Abstract
Background
SAGE-217, a novel γ-aminobutyric acid A (GABAA) receptor positive allosteric modulator, was evaluated in phase I, double-blind, placebo-controlled, single ascending dose (SAD) and multiple ascending dose (MAD) studies to assess the safety and pharmacokinetics (PK) of SAGE-217 following administration as an oral solution.
Methods
In the SAD study, subjects were randomized 6:2 to a single dose of SAGE-217 or placebo. Doses ranged from 0.25 to 66 mg across nine cohorts. In the MAD study, subjects were randomized 9:3 and received SAGE-217 (15, 30, or 35 mg) or placebo once daily for 7 days. In both studies, PK, maximum tolerated dose (MTD; against predetermined criteria), safety, and tolerability were assessed.
Results
A total of 108 healthy volunteers enrolled in the studies—72 subjects in the SAD study and 36 subjects in the MAD study. SAGE-217 was orally bioavailable, with a terminal-phase half-life of 16–23 h and a tmax of approximately 1 h. The MTDs for the oral solution of SAGE-217 in the SAD and MAD studies were determined to be 55 and 30 mg daily, respectively. In both studies, SAGE-217 was generally well tolerated, and no serious adverse events (SAEs) were reported. Most AEs were mild, dose-dependent, transient, occurred around the tmax, and related to drug pharmacology.
Conclusions
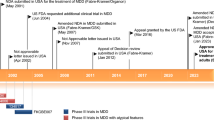
SAGE-217 was generally well tolerated, and its PK profile was well characterized. Based on this profile, SAGE-217 has been advanced into multiple phase II clinical programs and pivotal studies of major depressive disorder and postpartum depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
SAGE-217 is a neuroactive steroid (NAS) and a positive allosteric modulator (PAM) of γ-aminobutyric acid A (GABAA) receptors [1]. Dysfunction in GABAergic neurotransmission has been associated with the pathophysiology of multiple diseases, including a variety of both mood and movement disorders [2,3,4,5,6,7]. As the primary inhibitory neurotransmitter in the nervous system, GABA, acting in part via the GABAA receptor, can exert an influence in many brain circuits that are crucial to behavioral states, such as anxiety, mood, seizures, sleep, vigilance, and memory [8,9,10,11,12]. Thus, drugs such as benzodiazepines, barbiturates, and anesthetics all target GABAA receptors.
Some endogenous NASs, such as the progesterone metabolite allopregnanolone, can potently modulate neuronal excitability, primarily through positive allosteric modulation of synaptic and extrasynaptic GABAA receptors [13, 14]. Systemic administration of allopregnanolone has been demonstrated to produce anxiolysis and mood improvement in preclinical models [15,16,17].
Brexanolone injection, a proprietary formulation of allopregnanolone for intravenous infusion, has demonstrated efficacy in human studies of postpartum depression [18,19,20]. SAGE-217 is a synthetic NAS GABAA receptor PAM that shares a similar molecular pharmacological profile as brexanolone injection [1]. However, initial in vitro and in vivo drug metabolism and pharmacokinetic (DMPK) studies of SAGE-217 in animals have shown that it is orally bioavailable, with low to moderate clearance (CL), which supports further development of this compound as a drug candidate [1]. The potential to deliver SAGE-217 via an oral formulation represents an opportunity to further understand the potential therapeutic role for NASs in a broad range of mood and movement disorders.
The aim of these first-in-human studies was to examine SAGE-217 in single ascending dose (SAD) and multiple ascending dose (MAD) protocols in order to investigate its safety, tolerability, and pharmacokinetic (PK) profiles. These phase I results have helped build a foundation for pivotal studies of SAGE-217 in mood disorders.
2 Methods
2.1 Study Population
The SAD and MAD studies were approved by the Institutional Review Boards at each study site and were performed in accordance with ethical standards as described in the 1964 Declaration of Helsinki and its later amendments. Written informed consent was provided at screening and was required for enrollment in each study. Participants were of both sexes, ranging in age from 22 to 55 years. No formal sample size calculations were undertaken for these PK, safety, and tolerability studies. The number of subjects in each cohort and at each dose level was thought to be sufficient to assess PK, safety, and tolerability for determining escalating doses of SAGE-217 according to predetermined criteria.
2.2 Single Ascending Dose (SAD) and Multiple Ascending Dose (MAD) Study Designs
The SAD trial was a multicenter, double-blind, placebo-controlled trial conducted at two sites in the US from 29 September 2015 (first subject enrolled) to 7 June 2016 (last subject, last visit), while the MAD trial was a single center, double-blind, placebo-controlled study conducted in the US from 6 January 2016 (first subject enrolled) to 28 April 2016 (last subject, last visit). The staggered start of the trials allowed the SAD trial to inform MAD dosing, although the trials ran in parallel after MAD trial initiation. All authors vouch for the accuracy and completeness of the data, data analyses, and the fidelity of this publication to the study protocol.
The SAD and MAD studies were conducted in a double-blind manner. The active and placebo treatments were identical in appearance within each study. In order to facilitate dose selection for future cohorts, Sage Therapeutics, Inc. may have unblinded individual or group data from a cohort once all subjects in that cohort completed their follow-up visits and any AEs were resolved.
Subjects were randomly assigned to either placebo or active treatment with SAGE-217 according to a randomization schedule prepared by an independent statistician. In each of the SAD cohorts, subjects were randomly assigned to receive either SAGE-217 (six subjects) or placebo (two subjects) in a blinded manner, and in each of the MAD cohorts, subjects were randomly assigned to receive either SAGE-217 (nine subjects) or placebo (three subjects) in a blinded manner.
2.3 SAD and MAD Procedures
SAGE-217 doses were prepared in an aqueous solution containing hydroxypropyl β-cyclodextrin and administered as single oral doses in each study. Sentinel dosing was employed for the first SAD cohort, with one subject randomized to receive SAGE-217 and the other subject randomized to receive placebo on the first day. The other six subjects in the first cohort were dosed approximately 24 h later. Escalation to the next dose cohort was undertaken only after safety and PK data were reviewed by the Safety Review Committee (SRC) and agreement reached that it was safe to increase the dose. Each SAD cohort was dosed at approximately weekly intervals to allow adequate time for collection and review of safety and PK data. Six subjects in each of the nine SAD cohorts received a single SAGE-217 dose of 0.25, 0.75, 2, 5.5, 11, 22, 44, 55, or 66 mg. Doses were selected to interrogate a predefined exposure range bounded by a maximum recommended starting dose determined from non-clinical studies and doses triggering predefined stopping criterion, informed by emerging pharmacodynamic and tolerability data. The utilization of a solution formulation allowed flexibility in dose selection. The starting dose of 0.25 mg was selected based on established guidelines, and provided a > 50-fold margin below the no adverse effect dose observed in non-clinical toxicology studies [21].
The total daily dose for each MAD cohort was based on information obtained from the SAD study. Nine subjects each received single SAGE-217 doses of 15 mg (Cohort 1), 35 mg (Cohort 2), and 30 mg (Cohort 3) in the morning for 7 days; nine subjects received placebo for 7 days. Subjects participating in Cohort 3 were dosed in the morning for 7 days (Part 1), and after a suitable washout period of at least 7 days, they returned for a second period of 7 days of dosing in the evening (Cohort 3, Part 2) to determine if there was a differential tolerability profile compared with morning dosing. For both the SAD and MAD studies, dosing was escalated until the maximum tolerated dose (MTD) was achieved based on prespecified stopping criteria (see the outcomes below; MTD guidelines are shown in the electronic supplementary material).
2.4 Bioanalysis
Bioanalysis of plasma samples for the determination of SAGE-217 levels was conducted utilizing a validated liquid chromatography-tandem mass spectrometry method at Agilux Laboratories (Worcester, MA, USA). Plasma sample (50 µL) was spiked with stable isotopic-labeled internal standard (d3-SAGE-217), and the sample was extracted using protein precipitation. The analyte was separated on a C18 column using a gradient, and ionized using electrospray in a positive ion mode. Multiple reaction monitoring (MRM) was employed to monitor SAGE-217. The peak area ratio of SAGE-217 to internal standard was used to determine the concentration. The calibration curve was validated using linear regression with 1/x2 weighting. The concentrations of the quality controls and PK samples were interpolated from the calibration standard curve. The method was validated with a dynamic range of 1.00–1000 ng/mL. The intra-assay accuracy and precision ranged from − 5.7 to 7.0 (% bias) and from 2.3 to 15.9 (percentage coefficient of variation [%CV]). The interassay accuracy and precision ranged from − 4.8 to 3.0 (% bias) and from 4.1 to 14.3 (%CV). Stability was established for four freeze/thaw cycles when stored at − 20 or − 80 °C, and for 2 h as whole blood at room temperature. SAGE-217 long-term storage stability in frozen plasma was established for 367 days at − 20 and − 80 °C.
2.5 SAD and MAD Outcomes
Determination of the MTD was an endpoint of both the SAD and MAD studies. The MTD in both trials was determined by prespecified stopping criteria (see the electronic supplementary material for details). Briefly, dosing was escalated in both studies until an ascending dose triggered one or more of the defined stopping criteria. At this point, a lower dose was tested, and if this dose did not trigger any of the defined stopping criteria, it was considered the MTD. Overall safety and tolerability of SAGE-217 were assessed by the frequency and severity of adverse events (AEs), the Stanford Sleepiness Scale (SSS) [22], the Modified Observer’s Assessment of Alertness/Sedation Scale (MOAA/S) [23], vital signs, changes in clinical laboratory measures, physical examinations, electrocardiograms (ECGs), and suicide ideation using the Columbia-Suicide Severity Rating Scale (C-SSRS) [24].
Plasma samples were taken from all cohorts in both studies for PK analyses. Plasma samples for PK analysis were collected according to the sampling collection times specified. For both the SAD and MAD studies, blood samples were taken for analysis at 0, 0.25, 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 7, 8, 10, 12, 16, 24, 28, 32, 36, and 48 h. Time zero samples were collected just prior to study drug administration. An additional PK sample may have been collected at any time if clinically indicated and at the discretion of the Investigator (e.g. for unusual or severe AEs).
Derived PK parameters included area under the plasma concentration–time curve from the time of dosing extrapolated to infinity (AUC∞), the terminal-phase half-life (t½), Cmax, time to reach maximum concentration (tmax), and apparent clearance (CL/F). PK parameters were calculated from the individual plasma concentrations, and summarized using appropriate descriptive statistics.
2.6 Statistical Analysis
The safety population was defined as all subjects who were administered study drug, while the PK population was defined as all subjects who were administered SAGE-217 and had at least one quantifiable plasma concentration. For each measured parameter, the change from baseline value was calculated at each time point and was summarized. Out-of-range safety endpoints were categorized as low or high, where applicable. Plasma concentrations that were below the limit of quantification were substituted with zero for the calculation of descriptive statistics by time point. SAGE-217 concentrations in plasma were measured utilizing a validated method with liquid chromatography and tandem mass spectrometry (see the Bioanalysis, above).
Descriptive summaries were presented by treatment and time point, where applicable. For categorical endpoints, summaries included counts and percentages, and for continuous endpoints, summaries included number of observations, mean, median, standard deviation, coefficient of variation, minimum, and maximum. Dose proportionality was analyzed using regression analysis [25].
3 Results
3.1 Disposition and Demographics
In the SAD study, a total of 72 subjects with a mean age of 35.9 years were randomized (Table 1), 54 subjects to SAGE-217 and 18 subjects to placebo. Seventy-one subjects completed the study; however, one subject in the 44 mg cohort was lost to follow-up.
Thirty-six subjects were enrolled and treated in the MAD study (12 subjects in each of the MAD cohorts), with a mean age of 38.3 years (Table 1). All subjects who received SAGE-217 15 mg, SAGE-217 35 mg, and placebo completed the study. Of the nine subjects who received SAGE-217 30 mg in the morning for 7 days, seven (77.8%) completed a second period of 7 days dosing in the evening after a washout period. Two of the nine subjects (22.2%) discontinued from the study, one due to pre-existing vagotonia discovered after the first dose of study drug, and one due to the investigator’s discretion regarding a low hemoglobin on period 1, day 14. The total SAGE-217 group included 27 subjects, while the placebo group included 9 subjects. Additional demographic information is provided in Table 1.
3.2 Outcomes
Following a single dose of SAGE-217 oral solution, plasma concentrations rapidly increased and reached maximum concentrations approximately 1 h postdose. Concentrations then declined in a biphasic manner and exhibited a terminal-phase half-life ranging from 16 to 23 h (Fig. 1a, b; Tables 2a, b). Terminal-phase half-life estimates were determined from the higher doses of the SAD cohort (≥ 11 mg), where there were sufficient time points above the assay limit of quantitation (1 ng/mL). For both single and repeated dose administration, tmax and terminal-phase half-life showed dose independence. The dose proportionality of SAGE-217 was examined using data from both the SAD and MAD studies, encompassing a 264-fold range of doses. SAGE-217 exhibited dose proportionality as indicated by the analysis of Cmax, area under the concentration–time curve from time zero to the last measurable concentration (AUClast), or AUC∞, with point estimates for the slope near 1 in the SAD study and 95% confidence intervals containing 1 in the MAD study over the dose range studied (Fig. 2, Table 3). Accumulation of SAGE-217 after 7 days of dosing was less than twofold and was consistent with steady-state predictions based on terminal-phase half-life (Table 2a, b). Negligible SAGE-217 was detected in urine, indicating that renal excretion of unchanged drug does not contribute to CL (data not shown).
a SAGE-217 plasma concentration over time (SAD). Mean plasma concentration of SAGE-217 by dose over time (n = 6 for each dose). b SAGE-217 plasma concentration over time (MAD). Mean plasma concentration of SAGE-217 by dose over time; day 7 dosing (n = 9 for each dose). SAD single ascending dose, MAD multiple ascending dose
Dose proportionality and linearity in the SAD and MAD studies. Combined data from the SAD and MAD studies was used to assess dose linearity. a AUC∞ over SAGE-217 dose. bCmax over SAGE-217 dose. SAD single ascending dose, MAD multiple ascending dose, AUC∞ area under the concentration–time curve from the time of dosing extrapolated to infinity, Cmax maximum concentration
The MTD for both the SAD and MAD studies was determined by application of predefined stopping criteria (see the electronic supplementary material). These stopping criteria were assembled to assess AEs anticipated based on the primary pharmacology of SAGE-217 (i.e. sedation due to GABAA receptor PAM activity). The maximum dose in each study (66 mg for SAD; 35 mg for MAD) triggered the MOAA/S stopping criterion of a recorded and confirmed MOAA/S score of ≤ 2 during normal waking hours. Two subjects in the 66 mg SAD cohort recorded MOAA/S scores ≤ 2 within the first 2 h postdose, and two subjects in the 35 mg MAD cohort recorded MOAA/S scores ≤ 2 within the first hour postdose, resulting in cessation of dose escalation in the respective studies. MOAA/S scores for these subjects returned to normal by 7 h postdose. In each study, dosing was reduced to the MTD in the subsequent cohort, which did not trigger any stopping criteria. The SAD MTD was established at 55 mg, and the MAD MTD was 30 mg/day.
In both the SAD and MAD studies, there were no serious treatment-emergent AEs or AEs leading to withdrawal from the study (electronic supplementary Tables S1a, b). No subjects reported severe AEs in the MAD study, while four subjects reported severe AEs in the SAD study, all at the highest dose of 66 mg of SAGE-217 (change in mental status, n = 2; unresponsive to stimuli, n = 2; and somnolence, n = 1). Most AEs were reported to be mild. Sedation was the most common AE overall, occurring in 23 of 72 subjects (31.9%; including three placebo subjects) in the SAD study, and 25 of 43 (58.1%; including two placebo subjects and three SAGE-217 30 mg evening-dose subjects) in the MAD study. In both studies, sedation increased with increasing dose of SAGE-217, consistent with the pharmacology of GABAA receptor PAMs (electronic supplementary Tables S1a,b). There were no reported AEs of loss of consciousness in either the SAD or MAD study at any dose. Fewer AEs related to the primary pharmacology of the drug (such as sedation, somnolence, dizziness, and fatigue) were reported with evening dosing compared with daytime dosing.
As dose-dependent changes in sedation was a predicted effect based on both the proposed mechanism of action for SAGE-217 and preclinical animal studies, the SSS [22] and MOAA/S scale [23] were used in concert with AE reporting to investigate any relationship between SAGE-217 concentrations and reports of sedation or somnolence. The SSS is a self-reported measure of sleepiness, where a score of 1 is ‘subject feeling active, vital, alert, or wide awake’ and the highest score of 7 indicates ‘no longer fighting sleep, sleep onset soon; having dream-like thoughts’. The MOAA/S scale is a clinician-rated scale of sedation where 0 indicates ‘no response after a painful trapezius squeeze’ and 5 indicates ‘readily responds to name spoken in a normal tone’. The maximum mean SSS and minimum mean MOAA/S scores for each dosing period occurred at 1 h postdosing for all doses, with no apparent change in the temporal relationship between dosing and maximum score over 7 days of dosing. The mean values for the 30 mg morning MTD group are shown in Fig. 3. In this dosing condition, the highest recorded SSS score for any subject was 6, and all such values were recorded between 1 and 3 h after dosing. Similarly, the lowest MOAA/S score recorded in a subject in the 30 mg dose group was 4 at 2 h after dosing. In contrast, the 35 mg dosing condition triggered the MOAA/S stopping criterion (see above).
The 30 mg evening dosing condition also resulted in a maximum individual SSS score of 6 between 1 and 3 h after dosing, and the lowest MOAA/S score of 3 was recorded in one subject at 3 h after dosing in a single dosing period. At the next measured time point (12 h postdose, the morning following dosing), no subject reported an SSS score higher than 2 in any dosing period, and all subjects reported the maximum MOAA/S score (i.e. the least sedated) of 5 at the 12-h time point in every dosing period.
4 Discussion
Given the role of GABAA receptors in the pathophysiology of neurologic and neuropsychiatric disorders, GABAA receptor PAMs are being explored for the treatment of mood disorders [26]. Endogenous and synthetic NASs have been demonstrated to enhance GABAergic neurotransmission at multiple GABAA receptor subtypes, both by potentiating receptor current and by increasing receptor expression [1, 27,28,29]. SAGE-217 potentiates representative examples of both synaptic and extrasynaptic GABAA receptors, preclinically differentiating it from other, currently approved GABAA receptor PAMs, such as members of the benzodiazepine class [1]. A potential role for synaptic and extrasynaptic GABAA receptor PAMs in the treatment of mood disorders is also supported by recent clinical studies of brexanolone injection, an investigational formulation of allopregnanolone for intravenous infusion, in postpartum depression [18,19,20].
Although the PK profile of SAGE-217 has previously been examined in preclinical studies, the current studies were the first to evaluate SAGE-217 in human subjects. SAGE-217 oral solution was found to be orally bioavailable and exhibit low variability in human subjects. The PK profile is well characterized, and exposure was observed to increase in proportion to dose. Minimal accumulation was noted after 7 days of dosing, suggesting that loading doses would not be necessary and that patients would reach target concentrations relatively quickly after initiation of treatment. There was low intersubject variability in exposure parameters, with %CVs generally below 30%. The predictable, dose-dependent, and low-variability PK are an important feature of SAGE-217 in evaluating clinical PK/PD relationships.
The PK profile of SAGE-217, in particular oral bioavailability, substantially expands the opportunity to treat mood disorder patients with NAS-mediated modulation of the GABAA receptor system beyond those amenable to intravenous treatment. Moreover, further elucidation of the PK/PD profile may yield opportunities to enhance the therapeutic profile with use of modified-release formulations to optimize the PK profile of SAGE-217. Most notably, in this study of SAGE-217 oral solution, sedation AEs were associated with Cmax and tmax, and a modified-release formulation could offer the potential to reduce Cmax and/or increase tmax. Ongoing studies of SAGE-217 in mood disorders are using capsule-based formulations.
In both the SAD and MAD studies, the MOAA/S stopping criterion defined the MTD, a finding that was entirely consistent with the GABAA receptor PAM pharmacology of SAGE-217. Maximal SSS scores and minimal MOAA/S scores (as measures of sedation) occurred with proximity to tmax. SAGE-217 was generally well tolerated in these trials, and the four subjects with severe AEs reported in the SAD study received the highest dose, which was not tolerated. No severe AEs were reported at the MTD in either the SAD or MAD studies.
The most common AE associated with SAGE-217 administration across both studies was sedation, but no loss of consciousness was reported in either study. With the exception of a minority of subjects in the highest, non-tolerated dose cohorts, MOAA/S results indicate that these subjects were able to be roused in response to stimuli, and the lowest MOAA/S scores in the 30 mg morning cohort corresponded to 4, ‘lethargic response readily to name spoken in normal tone’. Peak sedation occurred in the 1–2 h following dosing and likely reflects the early higher concentrations of SAGE-217, suggesting that future formulation development could modulate PK to reduce sedation levels.
The sedation signal in the 30 mg evening cohort of the MAD study was reduced compared with the morning dosing conditions, likely due to the highest drug concentrations corresponding with normal sleeping hours. Three of seven subjects who received 30 mg SAGE-217 in the evening reported sedation, but no subjects in the evening dosing cohort showed a significant sedation signal in the morning following dosing.
Although the absolute doses used in these studies were not substantially different, the results from this clinical study demonstrated dose-related changes in exposure and tolerability. SAGE-217 demonstrated an AE profile consistent with its known effects on GABAA receptor pharmacology and predictable dose–exposure and dose–sedation relationships.
It is noteworthy that fewer sedation-related AEs were observed in the evening dosing 30 mg cohort versus the morning dosing 30 mg cohort. Based on these findings, evening dosing with SAGE-217 30 mg has been employed in phase II studies of the SAGE-217 development program.
These single and multiple ascending dose studies assessed the PK and tolerability profiles of orally administered SAGE-217. SAGE-217 was found to be orally bioavailable, with an observed terminal-phase half-life of 16–23 h. The MTDs for the SAD and MAD studies were 55 and 30 mg, respectively. SAGE-217 was not associated with any SAEs across both studies. The pharmacological effects observed were anticipated and consistent with the GABAA receptor PAM mechanism of action and the pharmacologic profile of SAGE-217, with sedation observed at peak drug exposure [30]. Overall, the tolerability profile of SAGE-217 supported advancement of SAGE-217 into further development in mood disorders.
5 Conclusions
Data from the SAD and MAD studies of SAGE-217 are an enabling dataset to support and inform the ongoing SAGE-217 developmental program in phase II and III trials. Based on the PK profile established in these studies, a capsule formulation of SAGE-217 was advanced into multiple phase II trials, and is currently under development in disorders where enhancement of GABAA receptor function may provide therapeutic benefits, including major depressive disorder and postpartum depression.
References
Martinez Botella G, Salituro FG, Harrison BL, et al. Neuroactive steroids. 2. 3α-hydroxy-3β-methyl-21-(4-cyano-1H-pyrazol-1′-yl)-19-nor-5β-pregnan-20-one (SAGE-217): a clinical next generation neuroactive steroid positive allosteric modulator of the (γ-aminobutyric acid)A receptor. J Med Chem. 2017;60(18):7810–9.
Boecker H, Weindl A, Brooks DJ, et al. GABAergic dysfunction in essential tremor: an 11C-flumazenil PET study. J Nucl Med. 2010;51(7):1030–5.
Deligiannidis KM, Sikoglu EM, Shaffer SA, et al. GABAergic neuroactive steroids and resting-state functional connectivity in postpartum depression: a preliminary study. J Psychiatr Res. 2013;47(6):816–28.
Gironell A. The GABA hypothesis in essential tremor: lights and shadows. Tremor Other Hyperkinet Mov (N Y). 2014;4:254.
Lener MS, Niciu MJ, Ballard ED, et al. Glutamate and gamma-aminobutyric acid systems in the pathophysiology of major depression and antidepressant response to ketamine. Biol Psychiatry. 2017;81(10):886–97.
Maguire J, Mody I. GABA(A)R plasticity during pregnancy: relevance to postpartum depression. Neuron. 2008;59(2):207–13.
Luscher B, Fuchs T. GABAergic control of depression-related brain states. Adv Pharmacol. 2015;73:97–144.
Kent JM, Mathew SJ, Gorman JM. Molecular targets in the treatment of anxiety. Biol Psychiatry. 2002;52(10):1008–30.
Mignot E, Taheri S, Nishino S. Sleeping with the hypothalamus: emerging therapeutic targets for sleep disorders. Nat Neurosci. 2002;5(Suppl):1071–5.
Rye DB, Bliwise DL, Parker K, et al. Modulation of vigilance in the primary hypersomnias by endogenous enhancement of GABAA receptors. Sci Transl Med. 2012;4(161):161ra151.
Szodorai E, Bampali K, Romanov RA, et al. Diversity matters: combinatorial information coding by GABAA receptor subunits during spatial learning and its allosteric modulation. Cell Signal. 2018;50:142–59.
Treiman DM. GABAergic mechanisms in epilepsy. Epilepsia. 2001;42(Suppl 3):8–12.
Belelli D, Harrison NL, Maguire J, Macdonald RL, Walker MC, Cope DW. Extrasynaptic GABAA receptors: form, pharmacology, and function. J Neurosci. 2009;29(41):12757–63.
Lambert JJ, Belelli D, Harney SC, Peters JA, Frenguelli BG. Modulation of native and recombinant GABA(A) receptors by endogenous and synthetic neuroactive steroids. Brain Res Brain Res Rev. 2001;37(1–3):68–80.
Frye CA, Walf AA. Hippocampal 3alpha,5alpha-THP may alter depressive behavior of pregnant and lactating rats. Pharmacol Biochem Behav. 2004;78(3):531–40.
Schiller CE, Meltzer-Brody S, Rubinow DR. The role of reproductive hormones in postpartum depression. CNS Spectr. 2015;20(1):48–59.
Schule C, Nothdurfter C, Rupprecht R. The role of allopregnanolone in depression and anxiety. Prog Neurobiol. 2014;113:79–87.
Meltzer-Brody S, Colquhoun H, Riesenberg R, et al. Brexanolone injection in post-partum depression: two multicentre, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet. 2018;392(10152):1058–70.
Kanes S, Colquhoun H, Gunduz-Bruce H, et al. Brexanolone (SAGE-547 injection) in post-partum depression: a randomised controlled trial. Lancet. 2017;390(10093):480–9.
Kanes SJ, Colquhoun H, Doherty J, et al. Open-label, proof-of-concept study of brexanolone in the treatment of severe postpartum depression. Hum Psychopharmacol. 2017;32(2):e2576.
US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research. Guidance for Industry: Estimating the Maximum Safe Starting Dose in Initial Clinical Trials for Therapeutics in Adult Healthy Volunteers. US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research; 2005.
Hoddes E, Zarcone V, Smythe H, Phillips R, Dement WC. Quantification of sleepiness: a new approach. Psychophysiology. 1973;10(4):431–6.
Chernik DA, Gillings D, Laine H, et al. Validity and reliability of the Observer’s Assessment of Alertness/Sedation Scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990;10(4):244–51.
Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–77.
Smith BP, Vandenhende FR, DeSante KA, et al. Confidence interval criteria for assessment of dose proportionality. Pharm Res. 2000;17(10):1278–83.
Luscher B, Shen Q, Sahir N. The GABAergic deficit hypothesis of major depressive disorder. Mol Psychiatry. 2011;16(4):383–406.
Abramian AM, Comenencia-Ortiz E, Modgil A, et al. Neurosteroids promote phosphorylation and membrane insertion of extrasynaptic GABAA receptors. Proc Natl Acad Sci USA. 2014;111(19):7132–7.
Hammond RS, Althaus AL, Ackley MA, et al. Anticonvulsant profile of the neuroactive steroid, SGE-516, in animal models. Epilepsy Res. 2017;134:16–25.
Modgil A, Parakala ML, Ackley MA, Doherty JJ, Moss SJ, Davies PA. Endogenous and synthetic neuroactive steroids evoke sustained increases in the efficacy of GABAergic inhibition via a protein kinase C-dependent mechanism. Neuropharmacology. 2017;113(Pt A):314–22.
Antkowiak B, Rudolph U. New insights in the systemic and molecular underpinnings of general anesthetic actions mediated by gamma-aminobutyric acid A receptors. Curr Opin Anaesthesiol. 2016;29(4):447–53.
Acknowledgements
Sage Therapeutics, Inc., Cambridge MA, USA, funded all aspects of the trial. The authors thank Jeffrey R. Skaar and Anna K. Talaga at Boston Strategic Partners, Inc. (supported by Sage Therapeutics, Inc.) and Claire Sauvageot and Paul Miller at Sage Therapeutics, Inc. for editorial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Ethan Hoffmann, Amy Bullock, Abdul J. Sankoh, James Doherty, Stephen J. Kanes, and Helen Colquhoun are employees of Sage Therapeutics, Inc., with stock/stock options. George G. Nomikos was formerly an employee of Sage Therapeutics, Inc., with stock/stock options during the conduct of this study. He is currently in Clinical Development with Biogen, Inc. Inder Kaul is an employee of Kaul Consulting, LLC, which was contracted by Sage Therapeutics, Inc. for this study. Shane Raines is an employee of 2b Analytics, LLC, which was contracted by Sage Therapeutics, Inc. for this study. Jeff Wald is an employee of qPharmetra, LLC, which was contracted by Sage Therapeutics, Inc. for this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hoffmann, E., Nomikos, G.G., Kaul, I. et al. SAGE-217, A Novel GABAA Receptor Positive Allosteric Modulator: Clinical Pharmacology and Tolerability in Randomized Phase I Dose-Finding Studies. Clin Pharmacokinet 59, 111–120 (2020). https://doi.org/10.1007/s40262-019-00801-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-019-00801-0