Abstract
Background
We evaluated the potential for QT/corrected QT (QTc) interval prolongation after sugammadex given with propofol or sevoflurane anaesthesia.
Methods
This was a two-factorial, randomized, parallel-group study in 132 healthy subjects. Anaesthesia was maintained with sevoflurane or propofol. At ~20 min following sevoflurane/propofol initiation, sugammadex 4 mg/kg or placebo was administered. Neuromuscular blocking agents were not administered. Electrocardiograms were recorded regularly. The primary variable was the time-matched mean difference in the Fridericia-corrected QT interval (QTcF) change from baseline for sugammadex versus placebo when combined with propofol or sevoflurane. No relevant QTcF prolongation was concluded if the upper one-sided 95 % confidence interval (CI) was below the 10 ms margin of regulatory non-inferiority, up to 30 min post-study drug. Blood samples were taken for pharmacokinetic analysis. An exploratory analysis evaluated potential QT/QTc effects of neostigmine 50 μg/kg/glycopyrrolate 10 μg/kg in combination with propofol.
Results
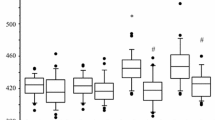
The estimated mean QTcF differences between sugammadex and placebo ranged from −2.4 to 0.6 ms when combined with either anaesthetic. The largest upper one-sided 95 % CI for the mean QTcF difference between sugammadex and placebo was 2 ms, occurring 2 min post-dosing. Propofol and sevoflurane resulted in mean QTcF increases exceeding 10 and 30 ms, respectively. On top of these prolongations, the effect of sugammadex was negligible at all timepoints. The mean peak sugammadex concentration was 66.5 μg/mL, with exposure similar in the sevoflurane/propofol groups. The mean QTcF changes from baseline following neostigmine/glycopyrrolate in 10 healthy subjects ranged between −1.4 and 3.6 ms.
Conclusion
Sugammadex 4 mg/kg does not cause clinically relevant QTc interval prolongation versus placebo when combined with propofol or sevoflurane.




Similar content being viewed by others
References
Adam JM, Bennett DJ, Bom A, et al. Cyclodextrin-derived host molecules as reversal agents for the neuromuscular blocker rocuronium bromide: synthesis and structure–activity relationships. J Med Chem. 2002;45:1806–16.
Bom A, Bradley M, Cameron K, et al. A novel concept of reversing neuromuscular block: chemical encapsulation of rocuronium bromide by a cyclodextrin-based synthetic host. Angew Chem Int Ed Engl. 2002;41:266–70.
Bom A, Epemolu O, Hope F, et al. Selective relaxant binding agents for reversal of neuromuscular blockade. Curr Opin Pharmacol. 2007;7:298–302.
Jones RK, Caldwell JE, Brull SJ, Soto RG. Reversal of profound rocuronium-induced blockade with sugammadex: a randomized comparison with neostigmine. Anesthesiology. 2008;109:816–24.
Blobner M, Eriksson LI, Scholz J, et al. Reversal of rocuronium-induced neuromuscular blockade with sugammadex compared with neostigmine during sevoflurane anaesthesia: results of a randomised, controlled trial. Eur J Anaesthesiol. 2010;27:874–81.
Khuenl-Brady KS, Wattwil M, Vanacker BF, et al. Sugammadex provides faster reversal of vecuronium-induced neuromuscular blockade compared with neostigmine: a multicenter, randomized, controlled trial. Anesth Analg. 2010;110:64–73.
Lemmens HJ, El-Orbany MI, Berry J, et al. Reversal of profound vecuronium-induced neuromuscular block under sevoflurane anesthesia: sugammadex versus neostigmine. BMC Anesthesiol. 2010;10:15.
Saarnivaara L, Klemola UM, Lindgren L, et al. QT interval of the ECG, heart rate and arterial pressure using propofol, methohexital or midazolam for induction of anaesthesia. Acta Anaesthesiol Scand. 1990;34:276–81.
Kleinsasser A, Kuenszberg E, Loeckinger A, et al. Sevoflurane, but not propofol, significantly prolongs the Q-T interval. Anesth Analg. 2000;90:25–7.
Chang DJ, Kweon TD, Nam SB, et al. Effects of fentanyl pretreatment on the QTc interval during propofol induction. Anaesthesia. 2008;63:1056–60.
Paventi S, Santevecchi A, Ranieri R. Effects of sevoflurane versus propofol on QT interval. Minerva Anestesiol. 2001;67:637–40.
Yildirim H, Adanir T, Atay A, et al. The effects of sevoflurane, isoflurane and desflurane on QT interval of the ECG. Eur J Anaesthesiol. 2004;21:566–70.
de Kam PJ, van Kuijk J, Prohn M, et al. Effects of sugammadex doses up to 32 mg/kg alone or in combination with rocuronium or vecuronium on QTc prolongation: a thorough QTc study. Clin Drug Investig. 2010;30:599–611.
de Kam PJ, van Kuijk J, Smeets J, et al. Sugammadex is not associated with QT/QTc prolongation: methodology aspects of an intravenous moxifloxacin-controlled thorough QT study. Int J Clin Pharmacol Ther. 2012;50:595–604.
Schneider TW, Minto CF, Gambus PL, et al. The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology. 1998;88:1170–82.
Guidance for industry: E14 clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs. 2005. http://www.fda.gov/downloads/RegulatoryInformation/Guidances/ucm129357.pdf. Accessed January 2013.
Saarnivaara L, Simola M. Effects of four anticholinesterase-anticholinergic combinations and tracheal extubation on QTc interval of the ECG, heart rate and arterial pressure. Acta Anaesthesiol Scand. 1998;42:460–3.
Van den Broek L, Proost JH, Wierda JM, et al. Neuromuscular and cardiovascular effects of neostigmine and methyl-atropine administered at different degrees of rocuronium-induced neuromuscular block. Eur J Anaesthesiol. 1994;11:481–7.
van Vlymen JM, Parlow JL. The effects of reversal of neuromuscular blockade on autonomic control in the perioperative period. Anesth Analg. 1997;84:148–54.
Chiladakis J, Kalogeropoulos A, Arvanitis P, et al. Preferred QT correction formula for the assessment of drug-induced QT interval prolongation. J Cardiovasc Electrophysiol. 2010;21:905–13.
Lock G, Fialho GL, Castro DL, Almeida MCS. Electrocardiographic changes after neostigmine-atropine mixture. J Anesth Clinic Res. 2012;3:2.
Acknowledgments
Pieter-Jan de Kam and Justin Dennie are employees of Merck Sharp & Dohme Corp. (Whitehouse Station, NJ, USA). Peter Grobara, Marjan LF Jagt-Smook and Michiel W van den Heuvel are employees of MSD (Oss, The Netherlands). Employees of Merck Sharp & Dohme Corp. and MSD may potentially own stock and/or hold stock options in the company. Pierre AM Peeters and Rob JW Berg were formerly employees of MSD. Guy Cammu has received lecture fees from MSD and research grants for funded work on sugammadex from MSD. Pierre Peeters received stocks from MSD during his time of employment by them. Steven Ramael is an employee of SGS Life Science Services (Antwerp, Belgium), and his institution received funding for the current study from MSD. Medical writing support was provided by Melanie More of Prime Medica Ltd (Knutsford, Cheshire, UK). This assistance was funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc. (Whitehouse Station, NJ, USA). This study was funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc. (Whitehouse Station, NJ, USA). Support with ECG analysis was provided by Biomedical Systems [BMS] (St Louis, MO, USA), with logistical support from BMS in Brussels, Belgium. The design and conduct of the study, as well as the analysis of the study data and opinions, conclusions, and interpretation of the data, were the responsibility of the authors.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
de Kam, PJ., Grobara, P., Dennie, J. et al. Effect of Sugammadex on QT/QTc Interval Prolongation when Combined with QTc-Prolonging Sevoflurane or Propofol Anaesthesia. Clin Drug Investig 33, 545–551 (2013). https://doi.org/10.1007/s40261-013-0095-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-013-0095-8