Abstract
Background and Objectives
Fexinidazole is a 5-nitroimidazole recently included in a clinical efficacy trial as an oral drug for the treatment of human African trypanosomiasis (HAT). Preclinical studies showed it acts as a pharmacologically active pro-drug with two key active metabolites: sulfoxide and sulfone (the most active metabolite). The present studies aimed to determine the best dose regimen for the treatment of stage 2 sleeping sickness patients, which could eventually also treat stage 1 patients.
Methods
Fexinidazole was assessed in 154 healthy adult male subjects of sub-Saharan African origin. Three initial first-in-human studies and two additional studies assessed a single ascending dose and multiple ascending doses (both under fasted conditions), tablet versus suspension formulation and food effect (fasted vs. high-fat meal and field-adapted food), and multiple ascending doses with a loading dose regimen under fed conditions.
Results
Fexinidazole was well-tolerated in a single dose from 100 to 3,600 mg, with quick absorption of the parent drug and rapid metabolism into sulfoxide [time to maximum concentration (t max) 2–5 h] and sulfone (t max 18–24 h). The tablet formulation was approximately 25 % less bioavailable than the suspension, and food intake increased drug absorption and plasma concentrations of fexinidazole and its two metabolites by approximately 200 %. Fourteen-day multiple ascending dosing administered up to 3,600 mg/day in fasted conditions showed that fexinidazole was generally well-tolerated (mild to moderate, spontaneously reversible drug-related adverse events). Following the high-fat food effect finding, another study was conducted to evaluate the impact of a low-fat regimen closer to that of the target population, showing that the type of meal does not influence fexinidazole absorption. The last study showed that a loading dose of 1,800 mg/day for 4 days followed by a 1,200 mg/day regimen for 6 days with a normal meal provided the desired exposure of fexinidazole and its metabolites, particularly sulfone, with good tolerability. Based on preclinical evidence from a chronic infection mouse model, systemic drug concentrations obtained are expected to be clinically effective in stage 2 HAT.
Conclusions
These studies show that fexinidazole can be safely assessed in patients as a potential oral cure for both stages of HAT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Human African trypanosomiasis (HAT) is transmitted through the bite of tse-tse flies infected with either Trypanosoma brucei gambiense (in west and central Africa) or Trypanosoma brucei rhodesiense (in eastern and southern Africa), causing chronic or acute sleeping sickness, respectively [1, 2]. Both forms of the disease occur in two stages, the first of which is characterised by non-specific symptoms, such as fever, headache, malaise and peripheral oedema. The second stage, which occurs once the parasite has crossed the blood–brain barrier, includes severe neurological symptoms, such as sleeping disturbances, behavioural changes and convulsions that, without treatment, progress to coma and eventually death.
Coordinated efforts to control the disease have resulted in a sustained decrease in the number of cases over the last 10 years, down to 10,000 new cases in 2010. Sub-Saharan Africa remains the worst affected area, with approximately 7,000 new cases reported in 2012, and approximately 69 million people are at risk of contracting HAT, the majority from T.b. gambiense infection (57 million). Therefore, much needs to be done if the WHO goal of global HAT elimination by 2020 is to be achieved [3, 4].
Current treatment for stage 2 HAT relies on toxic and difficult to use drugs. For example, melarsoprol treatment is highly toxic with up to 9 % drug-induced mortality in patients treated with the drug due to reactive encephalopathies [5]. Eflornithine treatment is expensive and logistically difficult in rural clinics as it requires four daily intravenous infusions over 14 days [6]. Despite being a clear improvement on other alternatives, the recently implemented combination of a simple regimen of intravenous eflornithine and oral nifurtimox [nifurtimox–eflornithine combination treatment (NECT)] [7, 8] remains far from ideal, as it still requires slow intravenous drug administration (14 infusions over 7 days), a procedure that can only be performed by well-trained staff in a hospital setting. The populations at risk of sleeping sickness are most often economically disadvantaged, living in rural communities far away from treatment centres and would therefore greatly benefit from a safe, easy-to-use, oral treatment.
Fexinidazole was recently developed as a novel drug candidate for HAT through a screening of over 700 nitroheterocyclic molecules against T. brucei [9]. Fexinidazole is a 2-substituted 5-nitroimidazole that exhibits in vitro and in vivo activity against both T.b. rhodesiense and T.b. gambiense [9, 10]. Oral administration of fexinidazole cures mouse models of both acute and chronic HAT infection, and pre-clinical absorption, distribution, metabolism and elimination studies show that it is well-absorbed and readily distributes throughout the body, including the brain [9]. Whilst fexinidazole, like many nitroheterocycles, is mutagenic in the Ames test, it is not genetically toxic to mammalian cells in vitro or in vivo and is therefore not expected to pose a genotoxic risk for humans [9, 11]. In all investigated animal species, fexinidazole was rapidly metabolised through oxidation, resulting in the formation of at least two pharmacologically active metabolites, fexinidazole sulfoxide (M1) and fexinidazole sulfone (M2), which are presumed to account for much of the trypanocidal activity in animal models [9]. No formal studies have been carried out to determine the mode of action of fexinidazole, but it is likely that the compound acts in a similar fashion to other 5-nitroimidazole drugs, which have a negative redox potential [12–14]. In order to investigate safety, tolerability and pharmacokinetics of fexinidazole, and establish a phase II dosing regimen to be assessed in patients with second stage sleeping sickness, we conducted a series of five studies in which healthy human subjects received single ascending doses (SAD), single fixed doses or multiple ascending doses (MAD) of orally administered fexinidazole according to different dosing regimens; we also investigated the relative bioavailability of different oral formulations, and the impact on bioavailability of different types of food.
2 Methods
The study protocols were approved by an independent ethics committee (CPP Ile de France III, Paris, France) and by the French health authorities (AFSSAPS; the French Agency for the Safety of Health Products) prior to the start of each study and written informed consent was obtained from all participants. The studies were conducted in accordance with the ethical principles stated in the Declaration of Helsinki (as revised by the 59th World Medical Association General Assembly in Seoul, Korea, October 2008), French Huriet law (No. 2004-806), and the Good Clinical Practice guidelines [15] and standard operating procedures for clinical investigation and documentation in force at the study site.
Details of study design and analytical methods employed are provided in the Electronic Supplementary Material.
2.1 Participants
Eligible subjects were healthy male volunteers, French residents of sub-Saharan origin, 18–45 years of age, with both parents of sub-Saharan African origin and a body mass index of 18–28 kg/m2 at the time of screening. Any subject with evidence of clinically significant acute or chronic disease, including known or suspected HIV, hepatitis B or C virus infection, who had previously received fexinidazole, or who had a positive drug screening test was excluded from the studies. Liver enzymes [aspartate aminotransferase (AST), alanine aminotransferase (ALT) and alkaline phosphatase] were required to be within normal ranges.
2.2 Procedures
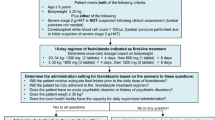
The first protocol was a combined, three-part under fasting conditions, sequential first-in-human study designed to obtain safety, tolerability and pharmacokinetic data after single and multiple oral administration of ascending doses of fexinidazole. The study was divided into three successive parts. Study 1A was a double-blind placebo-controlled SAD study. Study 1B was an open-label, crossover comparative bioavailability study of tablet versus suspension, and food effect with tablet—tablet/fasted versus tablet/high-fat rich meal. Study 1C was a double-blind placebo-controlled MAD study. The tablet was used in all consecutive studies. Following completion of these studies, two additional studies were carried out, the first to assess the impact of different types of food (Plumpy’Nut® and rice and beans) on the relative bioavailability of fexinidazole (Study 2); the final study was a double-blind placebo-controlled study under fed conditions (Study 3) to select one of the two optimised multiple dosing schedules to be used in subsequent clinical trials in patients based on modelling of pharmacokinetic data.
2.3 Dosage and Formulation Justification
The starting dose in the initial SAD study was defined on the basis of the 200 mg/kg/day no observed adverse effect level dose determined in 4-week toxicity studies in the fasted rat and dog [9] and, considering the lowest of these human equivalent doses and a safety margin of 1:20, a starting dose of 1.6 mg/kg was calculated with an initial single dose of 100 mg for both the suspension and tablet forms.
2.4 Study Drugs
Fexinidazole (1H-imidazole, 1-methyl-2-[[4-(methylthio) phenoxy] methyl] 5-nitro-imidazole) is insensitive to light, air, oxygen and moisture and is stable under accelerated storage conditions of 40 °C/75 % relative humidity for at least 6 months and for at least 24 months at 25 °C/60 % relative humidity.
The drug products used in the present studies consisted of two forms with matching placebo:
-
A powder-in-bottle (PIB) formulation consisting of 100, 200 or 600 mg micronised fexinidazole powder or matching placebo reconstituted in an aqueous solution as an oral suspension.
-
A tablet form consisting of 200 or 600 mg tablets of the investigational product with matching placebo. The 600 mg dosage form was selected for further clinical studies and potential commercialisation. Fexinidazole tablets have an estimated shelf-life of 24 months.
2.5 Design of Studies
Full details of the study designs are provided in the Electronic Supplementary Material.
A safety review committee (SRC) was constituted to oversee ascending-dose studies to allow dose progression; it consisted, at minimum, of the investigator or deputy and at least one sponsor representative. Additional SRC members were appointed or called in ad hoc, as required, including a statistician, pharmacokinetics experts and an independent third-party representative. In all studies, serious adverse events (SAEs) were defined as per the Good Clinical Practice guideline [15].
2.5.1 Study Protocol 1 (NCT00982904)
Study protocol 1 was a combined protocol that included three parts (study 1A–C).
Study 1A was a double-blind, within-cohort placebo-controlled SAD study of ascending doses of fexinidazole ranging from 100 to 3,600 mg in the form of an oral suspension of the PIB formulation carried out in cohorts of eight subjects (six active and two placebo) to determine safety and tolerability of the drug [16]. For each dose, adverse events (AEs), electrocardiogram (ECG) findings, vital signs and clinical laboratory tests (haematology, blood chemistry and urinalysis) were assessed for up to 48 h post-dose in a blinded fashion by the SRC before administration of the next dose. Blood samples for drug assay and plasma pharmacokinetic analysis were drawn until discharge. Urine was also collected for pharmacokinetic analysis.
A randomised, open-label, three-way crossover pharmacokinetic study (Study 1B) was carried out to assess the effect of single-dose fexinidazole, either as a suspension (PIB formulation) under fasted conditions (x) or as tablets under fasted (y) or fed conditions (z) on the bioavailability and safety of the study drug. Food consisted of a standard high-fat content meal. Twelve subjects were randomised; each subject received one of the three treatments (x, y or z) on three occasions in an open, randomised crossover design separated by a 14-day washout. The administered dose of 1,200 mg corresponded to a third of the maximum dose administered in study 1A. Determination of the free fraction of fexinidazole and its two metabolites was included in this study.
A randomised, double-blind, within-cohort, placebo-controlled MAD study evaluated fexinidazole 1,200, 2,400 and 3,600 mg doses (tablet formulation) as a single daily dose in three cohorts of eight subjects (six active and two placebo) for 14 days under fasting conditions (Study 1C). For each dose level, standard safety and tolerability measurements were regularly performed (AEs, ECG recordings, vital signs and biochemical analyses: haematology, biochemistry, enzymology and haemostasis) up to 48 h after the last dose on day 14 and were assessed in a blinded fashion by the SRC. Moreover, 24-h 12-lead Holter ECG was recorded before dosing and on day 14.
2.5.2 Study Protocol 2 (NCT01340157)
Study protocol 2 was a food interaction study performed to evaluate, in addition to the previous high-fat rich meal (Study 1B), the effect on fexinidazole bioavailability of two different meals, more representative of the local diet in target regions: a field-adapted meal of rice and beans, an easily quantifiable and non-fat carbohydrate food; and a field-available high-fat meal (Plumpy’Nut®). The design was a randomised, open-label, three-way crossover study to assess the effect of the two different types of food versus fasted conditions on the bioavailability and safety of a single 1,200 mg dose (two tablets of 600 mg). At each treatment sequence (treatment x = fasted, treatment y = Plumpy’Nut®, and treatment z = rice and beans) safety and tolerability follow-up were done up to 48 h post-dose, and an end-of-study visit was performed on day 8 of the last period of treatment before final discharge. Subjects participated in each of the three food regimens in a randomised order separated by a wash-out period of at least 14 days between doses, based on the available pharmacokinetic data from Study 1A, in order to prevent any carryover effects. In addition, blood samples for drug assay and pharmacokinetic analysis were taken until day 8 post each dosing.
2.5.3 Study Protocol 3 (NCT0148370)
Study protocol 3 was carried out following a population pharmacokinetic evaluation using all available data from the preceding studies exploring the various dosing regimens with food. The aim was to ascertain the most efficient dosing schedule in terms of rapidity to peak steady state and extended duration of systemic bioavailability of the fexinidazole sulfone metabolite M2. Simulations of the cerebrospinal fluid concentration were included using the free fraction determined in plasma in Study 1B. The target was to obtain the same plasma concentration that provided a curative effect in the GVR35 chronic mouse model [9, 10]. This murine model is, to date, the most widely studied laboratory model of the chronic disease, and fexinidazole cured the disease in this model, with oral dosing resulting in plasma drug concentrations of the sulfone metabolite of >10,000 ng/mL for a number of hours post-dosing.
The design was a randomised, double-blind, placebo-controlled MAD study performed in two cohorts of 16 subjects (12 active and six placebo) to evaluate two dosing regimens determined through pharmacokinetic modelling and simulation analysis. For each dose level, standard safety and tolerability (AEs, ECG findings, vital signs and clinical laboratory test results) up to 48 h after the last dose on day 10 were assessed in a blinded fashion by the SRC. Moreover, 24-h 12-lead Holter ECG was recorded before dosing and on days 4, 7 and 10 after dosing. Blood samples for drug assay and pharmacokinetic analysis were drawn until the end of study visit.
The following dosing regimens were studied sequentially:
Cohort 1: fexinidazole 1,800 mg or placebo from day 1 to day 4, then fexinidazole 1,200 mg or placebo from day 5 to day 10.
Cohort 2: fexinidazole 2,400 mg or placebo from day 1 to day 4, then fexinidazole 1,200 mg or placebo from day 5 to day 10.
2.6 Bioanalytical Assay
Fexinidazole and its sulfoxide (M1) and sulfone (M2) metabolites were analysed on a Supelco Ascentis® Express C18, 2.7 μm, 50 × 4.6 mm I.D. column using a validated liquid chromatography–tandem mass spectrometry (LC-MS/MS) method. In lithium heparinised plasma, the quantification limit of fexinidazole, M1 and M2 was 0.5, 10 and 10 ng/mL, respectively (see the Electronic Supplementary Material for further details).
2.7 Pharmacokinetic Analysis
Pharmacokinetic parameters for fexinidazole and its sulfoxide (M1) and sulfone (M2) metabolites were estimated using non-compartmental methods (WinNonlin® software, version 5.2, Pharsight Corporation, Mountain View, CA, USA). The pharmacokinetic parameters studied were maximum plasma concentration (C max), time to reach C max (t max), elimination rate constant (k e), area under the plasma concentration–time curve (AUC) from time zero to the last measurable concentration (AUClast) and, when applicable, AUC from time zero to 24 h post-dose and from time zero to infinity (AUC24 and AUC∞) determined by a linear trapezoidal method, terminal elimination half-life (t ½β) determined by linear regression using at least three time points, apparent total clearance of the drug from plasma (CL) after oral administration (CL/F) estimated using the ratio of dose to AUC, apparent volume of distribution after oral administration (V d/F) determined as CL/k e. Renal clearance of the drug from plasma (CLR) was estimated using the ratio of the amount of unchanged drug excreted into urine to the AUC for the time period considered.
2.8 Statistical Analysis
In Studies 1A and 1C, dose proportionality of fexinidazole was assessed based on plasma pharmacokinetic parameters over the complete dose range at each day of complete pharmacokinetic assessment using the power model of Gough et al. [17]. C max or AUCs and the dose value were log-transformed and evaluated using a linear mixed-effect model including a fixed effect due to log (dose) and a random effect due to subject. The dose proportionality was confirmed if the 90 % confidence interval (CI) (βl, βu) of the mean slope β was contained completely within the following critical region:
where r, defined as the dose ratio, is equal to h/l, h being the highest dose and l the lowest dose.
In Studies 1B and 2, analyses of C max and AUC for food and formulation effects were carried out by analysis of variance using PROC MIXED on the logarithmically transformed data including fixed factors for treatment, period and sequence. A random effect for the subject nested within the sequence was included in the model. The 90 % standard CI limits for relative treatment differences were calculated by geometric means based on logarithmic transformation of the intra-individual ratios of C max and AUC.
3 Results
3.1 Safety and Tolerability
Summary demographic data for all study subjects are shown in Table 1.
3.1.1 Study Protocol 1
3.1.1.1 Study 1A
In Study 1A, a total of 72 subjects were dosed, and all completed the study without relevant protocol deviations. Fifty-four subjects received the active drug. A total of eight mild AEs were reported, only three of which were considered to be possibly related to fexinidazole administration, the most frequent being headache. Two headaches were considered as probably related, and one case of pruritus was considered as unlikely to be related. No subjects were discontinued from the study due to AEs; no subject had SAEs. Neither trends nor relevant changes from baseline were observed in vital signs, ECG parameters, physical examination, or in any laboratory parameters assessed. The maximum tolerated dose was not reached and the highest administered dose, defined as the maximum administered dose, was 3,600 mg.
3.1.1.2 Study 1B
Further to replacement of one subject who withdrew consent for personal reasons, a total of 13 subjects were dosed in Study 1B with fexinidazole 1,200 mg, either as a suspension under fasted conditions (x) or as tablets under fasted (y) or fed conditions (z).
Twelve subjects completed the study without any relevant protocol deviation. Eleven AEs were reported, none of which were serious according to the definitions given by International Conference on Harmonisation (ICH) guidelines [18]. Six were considered possibly related to fexinidazole (five mild and one moderate), the most frequent being headache. Neither trends nor relevant changes from baseline were observed in vital signs, ECG parameters, physical examination, or in any laboratory parameters assessed.
3.1.1.3 Study 1C
In Study 1C, 27 subjects were given ascending doses of fexinidazole/placebo tablets, 17 of whom received active drug for 14 days, and nine received placebo for 14 days. One received treatment for 7 days only (the last subject in the study). It was decided to interrupt the treatment early after an SAE (before blind break) was reported for another subject—it was subsequently discovered that the subject had actually received placebo. Of the 27 subjects, 15 experienced at least one AE. All AEs recovered spontaneously or following single episodic symptomatic treatment. The most frequent AE was headache, with a total of 17 episodes reported by 11 subjects.
Two SAEs were reported by subjects who received fexinidazole: one subject (2,400 mg) asked to stop the study after 9 days of treatment due to intermittent headache, anxiety, vomiting, liquid stool episodes and myalgia of inferior limbs. Moderate anxiety had started the day preceding the first study drug administration and appeared to be the only cause of hospitalisation. The other SAE, on day 15, was observed in a second subject (3,600 mg) who exhibited a marked elevation in AST (10 times the normal upper limit) and ALT (7.4 times the normal upper limit). The volunteer was kept in the unit for surveillance for 48 h as the decrease was as strong as the increase. The subject was followed up for an additional 15 days until transaminase values were back to normal. Bilirubinaemia remained normal throughout the follow-up period.
Other laboratory abnormalities were observed in subjects under active treatment. Most of these were considered to be incidental and not clinically relevant, but it was also noted that, whilst remaining within normal ranges, creatinine levels increased progressively from the fourth day of treatment to its end, and returned to baseline values thereafter. This increase was not dose related and no other renal parameters were found to be similarly increased. Variations in creatinine were considered likely to be related to the drug class [19]. In addition, transaminase levels increased above normal upper limits, generally after treatment completion, regardless of the dose, even though the extent of the increase appeared to be dose related. Neither trends nor relevant changes from baseline were observed in vital signs and physical examination. Changes in ECG parameters consisting of an increase of heart rate and prolongation of the QT interval (within normal range) were observed across several dose levels, with no clear dose effect seen. These changes were of limited magnitude and generally remained strictly within normal ranges. None of the changes were considered to be of clinical relevance.
3.1.2 Study Protocol 2
Among the 12 subjects in Study 2 receiving fexinidazole 1,200 mg as oral tablets under fasted conditions or with one of the two meals, one withdrew consent and was not replaced. A total of nine AEs were reported, none of which was serious. Seven of the reported AEs were considered to be possibly related to fexinidazole administration (one under fasted conditions, one with concomitant Plumpy’Nut® intake, and five with concomitant rice and beans consumption). The intensity of AEs were mild (n = 5) or moderate (n = 2). The most frequent AE reported was headache (four cases reported by three subjects). No subjects were discontinued from the study due to AEs. Neither trends nor relevant changes from baseline were observed in vital signs, ECG parameters, physical examination, or in any laboratory parameters assessed.
3.1.3 Study Protocol 3
Thirty subjects were randomised in Study 3. In the first cohort of nine subjects receiving fexinidazole 1,800 + 1,200 mg as oral tablets, five subjects withdrew consent during the course of the study due to digestive disorders (nausea and vomiting). As a cohort effect was suspected, all were replaced and dosed in subgroups of three subjects per group. Using this dosing schedule, all subjects completed the dosing regimen. In the second cohort receiving fexinidazole 2,400 + 1,200 mg as oral tablets, two subjects withdrew due to AEs and were not replaced. This second dosing regimen was stopped after the inclusion of six subjects into the cohort. Overall, 22 of the 30 included subjects completed the study (18/24 in the first cohort and 4/6 in the second cohort). A total of 98 AEs were reported, of which only three were not considered to be related to the study drug (nasopharyngitis, and one episode of dizziness and headache; see details in Table 3). The incidence of AEs was higher within the first days following treatment initiation (loading dose). Of the AEs with a possible relationship to the study drug (83 %), the most frequent were gastrointestinal and nervous system disorders. Gastrointestinal disorders consisted mainly in vomiting (23/50), while central nervous system disorders were essentially headache (27/32). Vomiting episodes generally occurred up to 6–9 h post-dose. Given that the t max of fexinidazole is 2–4 h, the drug has long been absorbed by the time vomiting starts, suggesting that it is due to central effects. Two subjects in the second cohort experienced sustained anxiety with isolated episodes of panic attacks on the fifth day of dosing, which disappeared over the following 2–3 days after cessation of study drug treatment.
Mean haematology parameters remained within normal ranges throughout the study duration and, whilst sporadic individual abnormalities were observed, none was considered of clinical relevance. Mean biochemistry parameters also remained within normal limits, except for creatinine and creatine phosphokinase (CPK). Creatinine elevations had also been observed in Study 1C and, as no other abnormalities in renal parameters were observed, they were considered likely to be related to the drug class [19]. It is also possible that the observed CPK increases were related to physical exertion; the abnormal values were not considered clinically relevant. A total of ten post-dose elevations of liver function parameters were observed in both cohorts. Mean bilirubin (conjugated, free and total) values were comparable between the placebo and the two active dose groups, with no major trend in changes from baseline. Most of these were limited, and none of these abnormalities in laboratory data were considered to be of clinical relevance.
No abnormalities or out of range values were detected in the safety ECG analyses. Only one Holter-extracted ECG out of more than 4,000 revealed an increase from baseline of 60 ms, but remained within the normal ranges. The 24 h Holter recordings were analysed using an analytical method similar to that of Malik et al. [20] using five replicates per time point; double delta from baseline for corrected QT (QTc) interval and individual corrections based on QT/RR pattern at D-1.
As the regimen to be implemented in the planned pivotal efficacy study had been completed (cohort 1), and due to the poor tolerability observed in subjects in the second cohort, it was decided not to expose more subjects to this second dosage regimen and to stop the study.
A summary of AEs is provided in Tables 2 (single dose) and 3 (multiple-dose studies).
3.2 Pharmacokinetics
3.2.1 Pharmacokinetics of Fexinidazole and its Metabolites Fexinidazole Sulfoxide (M1) and Fexinidazole Sulfone (M2)
The pharmacokinetics of fexinidazole and its principle metabolites are summarised in Tables 4, 5, 6, 7 and 8. Examples of mean fexinidazole, M1 and M2 plasma concentrations versus time profiles under different conditions of administration are illustrated in Figs. 1 and 2. Overall, the profile of plasma concentrations of fexinidazole and its two principle metabolites is similar to that seen in laboratory animals [9, 12, 14].
Dose proportionality of increasing doses of fexinidazole oral suspension following increasing doses of fexinidazole suspension and fexinidazole sulfone (M2) assessed from the single ascending dose study (Study 1A): a C max, b AUC0–∞. C max maximum plasma concentration, AUC 0–∞ area under the plasma concentration–time curve from time zero to infinity
3.2.2 Single-Dose Pharmacokinetics of Fexinidazole (Study 1A, Study 1B and Study 2)
After administration of single doses of fexinidazole in fasted conditions, the drug was rapidly absorbed (median t max between 3 and 4 h post-dose). Thereafter, plasma concentrations exhibited a multiphasic decline, with a comparable elimination (geometric mean t ½β) for all dose levels of between 9 and 15 h. The primary metabolite, M1, exhibited a pharmacokinetic profile more consistent with the parent drug, since the C max as well as the terminal plasma t ½β occurred rapidly and in a similar range (median t max between 2 and 5 h post-dose and a geometric mean t ½ at around 8–15 h). Fexinidazole sulfone (M2) was found to be the major metabolite following oral administration of fexinidazole. Its plasma concentrations increased more slowly than the parent compound (or M1), reaching a maximum with a median time between 18 and 24 h post-dose, following which plasma concentrations decreased progressively with a geometric mean t ½β of about 18–25 h (Fig. 1). Inter-individual variability of C max and AUCs were slightly higher for the parent compound than for the metabolites and ranged between 19 and 77 % for fexinidazole, 8 and 59 % for M1, and 14 and 55 % for M2. Summary data are shown in Tables 4, 5 and 6.
Between 0.75 and 3.15 % of the fexinidazole dose was recovered in urine over the 168 h measured (sum of unchanged and transformed drug), after oral administration of ascending single doses, indicating that the elimination route of fexinidazole is almost entirely extra-renal. The corresponding renal clearance ranged from 1.23 to 6.01 mL/h.
The rate and extent of absorption of fexinidazole was less than dose proportional over the studied dose range (100–3,600 mg). When the administered dose was increased twofold, C max and AUC∞ increased 1.46- and 1.65-fold, respectively. The same held true for the metabolites, as a doubling of the dose resulted in an increase in C max and AUC∞ by 1.33- and 1.65-fold for M1 and 1.47 and 1.55-fold for M2, respectively. The observed dose proportionality of C max and AUC∞ is illustrated in Fig. 2 for fexinidazole and the M2 metabolite.
Comparison of the tablet formulation and the oral suspension (fexinidazole 1,200 mg dose: Study 1B) showed that the dissolution and distribution profiles of fexinidazole were very comparable, but that there was a decrease of about 25 % of the relative bioavailability of the tablet form.
Unexpectedly, when fexinidazole 1,200 mg tablets were administered with a high-fat breakfast (Study 1B), the relative bioavailability of the drug compared with fasted conditions showed a threefold increase for both rate and extent of absorption, as expressed by C max and AUC∞ (Table 4; Fig. 3). In parallel, the levels of M1 and M2 increased proportionally.
Comparable results were obtained when fexinidazole was taken with either a high-fat (Plumpy’Nut®) meal or a non-fat meal of rice and beans likely to be available to HAT patients in the field (Study 2), as summarised in Table 4. These results were unexpected and could not be predicted on the basis of known data with other drugs of the same class [21, 22]. Overall, concomitant food intake, such as Plumpy’Nut® or rice and beans, induced a marked increase of the relative bioavailability of fexinidazole: 2.8- and 1.6-fold increase for C max and AUC∞, respectively, with Plumpy’Nut® and 2.9- and 2-fold increase for C max and AUC∞ with rice and beans. The concentrations of M1 and M2 increased proportionally. In addition, systemic concentrations of fexinidazole and both metabolites were increased to a slightly higher extent after dosing with the rice and beans meal than with Plumpy’Nut®; on average, by +20, +19, +16 % (based on AUCs) for fexinidazole, M1 and M2, respectively. The metabolic ratios (metabolite vs. fexinidazole) of C max and AUCs were comparable between the three treatments, although there was a slight reduction under both fed conditions. This decrease seemed to be limited, suggesting that the increase of relative bioavailability induced by the concomitant food intake did not lead to significant changes in the rate of biotransformation of fexinidazole to M1, or of M1 into M2.
Protein binding was estimated from the ratio of the free fraction concentration over the corresponding total concentration measured, and appeared to be constant across time with the free fractions accounting for about 2 % for fexinidazole, 59 % for M1 and 43 % for M2, reflecting the known in vitro data [10].
3.2.3 Multiple-Dose Pharmacokinetics of Fexinidazole (Study 1C and Study 3)
After multiple oral administrations of fexinidazole tablets with doses ranging from 1,200 to 3,600 mg for 14 days, steady-state plasma drug concentrations were reached between 5 and 7 days for fexinidazole and M1, and between days 9 and 10 for M2. Overall, pharmacokinetic parameters remained unchanged when compared to single-dose studies. The rate and extent of absorption of fexinidazole and both metabolites were markedly less than dose proportional over the studied dose range since, after a 14-day administration, mean C max and AUClast increased by 1.17 and 1.34, respectively, when the dose doubled and by 1.50 and 1.61, respectively, for a threefold increase in dose. The same held true for the metabolites, as the mean C max and AUClast of M1 increased by 1.72 and 1.86 when the dose increased from 1,200 to 3,600 mg, while the mean C max and AUClast of M2 increased by 2.08 and 2.005. Summary data are shown in Table 7.
Based on the area over the dosing interval AUClast data there was an accumulation on day 7 compared with day 1 of 1.5, 2.1 and 7.3 for fexinidazole, M1 and M2, respectively. On day 14 the accumulation was comparable with day 7.
As reported with single-dose administration, urinary elimination of fexinidazole, M1 and M2 was negligible.
The effect of a loading dose and concomitant food intake following multiple dosing were assessed in Study 3. In terms of the simulated concentrations that could be expected, the median M2 C max of the highest regimen was predicted to be around 35,000 ng/mL and the median maximum AUC to be around 793,000 ng·h/mL compared with the plasma concentration observed in healthy volunteers after administration of 3,600 mg for 14 days, which was close to the maximum AUC observed (603,000 ng·h/mL) at maximum dose of Study 1C. As the dose was well-tolerated, the SRC authorised continuation to the second dose regimen of 2,400 mg, followed by 1,200 mg. The study shows that the dosage regimen used for cohort 1 yields high M2 concentrations, with plasma concentrations of at least 10,000 ng/mL, which is consistent with potential efficacy in the second stage of the disease. The study shows a peak in M2 concentrations between day 4 (C max 18,800 ng/mL) and day 7, with elevated levels maintained until day 10 (C max 12,000 ng/mL) (Table 8). Taking into account the high free fraction of the two metabolites, these results indicate that this drug regimen would yield M2 concentrations above required levels for efficacy, deduced from the mice study (>10,000 ng/mL for at least 2 days [9]), for at least 6 days (day 4 to day 10) in at least 83 % of subjects. These data are illustrated in Fig. 4, and are compared to the predicted concentration of the drugs from animal models required to kill 100 % of parasites in the central nervous system.
Geometric means of the maximum plasma concentration (n = 12) for fexinidazole, fexinidazole sulfoxide (M1) and fexinidazole sulfone (M2) at days 1, 4, 7 and 10 after oral dosing with fexinidazole tablets as per cohort 1 in Study 3. C max maximum plasma concentration, IC 90 concentration needed to inhibit 90 % parasite growth
4 Discussion
There is a great need for a safe, effective and preferably oral treatment for HAT. The coadministration of oral nifurtimox with intravenous eflornithine (NECT) is much safer than the previously used highly toxic, arsenic-based melarsoprol, and is the current best treatment for stage 2 HAT, having been included on the WHO Essential Medicines list since 2009. However, NECT still requires hospitalisation during the administration of the slow twice-daily infusions of eflornithine over a period of 7 days together with thrice-daily administration of nifurtimox for 10 days.
Nitroimidazoles have long been used for the treatment of parasitic diseases: metronidazole, the first class of nitroimidazoles, was discovered in the mid 1950s at Rhône-Poulenc during the search for a cure for the sexually transmitted disease trichomoniasis. Since then, derivatives have been used for the treatment of a number of bacterial and protozoan diseases. Fexinidazole was identified by DNDi out of hundreds of nitroimidazole compounds as a promising anti-protozoal drug candidate for the treatment of sleeping sickness.
In Study 1A, doses of fexinidazole ranging from 100 to 3,600 mg were found to be safe and well-tolerated. The decision to stop dosing at 3,600 mg was not based on potential safety or tolerability issues, but rather on the fact it was considered extremely unlikely that higher doses could be used in a clinical trial setting. The tolerability issue affecting transaminase levels observed following multiple dosing with the 3,600 mg/day oral tablet in one single subject at day 15 (Study 1C) further supported this decision. After oral administration, fexinidazole was absorbed and metabolised rapidly via a wide range of cytochrome P450 (CYP) enzymes and via the human flavine mono-oxygenase-3 (FMO-3) enzyme, observed in vitro (unpublished data on file), indicating a low risk of adverse drug interactions—the wide range of possible metabolic pathways via CYP indicates a low adverse drug reaction risk (drug–drug interaction) as alternative metabolic pathways exist if there is any drug–drug competition for a particular metabolic pathway.
The first metabolite, M1, appeared rapidly in plasma. The M2 metabolite peaked around 24 h after fexinidazole administration, with a mean terminal t ½ of about 24 h. As a result of these contrasting t ½ values, once-daily administration did not lead to marked accumulation of fexinidazole and M1, whilst the accumulation ratio for M2 was about 7. In these human studies, the free fraction of fexinidazole and its metabolites was 2 % for fexinidazole and about 60 and 43 % for M1 and M2, respectively, matching the available in vitro data [10]. The pattern of absorption, metabolism and elimination is qualitatively similar to that seen in animal studies [9]. After oral administration of ascending single doses between 0.75 and 3.15 % of the fexinidazole dose was recovered unchanged or as M1 or M2 in urine over 168 h. This indicates that the elimination route of fexinidazole is almost entirely extra-renal. This conclusion is supported by the renal clearance rate, which is low (mean values around about 1.2–6.0 mL/h, Study 1A) when compared with the apparent oral clearance (mean CL/F of more than 80 L/h for all three compounds).
Data from Study 1B indicate that the tablet form is absorbed approximately 25 % less efficiently than the suspension form. It is likely that this reduction in overall absorption of fexinidazole in the tablet form reflects the time taken for full disintegration and dissolution of the tablets relative to the rate of gastric emptying. Fexinidazole can be considered to be a Biopharmaceutical Classification System (BCS) Class III drug [19] in terms of its solubility and absorption properties, such that the rate of drug dissolution is likely to be the determining factor for the degree of absorption within a given gastric transit period.
The effect of concomitant food intake on fexinidazole bioavailability was unexpected given the preclinical data or existing literature on the drug class [21, 23]. There is evidence that metronidazole absorption is retarded if taken with food [22], and whilst it is recommended that the clinically available 5-nitroimidazole drugs be taken with food to reduce the risk of gastrointestinal adverse effects, no change in oral bioavailability has been described [24]. These data, coupled with the results from Study 2 indicating that the type of food taken does not influence the bioavailability, support the notion that the observed bioavailability increase is due to a delay in gastric emptying, rather than to an effect on gastrointestinal tract physiology. Overall, it is possible that an increase in time available for gastric absorption may allow for a prolonged residence time for fexinidazole at the site of intestinal absorption, thus increasing initial metabolism in the gastric intestinal mucosa, providing for higher overall levels of M1, and subsequently M2, in the systemic circulation, as has been proposed for some cephalosporin pro-drugs [25]. The minimal changes in metabolic ratios after food also suggest that the increased bioavailability is not due to changes in the rate of biotransformation of fexinidazole to M1 or of M1 to M2. A decrease in gastric pH may also contribute to an improved disintegration and dissolution profile for fexinidazole tablets and thus an increased absorption potential; however, it is not known whether such a decrease occurred in the current studies.
In Study 1C, clinically significant changes in safety laboratory tests were observed after the last day of dosing, especially in the liver function test (LFT). In one subject, LFT plasma levels rapidly increased before rapidly decreasing the next day. On further expert analysis, it was concluded that the results did not follow Hay’s law (hepatocellular injury sufficient to cause hyperbilirubinaemia acts as an indicator of the potential for a drug to cause serious liver injury) [26, 27] and thus could be considered as an isolated reaction to the study drug. The variations in creatinine seen in Study 1C were considered likely to have been caused via inhibition of renal tubular secretion of creatinine, as reported for the drug class [19], and it is also likely that the smaller increases in transaminases noted were due to the conditions of the study, as such rises have been seen in many first-in-man trials [28].
The increase in absorption of the drug when taken with food clearly provides an opportunity for maximising systemic drug concentrations. Typically, the carbohydrate staple of the main meal in endemic areas is ‘fufu’, a solid paste of manioc with or without maize, or sometimes just rice. Chicken or fish cooked in palm oil are a source of protein. The food type comparison data from Study 2 showed that a normal meal, likely to be readily available to HAT patients, was sufficient to obtain 2.5–3 times higher plasma concentrations, particularly of M2, when compared with fasted condition. Therefore, a population pharmacokinetic model was developed [29] in order to find a treatment schedule that allowed high plasma M2 (>10,000 ng/mL,) levels to be reached on day 2–3 (compared with day 4 under fasted conditions) and maintained for at least 4 days. These simulated results were tested in healthy volunteers to ensure that such an increase does not introduce unacceptable adverse effects. The aim of this last study (Study 3) was to select the best treatment regimen to be used for a phase II/III trial.
Study 3 shows the best tolerated treatment regimen to be 1,800 mg once a day for 4 days followed by 1,200 mg once a day for 6 days after the main meal of the day. The tolerability was considered to be acceptable, and although some headache and nausea AEs occurred initially, they were only of mild to moderate severity and spontaneously reverted during treatment. Safety laboratory tests conducted during the study did not detect any of the abnormalities seen in the 14-day dosing regimen used in Study 1C. This improved tolerability, particularly in relation to the concerns around the LFTs, supported the hypothesis that a possible accumulation of high-dose drug product rather than any specific product sensitivity of the liver were the most likely causes of the LFT abnormalities seen during the 14-day multiple-dose study.
Electrocardiograms were recorded during all studies and were specifically analysed by an independent cardiologist for variations in QT/QTc intervals. No out-of-range values of the QTc in all the ECGs were detected. However, compared with placebo and baseline, an average, non-dose-dependent variation was elicited in QT/QTc of around 16 ms.
5 Conclusions
First-in-man clinical studies have demonstrated that doses of up to 3,600 mg of fexinidazole in fasted conditions are safe and well-tolerated in healthy male subjects of sub-Saharan origin. The main reported AEs were headache and vomiting of acceptable intensity, which spontaneously resolved in all cases. A dosing regimen of fexinidazole 1,800 mg for 4 days and 1,200 mg for 6 days with concomitant food was shown to meet the required criteria of effective drug concentrations with a good safety profile. Based on the available in vitro and animal model data, it can be predicted that the proposed dosing regimen would be effective in curing both stage 2 and stage 1 HAT. This prediction is currently being tested in a pivotal phase II/III comparative study in stage 2 patients in HAT endemic regions and, if successful, will provide patients with the first oral treatment for stage 2 sleeping sickness, which could revolutionise treatment in the field.
The oxaborole SCYX-7158 has recently entered phase I clinical studies for the treatment of sleeping sickness. As far as we are aware, fexinidazole is the only new drug currently in phase II/III clinical development for the treatment of stage 2 sleeping sickness. Moreover, it has recently been shown to be active against visceral leishmaniasis and Chagas disease [12, 30]. These findings illustrate the potential of fexinidazole as a drug candidate for the treatment of different kinetoplastid diseases.
References
Brun R, Blum J, Chappuis F, Burri C. Human African trypanosomiasis. Lancet. 2010;375:148–59.
Barrett MP, Boykin DW, Brun R, Tidwell RR. Human African trypanosomiasis: pharmacological re-engagement with a neglected disease. Br J Pharmacol. 2007;152:1155–71.
Joubert J. Report of a WHO meeting on elimination of African trypanosomiasis (Trypanosoma brucei gambiense). Geneva, 3–5 December 2012. Geneva: WHO; 2013. p. 1754–824.
Hasker E, Lutumba P, Chappuis F, Kande V, Potet J, De Weggheleire A, et al. Human African trypanosomiasis in the Democratic Republic of the Congo: a looming emergency? PLoS Negl Trop Dis. 2012;6:e1950.
World Health Organization. Control and surveillance of human African trypanosomiasis: report of a WHO expert committee. WHO Technical Report Series 984. Geneva: WHO; 2013.
Bacchi CJ. Chemotherapy of human African trypanosomiasis. Interdiscip Perspect Infect Dis. 2009;2009:195040.
Priotto G, Kasparian S, Mutombo W, Ngouama D, Ghorashian S, Arnold U, et al. Nifurtimox-eflornithine combination therapy for second-stage African Trypanosoma brucei gambiense trypanosomiasis: a multicentre, randomised, phase III, non-inferiority trial. Lancet. 2009;374:56–64.
Schmid C, Kuemmerle A, Blum J, Ghabri S, Kande V, Mutombo W, et al. In-hospital safety in field conditions of nifurtimox eflornithine combination therapy (NECT) for T. b. gambiense sleeping sickness. PLoS Negl Trop Dis. 2012;6:e1920.
Torreele E, Bourdin Trunz B, Tweats D, Kaiser M, Brun R, Mazue G, et al. Fexinidazole—a new oral nitroimidazole drug candidate entering clinical development for the treatment of sleeping sickness. PLoS Negl Trop Dis. 2010;4:e923.
Kaiser M, Bray MA, Cal M, Bourdin Trunz B, Torreele E, Brun R, et al. Antitrypanosomal activity of fexinidazole, a new oral nitroimidazole drug candidate for treatment of sleeping sickness. Antimicrob Agents Chemother. 2011;55:5602–8.
Tweats D, Bourdin Trunz B, Torreele E. Genotoxicity profile of fexinidazole—a drug candidate in clinical development for human African trypanomiasis (sleeping sickness). Mutagenesis. 2012;27:223–32.
Wyllie S, Patterson S, Stojanovski L, Simeons FRC, Norval S, Kime R, et al. The anti-trypanosome drug fexinidazole shows potential for treating visceral leishmaniasis. Sci Transl Med. 2012;4:119re1.
Wilkinson SR, Taylor MC, Horn D, Kelly JM, Cheeseman I. A mechanism for cross-resistance to nifurtimox and benznidazole in trypanosomes. Proc Natl Acad Sci U S A. 2008;105:5022–7.
Sokolova AY, Wyllie S, Patterson S, Oza SL, Read KD, Fairlamb AH. Cross-resistance to nitro-drugs and implications for the treatment of human African trypanosomiasis. Antimicrob Agents Chemother. 2010;54:2893–900.
ICH harmonised tripartite guideline for good clinical practice E6(R1). http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6_R1/Step4/E6_R1__Guideline.pdf. Accessed 11 Feb 2011.
Tarral A, Valverde O, Blesson S, Strub-Wourgaft N, Hosvepian L, Evene E. Single-dose safety and pharmacokinetics of fexinidazole in healthy subjects. 7th European Congress on Tropical Medicine & International Health; 3–6 Oct 2011; Barcelona. http://www.dndi.org/media-centre/events/events-2011/216-media-centre/events/980-barcelona.html. Accessed 11 Feb 2011.
Gough K, Hutchison M, Keene O, Byrom B, Ellis S, Lacey L, et al. Assessment of dose proportionality: report from the Statisticians in the Pharmaceutical Industry/Pharmacokinetics UK Joint Working Party. Drug Inf J. 1995;29:1039–48.
Note for guidance on clinical safety data management: definitions and standards for expedited reporting (CPMP/ICH/377/95); 2006. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002749.pdf. Accessed 11 Feb 2011.
Amidon G, Lennernäs H, Shah V, Crison J. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995;12:413–20.
Malik M, Hnatkova K, Ford J, Madge D. Near-thorough QT study as part of a first-in-man study. J Clin Pharmacol. 2008;48:1146–57.
Lamp KC, Freeman CD, Klutman NE, Lacy MK. Pharmacokinetics and pharmacodynamics of the nitroimidazole antimicrobials. Clin Pharmacokinet. 1999;36(5):353–73.
Spénard J, Aumais C, Massicotte J, Brunet J-S, Tremblay C, Grace M, et al. Effects of food and formulation on the relative bioavailability of bismuth biskalcitrate, metronidazole, and tetracycline given for Helicobacter pylori eradication. Br J Clin Pharmacol. 2005;60:374–7.
Lau AH, Lam NP, Piscitelli SC, Wilkes L, Danziger LH. Clinical pharmacokinetics of metronidazole and other nitroimidazole anti-infectives. Clin Pharmacokinet. 1992;23:328–64.
Mission Pharmacal Company. Tindamax (tinidazole) tablet, film coated for oral use. Daily Med; 2007. http://dailymed.nlm.nih.gov/dailymed/archives/fdaDrugInfo.cfm?archiveid=5060. Accessed 11 Feb 2011.
Hughes DL, Barker KB, Patel RK, Spillers CR, Watts KC, Batts DHE. The effects of gastric pH and food on the pharmacokinetics of a new oral cephalosporin, cefpodoxime proxetil. Clin Pharmacol Ther. 1989;46:674–85.
Zimmerman HJ. Drug-induced liver disease. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1999. p. 427–57.
FDA/CDER/CBER. Guidance for industry. Drug-induced liver injury: premarketing clinical evaluation. Rockville: U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER); 2009.
Rosenzweig P, Miget T, Brohier S. Transaminase elevation on placebo during phase I trials: prevalence and significance. Br J Clin Pharmacol. 1999;48:19–23.
Gualano V, Felices M, Evene E, Blesson S, Tarral A. Dose regimen assessment for oral fexinidazole [abstract no. 2572]. PAGE. Abstracts of the annual meeting of the Population Approach Group in Europe. ISSN 1871-6032; 2012. p. 21. http://www.page-meeting.org/?abstract=2572. Accessed 11 Feb 2011.
Bahia MT, de Andrade IM, Martins TAF, do Nascimento ÁFDS, Diniz LDF, Caldas IS, et al. Fexinidazole: a potential new drug candidate for Chagas disease. PLoS Negl Trop Dis. 2012;6:e1870.
Winkelmann E, Raether W. New chemotherapeutically active nitroimidazoles. Curr Chemother Infect Dis, Proc 11th Int Congr Chemother. 1980;2:969–70.
Acknowledgments
The clinical studies were carried out by the SGS Aster Clinical Unit (Paris, France) with Phinc Development (Evry, France) performing pharmacokinetic and statistical analysis, and manuscript preparation; the work was funded by the Drugs for Neglected Diseases initiative (DNDi) through a donor grant from the Bill and Melinda Gates Foundation. The donor had no role in study design, data collection, data analysis, data interpretation or writing of the report.
The authors wish to thank the Sanofi Research & Development and Access to Medicines departments for their review of the initial study. We would also like to thank Hana Bilak and Susan Wells (DNDi) for help writing and editing the manuscript.
Author contributions
AT, SB, OVM, ET, DS, MB, NSW and VG conceived and designed the experiments; LH performed the clinical studies; VG, MF and EE analysed the data and performed the statistical and pharmacokinetic analyses; AT, MB and VG wrote the paper.
VG, EE and MF are employees of Phinc. AT, SB, OVM, ET, DS, MB, NSW and LH have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The studies were registered with ClinicalTrials.gov under the following numbers: NCT00982904, NCT01340157 and NCT0148370.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Tarral, A., Blesson, S., Mordt, O.V. et al. Determination of an Optimal Dosing Regimen for Fexinidazole, a Novel Oral Drug for the Treatment of Human African Trypanosomiasis: First-in-Human Studies. Clin Pharmacokinet 53, 565–580 (2014). https://doi.org/10.1007/s40262-014-0136-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-014-0136-3