Abstract
Introduction
Venetoclax is a selective B cell lymphoma-2 inhibitor. It is approved for treatment of chronic lymphocytic leukemia and is being investigated for other hematological malignancies. Venetoclax is predominantly eliminated by the liver; therefore, there is a need to investigate the effect of hepatic insufficiency on venetoclax pharmacokinetics.
Methods
A phase I study was carried out in 24 women with normal hepatic function or mild, moderate, or severe hepatic impairment (based on Child–Pugh scores), who received a single 50 mg dose of venetoclax with a low-fat meal. Blood samples were collected up to 120 h after venetoclax administration. Pharmacokinetic parameters were estimated using non-compartmental methods.
Results
Venetoclax maximum observed plasma concentration (Cmax) and area under the plasma concentration–time curve (AUC) in subjects with mild or moderate hepatic impairment were similar to subjects with normal hepatic function. Mean venetoclax AUC in subjects with severe hepatic impairment was 2.3- to 2.7-fold higher than in subjects with normal hepatic function. The half-life of venetoclax in subjects with severe hepatic impairment was approximately two-fold longer than in subjects with normal hepatic function and subjects with mild or moderate hepatic impairment. Unbound fractions of venetoclax in subjects with mild, moderate, and severe hepatic impairment were similar to the subjects with normal hepatic function. No significant adverse safety events were reported.
Conclusions
No venetoclax dosage adjustment is required in subjects with mild or moderate hepatic impairment. In subjects with severe hepatic impairment, a 50% dose reduction of venetoclax is recommended to account for higher exposures and the longer half-life.




Similar content being viewed by others
References
Davids MS, Roberts AW, Seymour JF, Pagel JM, Kahl BS, Wierda WG, et al. Phase I first-in-human study of venetoclax in patients with relapsed or refractory non-Hodgkin lymphoma. J Clin Oncol. 2017;35(8):826–33. https://doi.org/10.1200/JCO.2016.70.4320.
Moreau P, Chanan-Khan A, Roberts AW, Agarwal AB, Facon T, Kumar S, et al. Promising efficacy and acceptable safety of venetoclax plus bortezomib and dexamethasone in relapsed/refractory MM. Blood. 2017;130(22):2392–400. https://doi.org/10.1182/blood-2017-06-788323.
de Vos S, Swinnen LJ, Wang D, Reid E, Fowler N, Cordero J, et al. Venetoclax, bendamustine, and rituximab in patients with relapsed or refractory NHL: a phase Ib dose-finding study. Ann Oncol. 2018;29(9):1932–8. https://doi.org/10.1093/annonc/mdy256.
Stilgenbauer S, Eichhorst B, Schetelig J, Hillmen P, Seymour JF, Coutre S, et al. Venetoclax for patients with chronic lymphocytic leukemia with 17p deletion: results from the full population of a phase II pivotal trial. J Clin Oncol. 2018;36(19):1973–80. https://doi.org/10.1200/JCO.2017.76.6840.
Jones JA, Mato AR, Wierda WG, Davids MS, Choi M, Cheson BD, et al. Venetoclax for chronic lymphocytic leukaemia progressing after ibrutinib: an interim analysis of a multicentre, open-label, phase 2 trial. Lancet Oncol. 2018;19(1):65–75. https://doi.org/10.1016/S1470-2045(17)30909-9.
Salem AH, Agarwal SK, Dunbar M, Enschede SL, Humerickhouse RA, Wong SL. Pharmacokinetics of venetoclax, a novel BCL-2 inhibitor, in patients with relapsed or refractory chronic lymphocytic leukemia or non-Hodgkin lymphoma. J Clin Pharmacol. 2017;57(4):484–92. https://doi.org/10.1002/jcph.821.
Agarwal SK, DiNardo CD, Potluri J, Dunbar M, Kantarjian HM, Humerickhouse RA, et al. Management of venetoclax-posaconazole interaction in acute myeloid leukemia patients: evaluation of dose adjustments. Clin Ther. 2017;39(2):359–67. https://doi.org/10.1016/j.clinthera.2017.01.003.
Agarwal SK, Hu B, Chien D, Wong SL, Salem AH. Evaluation of rifampin’s transporter inhibitory and CYP3A inductive effects on the pharmacokinetics of venetoclax, a BCL-2 inhibitor: results of a single- and multiple-dose study. J Clin Pharmacol. 2016;56(11):1335–43. https://doi.org/10.1002/jcph.730.
Agarwal SK, Salem AH, Danilov AV, Hu B, Puvvada S, Gutierrez M, et al. Effect of ketoconazole, a strong CYP3A inhibitor, on the pharmacokinetics of venetoclax, a BCL-2 inhibitor, in patients with non-Hodgkin lymphoma. Br J Clin Pharmacol. 2017;83(4):846–54. https://doi.org/10.1111/bcp.13175.
Cheung TT, Salem AH, Menon RM, Munasinghe WP, Bueno OF, Agarwal SK. Pharmacokinetics of the BCL-2 inhibitor venetoclax in healthy chinese subjects. Clin Pharmacol Drug Dev. 2018;7(4):435–40. https://doi.org/10.1002/cpdd.395.
Chiney MS, Menon RM, Bueno OF, Tong B, Salem AH. Clinical evaluation of P-glycoprotein inhibition by venetoclax: a drug interaction study with digoxin. Xenobiotica. 2017. https://doi.org/10.1080/00498254.2017.1381779.
Freise KJ, Hu B, Salem AH. Impact of ritonavir dose and schedule on CYP3A inhibition and venetoclax clinical pharmacokinetics. Eur J Clin Pharmacol. 2018;74(4):413–21. https://doi.org/10.1007/s00228-017-2403-3.
Salem AH, Hu B, Freise KJ, Agarwal SK, Sidhu DS, Wong SL. Evaluation of the pharmacokinetic interaction between venetoclax, a selective BCL-2 inhibitor, and warfarin in healthy volunteers. Clin Drug Investig. 2017;37(3):303–9. https://doi.org/10.1007/s40261-016-0485-9.
Agarwal SK, Tong B, Bueno OF, Menon RM, Salem AH. Effect of azithromycin on venetoclax pharmacokinetics in healthy volunteers: implications for dosing venetoclax with P-gp inhibitors. Adv Ther. 2018;35(11):2015–23. https://doi.org/10.1007/s12325-018-0793-y.
Salem AH, Dunbar M, Agarwal SK. Pharmacokinetics of venetoclax in patients with 17p deletion chronic lymphocytic leukemia. Anticancer Drugs. 2017;28(8):911–4. https://doi.org/10.1097/CAD.0000000000000522.
Liu H, Michmerhuizen MJ, Lao Y, Wan K, Salem AH, Sawicki J, et al. Metabolism and disposition of a novel B-cell lymphoma-2 inhibitor venetoclax in humans and characterization of its unusual metabolites. Drug Metab Dispos. 2017;45(3):294–305. https://doi.org/10.1124/dmd.116.071613.
Freise KJ, Shebley M, Salem AH. Quantitative prediction of the effect of CYP3A inhibitors and inducers on venetoclax pharmacokinetics using a physiologically based pharmacokinetic model. J Clin Pharmacol. 2017;57(6):796–804. https://doi.org/10.1002/jcph.858.
Freise KJ, Jones AK, Eckert D, Mensing S, Wong SL, Humerickhouse RA, et al. Impact of venetoclax exposure on clinical efficacy and safety in patients with relapsed or refractory chronic lymphocytic leukemia. Clin Pharmacokinet. 2017;56(5):515–23. https://doi.org/10.1007/s40262-016-0453-9.
Freise KJ, Dunbar M, Jones AK, Hoffman D, Enschede SL, Wong S, et al. Venetoclax does not prolong the QT interval in patients with hematological malignancies: an exposure-response analysis. Cancer Chemother Pharmacol. 2016;78(4):847–53. https://doi.org/10.1007/s00280-016-3144-1.
Freise KJ, Jones AK, Menon RM, Verdugo ME, Humerickhouse RA, Awni WM, et al. Relationship between venetoclax exposure, rituximab coadministration, and progression-free survival in patients with relapsed or refractory chronic lymphocytic leukemia: demonstration of synergy. Hematol Oncol. 2017;35(4):679–84. https://doi.org/10.1002/hon.2373.
Freise KJ, Jones AK, Verdugo ME, Menon RM, Maciag PC, Salem AH. Moving beyond maximum tolerated dose for targeted oncology drugs: use of clinical utility index to optimize venetoclax dosage in multiple myeloma patients. Clin Pharmacol Ther. 2017;102(6):970–6. https://doi.org/10.1002/cpt.712.
Parikh A, Gopalakrishnan S, Freise KJ, Verdugo ME, Menon RM, Mensing S, et al. Exposure-response evaluations of venetoclax efficacy and safety in patients with non-Hodgkin lymphoma. Leuk Lymphoma. 2018;59(4):871–9. https://doi.org/10.1080/10428194.2017.1361024.
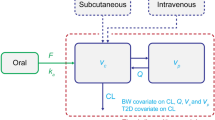
Jones AK, Freise KJ, Agarwal SK, Humerickhouse RA, Wong SL, Salem AH. Clinical predictors of venetoclax pharmacokinetics in chronic lymphocytic leukemia and non-Hodgkin’s lymphoma patients: a pooled population pharmacokinetic analysis. AAPS J. 2016;18(5):1192–202. https://doi.org/10.1208/s12248-016-9927-9.
US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER). Guidance for industry: pharmacokinetics in patients with impaired hepatic function: study design, data analysis, and impact on dosing and labeling. Rockville: Food and Drug Administration; 2003.
AbbVie Inc. Prescribing information for venclexta. North Chicago: AbbVie Inc; 2018.
Kalvass JC, Phipps C, Jenkins GJ, Stuart P, Zhang X, Heinle L, et al. Mathematical and experimental validation of flux dialysis method: an improved approach to measure unbound fraction for compounds with high protein binding and other challenging properties. Drug Metab Dispos. 2018;46(4):458–69. https://doi.org/10.1124/dmd.117.078915.
EMC. Venclyxto film-coated tablets. EMC. 2018. https://www.medicines.org.uk/emc/product/2267. Accessed 11 Oct 2018.
Verbeeck RK. Pharmacokinetics and dosage adjustment in patients with hepatic dysfunction. Eur J Clin Pharmacol. 2008;64(12):1147–61. https://doi.org/10.1007/s00228-008-0553-z.
Masters JC, Wiernik PH. Are we ready to include organ-impaired patients in oncology trials? A clinical pharmacology perspective on recent recommendations. J Clin Pharmacol. 2018;58(6):701–3. https://doi.org/10.1002/jcph.1127.
LoRusso PM, Venkatakrishnan K, Ramanathan RK, Sarantopoulos J, Mulkerin D, Shibata SI, et al. Pharmacokinetics and safety of bortezomib in patients with advanced malignancies and varying degrees of liver dysfunction: phase I NCI Organ Dysfunction Working Group Study NCI-6432. Clin Cancer Res. 2012;18(10):2954–63. https://doi.org/10.1158/1078-0432.CCR-11-2873.
Ramalingam SS, Kummar S, Sarantopoulos J, Shibata S, LoRusso P, Yerk M, et al. Phase I study of vorinostat in patients with advanced solid tumors and hepatic dysfunction: a National Cancer Institute Organ Dysfunction Working Group study. J Clin Oncol. 2010;28(29):4507–12. https://doi.org/10.1200/JCO.2010.30.2307.
Pearl T, Zhou D, Moorthy G, Masson E, Vishwanathan K. Comparison of Child–Pugh classification and NCI classification of hepatic impairment [abstract]. American Society for Clinical Pharmacology and Therapeutics: Abstracts of 2018 Annual Meeting. Clinical Pharmacology and Therapeutics. 2018. p. 93.
Salem AH, Agarwal SK, Dunbar M, Nuthalapati S, Chien D, Freise KJ, et al. Effect of low- and high-fat meals on the pharmacokinetics of venetoclax, a selective first-in-class BCL-2 inhibitor. J Clin Pharmacol. 2016;56(11):1355–61. https://doi.org/10.1002/jcph.741.
Dave N, Gopalakrishnan S, Mensing S, Salem AH. Effect of venetoclax on B-lymphocytes in healthy subjects. Clin Pharmacol Drug Dev. 2018;7(S1):1–104. https://doi.org/10.1002/cpdd.610.
Roberts AW, Davids MS, Pagel JM, Kahl BS, Puvvada SD, Gerecitano JF, et al. Targeting BCL2 with venetoclax in relapsed chronic lymphocytic leukemia. N Engl J Med. 2016;374(4):311–22. https://doi.org/10.1056/NEJMoa1513257.
Acknowledgements
The authors thank Mia DeFino, MS, a freelance medical writer under contract with AbbVie, for medical writing support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ahmed Hamed Salem, Nimita Dave, Beibei Hu, Suresh K. Agarwal, Orlando F. Bueno, and Rajeev M. Menon are/were employees of AbbVie and may hold AbbVie stock or stock options. Thomas Marbury is an employee and equity owner of Orlando Clinical Research Center. Dale Miles is an employee of Genentech and may hold Genentech stock or stock options.
Funding
Venetoclax is being developed in collaboration between AbbVie and Genentech/Roche. The study was sponsored by AbbVie and Genentech/Roche. AbbVie and Genentech/Roche contributed to the study design, research, and interpretation of data, and the writing, reviewing, and approving of the publication.
Rights and permissions
About this article
Cite this article
Salem, A.H., Dave, N., Marbury, T. et al. Pharmacokinetics of the BCL-2 Inhibitor Venetoclax in Subjects with Hepatic Impairment. Clin Pharmacokinet 58, 1091–1100 (2019). https://doi.org/10.1007/s40262-019-00746-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-019-00746-4