Abstract
Introduction
Newer antiepileptic drugs (AEDs) are increasingly prescribed; however, relatively limited data are available regarding their use in status epilepticus (SE) and the impact on outcome.
Objectives
The aim of this study was to explore the evolution in prescription patterns of newer and traditional AEDs in this clinical setting, and their association with prognosis.
Methods
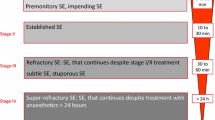
We analyzed our prospective adult SE registry over a 10-year period (2007–2016) and assessed the yearly use of newer and traditional AEDs and their association with mortality, return to baseline conditions at discharge, and SE refractoriness, defined as treatment resistance to two AEDs, including benzodiazepines.
Results
In 884 SE episodes, corresponding to 719 patients, the prescription of at least one newer AED increased from 0.38 per SE episode in 2007 to 1.24 per SE episode in 2016 (mostly due to the introduction of levetiracetam and lacosamide). Traditional AEDs (excluding benzodiazepines) decreased over time from 0.74 in 2007 to 0.41 in 2016, correlating with the decreasing use of phenytoin. The prescription of newer AEDs was independently associated with a lower chance of return to baseline conditions at discharge (odds ratio [OR] 0.58, 95% confidence interval [CI] 0.40–0.84) and a higher rate of SE refractoriness (OR 19.84, 95% CI 12.76–30.84), but not with changes in mortality (OR 1.08, 95% CI 0.58–2.00).
Conclusion
We observed a growing trend in the prescription of newer AEDs in SE over the last decade; however, our findings might suggest an associated increased risk of SE refractoriness and new disability at hospital discharge. Pending prospective, comparative studies, this may justify some caution in the routine use of newer AEDs in SE.




Similar content being viewed by others
References
Claassen J, Riviello JJ, Silbergleit R. Emergency neurological life support: status epilepticus. Neurocrit Care. 2015;23(Suppl 2):S136–42.
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23.
Meierkord H, Boon P, Engelsen B, Göcke K, Shorvon S, Tinuper P, et al. EFNS guideline on the management of status epilepticus in adults. Eur J Neurol. 2010;17(3):348–55.
Glauser T, Shinnar S, Gloss D, Alldredge B, Arya R, Bainbridge J, et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the Guideline Committee of the American Epilepsy Society. Epilepsy Curr. 2016;16(1):48–61.
Glauser T, Ben-Menachem E, Bourgeois B, Cnaan A, Guerreiro C, Kälviäinen R, et al. Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2013;54(3):551–63.
de Groot MCH, Schuerch M, de Vries F, Hesse U, Oliva B, Gil M, et al. Antiepileptic drug use in seven electronic health record databases in Europe: a methodologic comparison. Epilepsia. 2014;55(5):666–73.
Landmark CJ, Fossmark H, Larsson PG, Rytter E, Johannessen SI. Prescription patterns of antiepileptic drugs in patients with epilepsy in a nation-wide population. Epilepsy Res. 2011;95(1–2):51–9.
Berman E, Marom E, Ekstein D, Blatt I, Eyal S. Utilization of antiepileptic drugs in Israel. Epilepsy Behav. 2016;61:82–5.
Italiano D, Capuano A, Alibrandi A, Ferrara R, Cannata A, Trifirò G, et al. Indications of newer and older anti-epileptic drug use: findings from a southern Italian general practice setting from 2005–2011. Br J Clin Pharmacol. 2015;79(6):1010–9.
Savica R, Beghi E, Mazzaglia G, Innocenti F, Brignoli O, Cricelli C, et al. Prescribing patterns of antiepileptic drugs in Italy: a nationwide population-based study in the years 2000–2005. Eur J Neurol. 2007;14(12):1317–21.
Novy J, Rossetti AO. Oral pregabalin as an add-on treatment for status epilepticus. Epilepsia. 2010;51(10):2207–10.
Madžar D, Kuramatsu JB, Gerner ST, Huttner HB. Assessing the value of topiramate in refractory status epilepticus. Seizure. 2016;38:7–10.
Santamarina E, Toledo M, Sueiras M, Raspall M, Ailouti N, Lainez E, et al. Usefulness of intravenous lacosamide in status epilepticus. J Neurol. 2013;260(12):3122–8.
Kellinghaus C, Berning S, Immisch I, Larch J, Rosenow F, Rossetti AO, et al. Intravenous lacosamide for treatment of status epilepticus. Acta Neurol Scand. 2011;123(2):137–41.
Knake S, Gruener J, Hattemer K, Klein KM, Bauer S, Oertel WH, et al. Intravenous levetiracetam in the treatment of benzodiazepine refractory status epilepticus. J Neurol Neurosurg Psychiatry. 2008;79(5):588–9.
Rüegg S, Naegelin Y, Hardmeier M, Winkler DT, Marsch S, Fuhr P. Intravenous levetiracetam: treatment experience with the first 50 critically ill patients. Epilepsy Behav. 2008;12(3):477–80.
Chakravarthi S, Goyal MK, Modi M, Bhalla A, Singh P. Levetiracetam versus phenytoin in management of status epilepticus. J Clin Neurosci. 2015;22(6):959–63.
Alvarez V, Januel J-M, Burnand B, Rossetti AO. Second-line status epilepticus treatment: comparison of phenytoin, valproate, and levetiracetam. Epilepsia. 2011;52(7):1292–6.
Brigo F, Bragazzi N, Nardone R, Trinka E. Direct and indirect comparison meta-analysis of levetiracetam versus phenytoin or valproate for convulsive status epilepticus. Epilepsy Behav. 2016;64 (Part A):110–5.
Jaques L, Rossetti AO. Newer antiepileptic drugs in the treatment of status epilepticus: impact on prognosis. Epilepsy Behav. 2012;24(1):70–3.
Novy J, Logroscino G, Rossetti AO. Refractory status epilepticus: a prospective observational study. Epilepsia. 2010;51(2):251–6.
Marchi NA, Novy J, Faouzi M, Stähli C, Burnand B, Rossetti AO. Status epilepticus: impact of therapeutic coma on outcome. Crit Care Med. 2015;43(5):1003–9.
Lowenstein DH, Bleck T, Macdonald RL. It’s time to revise the definition of status epilepticus. Epilepsia. 1999;40(1):120–2.
Rossetti AO, Hurwitz S, Logroscino G, Bromfield EB. Prognosis of status epilepticus: role of aetiology, age, and consciousness impairment at presentation. J Neurol Neurosurg Psychiatry. 2006;77(5):611–5.
Rossetti AO, Logroscino G, Milligan TA, Michaelides C, Ruffieux C, Bromfield EB. Status Epilepticus Severity Score (STESS): a tool to orient early treatment strategy. J Neurol. 2008;255(10):1561–6.
Redecker J, Wittstock M, Benecke R, Rösche J. Comparison of the effectiveness of four antiepileptic drugs in the treatment of status epilepticus according to four different efficacy criteria. Epilepsy Behav. 2015;49:351–3.
Marson AG, Al-Kharusi AM, Alwaidh M, Appleton R, Baker GA, Chadwick DW, et al. The SANAD study of effectiveness of carbamazepine, gabapentin, lamotrigine, oxcarbazepine, or topiramate for treatment of partial epilepsy: an unblinded randomised controlled trial. Lancet. 2007;369(9566):1000–15.
Marson AG, Al-Kharusi AM, Alwaidh M, Appleton R, Baker GA, Chadwick DW, et al. The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalised and unclassifiable epilepsy: an unblinded randomised controlled trial. Lancet. 2007;369(9566):1016–26.
Vazquez B. Monotherapy in epilepsy: role of the newer antiepileptic drugs. Arch Neurol. 2004;61(9):1361–5.
Kwan P, Brodie MJ. Clinical trials of antiepileptic medications in newly diagnosed patients with epilepsy. Neurology. 2003;60(11 Suppl 4):S2–12.
Ney JP, van der Goes DN, Nuwer MR, Nelson L, Eccher MA. Continuous and routine EEG in intensive care: utilization and outcomes, United States 2005–2009. Neurology. 2013;81(23):2002–8.
Betjemann JP, Josephson SA, Lowenstein DH, Burke JF. Trends in status epilepticus-related hospitalizations and mortality: redefined in US practice over time. JAMA Neurol. 2015;72(6):650–5.
Navarro V, Dagron C, Elie C, Lamhaut L, Demeret S, Urien S, et al. Prehospital treatment with levetiracetam plus clonazepam or placebo plus clonazepam in status epilepticus (SAMUKeppra): a randomised, double-blind, phase 3 trial. Lancet Neurol. 2016;15(1):47–55.
Alvarez V, Lee JW, Drislane FW, Westover MB, Novy J, Dworetzky BA, et al. Practice variability and efficacy of clonazepam, lorazepam, and midazolam in status epilepticus: a multicenter comparison. Epilepsia. 2015;56(8):1275–85.
Tong X, Patsalos PN. A microdialysis study of the novel antiepileptic drug levetiracetam: extracellular pharmacokinetics and effect on taurine in rat brain. Br J Pharmacol. 2001;133(6):867–74.
Nicolas J-M, Hannestad J, Holden D, Kervyn S, Nabulsi N, Tytgat D, et al. Brivaracetam, a selective high-affinity synaptic vesicle protein 2A (SV2A) ligand with preclinical evidence of high brain permeability and fast onset of action. Epilepsia. 2016;57(2):201–9.
Doheny HC, Ratnaraj N, Whittington MA, Jefferys JG, Patsalos PN. Blood and cerebrospinal fluid pharmacokinetics of the novel anticonvulsant levetiracetam (ucb L059) in the rat. Epilepsy Res. 1999;34(2–3):161–8.
Wang X, Patsalos PN. A comparison of central brain (cerebrospinal and extracellular fluids) and peripheral blood kinetics of phenytoin after intravenous phenytoin and fosphenytoin. Seizure. 2003;12(6):330–6.
Rossetti AO, Alvarez V, Januel J-M, Burnand B. Treatment deviating from guidelines does not influence status epilepticus prognosis. J Neurol. 2013;260(2):421–8.
Bleck T, Cock H, Chamberlain J, Cloyd J, Connor J, Elm J, et al. The Established Status Epilepticus Trial 2013. Epilepsia. 2013;54(Suppl 6):89–92.
Acknowledgements
The authors thank Christine Stähli, RN, and the EEG technologists and fellows for help in data acquisition.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
Isabelle Beuchat, Jan Novy and Andrea Rossetti declare no conflicts of interest with regard to the findings reported in this study.
Rights and permissions
About this article
Cite this article
Beuchat, I., Novy, J. & Rossetti, A.O. Newer Antiepileptic Drugs in Status Epilepticus: Prescription Trends and Outcomes in Comparison with Traditional Agents. CNS Drugs 31, 327–334 (2017). https://doi.org/10.1007/s40263-017-0424-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-017-0424-1