], viloxazine ER statistically significantly and clinically meaningfully [30, 31] reduced ADHD symptoms and improved functional impairment [32], executive function [44], and learning/school performance [33]. Additionally, viloxazine ER showed no pharmacokinetic interactions with ADHD stimulant treatments (e.g., lisdexamfetamine and methylphenidate) [34, 35] nor was the pharmacokinetics of viloxazine ER meaningfully affected by strong cytochrome P450 (CYP) 2D6 inhibitors such as paroxetine or the presence of CYP2D6 genetic polymorphisms [36, 37]. The aim of this study was to evaluate the efficacy and safety of viloxazine ER in the treatment of ADHD in adults.
2 Methods
2.1 Study Design
This was a phase III, randomized, double-blind, placebo-controlled, parallel-group, flexible-dose, multicenter clinical trial evaluating the efficacy and safety of viloxazine ER 200–600 mg/day in adults with ADHD. This study was conducted at 38 research centers in the USA (NCT04016779). The study schematic is presented in Fig. 1. After signing the informed consent, potential subjects underwent initial screening evaluation at visit 1 to confirm eligibility. Eligible subjects returned to the center for visit 2 (baseline/randomization; day 1) within 35 days of screening. At this visit, subjects who continued to meet inclusion/exclusion criteria and had a negative urine drug screen were randomized 1:1 to viloxazine ER flexible-dose or matched-placebo arms using a parallel design. Randomization and allocation to study treatment occurred centrally via an interactive web response system using a randomization schedule to determine treatment assignment. The randomization schedule was generated using SAS® PROC PLAN. All study subjects and all personnel involved with the conduct and interpretation of the study, including care providers, investigators, and outcome assessors were blinded to randomization schedule and study medication.
Study design. Clinical trial design illustrating timing of study visits, efficacy assessments, and dose titration. Fixed doses were used during weeks 1 and 2; flexible doses of viloxazine extended release (ER) were used during weeks 3–6. Efficacy assessments were conducted at screening, baseline, and the end of weeks 1, 2, 3, 4, and 6. No study visit was scheduled at the end of week 5. AISRS Adult ADHD Investigator Symptom Rating Scale, BRIEF-A Behavior Rating Inventory of Executive Function-Adult Version, CGI Clinical Global Impressions scale, CGI-I CGI-Improvement, CGI-S CGI-Severity, EOS end of study, GAD-7 General Anxiety Disorder-7 scale
Study medication (provided as viloxazine ER 200-mg capsules or matching placebo capsules) was administered once daily in the morning with or without food for the 6-week treatment period. During weeks 1 and 2, all subjects took two capsules once daily. Subjects assigned to viloxazine ER received viloxazine ER 200 mg (one viloxazine ER capsule and one placebo capsule) once daily during week 1 and viloxazine ER 400 mg (two viloxazine ER capsules) once daily during week 2. Subjects assigned to placebo took two placebo capsules. At study visits from week 3 through week 6, at the investigator’s discretion, the subject’s dose could be titrated to three capsules (maximum 600 mg/day) or tapered to one capsule (minimum of 200 mg/day) in increments of 200 mg/day per week based on the subject’s clinical response and tolerability. Study medication compliance was assessed at each study visit by comparing the number of medication doses returned to the number dispensed. If a subject missed doses of the study medication, the investigator counseled the subject on the importance of compliance. Subjects who consistently missed doses could be discontinued from the study at the discretion of the site investigator.
At each scheduled post-baseline study visit (weeks 1, 2, 3, 4, and 6), subjects underwent efficacy and safety evaluations. Recent phase III pediatric studies demonstrated that most improvement occurred from the start of treatment through weeks 3 or 4, and stabilized by week 5 [27,28,29, 38]; therefore, no visit was scheduled at week 5 in the present study in order to minimize the burden on subjects and sites.
In order to minimize the placebo/nocebo response in this trial [39], site staff and investigator/raters completed a didactic tutorial and video training on placebo response prior to the initiation of the trial, and subjects viewed a training video on placebo response prior to any assessments at screening (visit 1) and baseline (visit 2) and post-randomization after week 2 and week 4 of treatment (visits 4 and 6, respectively). Subjects who completed the study were eligible to enroll in a separate open-label extension safety study (NCT04143217). Subjects who did not enroll in the open-label extension safety study received a phone call 1 week after completing the double-blind end-of-study (EOS) visit for the safety follow-up.
2.2 Subjects
2.2.1 Inclusion criteria
Male and female individuals aged 18–65 years were eligible to participate if they had a primary diagnosis of ADHD per the DSM-5, made at least 6 months prior to screening. The ADHD diagnosis was also confirmed with the Structured Clinical Interview for DSM-5 Clinical Trials version at screening. Subjects were required to have an Adult ADHD Investigator Symptom Rating Scale (AISRS) total score ≥26 and a Clinical Global Impressions - Severity of Illness (CGI-S) score ≥4 (i.e., moderately ill or worse) at screening and baseline (day 1). Subjects were required to have a body mass index between 18.0 and 35.0 kg/m2, and be able to swallow capsules whole without crushing, chewing, or cutting. Subjects had to be considered medically healthy by the study investigator based on a physical examination, medical history, clinical laboratory tests, vital signs, and electrocardiogram (ECG).
Subjects were also required to refrain from taking other ADHD medications for a minimum of 1 week or five half-lives (whichever was longer) prior to baseline (day 1) and for the study duration, and refrain from taking any other investigational drugs, prohibited medications, or known CYP1A2 substrates (viloxazine ER is a CYP1A2 inhibitor) within 30 days or five half-lives prior to baseline (whichever was longer). Although caffeine is a CYP1A2 substrate, its use was not prohibited during the trial.
2.2.2 Exclusion Criteria
Subjects with treatment-resistant ADHD (i.e., two or more approved ADHD medications had failed to adequately improve the subject’s symptoms) were excluded, but subjects who were naïve to ADHD treatment were eligible. Subjects who had a history of autism, schizophrenia, schizoaffective disorder, bipolar disorder, post-traumatic stress disorder, obsessive-compulsive disorder, personality disorder, or who had a current diagnosis of any psychiatric disorder (other than ADHD) according to the DSM-5 were excluded. However, provided ADHD was the primary diagnosis, subjects who had a secondary diagnosis of major depressive disorder, nicotine dependence, social anxiety disorder, generalized anxiety disorder, or phobias were allowed to participate if the subject was not receiving pharmacological treatment for the comorbidity/secondary diagnoses at the time of screening and for the duration of the study. Regardless of the presence of any secondary diagnosis, subjects who had a Symptoms of Depression Questionnaire mean score >3.0 or a Hamilton Anxiety Rating Scale score >21 were excluded from study participation, as were subjects with evidence of suicidality (defined as more than one lifetime suicide attempt, or active suicidal plan or thoughts within the past 6 months).
Subjects with a major neurological disorder (including seizures or a history of seizure disorder within the immediate family, or a history of seizure-like events), cardiovascular disorder, arrhythmia, clinically relevant vital sign abnormality and/or systemic disease that took priority over treatment of ADHD or that would affect study assessments were excluded. Subjects were also excluded if they had a positive drug screen for drugs of abuse during the screening period, were identified as a chronic or habitual cannabis user, or had a current diagnosis or history of substance use disorder, including alcohol use disorder (per DSM-5 criteria), within the past year or were assessed as having regularly consumed excessive alcohol within the past year. Additionally, subjects with a history of intolerance or allergic reaction to viloxazine or its excipients were excluded. Finally, subjects who were pregnant, breastfeeding, or refused to practice abstinence or acceptable birth control throughout the study were excluded. A urine pregnancy test (female individuals of childbearing potential only), and a rapid point-of-collection urine drug screen was conducted prior to efficacy and safety assessments at baseline and all post-baseline study visits. If either test was positive, only safety assessments would be performed at the visit, and the subject would be discontinued.
2.3 Efficacy Assessments
2.3.1 Investigator-Rated Scales
The AISRS is an 18-item symptom (presence and severity) scale for use in adults with ADHD [40]. It is equally divided into two subscales for inattention (nine items) and hyperactivity/impulsivity (nine items), and conducted as a semi-structured interview by a trained clinician investigator [40]. Each item is rated on a 4-point scale (0 = none to 3 = severe). The sum of the 18 items yields a total score, with a range from 0 to 54 (0 to 27 for each subscale). The higher the score, the more severe the ADHD symptoms [40]. The AISRS was conducted at each study visit from screening to EOS (i.e., visit 1 to visit 7).
The CGI scales (CGI-S and CGI-Improvement [CGI-I]) were conducted by the same clinician who performed the AISRS and administered as brief stand-alone global assessments of symptom severity or change from the clinician’s perspective [41]. The CGI-S rating reflects a subject’s ADHD symptom severity relative to the clinician’s total experience with patients with ADHD. The CGI-S is rated on a 7-point scale, where 1 = normal, not at all ill, asymptomatic, 2 = borderline ill, 3 = mildly ill, 4 = moderately ill, 5 = markedly ill, 6 = severely ill, and 7 = among the most extremely ill patients. The CGI-S was conducted at each study visit from screening to week 6 (EOS).
The CGI-I rating represents the clinician’s opinion of how much the subject’s condition has changed (improved, worsened, or no change) during treatment relative to the subject’s condition at baseline before treatment. The CGI-I is rated on a 7-point scale where 1 = very much improved, 2 = much improved, 3 = minimally improved, 4 = no change, 5 = minimally worse, 6 = much worse, and 7 = very much worse. The baseline CGI-S assessment served as a basis for the investigator’s assessment of CGI-I during the treatment period. The CGI-I was conducted at each post-baseline study visit (week 1 to week 6 [EOS]).
2.3.2 Self-Reported Scales
The Behavior Rating Inventory of Executive Function - Adult Version (BRIEF-A) Self-Report assesses aspects of executive function and problems with self-regulation from the perspective of the subject [42, 43]. The BRIEF-A is a 75-item scale with nine nonoverlapping clinical scales that comprise two summary index scales, the Behavioral Regulation Index and the Metacognition Index. The Behavioral Regulation Index assesses the individual’s ability to control one’s behavior and emotional responses. The Metacognition Index assesses the individual’s ability to initiate activity and generate problem-solving ideas, sustain working memory, plan/organize problem-solving approaches, monitor success/failure in problem solving, and organize materials/environment. The two indices combined provide an overall assessment of executive function, termed the Global Executive Composite. The BRIEF-A has been used to assess executive function across a variety of neurological and psychiatric disorders, including ADHD [44, 45]. Subjects rate each item on a 3-point scale (1 = never, 2 = sometimes, or 3 = often) based on their experiences within the last month. BRIEF-A raw scores were converted to T-scores, where higher T-scores indicate worse executive function. The BRIEF-A was administered at baseline and EOS.
The Generalized Anxiety Disorder 7-Item scale (GAD-7) measures the severity of generalized anxiety disorder symptoms [46]. The subject rates each item on a 4-point scale based on the previous 2 weeks, where 0 = not at all, 1 = several days, 2 = over half the days, and 3 = nearly every day. All seven items are summated to yield a total score (range 0–21) with higher scores indicating greater anxiety. The GAD-7 was administered every 2 weeks to subjects at baseline and weeks 2, 4, and 6 (EOS).
2.4 Endpoints and Statistical Analysis
The safety population included all randomized subjects who received at least one dose of study medication; the full analysis set (FAS) population for efficacy included all randomized subjects who took at least one dose of study medication and had a baseline and at least one post-baseline AISRS assessment. Sample size calculations indicated that, assuming a Cohen’s d effect size of 0.407, 128 subjects per treatment group (256 total subjects for two arms) in the FAS population would yield 90% power across treatment groups at a significance level of 0.05 (two-sided) to reject the null hypothesis. The targeted sample size was adjusted to 366 subjects (183 per arm) to account for an expected dropout rate of 30%. The type I error rate was controlled at the 5% significance level by using sequential (hierarchical) testing for the primary and key secondary efficacy endpoints. The key secondary endpoint would only be tested if treatment with viloxazine ER was significantly different for placebo for the primary endpoint. No adjustments were made for multiple comparisons for other endpoints. All statistical analyses were performed using SAS version 9.4 or higher.
2.4.1 Primary Endpoint
The primary efficacy endpoint was the change from baseline (CFB) at EOS in the AISRS total score, analyzed using a mixed model for repeated measures (MMRM), which assumes that missing data are missing at random. The MMRM analysis uses all available data, including subjects with partial data (i.e., with missing data) to arrive at an estimate of the mean treatment effect without filling in the missing values. The MMRM model included CFB in the AISRS score as the dependent variable, and fixed-effect terms for baseline AISRS total score, treatment, study visit, and treatment-by-study visit interaction as independent variables. The primary comparison was between viloxazine ER and placebo at EOS (i.e., week 6).
The model parameters were estimated using the restricted maximum likelihood method with an unstructured variance-covariance matrix and Kenward–Roger approximation to estimate denominator degrees of freedom. If the unstructured covariance model failed to converge, the first (co)variance structure that did not have a convergence problem was used for the analysis from the following ordered list: (1) Toeplitz, (2) autoregressive of order 1, and (3) compound symmetry. A sensitivity analysis was performed and assumed that missing AISRS total scores were missing not at random.
2.4.2 Key Secondary Endpoint
The key secondary efficacy endpoint was the CFB at EOS in the CGI-S score, analyzed using MMRM. The model included CFB at EOS in CGI-S score as the dependent variable, the baseline CGI-S score as a covariate, and treatment, study visit, and treatment-by-study visit interaction as independent fixed-effect variables.
2.4.3 Additional Secondary Endpoints
Additional secondary endpoints assessing continuous variables at EOS included: the CFB AISRS Inattention and Hyperactivity/Impulsivity subscale scores (analyzed via MMRM); the CFB BRIEF-A T-score for Global Executive Composite, the Behavioral Regulation Index, and the Metacognition Index (analyzed via analysis of covariance with baseline T-scores and treatment as fixed independent variables); and the CFB GAD-7 total score (analyzed via MMRM). The absolute CGI-I score was analyzed using MMRM with the CGI-I score as the dependent variable, the baseline CGI-S score as a covariate, and treatment, study visit, and treatment-by-study visit interaction as independent fixed-effect factors.
Additional secondary endpoints assessing categorical variables at EOS included: the AISRS 30% responder rate (the percentage of subjects with a ≥30% reduction in the CFB AISRS total score), the AISRS 50% responder rate (the percentage of subjects with a ≥50% reduction in the CFB AISRS total score), and CGI-S and CGI-I responder rates (the percentage of subjects with a score ≤2). Between-group difference in responder rates was analyzed using a two-sided Pearson’s chi-squared test.
2.4.4 Safety Endpoints
Safety and tolerability were assessed by monitoring the incidence of treatment-emergent adverse events (TEAEs), including assessment of severity, relationship to study medication and seriousness, as well as laboratory tests, vital signs, 12-lead ECG, physical examination, and the Columbia-Suicide Severity Rating Scale. In addition, AEs of special interest, defined as seizure or AEs that might represent a seizure, including, but not limited to, syncope/syncopal episode, pseudoseizure, myoclonus, and severe muscle spasms were evaluated. No inferential statistics were performed on safety or tolerability measures.
3 Results
3.1 Demographics and Baseline Characteristics
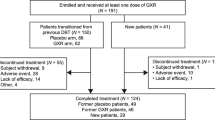
The trial was conducted between November 2019 and October 2020. A total of 601 subjects were screened (Fig. 2); 27.6% failed to meet eligibility and were not randomized. A total of 374 subjects were randomized (viloxazine ER, n = 190; placebo, n = 184), with 372 subjects in the safety population (viloxazine ER, n = 189; placebo, n = 183) and 354 subjects in the FAS population (viloxazine ER, n = 175; placebo, n = 179) (Table 1).
Disposition of subjects. Asterisk: One patient randomized to placebo was randomized in error and discontinued prior to receiving treatment with study medication; one subject randomized to viloxazine extended release (ER) had a positive pregnancy test and was withdrawn from the study prior to receiving treatment with study medication. N number of subjects
Demographics and baseline characteristics in the placebo and viloxazine ER treatment groups were similar (Table 1), as were the baseline AISRS total and subscale scores (Table 2) and CGI-S score (Table 3). Most subjects were male (54.8%) and white (78.5%). Stimulant medications or atomoxetine had been previously used by approximately 23% of subjects (~24% viloxazine ER and ~21% placebo). Of those subjects with data available at week 6, 60.2% (n = 80) of subjects in the viloxazine ER group were receiving 600 mg per day versus 81.2% (n = 121) of subjects in the placebo group, 31.6% (n = 42) were receiving 400 mg per day versus 17.4% (n = 26) placebo, and 8.3% (n = 11) were receiving 200 mg per day versus 1.3% (n = 2) placebo. The mean dose at week 6 was viloxazine ER 504 mg.
3.2 Primary Endpoint: Adult ADHD Investigator Symptom Rating Scale (AISRS)
At week 6 (EOS), the reduction (improvement) in the AISRS total score (CFB; least-squares [LS] mean ± standard error [SE]) was significantly greater in the viloxazine ER group (−15.5 ± 0.91) than in the placebo group (−11.7 ± 0.90), and the difference (−3.7 ± 1.28) was statistically significant (p = 0.0040). Both placebo and viloxazine ER-treated groups demonstrated a decrease in AISRS total score each week (relative to baseline); however, the improvement was significantly greater in the viloxazine ER group as early as week 2 (p = 0.0397) and at each assessment timepoint through EOS (p < 0.01) (Fig. 3a).
Adult ADHD Investigator Symptom Rating Scale (AISRS). Results from the AISRS demonstrate significant symptomatic improvements within 2 or 3 weeks following initiation of viloxazine extended release (ER) treatment and continuing through end of study (EOS). This was true for the changes from baseline in the AISRS total score (a), the Inattention subscale (b), and the Hyperactivity/Impulsivity subscale (c) (baseline plotted as 0 for reference). Significantly more subjects treated with viloxazine ER responded to treatment as assessed by an AISRS reduction of 30% (d) and 50% (e) response criteria from baseline. No study visit was scheduled for week 5. a–c Shown as least-squares means ± standard error; d, e are percent of subjects. *p < 0.05; **p < 0.01; ***p < 0.001 (relative to placebo). ADHD attention-deficit/hyperactivity disorder
3.3 Key Secondary Endpoint: Clinical Global Impression-Severity of Illness (CGI-S)
At week 6 (EOS), the reduction in the CGI-S score (CFB; LS mean ± SE) was significantly greater (improved, relative to baseline) in the viloxazine ER group (−1.4 ± 0.10) than the placebo group (−1.0 ± 0.10), p = 0.0023 (Table 3, Fig. 4a). Although both groups demonstrated a decrease in the CGI-S score at each assessment timepoint, the viloxazine ER group consistently demonstrated significantly greater improvement relative to placebo, starting at week 2 (p = 0.0203), and at each subsequent assessment through EOS (p < 0.01).
Clinical Global Impressions (CGI) scales. Results from the CGI scales demonstrate significant overall improvements beginning within 2 weeks of treatment with viloxazine extended release (ER) and continuing through end of study (EOS) on the Clinical Global Impressions-Severity of Illness scale (CGI-S) change from baseline (a) and Clinical Global Impressions-Improvement (CGI-I) scale raw scores (b). Significantly more subjects treated with viloxazine ER responded to treatment (i.e., score of 1 or 2) as assessed by CGI-S (c) and CGI-I (d) response criteria on weeks 2, 3, and 4. No study visit was scheduled for week 5. a, b Shown as least-squares means ± standard error; c, d are percent of subjects. *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001 (relative to placebo)
3.4 Additional Secondary Endpoints; Continuous Variables
3.4.1 AISRS Inattention and Hyperactivity/Impulsivity Subscales
Both placebo and viloxazine ER groups demonstrated notable decreases (improvement) in AISRS Inattention and Hyperactivity/Impulsivity subscale scores with each week of treatment. Viloxazine ER-treated subjects improved more than placebo-treated subjects, with a significantly lower LS mean score at EOS for the Inattention subscale (p = 0.0015) and for the Hyperactivity/Impulsivity subscale (p = 0.0380). Significantly greater improvement was observed at every timepoint for the Inattention subscale beginning at week 2 (p = 0.0113) through EOS (p-values < 0.01) (Table 2, Fig. 3b) and for the Hyperactivity/Impulsivity subscale beginning at week 3 (p = 0.0073) through to EOS (p-values < 0.05) (Table 2, Fig. 3c).
3.4.2 Clinical Global Impressions-Improvement (CGI-I)
At week 6 (EOS), the absolute LS mean (± SE) CGI-I score was significantly lower (i.e., greater improvement) in the viloxazine ER group (2.6 ± 0.09) than in the placebo group (2.9 ± 0.09), p = 0.0076. Although both groups demonstrated a decrease (improvement) in CGI-I score at each assessment timepoint, the viloxazine ER group demonstrated a significantly greater improvement on this measure relative to placebo starting at week 2 (p = 0.0156) and at each subsequent assessment through EOS (p-values <0.05) (Table 3, Fig. 4b).
3.4.3 Behavior Rating Inventory of Executive Function-Adult (BRIEF-A)
At baseline, mean (± standard deviation [SD]) Global Executive Composite T-score on the BRIEF-A was similar between placebo (70.9 ± 10.93) and viloxazine ER (71.0 ± 10.09) groups (Table 3). At EOS, the viloxazine ER-treated subjects had lower (i.e., improved) mean (± SD) T-scores than placebo-treated subjects (61.4 ± 12.5 vs 63.8 ± 12.8, respectively). The reduction (improvement) in Global Executive Composite T-scores (CFB; LS mean ± SE) at EOS was significantly greater in the viloxazine ER group (−9.3 ± 0.87) versus the placebo group (−6.8 ± 0.85), p = 0.0468, suggesting that viloxazine ER improved executive function more than placebo. Similar analyses of the BRIEF-A indices demonstrated a significant treatment effect for the Metacognition Index (viloxazine ER = −9.8 ± 0.92, placebo = −6.5 ± 0.90, p = 0.0100), but not for the Behavioral Regulation Index (p = 0.4462).
3.4.4 Generalized Anxiety Disorder 7-Item Scale
At baseline, 45 of 179 (25.1%) placebo subjects and 35 of 175 (20.0%) viloxazine ER subjects had a GAD-7 total score of 10 or greater (associated with moderate to severe anxiety symptoms [46]). The mean (± SD) GAD-7 total score at baseline was similar between the viloxazine ER (6.0 ± 4.63) and the placebo group (6.4 ± 4.96) (Table 3). At EOS, the LS mean (± SE) CFB GAD-7 total score between the viloxazine ER group (−1.6 ± 0.31) and the placebo group (−1.6 ± 0.30) was not statistically different (p = 0.9205).
3.5 Additional Secondary Endpoints; Categorical Variables
3.5.1 AISRS 30% Responder Rate Analysis
The AISRS 30% responder rate was significantly greater in the viloxazine ER group (60.0%) compared with placebo (47.6%) at EOS (p = 0.0395); it was also greater (p-values < 0.05) in the viloxazine ER group compared with placebo at every visit starting from week 2 (Table 2, Fig. 3d).
3.5.2 AISRS 50% Responder Rate Analysis
The AISRS 50% responder rate was not statistically different between viloxazine ER (39.2%) and placebo (32.9%) at EOS (p = 0.2736), although significant differences (p-values < 0.05) favoring viloxazine ER were observed at weeks 2, 3, and 4 (Table 2, Fig. 3e).
3.5.3 Clinical Global Impressions-Severity of Illness (CGI-S) Responder Rate
The CGI-S responder rate was not statistically different between viloxazine ER (30.8%) and placebo (25.2%) at EOS (p = 0.3030), although significant differences (p-values < 0.01) favoring viloxazine ER were observed at weeks 2, 3, and 4 (Table 3, Fig. 4c).
3.5.4 Clinical Global Impressions-Improvement (CGI-I) Responder Rate
The CGI-I responder rate was also not statistically different between the viloxazine ER group (48.5%) compared to placebo (37.8%) at EOS (p = 0.0744), although significant differences (p-values < 0.05) favoring viloxazine ER were observed at weeks 2, 3, and 4 (Table 3, Fig. 4d).
3.6 Safety and Tolerability
3.6.1 Treatment-Emergent Adverse Events
Overall, 60.3% of subjects randomized to viloxazine ER experienced an AE (49.7% placebo). The most common TEAEs (occurring in ≥5% of subjects in any group) were insomnia (viloxazine ER [%] vs placebo [%]; 15.9% vs 4.9%), fatigue (12.2% vs 3.3%), nausea (12.2% vs 2.7%), decreased appetite (10.1% vs 2.7%), dry mouth (9.5% vs 2.2%), headache (12.2% vs 6.6%), and constipation (5.8% vs 1.1%) (Table 4). Most TEAEs were assessed by investigators as “mild” or “moderate” in severity; 5.3% receiving viloxazine ER (vs 1.1% placebo) experienced any TEAE assessed as “severe”, most commonly headache (n = 3, 1.6%) and insomnia (n = 2, 1.1%). Treatment-emergent adverse events were considered related to the study medication in 50.8% of subjects treated with viloxazine ER compared with 32.8% in those treated with placebo. The most common treatment-related TEAEs (considered related to the study medication by the site investigator and occurring in ≥5% of subjects in any group) were insomnia (14.8% vs 4.4%), fatigue (11.6% vs 2.7%), nausea (10.1% vs 2.2%), decreased appetite (10.1% vs 2.2%), dry mouth (9.0% vs 2.2%), and headache (9.0% vs 4.9%). Serious AEs were reported in only two subjects; both received placebo, and each event (congestive heart failure and pancreatitis) resulted in discontinuation. No subject taking viloxazine ER experienced any serious AE. There were no deaths in the study.
No subject experienced any AEs of special interest (seizure, seizure-like event, or myoclonus). More subjects in the viloxazine ER group had a TEAE that led to study discontinuation (9.0%) compared with the placebo group (4.9%) (Table 4). Treatment-emergent adverse events leading to study discontinuation in two or more viloxazine ER-treated subjects (and greater than placebo) were fatigue (n = 4), constipation (n = 3), insomnia (n = 3), and headache (n = 2).
3.6.2 Clinical Laboratory and Hematology Evaluations
Safety evaluation of laboratory test results revealed no remarkable changes between baseline and EOS for any clinical chemistry, hematology, or urinalysis parameter, and no important treatment group differences were observed. Likewise, evaluation of individual changes showed similar percentages of subjects with shifts from a value within the normal range at baseline to a high or low value at week 6, with the exception that more subjects in the placebo group (n = 12, 6.6%) had high bicarbonate values at EOS than the viloxazine ER group (n = 5, 2.6%). Instances of clinical chemistry abnormalities (relative to laboratory reference ranges) occurring in ≥5% of viloxazine ER-treated subjects included elevations in alanine aminotransferase (ALT; viloxazine ER, n = 18, 9.5%; placebo, n = 15, 8.2%), elevations in aspartate aminotransferase (AST; viloxazine ER, n = 18, 9.5%; placebo, n = 7, 3.8%), and observations of low blood urea nitrogen (viloxazine ER, n = 14, 7.4%; placebo, n = 11, 6.0%). For 11 subjects (viloxazine ER, n = 6; placebo, n = 5) abnormal laboratory values also represented TEAEs. One subject receiving viloxazine ER had TEAEs of positive urine leukocyte esterase and increased urine white blood cell count (each assessed as mild and not treatment related). Ten subjects (five viloxazine ER and five placebo) experienced a TEAE for increased transaminases, including ALT (all ten subjects) and AST (two viloxazine ER and three placebo). None of these elevations exceeded four times the upper limit of normal for viloxazine ER. None was considered severe, and none met criteria for a serious AE. The transaminase elevations were assessed as possibly related to study treatment in four of the five viloxazine ER-treated subjects (including the two subjects with both ALT and AST elevations) and in three of the five placebo-treated subjects (all of whom had elevations in both ALT and AST, though for one of these subjects, only the AST elevation was assessed as possibly related whereas the ALT elevation was judged as unlikely related). For two of the five subjects with AST and ALT elevations (one receiving viloxazine ER and one receiving placebo), the transaminase elevations resulted in study discontinuation. Transaminases subsequently returned to normal in each subject.
3.6.3 Vital Signs, Physical Examinations, Electrocardiograms (ECGs), and Suicidality
Evaluation of vital signs, body weight, ECG, and physical examination results did not indicate any safety concerns. There were no important between-group changes in vital signs. At any given study visit, no more than 7% of overall subjects experienced shifts from normal to high or low vital sign measurements. Five subjects had changes in blood pressure recorded as TEAEs (three placebo, two viloxazine ER). One subject in the placebo group experienced a TEAE of hypertension, which was considered moderate in severity and not related to the study medication. Additionally, two subjects (1.1%) in the placebo group had increased blood pressure reported as a TEAE, as did one subject (0.5%) in the viloxazine ER group; all were considered mild in severity and not related to study medication. One subject (0.5%) in the viloxazine ER group had increased diastolic and increased systolic blood pressure reported as TEAEs; both were assessed as mild and although each was considered possibly related to the study medication, both resolved without medication dose changes.
There was no evidence of a treatment effect on physical examination parameters. Decreased body weight was reported as a TEAE for two subjects (1.1%) in the viloxazine ER treatment group (none in the placebo group). Increased body weight was reported as a TEAE for one subject (0.5%) in the placebo group, but not for any subjects in the viloxazine ER treatment group. All weight changes were assessed as related to the study medication.
There was no evidence of a treatment effect on ECG parameters. At EOS, QT interval corrected for heart rate using Fridericia’s method (QTcF) was <450 ms for all participants except for three subjects (1.9%) in the placebo group and in two subjects (1.3%) in the viloxazine ER group who had QTcF intervals >450 ms but ≤480 ms. Likewise the CFB in QTcF interval was ≤30 ms for all but two subjects (1.2%) in the placebo group and two subjects (1.3%) in the viloxazine ER group who had excursions >30 to ≤60 ms. There were no excursions >60 ms and no QTcF values >480 ms.
According to Columbia-Suicide Severity Rating Scale assessments, at the baseline visit one subject (0.5%) in the viloxazine ER group reported suicidal ideation, and one subject (0.5%) in the viloxazine ER group reported non-suicidal self-injurious behavior. During the treatment period, three subjects (1.6%) in the viloxazine ER group reported suicidal ideation. One of these subjects reported suicidal ideation at week 1; the subject had no prior history of suicidal ideation, suicidal ideation was reported as an AE (mild in severity and possibly related to the study medication), and the subject was discontinued at week 1 because of an AE of insomnia after only taking two doses of the study medication. One subject reported suicidal ideation at week 3, week 4, and week 6; the subject had a history of suicidal ideation and a suicide attempt, but no suicide attempt in past 6 months prior to screening. Suicidal ideation was reported as an AE starting at week 3 until week 6 (mild in severity and not related to the study medication) and the subject was discontinued because of noncompliance (prohibited medication). The last subject reported suicidal ideation at week 6 and had no prior history of suicidal ideation and/or behavior; suicidal ideation was not reported as an AE. No subject in the placebo group reported suicidal ideation in this trial. No subject in either treatment group reported suicidal behavior or a suicide attempt or committed suicide during this trial.
4 Discussion
In this phase III trial in adults with ADHD, the primary efficacy endpoint (CFB at EOS in the AISRS total score) was met. Specifically, treatment with viloxazine ER resulted in a statistically significant improvement on the AISRS, indicating an improvement in ADHD symptoms and associated functional impairment after only 2 weeks of treatment, and was demonstrable at every timepoint thereafter (Fig. 3a). Similar improvement was observed for both AISRS Inattention and Hyperactivity/Impulsivity subscales, in which viloxazine ER statistically significantly improved symptoms of inattention within 2 weeks of treatment (Fig. 3b), and hyperactivity/impulsivity within 3 weeks (Fig. 3c). In addition, this study also met its key secondary endpoint (CFB at EOS in the CGI-S score). Treatment with viloxazine ER improved scores on this measure of overall illness severity at each clinic visit starting from week 2 through EOS (Fig. 4a). Likewise, CGI-I scores also demonstrated statistically significant overall improvement relative to placebo starting at week 2 (Fig. 4b). Consistent efficacy was thus demonstrated by viloxazine ER across various measures of ADHD symptomatology (including both inattention and hyperactivity/impulsivity) and functional impairment. The significant improvement on CGI-S and CGI-I supports the clinical relevance of ADHD symptom reduction noted on the AISRS.
These results are consistent with those published from three recent phase III pivotal trials in children and adolescents with ADHD, in which viloxazine ER statistically significantly reduced ADHD symptoms and improved overall function [27,28,29]. Specifically, scores on the ADHD Rating Scale, Fifth Edition began to improve after 1 week of treatment with viloxazine ER with continued improvement for several weeks thereafter [27,28,29]. Improvement was seen in both inattention and hyperactivity/impulsivity subscales. Similarly, the CGI-I scores at EOS were significantly improved relative to placebo in these pediatric studies (average score approximately 2.5 at EOS) [27,28,29, 38]. In the present study, after 6 weeks of treatment with viloxazine ER, subjects averaged a final CGI-I score of 2.6, suggesting considerable agreement between adult and pediatric studies.
In the present analysis, the percentage of responders was evaluated by several metrics: AISRS 30% and 50% responder rates and CGI-S and CGI-I responder rates. For the AISRS 30% responder rate, a significantly greater percentage of subjects receiving viloxazine ER versus placebo responded to treatment at all timepoints from week 2 to EOS, with 60% in the viloxazine ER group vs 48% in the placebo group achieving this level of response by EOS (Fig. 3d). These data are consistent with a recent post-hoc analysis of the four pediatric viloxazine ER pivotal trials (including a negative trial [38] with an unusually high placebo response) [31]. This post-hoc analysis found that, by EOS, a greater percentage of viloxazine ER-treated pediatric subjects (59%) responded to treatment (defined as a ≥30% improvement on the ADHD Rating Scale, Fifth Edition) versus placebo-treated subjects (41%) [31]. While the placebo response may have been more robust among adult subjects, responder rates for the viloxazine ER groups have been consistently around 60%, across pediatric and adult trials [39].
For the 50% responder rate, a statistically significantly greater percentage of subjects in the viloxazine ER group compared with the placebo group responded at weeks 2, 3, and 4, but not at week 6. This was despite a similar 50% responder rate for viloxazine ER at week 6 as for prior weeks of treatment (Fig. 3e). Similarly, for both CGI-S and CGI-I responder rates, while a statistically significantly greater percentage of viloxazine ER-treated subjects responded to treatment (Fig. 4c, d) at weeks 2, 3, and 4, this was not the case at week 6. This may be explained by the lack of statistical power and inherent limitations of responder rate analyses. For instance, the responder rate analyses are additional secondary endpoints that were not considered when powering the sample size for this trial. Moreover, unlike the analyses of continuous variables using an MMRM or analysis of covariance, responder rates are binary data (e.g., responder or non-responder) and missing data points for subjects who drop out are not considered. Because subjects discontinue as the study progresses, sample sizes for responder rate analyses are smaller at the endpoint relative to the overall FAS population, resulting in reduced power to detect a treatment difference.
4.1 Measures of Executive Function and Anxiety
This study also assessed executive function via the BRIEF-A. Viloxazine ER improved scores on the Global Executive Composite (the composite of all nine scales) and the Metacognitive Index statistically significantly more than placebo. These data are consistent with a recent post-hoc analysis in pediatric subjects (6–17 years of age), where subjects treated with viloxazine ER demonstrated statistically significant improvements in executive function over placebo, as assessed by the Conners Third Edition Parent Short Form Executive Function content scale [47]. Improvement in the BRIEF-A Behavioral Regulation Index was not statistically significant in adult subjects in this study.
Although the BRIEF-A is not an ADHD-specific scale, executive dysfunction is a central component of ADHD impairment [48, 49] and executive function deficits (EFDs) are significantly more common among adults with ADHD relative to non-ADHD controls [50]. In a comparison between adults with ADHD and those without, secondarily stratified by whether they presented with EFDs, ADHD and EFDs were independently associated with a range of functional impairments, many of which occurred above and beyond the ADHD diagnosis alone [50, 51]. Further, employment rates have been shown to decrease from 100% among non-ADHD adults with EFDs, to 52% in adults with ADHD without EFDs, to only 6.7% in adults with ADHD and EFDs [51]. Executive function deficits in young adults were also highly predictive of academic performance in a sample of college students with ADHD and EFDs, even after controlling for factors such as ADHD symptom severity and baseline academic performance [52]. Not surprisingly, adults with ADHD and EFDs had significantly greater impairments in academic, occupational, and safety outcomes, relative to adults with EFDs but not ADHD, or with ADHD but no EFDs [50]. These reports underscore the importance of recognizing and addressing EFDs among adults with ADHD.
Importantly, subjects in the present study were not pre-selected for EFDs, nor were they stratified as such during the analysis. At baseline, both placebo and viloxazine ER groups had a mean BRIEF-A T-score above 65 on the Global Executive Composite (70.9 and 71.0, respectively), which is generally considered the threshold for clinical impairment [53]. This suggests that on average, both groups entered the study with clinically significant EFDs. After treatment with viloxazine ER in this short-term 6-week trial, both groups had a mean Global Executive Composite T-score <65 (63.8 and 61.4 for placebo and viloxazine ER, respectively), and the reduction from baseline was statistically significantly greater for viloxazine ER versus placebo. These changes are encouraging and continued assessments during long-term treatment will provide further support of viloxazine ER effects on executive function in adults with ADHD.
In this study, viloxazine ER did not separate from placebo on the GAD-7, although viloxazine has a long history of anxiolytic properties, detailed in studies from the 1970s and 1980s when viloxazine was commonly studied as an antidepressant [26, 54,55,56,57]. The mechanism of action also predicts not only antidepressant, but anxiolytic properties [26]. There are several plausible explanations for this negative finding. Subjects with severe general or social anxiety disorders (Hamilton Anxiety Rating Scale score >21) were explicitly excluded from the study at screening. As a result, at baseline, few subjects (<23%) had moderate-to-severe anxiety as assessed by the GAD-7 (where generalized anxiety disorder is associated with scores ≥10 [46]). Not surprisingly, placebo and viloxazine ER subjects had low mean (± SD) baseline GAD-7 scores of 6.4 ± 4.96 and 6.0 ± 4.63, respectively, which are consistent with only mild anxiety (i.e., scores 5–9) [46]. Thus, most subjects had mild, minimal, or no anxiety, thereby limiting the potential for improvement on this measure (i.e., floor effects) when the FAS population was analyzed at EOS. Second, because the GAD-7 was a secondary endpoint, this study was neither designed nor statistically powered for this assessment. Thus, the present sample (N = 354) may be an insufficient sample size upon which to draw robust conclusions from the analysis. Additionally, the study was conducted during the coronavirus disease 2019 pandemic, which may have affected the GAD-7 results.
The results of the trial should be considered in the context of limitations. The primary efficacy outcome measure was based on an investigator-rated scale. While the investigators were required to be qualified and to complete training on the scale, no inter-rater reliability data in this trial were collected. Additionally, no ratings of patient satisfaction with treatment were obtained in this study. In the same respect, there were no patient-reported outcome data collected during the trial, indicating the impact of coronavirus disease 2019 on aspects of the subjects daily living or ADHD symptoms before and during the pandemic.
4.2 Safety Profile
Safety data provided in this flexible dosing trial in adults with ADHD indicate viloxazine ER was tolerated with no reported serious AEs and <10% of viloxazine ER-treated subjects discontinuing as a result of an AE. Viloxazine ER was generally safe with most reported TEAEs being assessed by investigators as “mild” or “moderate” in severity. The occurrence of “severe” TEAEs was 5.3% in subjects receiving viloxazine ER (placebo 1.1%). The only TEAEs occurring with an incidence of at least 5% in viloxazine ER-treated subjects and greater than placebo were insomnia, fatigue, nausea, decreased appetite, dry mouth, headache, and constipation. Three subjects receiving viloxazine ER reported suicidal ideation during the treatment period (one of whom had a prior history of suicidality) with no subject reporting suicidal behavior. There were no remarkable mean changes in laboratory test results, vital signs, and body weight between screening and EOS. In summary, at doses between 200 and 600 mg, viloxazine ER was general safe and tolerable.
5 Conclusions
Significant improvements in ADHD symptoms, executive function, and overall clinical improvement were seen during treatment with viloxazine ER in adults with ADHD. Across several measures, significant improvements were seen within 2 weeks of treatment initiation. These results are consistent with those reported in recent phase III studies in children and adolescents with ADHD. In the present study, viloxazine ER was generally safe and tolerable.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
Sibley MH, Arnold LE, Swanson JM, Hechtman LT, Kennedy TM, Owens E, et al. Variable patterns of remission from ADHD in the multimodal treatment study of ADHD. Am J Psychiatry. 2022;179(2):142–51.
Weiss G, Hechtman LT. Hyperactive children grown up: ADHD in children, adolescents, and adults. 2nd ed. New York: Guilford Press; 1993.
Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. Am J Psychiatry. 2000;157(5):816–8.
Turgay A, Goodman DW, Asherson P, Lasser RA, Babcock TF, Pucci ML, et al. Lifespan persistence of ADHD: the life transition model and its application. J Clin Psychiatry. 2012;73(2):192–201.
Franke B, Michelini G, Asherson P, Banaschewski T, Bilbow A, Buitelaar JK, et al. Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. Eur Neuropsychopharmacol. 2018;28(10):1059–88.
Epstein JN, Loren RE. Changes in the definition of ADHD in DSM-5: subtle but important. Neuropsychiatry. 2013;3(5):455.
Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: A meta-analytic review. Neurotherapeutics. 2012;9(3):490–9.
Kessler RC, Adler LA, Barkley R, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey replication. Am J Psychiatry. 2006;163(4):716–23.
Faraone, S.V., Banaschewski, T., Coghill, D., Zheng, Y., Biederman, J., Bellgrove, M.A. et al. The world federation of ADHD international consensus statement: 208 evidence-based conclusions about the disorder. Neurosci. Biobehav. Rev. (2021).
Song P, Zha M, Yang Q, Zhang Y, Li X, Rudan I. The prevalence of adult attention-deficit hyperactivity disorder: A global systematic review and meta-analysis. J Glob Health. 2021;11(11):04009.
Reynolds K, Pietrzak RH, El-Gabalawy R, Mackenzie CS, Sareen J. Prevalence of psychiatric disorders in US older adults: Findings from a nationally representative survey. World Psychiatry. 2015;14(1):74–81.
Stein DJ, Seedat S, Herman A, Moomal H, Heeringa SG, Kessler RC, et al. Lifetime prevalence of psychiatric disorders in South Africa. Br J Psychiatry. 2008;192(2):112–7.
Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. Am J Public Health. 2007;97(1):68–75.
Brod M, Schmitt E, Goodwin M, Hodgkins P, Niebler G. ADHD burden of illness in older adults: a life course perspective. Qual Life Res. 2012;21(5):795–9.
Cook J, Knight E, Hume I, Qureshi A. The self-esteem of adults diagnosed with attention-deficit/hyperactivity disorder (ADHD): a systematic review of the literature. Attent Defic Hyperact Disord. 2014;6(4):249–58.
Wajszilber D, Santiseban JA, Gruber R. Sleep disorders in patients with ADHD: impact and management challenges. Nat Sci Sleep. 2018;10:453.
Sun S, Kuja-Halkola R, Faraone SV, D’Onofrio BM, Dalsgaard S, Chang Z, et al. Association of psychiatric comorbidity with the risk of premature death among children and adults with attention-deficit/hyperactivity disorder. JAMA Psychiat. 2019;76(11):1141–9.
Dalsgaard S, Østergaard SD, Leckman JF, Mortensen PB, Pedersen MG. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385(9983):2190–6.
Sobanski E. Psychiatric comorbidity in adults with attention-deficit/hyperactivity disorder (ADHD). Eur Arch Psychiatry Clin Neurosci. 2006;256(1):i26-31.
Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40(1):57–87.
Shaw M, Hodgkins P, Caci H, Young S, Kahle J, Woods AG, et al. A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: effects of treatment and non-treatment. BMC Med. 2012;4(10):99.
Boland H, DiSalvo M, Fried R, Woodworth KY, Wilens T, Faraone SV, et al. A literature review and meta-analysis on the effects of ADHD medications on functional outcomes. J Psychiatr Res. 2020;123:21–30.
Cortese S, Adamo N, Del Giovane C, Mohr-Jensen C, Hayes AJ, Carucci S, et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2018;5(9):727–38.
Yu C, Garcia-Olivares J, Candler S, Schwabe S, Maletic V. New insights into the mechanism of action of viloxazine: serotonin and norepinephrine modulating properties. J Exp Pharmacol. 2020;12:285–300.
Findling RL, Candler S, Nasser A, Schwabe S, Yu C, Garcia-Olivares J, et al. Viloxazine in the management of CNS disorders: a historical overview and current status. CNS Drugs. 2021;35:643–53.
Nasser A, Liranso T, Adewole T, Fry N, Hull JT, Chowdhry F, et al. A phase 3, randomized, placebo-controlled trial to assess the efficacy and safety of once-daily SPN-812 (viloxazine extended release) in the treatment of ADHD in school-age children. Clin Ther. 2020;42(8):1452–66.
Nasser A, Liranso T, Adewole T, Fry N, Hull JT, Busse GD, et al. Once-daily SPN-812 200 and 400 mg in the treatment of ADHD in school-aged children: a phase III randomized, controlled trial. Clin Ther. 2021;43(4):684–700.
Nasser A, Liranso T, Adewole T, Fry N, Hull JT, Busse GD, et al. A phase 3, placebo-controlled trial of once-daily viloxazine extended-release capsules in adolescents with attention-deficit/hyperactivity disorder. J Clin Psychopharmacol. 2021;41(4):370–80.
Nasser A, Kosheleff AR, Hull JT, Liranso T, Qin P, Busse GD, et al. Translating attention-deficit/hyperactivity disorder rating scale-5 and Weiss functional impairment rating scale-parent effectiveness scores into clinical global impressions clinical significance levels in four randomized clinical trials of SPN-812 (viloxazine extended-release) in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2021;31(3):214–26.
Nasser A, Kosheleff AR, Hull JT, Liranso T, Qin P, Busse GD, et al. Evaluating the likelihood to be helped or harmed after treatment with viloxazine extended-release in children and adolescents with attention deficit/hyperactivity disorder. Int J Clin Pract. 2021;75(8):1–11.
Nasser A, Hull JT, Liranso T, Busse GD, Melyan Z, Childress AC, et al. The effect of viloxazine extended-release capsules on functional impairments associated with attention-deficit/hyperactivity disorder (ADHD) in children and adolescents in four phase 3 placebo-controlled trials. Neuropsychiatr Dis Treat. 2021;17:1751–62.
Faraone SV, Gomeni R, Hull JT, Busse GD, Melyan Z, Rubin J, et al. A post hoc analysis of the effect of viloxazine extended-release capsules on learning and school problems in children and adolescents with attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry. 2021.
Faison SL, Fry N, Adewole T, Odebo O, Wang Z, Maletic V, et al. Pharmacokinetics of co-administered viloxazine extended-release (SPN-812) and lisdexamfetamine in healthy adults. J Clin Psychopharm. 2021;41(2):155–62.
Faison SL, Fry N, Adewole T, Odebo O, Wang Z, Maletic V, et al. Pharmacokinetics of co-administered viloxazine extended-release (SPN-812) and methylphenidate in healthy adults. Clin Drug Investig. 2020;41:149–59.
Wang Z, Adeojo LW, Odebo O, Adewole T, Qin P, Schwabe S, et al. Impact of SPN-812 (viloxazine extended-release) on select cytochrome P450 (CYP) activity and the evaluation of CYP2D6 polymorphisms on SPN-812 pharmacokinetics. In: Society of Biological Psychiatry 2021 annual meeting; 29 April–1 May, 2021; virtual.
Wang Z, Kosheleff AR, Adeojo LW, Odebo O, Adewole T, Qin P, et al. Impact of paroxetine, a strong CYP2D6 inhibitor, on SPN-812 (viloxazine extended-release) pharmacokinetics in healthy adults. Clin Pharmacol Drug Dev. 2021.
Nasser A, Liranso T, Adewole T, Fry N, Hull JT, Chowdhry F, et al. A phase 3 placebo-controlled trial of once-daily 400-mg and 600-mg SPN-812 (viloxazine extended-release) in adolescents with ADHD. Psychopharm Bul. 2021;51(2):43–64.
Faraone SV, Newcorn JH, Cipriani A, Brandeis D, Kaiser A, Hohmann S, et al. Placebo and nocebo responses in randomised, controlled trials of medications for ADHD: a systematic review and meta-analysis. Mol Psychiatry. 2022;27(1):212–9.
Spencer TJ, Adler LA, Qiao M, Saylor KE, Brown TE, Holdnack JA, et al. Validation of the adult ADHD investigator symptom rating scale (AISRS). J Attent Disord. 2010;14(1):57–68.
Guy W. ECDEU assessment manual for psychopharmacology. Rockville: U.S. Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs. 1976.
Gioia GA, Isquith PK, Guy SC, Kenworthy L. Test review behavior rating inventory of executive function. Child Neuropsychol. 2000;6(3):235–8.
Roth RM, Gioia GA. Behavior rating inventory of executive function-adult version. Lutz (FL): Psychological Assessment Resources; 2005.
Adler L, Tanaka Y, Williams D, Trzepacz PT, Goto T, Allen AJ, et al. Executive function in adults with attention-deficit/hyperactivity disorder during treatment with atomoxetine in a randomized, placebo-controlled, withdrawal study. J Clin Psychopharmacol. 2014;34(4):461–6.
Roth RM, Lance CE, Isquith PK, Fischer AS, Giancola PR. Confirmatory factor analysis of the Behavior Rating Inventory of Executive Function-Adult version in healthy adults and application to attention-deficit/hyperactivity disorder. Arch Clin Neuropsychol. 2013;28(5):425–34.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Faraone SV, Gomeni R, Hull JT, Busse GD, Melyan Z, Rubin J, et al. Executive function outcome of SPN-812 (viloxazine extended-release) treatment in children and adolescents with attention-deficit/hyperactivity disorder: a post hoc analysis of four randomized clinical trials. Pediatr Drugs. 2021. (epub ahead of print).
Barkley RA, Murphy KR. The nature of executive function (EF) deficits in daily life activities in adults with ADHD and their relationship to performance on EF tests. J Psychopathol Behav Assess. 2011;33(2):137–58.
Brown TE. ADD/ADHD and impaired executive function in clinical practice. Curr Attent Disord Rep. 2009;1(1):37–41.
Biederman J, Petty C, Fried R, Fontanella J, Doyle AE, Seidman LJ, et al. Impact of psychometrically defined deficits of executive functioning in adults with attention deficit hyperactivity disorder. Am J Psychiatry. 2006;163(10):1730–8.
Halleland HB, Sørensen L, Posserud M-B, Haavik J, Lundervold AJ. Occupational status is compromised in adults with ADHD and psychometrically defined executive function deficits. J Attent Disord. 2019;23(1):76–86.
Dvorsky MR, Langberg JM. Predicting impairment in college students with ADHD: the role of executive functions. J Attent Disord. 2019;23(13):1624–36.
Roth RM, Isquith PK, Gioia GA. Assessment of executive functioning using the Behavior Rating Inventory of Executive Function (BRIEF). In: Goldstein S and Naglieri J (eds). Handbook of executive functioning. p. 301–31. New York: Springer; 2014.
Magnus RV. A placebo controlled trial of viloxazine with and without tranquillizers in depressive illness. J Int Med Res. 1975;3(3):207–13.
Bayliss PFC, Harcup JW, Mayer M, Million R, Murphy JE, Plant B, et al. An open study of two dose levels of ‘Vivalan’ (viloxazine hydrochloride ICI 58 834) in depression in general practice. J Int Med Res. 1974;2:253–9.
Bayliss PFC, Dewsbury AR, Donald JF, Harcup JW, Mayer M, Million R, et al. A double-blind controlled trial of “Vivalan” (viloxazine hydrochloride) and imipramine hydrochloride in the treatment of depression in general practice. J Int Med Res. 1974;2:260–4.
Kabes J, Dostal T, Nahunek K, Svestka J, Molcan J, Caplová T, et al. Multicentre study with viloxazine (Vivalan®) in depressed patients. Int Pharmacopsychiatr. 1980;15:228–39.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was entirely supported by Supernus Pharmaceuticals, Inc. Open access publication was funded by Supernus Pharmaceuticals, Inc.
Conflicts of interest/Competing interests
AN, JTH, TL, NF, and JR, are employees of Supernus Pharmaceuticals, Inc. SAC, OO, ARK, and SS were employees of Supernus Pharmaceuticals, Inc. at the time of this work. AJC has received research support from Aevi Genomics, Akili Interactive, Arbor Pharmaceuticals, Ironshore Pharmaceuticals, Janssen, KemPharm, Lundbeck, Neos Therapeutics (now Aytu BioPharma), Neurovance, Noven, Otsuka, Purdue Canada, Rhodes Pharmaceuticals, Shire, Sunovion, Supernus Pharmaceuticals, Inc., Takeda, and Tris Pharma. He has received fees for consulting, advisory boards, and promotional speaking from Adlon Therapeutics, Aevi Genomics, Akili Interactive, Arbor Pharmaceuticals, Atentiv, Cingulate Therapeutics, Corium, Ironshore Pharmaceuticals, Janssen, Lundbeck, MedAvante-ProPhase, Neos Therapeutics (now Aytu BioPharma), NLS Pharmaceutics, Noven, Otsuka, Shire, Sunovion, Supernus Pharmaceuticals, Inc., Takeda, and Tris Pharma. He is an employee and board member of the Neuroscience Education Institute. AC has received research support from, served as a consultant or speaker for, or served on an advisory board for Allergan, Takeda (Shire), Emalex, Pearson, Akili, Arbor, Cingulate Therapeutics, Ironshore, Lumos, Aevi Genomic Medicine, Neos Therapeutics, Neurovance, Noven, Otsuka, Pfizer, Purdue, Adlon, Rhodes, Sunovion, Tris, KemPharm, Supernus Pharmaceuticals, Inc., US Food and Drug Administration, NLS Pharma, and Jazz.
Ethics approval
The study was approved by the WIRB-Copernicus Group Institutional Review Board and conducted in accordance with the Helsinki Declaration and the International Council for Harmonisation Good Clinical Practice Guidelines.
Consent to participate
Each subject provided written informed consent prior to screening.
Consent for publication
Not applicable.
Availability of data and material
The data are not available in a repository, but requests can be directed to anasser@supernus.com.
Code availability
Not applicable.
Author contributions
Conceptualization and design: AN, JTH, TL, OO, SAC, SS. Methodology and data collection: AN, JTH, TL, OO, NF, AJC, SS, AC. Analysis and interpretation: AN, JTH, TL, OO, SAC, SS, JR. Writing, original draft preparation: AN, JTH, SAC, ARK. Writing, review and editing: AN, JTH, SAC, ARK, AJC, JR, AC. All authors have read and approve the final submitted manuscript and agree to be accountable for this work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nasser, A., Hull, J.T., Chaturvedi, S.A. et al. A Phase III, Randomized, Double-Blind, Placebo-Controlled Trial Assessing the Efficacy and Safety of Viloxazine Extended-Release Capsules in Adults with Attention-Deficit/Hyperactivity Disorder. CNS Drugs 36, 897–915 (2022). https://doi.org/10.1007/s40263-022-00938-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-022-00938-w