Abstract
Background and Objective
Ketamine, a noncompetitive, high-affinity antagonist of the N-methyl-d-aspartate type glutamate receptor, has been investigated for its high efficacy and rapid antidepressant effect and, more recently, for its potential utility in post-traumatic stress disorder (PTSD). The proposal that ketamine’s antidepressant and anti-suicidal mechanism may be in part due to its procognitive effect contrasts with the well-established decreased performance on spatial working memory and pattern recognition memory among long-term frequent users. We aimed to review the neurocognitive effects of subanesthetic doses of intravenous ketamine in pharmacological studies among healthy subjects and patients with PTSD or depression.
Methods
We included studies in English, among healthy adults, or with PTSD or unipolar or bipolar depression where the primary or secondary cognitive outcomes were measured by means of validated neuropsychological test. We excluded studies that reported the use of ketamine only in combination with other drugs or psychotherapy, or studies investigating emotion-laden cognitive functions.
Results
Ketamine administration among patients with depression and possibly with PTSD does not show significant impairment of cognitive functions in the short-term, in contrast with the immediate altered cognitive dysfunction found in healthy subjects. The potential procognitive effects of ketamine seem more pronounced in cognitive domains of executive function, which is in line with the putative molecular, cellular, and synaptic mechanisms of ketamine’s therapeutic action.
Conclusions
The potential procognitive effect of ketamine deserves further exploration. Whether ketamine has transient or sustained neurocognitive benefits beyond its antidepressant effects is unknown. Improved cognition by ketamine might be used to facilitate psychotherapy interventions for PTSD and depression.

Similar content being viewed by others
References
Green SM, Li J. Ketamine in adults: what emergency physicians need to know about patient selection and emergence reactions. Acad Emerg Med. 2000;7(3):278–81. https://doi.org/10.1111/j.1553-2712.2000.tb01076.x.
Zarate CA Jr, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63(8):856–64. https://doi.org/10.1001/archpsyc.63.8.856.
Murrough JW, Iosifescu DV, Chang LC, Al Jurdi RK, Green CE, Perez AM, et al. Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatry. 2013;170(10):1134–42. https://doi.org/10.1176/appi.ajp.2013.13030392.
Popova V, Daly EJ, Trivedi M, Cooper K, Lane R, Lim P, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019;176(6):428–38. https://doi.org/10.1176/appi.ajp.2019.19020172 (Erratum in: Am J Psychiatry. 2019;176(8):669).
Advisory Council on the Misuse of Drugs. Ketamine: a review of use and harm. https://www.gov.uk/government/publications/ketamine-report. Accessed 10 Dec 2013.
Ploski JE, Vaidya VA. The neurocircuitry of posttraumatic stress disorder and major depression: insights into overlapping and distinct circuit dysfunction—a tribute to Ron Duman. Biol Psychiatry. 2021;90(2):109–17. https://doi.org/10.1016/j.biopsych.2021.04.009.
Lam RW, Kennedy SH, Mclntyre RS, Khullar A. Cognitive dysfunction in major depressive disorder: effects on psychosocial functioning and implications for treatment. Can J Psychiatry. 2014;59(12):649–54. https://doi.org/10.1177/070674371405901206.
Torrent C, Martinez-Aran A, Daban C, Amann B, Balanza-Martinez V, del Mar BC, et al. Effects of atypical antipsychotics on neurocognition in euthymic bipolar patients. Compr Psychiatry. 2011;52(6):613–22. https://doi.org/10.1016/j.comppsych.2010.12.009.
Aupperle RL, Allard CB, Grimes EM, Simmons AN, Flagan T, Behrooznia M, et al. Dorsolateral prefrontal cortex activation during emotional anticipation and neuropsychological performance in posttraumatic stress disorder. Arch Gen Psychiatry. 2012;69(4):360–71. https://doi.org/10.1001/archgenpsychiatry.2011.1539.
Yang Z, Oathes DJ, Linn KA, Bruce SE, Satterthwaite TD, Cook PA, et al. Cognitive behavioral therapy is associated with enhanced cognitive control network activity in major depression and posttraumatic stress disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(4):311–9. https://doi.org/10.1016/j.bpsc.2017.12.006.
Lee Y, Syeda K, Maruschak NA, Cha DS, Mansur RB, Wium-Andersen IK, et al. A new perspective on the anti-suicide effects with ketamine treatment: a procognitive effect. J Clin Psychopharmacol. 2016;36(1):50–6. https://doi.org/10.1097/JCP.0000000000000441.
Morgan CJ, Muetzelfeldt L, Curran HV. Consequences of chronic ketamine self-administration upon neurocognitive function and psychological wellbeing: a 1-year longitudinal study. Addiction. 2010;105(1):121–33. https://doi.org/10.1111/j.1360-0443.2009.02761.x (Erratum in: Addiction. 2010;105(4):766).
Roiser JP, Sahakian BJ. Hot and cold cognition in depression. CNS Spectr. 2013;18(3):139–49. https://doi.org/10.1017/S1092852913000072.
Morgan CJ, Mofeez A, Brandner B, Bromley L, Curran HV. Acute effects of ketamine on memory systems and psychotic symptoms in healthy volunteers. Neuropsychopharmacology. 2004;29(1):208–18. https://doi.org/10.1038/sj.npp.1300342.
Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD, et al. Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry. 1994;51(3):199–214. https://doi.org/10.1001/archpsyc.1994.03950030035004.
Anand A, Charney DS, Oren DA, Berman RM, Hu XS, Cappiello A, et al. Attenuation of the neuropsychiatric effects of ketamine with lamotrigine: support for hyperglutamatergic effects of N-methyl-D-aspartate receptor antagonists. Arch Gen Psychiatry. 2000;57(3):270–6. https://doi.org/10.1001/archpsyc.57.3.270.
Krystal JH, Karper LP, Bennett A, D’Souza DC, Abi-Dargham A, Morrissey K, et al. Interactive effects of subanesthetic ketamine and subhypnotic lorazepam in humans. Psychopharmacology. 1998;135(3):213–29. https://doi.org/10.1007/s002130050503.
Krystal JH, Bennett A, Abi-Saab D, Belger A, Karper LP, D’Souza DC, et al. Dissociation of ketamine effects on rule acquisition and rule implementation: possible relevance to NMDA receptor contributions to executive cognitive functions. Biol Psychiatry. 2000;47(2):137–43. https://doi.org/10.1016/s0006-3223(99)00097-9.
D’Souza DC, Ahn K, Bhakta S, Elander J, Singh N, Nadim H, et al. Nicotine fails to attenuate ketamine-induced cognitive deficits and negative and positive symptoms in humans: implications for schizophrenia. Biol Psychiatry. 2012;72(9):785–94. https://doi.org/10.1016/j.biopsych.2012.05.009.
Ghoneim MM, Hinrichs JV, Mewaldt SP, Petersen RC. Ketamine: behavioral effects of subanesthetic doses. J Clin Psychopharmacol. 1985;5(2):70–7.
Krystal JH, Perry EB Jr, Gueorguieva R, Belger A, Madonick SH, Abi-Dargham A, et al. Comparative and interactive human psychopharmacologic effects of ketamine and amphetamine: implications for glutamatergic and dopaminergic model psychoses and cognitive function. Arch Gen Psychiatry. 2005;62(9):985–94. https://doi.org/10.1001/archpsyc.62.9.985.
Rowland LM, Astur RS, Jung RE, Bustillo JR, Lauriello J, Yeo RA. Selective cognitive impairments associated with NMDA receptor blockade in humans. Neuropsychopharmacology. 2005;30(3):633–9.
Adler CM, Goldberg TE, Malhotra AK, Pickar D, Breier A. Effects of ketamine on thought disorder, working memory, and semantic memory in healthy volunteers. Biol Psychiatry. 1998;43(11):811–6. https://doi.org/10.1038/sj.npp.1300642.
Koychev I, William Deakin JF, El-Deredy W, Haenschel C. Effects of acute ketamine infusion on visual working memory: event-related potentials. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2(3):253–62. https://doi.org/10.1016/j.bpsc.2016.09.008.
Malhotra AK, Pinals DA, Weingartner H, Sirocco K, Missar CD, Pickar D, et al. NMDA receptor function and human cognition: the effects of ketamine in healthy volunteers. Neuropsychopharmacology. 1996;14(5):301–7. https://doi.org/10.1016/0893-133X(95)00137-3.
Hetem LA, Danion JM, Diemunsch P, Brandt C. Effect of a subanesthetic dose of ketamine on memory and conscious awareness in healthy volunteers. Psychopharmacology. 2000;152(3):283–8. https://doi.org/10.1007/s002130000511.
Shiroma PR, Albott CS, Johns B, Thuras P, Wels J, Lim KO. Neurocognitive performance and serial intravenous subanesthetic ketamine in treatment-resistant depression. Int J Neuropsychopharmacol. 2014;17(11):1805–13. https://doi.org/10.1017/S1461145714001011.
Shiroma PR, Thuras P, Wels J, Albott CS, Erbes C, Tye S, et al. Neurocognitive performance of repeated versus single intravenous subanesthetic ketamine in treatment resistant depression. J Affect Disord. 2020;277:470–7. https://doi.org/10.1016/j.jad.2020.08.058.
Chen MH, Li CT, Lin WC, Hong CJ, Tu PC, Bai YM, et al. Cognitive function of patients with treatment-resistant depression after a single low dose of ketamine infusion. J Affect Disord. 2018;241:1–7. https://doi.org/10.1016/j.jad.2018.07.033.
Araujo-de-Freitas L, Santos-Lima C, Mendonca-Filho E, Vieira F, Franca R, Magnavita G, et al. Neurocognitive aspects of ketamine and esketamine on subjects with treatment-resistant depression: a comparative, randomized and double-blind study. Psychiatry Res. 2021;303: 114058. https://doi.org/10.1016/j.psychres.2021.114058.
Murrough JW, Burdick KE, Levitch CF, Perez AM, Brallier JW, Chang LC, et al. Neurocognitive effects of ketamine and association with antidepressant response in individuals with treatment-resistant depression: a randomized controlled trial. Neuropsychopharmacology. 2015;40(5):1084–90. https://doi.org/10.1038/npp.2014.298.
Keilp JG, Madden SP, Marver JE, Frawley A, Burke AK, Herzallah MM, et al. Effects of ketamine versus midazolam on neurocognition at 24 hours in depressed patients with suicidal ideation. J Clin Psychiatry. 2021. https://doi.org/10.4088/JCP.21m13921.
Murrough JW, Wan LB, Iacoviello B, Collins KA, Solon C, Glicksberg B, et al. Neurocognitive effects of ketamine in treatment-resistant major depression: association with antidepressant response. Psychopharmacology. 2013. https://doi.org/10.1007/s00213-013-3255-x.
Diamond PR, Farmery AD, Atkinson S, Haldar J, Williams N, Cowen PJ. Ketamine infusions for treatment resistant depression: a series of 28 patients treated weekly or twice weekly in an ECT clinic. J Psychopharmacol. 2014;28(6):536–44. https://doi.org/10.1177/0269881114527361.
Permoda-Osip A, Kisielewski J, Bartkowska-Sniatkowska A, Rybakowski JK. Single ketamine infusion and neurocognitive performance in bipolar depression. Pharmacopsychiatry. 2015;48(2):78–9. https://doi.org/10.1055/s-0034-1394399.
Zheng W, Zhou YL, Liu WJ, Wang CY, Zhan YN, Li HQ, et al. Neurocognitive performance and repeated-dose intravenous ketamine in major depressive disorder. J Affect Disord. 2018;246:241–7. https://doi.org/10.1016/j.jad.2018.12.005.
Basso L, Bonke L, Aust S, Gartner M, Heuser-Collier I, Otte C, et al. Antidepressant and neurocognitive effects of serial ketamine administration versus ECT in depressed patients. J Psychiatr Res. 2020;123:1–8. https://doi.org/10.1016/j.jpsychires.2020.01.002 (Erratum in: J Psychiatr Res. 2020;124:143).
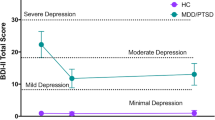
Albott CS, Lim KO, Erbes C, Thuras P, Wels J, Tye SJ, et al. Neurocognitive effects of repeated ketamine infusions in comorbid posttraumatic stress disorder and major depressive disorder. J Affect Disord. 2022;308:289–97. https://doi.org/10.1016/j.jad.2022.04.066.
Liu W, Zhou Y, Zheng W, Wang C, Zhan Y, Lan X, et al. Repeated intravenous infusions of ketamine: neurocognition in patients with anxious and nonanxious treatment-resistant depression. J Affect Disord. 2019;259:1–6. https://doi.org/10.1016/j.jad.2019.08.012.
Zhou Y, Zheng W, Liu W, Wang C, Zhan Y, Li H, et al. Neurocognitive effects of six ketamine infusions and the association with antidepressant response in patients with unipolar and bipolar depression. J Psychopharmacol. 2018;32(10):1118–26. https://doi.org/10.1177/0269881118798614.
Feder A, Costi S, Rutter SB, Collins AB, Govindarajulu U, Jha MK, et al. A randomized controlled trial of repeated ketamine administration for chronic posttraumatic stress disorder. Am J Psychiatry. 2021;178(2):193–202. https://doi.org/10.1176/appi.ajp.2020.20050596.
Koenigs M, Grafman J. The functional neuroanatomy of depression: distinct roles for ventromedial and dorsolateral prefrontal cortex. Behav Brain Res. 2009;201(2):239–43.
Rauch SL, Shin LM, Phelps EA. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research–past, present, and future. Biol Psychiatry. 2006;60(4):376–82.
Sheynin J, Liberzon I. Circuit dysregulation and circuit-based treatments in posttraumatic stress disorder. Neurosci Lett. 2017;10(649):133–8.
Yuksel C, Ongur D. Magnetic resonance spectroscopy studies of glutamate-related abnormalities in mood disorders. Biol Psychiatry. 2010;68(9):785–94.
Li N, Lee B, Liu RJ, Banasr M, Dwyer JM, Iwata M, et al. mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science. 2010;329(5994):959–64. https://doi.org/10.1126/science.1190287.
Clarke M, Razmjou S, Prowse N, Dwyer Z, Litteljohn D, Pentz R, et al. Ketamine modulates hippocampal neurogenesis and pro-inflammatory cytokines but not stressor induced neurochemical changes. Neuropharmacology. 2017;112(Pt A):210–20.
Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018;23(4):801–11.
Moghaddam B, Adams B, Verma A, Daly D. Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci. 1997;17(8):2921–7.
Rabiner EA. Imaging of striatal dopamine release elicited with NMDA antagonists: is there anything there to be seen? J Psychopharmacol. 2007;21(3):253–8.
Abdallah CG, Averill LA, Collins KA, Geha P, Schwartz J, Averill C, et al. Ketamine treatment and global brain connectivity in major depression. Neuropsychopharmacology. 2017;42(6):1210–9. https://doi.org/10.1038/npp.2016.186.
Norbury A, Rutter SB, Collins AB, Costi S, Jha MK, Horn SR, et al. Neuroimaging correlates and predictors of response to repeated-dose intravenous ketamine in PTSD: preliminary evidence. Neuropsychopharmacology. 2021;46(13):2266–77. https://doi.org/10.1038/s41386-021-01104-4.
Zheng W, Zhou YL, Liu WJ, Wang CY, Zhan YN, Li HQ, et al. Neurocognitive performance and repeated-dose intravenous ketamine in major depressive disorder. J Affect Disord. 2019;246:241–7. https://doi.org/10.1016/j.jad.2018.12.005.
Wilkinson ST, Wright D, Fasula MK, Fenton L, Griepp M, Ostroff RB, et al. Cognitive behavior therapy may sustain antidepressant effects of intravenous ketamine in treatment-resistant depression. Psychother Psychosom. 2017;86(3):162–7. https://doi.org/10.1159/000457960.
Shiroma PR, Thuras P, Wels J, Erbes C, Kehle-Forbes S, Polusny M. A proof-of-concept study of subanesthetic intravenous ketamine combined with prolonged exposure therapy among veterans with posttraumatic stress disorder. J Clin Psychiatry. 2020;81(6):20113406. https://doi.org/10.4088/JCP.20113406.
Ben-Zion Z, Fine NB, Keynan NJ, Admon R, Green N, Halevi M, et al. Cognitive flexibility predicts PTSD symptoms: observational and interventional studies. Front Psychiatry. 2018;9:477. https://doi.org/10.3389/fpsyt.2018.00477.
Reiff CM, Richman EE, Nemeroff CB, Carpenter LL, Widge AS, Rodriguez CI, et al. Psychedelics and psychedelic-assisted psychotherapy. Am J Psychiatry. 2020;177(5):391–410. https://doi.org/10.1176/appi.ajp.2019.19010035.
Dumont GJ, Sweep FC, van der Steen R, Hermsen R, Donders AR, Touw DJ, et al. Increased oxytocin concentrations and prosocial feelings in humans after ecstasy (3,4-methylenedioxymethamphetamine) administration. Soc Neurosci. 2009;4(4):359–66. https://doi.org/10.1080/17470910802649470.
Dumont GJ, van Hasselt JG, de Kam M, van Gerven JM, Touw DJ, Buitelaar JK, et al. Acute psychomotor, memory and subjective effects of MDMA and THC co-administration over time in healthy volunteers. J Psychopharmacol. 2011;25(4):478–89. https://doi.org/10.1177/0269881110376687.
Hasler F, Studerus E, Lindner K, Ludewig S, Vollenweider FX. Investigation of serotonin-1A receptor function in the human psychopharmacology of MDMA. J Psychopharmacol. 2009;23(8):923–35. https://doi.org/10.1177/0269881108094650.
Schmidt A, Muller F, Dolder PC, Schmid Y, Zanchi D, Liechti ME, et al. Comparative effects of methylphenidate, modafinil, and MDMA on response inhibition neural networks in healthy subjects. Int J Neuropsychopharmacol. 2017;20(9):712–20. https://doi.org/10.1093/ijnp/pyx037.
Gamma A, Buck A, Berthold T, Liechti ME, Vollenweider FX. 3,4-Methylenedioxymethamphetamine (MDMA) modulates cortical and limbic brain activity as measured by [H(2)(15)O]-PET in healthy humans. Neuropsychopharmacology. 2000;23(4):388–95. https://doi.org/10.1016/S0893-133X(00)00130-5 (Erratum in: Neuropsychopharmacology 2000;23(5):following 598. Hell, D [corrected to Liechti, ME]).
Agurto C, Cecchi GA, Norel R, Ostrand R, Kirkpatrick M, Baggott MJ, et al. Detection of acute 3,4-methylenedioxymethamphetamine (MDMA) effects across protocols using automated natural language processing. Neuropsychopharmacology. 2020;45(5):823–32. https://doi.org/10.1038/s41386-020-0620-4.
Pantoni MM, Anagnostaras SG. Cognitive effects of MDMA in laboratory animals: a systematic review focusing on dose. Pharmacol Rev. 2019;71(3):413–49. https://doi.org/10.1124/pr.118.017087 (Erratum in: Pharmacol Rev. 2021 Apr;73(2):729).
Doss MK, Povazan M, Rosenberg MD, Sepeda ND, Davis AK, Finan PH, et al. Psilocybin therapy increases cognitive and neural flexibility in patients with major depressive disorder. Transl Psychiatry. 2021;11(1):574. https://doi.org/10.1038/s41398-021-01706-y.
Chun MM, Turk-Browne NB. Interactions between attention and memory. Curr Opin Neurobiol. 2007;17(2):177–84. https://doi.org/10.1016/j.conb.2007.03.005.
Koyama AK, Hagan KA, Okereke OI, Weisskopf MG, Rosner B, Grodstein F. Evaluation of a self-administered computerized cognitive battery in an older population. Neuroepidemiology. 2015;45(4):264–72. https://doi.org/10.1159/000439592.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by U.S. Department of Veterans Affairs Clinical Sciences Research and Development Merit Review Award (grant I01 CX001803 to Dr Shiroma). The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflicts of interest
The authors report no financial relationships with commercial interests.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
PRS and MRV-S contributed to conception and design of the review and writing of the manuscript. PRS, MRV-S, and YV provided critical review of the work and final approval of manuscript.
Rights and permissions
About this article
Cite this article
Shiroma, P.R., Velit-Salazar, M.R. & Vorobyov, Y. A Systematic Review of Neurocognitive Effects of Subanesthetic Doses of Intravenous Ketamine in Major Depressive Disorder, Post-Traumatic Stress Disorder, and Healthy Population. Clin Drug Investig 42, 549–566 (2022). https://doi.org/10.1007/s40261-022-01169-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-022-01169-z