Abstract
Background and Objective
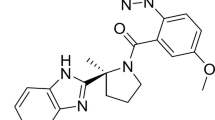
Daridorexant is a new dual orexin receptor antagonist currently in late-stage clinical development for the treatment of insomnia. This randomized, double-blind, placebo-controlled, four-period crossover study investigated the effect of daridorexant at a therapeutic and supratherapeutic dose on QT interval duration.
Methods
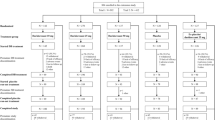
Thirty-six healthy subjects received single oral doses of daridorexant (50 mg; 200 mg), moxifloxacin (400 mg; open label), and placebo. All treatments were administered at bedtime to mimic therapeutic practice. The primary analysis was based on linear mixed-effects concentration-QT modelling. Triplicate ECG data were extracted from Holter recordings at baseline and until 24 h post dosing at time points matching those for pharmacokinetic sampling. Plasma concentrations of daridorexant were determined over 24 h.
Results
Assay sensitivity was demonstrated based on mean baseline- and placebo-corrected QT interval using Fridericia’s formula (ΔΔQTcF) > 5 ms following moxifloxacin administration (p < 0.01). Following daridorexant administration, mean (90% confidence interval, CI) ΔΔQTcF was 1.40 ms (0.48; 2.32 ms) and 1.84 ms (−0.12; 3.79 ms) at the Cmax of 747 ng/mL (50 mg dose) and 1809 ng/mL (200 mg dose), respectively, i.e., the upper bounds of the CIs were < 10 ms defined as threshold of regulatory concern. Lack of relevant QT prolongation was confirmed by secondary by-time point analysis and absence of relevant findings in the categorical outlier analysis. Daridorexant was safe and well tolerated and its pharmacokinetics were consistent with previous data.
Conclusion
Daridorexant does not impair cardiac repolarization evidenced by absence of relevant QT prolongation at therapeutic and supratherapeutic doses.
Clinical Trials Registration ID: NCT04250506.




Similar content being viewed by others
References
Reynolds CF, O’Hara R. DSM-5 sleep-wake disorders classification: overview for use in clinical practice. Am J Psychiatry. 2013;170(10):1099–101.
Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5 Suppl):S7-10.
Krystal AD, Prather AA, Ashbrook LH. The assessment and management of insomnia: an update. World Psychiatry. 2019;18(3):337–52.
Herring WJ, Roth T, Krystal AD, Michelson D. Orexin receptor antagonists for the treatment of insomnia and potential treatment of other neuropsychiatric indications. J Sleep Res. 2019;28(2):12782.
Sakurai T. The neural circuit of orexin (hypocretin): maintaining sleep and wakefulness. Nat Rev Neurosci. 2007;8(3):171–81.
Dauvilliers Y, Zammit G, Fietze I, Mayleben D, Seboek Kinter D, Pain S, Daridorexant HJ. a new dual orexin receptor antagonist to treat insomnia disorder. Ann Neurol. 2020;87(3):347–56.
Muehlan C, Vaillant C, Zenklusen I, Kraehenbuehl S, Dingemanse J. Clinical pharmacology, efficacy, and safety of orexin receptor antagonists for the treatment of insomnia disorders. Expert Opin Drug Metab Toxicol. 2020;16(11):1063–78.
Muehlan C, Heuberger J, Juif PE, Croft M, van Gerven J, Dingemanse J. Accelerated development of the dual orexin receptor antagonist ACT-541468: integration of a microtracer in a first-in-human study. Clin Pharmacol Ther. 2018;104(5):1022–9.
Boof ML, Alatrach A, Ufer M, Dingemanse J. Interaction potential of the dual orexin receptor antagonist ACT-541468 with CYP3A4 and food: results from two interaction studies. Eur J Clin Pharmacol. 2019;75(2):195–205.
Muehlan C, Fischer H, Zimmer D, Aissaoui H, Grimont J, Boss C, Croft M, van Gerven J, Krahenbuhl S, Dingemanse J. Metabolism of the dual orexin receptor antagonist ACT-541468, based on microtracer/accelerator mass spectrometry. Curr Drug Metab. 2019;20(4):254–65.
Gehin M, Wierdak J, Lemoine V, Sidharta PN, Dingemanse J. Effect of increased gastric pH and of a moderate CYP3A4 inducer on the pharmacokinetics of daridorexant, a dual orexin receptor antagonist. Annual Meeting Am Coll Clin Pharmacol. 2021 (abstract 28)
Stockbridge N, Morganroth J, Shah RR, Garnett C. Dealing with global safety issues: was the response to QT-liability of non-cardiac drugs well coordinated? Drug Saf. 2013;36(3):167–82.
Food and Drug Administration Center for Drug Evaluation and Research. Guidance for industry E14 clinical evaluation of QT/QTc interval prolongation and proarrythmic potential for non-antiarrhythmic drugs—questions and answers (R3). 2017. https://www.fda.gov/media/71379/download
Shah RR, Stonier PD. Withdrawal of prenylamine: perspectives on pharmacological, clinical and regulatory outcomes following the first QT-related casualty. Ther Adv Drug Saf. 2018;9(8):475–93.
Garnett C, Bonate PL, Dang Q, Ferber G, Huang D, Liu J, Mehrotra D, Riley S, Sager P, Tornoe C, Wang Y. Scientific white paper on concentration-QTc modeling. J Pharmacokinet Pharmacodyn. 2018;45(3):383–97.
Mueller MS, Sidharta PN, Voors-Pette C, Darpo B, Xue H, Dingemanse J. The effect of the glucosylceramide synthase inhibitor lucerastat on cardiac repolarization: results from a thorough QT study in healthy subjects. Orphanet J Rare Dis. 2020;15(1):303.
Murphy PJ, Yasuda S, Nakai K, Yoshinaga T, Hall N, Zhou M, Aluri J, Rege B, Moline M, Ferry J, Darpo B. Concentration-response modeling of ECG data from early-phase clinical studies as an alternative clinical and regulatory approach to assessing QT risk—experience from the development program of lemborexant. J Clin Pharmacol. 2017;57(1):96–104.
Fridericia LS. The duration of systole in an electrocardiogram in normal humans and in patients with heart disease 1920. Ann Noninvasive Electrocardiol. 2003;8(4):343–51.
Juif PE, Dingemanse J, Voors-Pette C, Ufer M. Association between vomiting and QT hysteresis: data from a TQT study with the endothelin a receptor antagonist clazosentan. Aaps J. 2020;22(5):103.
Upton RN, Mould DR. Basic concepts in population modeling, simulation, and model-based drug development: part 3-introduction to pharmacodynamic modeling methods. CPT Pharmacometrics Syst Pharmacol. 2014;3:e88.
Ferber G. Correcting QT for heart rate when both are affected by a drug. Drug Saf. 2019;42(3):335–7.
Malik M, Garnett C, Hnatkova K, Vicente J, Johannesen L, Stockbridge N. Implications of individual QT/RR profiles-part 1: inaccuracies and problems of population-specific QT/heart rate corrections. Drug Saf. 2019;42(3):401–14.
Malik M, Garnett C, Hnatkova K, Vicente J, Johannesen L, Stockbridge N. Implications of individual QT/RR profiles-part 2: zero QTc/RR correlations do not prove QTc correction accuracy in studies of QTc changes. Drug Saf. 2019;42(3):415–26.
Taubel J, Ferber G, Fernandes S, Camm AJ. Diurnal profile of the QTc interval following moxifloxacin administration. J Clin Pharmacol. 2019;59(1):35–44.
Ballesta A, Innominato PF, Dallmann R, Rand DA, Levi FA. Systems chronotherapeutics. Pharmacol Rev. 2017;69(2):161–99.
Gaspar LS, Alvaro AR, Carmo-Silva S, Mendes AF, Relogio A, Cavadas C. The importance of determining circadian parameters in pharmacological studies. Br J Pharmacol. 2019;176(16):2827–47.
Musiek ES, Fitzgerald GA. Molecular clocks in pharmacology. Handb Exp Pharmacol. 2013;217:243–60.
Taubel J, Ferber G, Lorch U, Batchvarov V, Savelieva I, Camm AJ. Thorough QT study of the effect of oral moxifloxacin on QTc interval in the fed and fasted state in healthy Japanese and Caucasian subjects. Br J Clin Pharmacol. 2014;77(1):170–9.
Hoever P, de Haas SL, Dorffner G, Chiossi E, van Gerven JM, Dingemanse J. Orexin receptor antagonism: an ascending multiple-dose study with almorexant. J Psychopharmacol. 2012;26(8):1071–80.
Treiber A, de Kanter R, Roch C, Gatfield J, Boss C, von Raumer M, Schindelholz B, Muehlan C, van Gerven J, Jenck F. The use of physiology-based pharmacokinetic and pharmacodynamic modeling in the discovery of the dual orexin receptor antagonist ACT-541468. J Pharmacol Exp Ther. 2017;362(3):489–503.
Muehlan C, Zuiker R, Peeters P, Rowles R, Dingemanse J. Pharmacokinetics and pharmacodynamics of the dual orexin receptor antagonist daridorexant in japanese and caucasian subjects. J Clin Psychopharmacol. 2020;40(2):157–66.
Bouvy JC, Koopmanschap MA, Shah RR, Schellekens H. The cost-effectiveness of drug regulation: the example of thorough QT/QTc studies. Clin Pharmacol Ther. 2012;91:281–8.
Wiśniowska B, Tylutki Z, Polak S. Thorough QT (TQT) studies: concordance with torsadogenesis and an evolving cardiac safety testing paradigm. Drug Discov Today. 2017;22:1460–5.
Gintant G, Sager PT, Stockbridge N. Evolution of strategies to improve preclinical cardiac safety testing. Nat Rev Drug Discov. 2016;15:457–71.
Strauss DG, Wu WW, Li Z, Koerner J, Garnett C. Translational models and tools to reduce clinical trials and improve regulatory decision making for QTc and proarrhythmia risk (ICH E14/S7B Updates). Clin Pharmacol Ther. 2021;109:319–33.
Muehlan C, Brooks S, Zuiker R, van Gerven J, Dingemanse J. Multiple-dose clinical pharmacology of ACT-541468, a novel dual orexin receptor antagonist, following repeated-dose morning and evening administration. Eur Neuropsychopharmacol. 2019;29(7):847–57.
Zammit G, Seboek Kinter D, Bassetti C, Leger D, Hermann V, Pain S, Roth T. Daridorexant (ACT-541468), a dual orexin receptor antagonist for the treatment of insomnia disorder: double-blind, randomized, phase 3 studies for efficacy and safety in adult and elderly patients. Sleep. 2020;43(Suppl1):A199–200.
Acknowledgements
The authors thank Dr. Jiří Liška and Dr. Luboš Janů (CEPHA s.r.o., Pilsen, Czech Republic) for the clinical conduct of the study, Dr. Susanne Globig and Giancarlo Sabattini (Department of Preclinical Pharmacokinetics and Metabolism, Idorsia Pharmaceuticals Ltd) for the bioanalytical analysis, Dr. Eric Ertel (Department of Pharmacology, Cardiovascular and Pulmonary, Idorsia Pharmaceuticals Ltd) for the preclinical studies, Biotrial (Rennes, France) for the Holter ECG extraction and reading, Kristyna Horakova and Kateřina Mertlíková (Aixial s.r.o., Brno, Czech Republic) for study monitoring, and Martin Wojcik (Department of Clinical Pharmacology, Idorsia Pharmaceuticals Ltd) for study project management.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by Idorsia Pharmaceuticals Ltd, Allschwil, Switzerland.
Conflict of interest
All authors were employees and/or shareholders of Idorsia Pharmaceuticals Ltd at the time the research was performed. Daridorexant is currently in clinical development by Idorsia Pharmaceuticals Ltd, Allschwil, Switzerland.
Availability of data and material
This study was registered on clinicaltrials.gov (NCT04250506). Data are available upon request from the corresponding author.
Ethics approval
The study protocol was approved by the Czech health authority (SUKL) as well as an Independent Ethics Committee (Ethics Committee of CEPHA s.r.o., Pilsen, Czech Republic). It was conducted in full accordance with the principles of the Declaration of Helsinki and ICH good clinical practice guidelines.
Consent to participate
Each study subject provided written informed consent prior to any treatment and study-related assessment.
Author contributions
US, CM, JD, and MU designed the study. AH and AK performed the concentration-QT modeling. US analyzed the data and drafted the manuscript. All authors reviewed the manuscript and approved its submission.
Consent for publication
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schilling, U., Henrich, A., Muehlan, C. et al. Impact of Daridorexant, a Dual Orexin Receptor Antagonist, on Cardiac Repolarization Following Bedtime Dosing: Results from a Thorough QT Study Using Concentration-QT Analysis. Clin Drug Investig 41, 711–721 (2021). https://doi.org/10.1007/s40261-021-01062-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-021-01062-1