Abstract
Major drug regulators have indicated in guidance their flexibility to accept some development data for biosimilars generated with reference product versions licensed outside their own jurisdictions, but most authorities require new bridging studies between these versions and the versions of them licensed locally. The costs of these studies are not trivial in absolute terms and, due to the multiplier effect of required repetition by each biosimilar sponsor, their collective costs are substantial. Yet versions of biologics licensed in different jurisdictions usually share the same development data, and any manufacturing changes between versions have been justified by a rigorous comparability process. The fact that a biosimilar is usually expected to be licensed in multiple jurisdictions, in each case as similar to the local reference product, confirms that minor analytical differences between versions of reference biologics are typically inconsequential for clinical outcomes and licensing. A greatly simplified basis for selecting a reference comparator, that does not require conducting new bridging studies, is proposed and justified based on the shared data of the reference product versions as well as the proof offered where biosimilars have already been approved. The relevance of this proposal to the interchangeability designation available in the US is discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Bridging studies between local and foreign versions of an originator biologic add significant costs to biosimilar development yet provide no patient benefit or scientific rigor for the local approval of the biosimilar. Moreover, new studies are at the discretion of local regulators, not legally required. |
The authors propose scientifically robust, simplified conditions for the selection of a comparator version of the originator for biosimilar development based upon its approval by a jurisdiction that has adopted International Conference on Harmonization (ICH) guidelines and the demonstrated reliability of the comparability approach to biologic product changes implemented thereunder. |
Comparisons of an approved biosimilar to the locally approved version of the originator are currently required to support an interchangeability designation in the US, based upon a theoretical risk of excess immunogenicity of undetermined significance following transitions between the reference product and the biosimilar. Given experience with comparability, and the accumulation of data on clinical transitions between biologics, revisiting core scientific and regulatory principles should permit the relaxation of this restriction, too. |
1 Introduction
The efficiency of the marketing authorization process for a new drug relies upon the balance between the degree of confidence in its clinical properties versus the time and resources required to establish those properties beyond doubt. Regulators assess the type and extent of all data available at the time of submission (the ‘totality of data’). Excessive regulatory demands for data prior to drug approvals can be seen as inconsistent with regulators’ mission to support public health [1].Footnote 1
Since the mid-2000s, regulators in major global jurisdictions have applied the same scientific and regulatory principles of reduced data burden as were applied earlier to generic drugs, to support abbreviated development pathways for the approval of biosimilars (albeit the regulatory acceptance of manufacturing changes to biologics based upon comparability was established earlierFootnote 2). The regulatory premise for both generic drugs and biosimilars is based on the scientific principle that molecules having the same, or closely similar, structures and analytical properties must have the same clinical properties. For biosimilars, the relative complexity of reference biologics led to the establishment of the concept of high similarity, established analytically, rather than chemical identity as is required for drugs. This principle has been used for many years to justify manufacturing changes to biologics, and has provided compelling experience that meaningful clinical differences do not result [2].Footnote 3
We recommend here that regulators, in jurisdictions in which new bridging studies between local and foreign versions of the reference product are required during biosimilar development, withdraw this requirement under specified circumstances. This would enable a single approved version of an originator biologic to act as a ‘global reference’ for all biosimilar development, saving unnecessary costs and avoiding the potentially unethical inclusion of participants in clinical studies.
2 Regulatory Requirements for Biosimilar Comparator Bridging Data
Biosimilars are close copies of specific, large, biologically produced therapeutic molecules, some or all of whose intellectual property protections have expired [3]. According to the European Medicines Agency (EMA), the active substances of a biosimilar and its reference product are “essentially the same” [4]. We shall refer to the locally licensed originator comparator for biosimilar development as the ‘reference biologic product’ (RBP), and the same product approved in other regulatory jurisdictions as ‘foreign approved comparators’ (FACs).
Clearly, if a sponsor has chosen to use an FAC, it must be shown to be ‘materially representative’ of the RBP; that is, that there are not necessarily no differences from the RBP (although this will be the case when there is common sourcing), but that there are no differences that would lead to a false conclusion, from comparisons of a biosimilar candidate to the FAC, that the candidate is, or is not, biosimilar to the RBP.
In most major jurisdictions, the use of an FAC for biosimilar development must be justified by the presentation of ‘bridging data’ to show that the FAC is comparable to the RBP (Table 1).
Regulatory guidance is local to each jurisdiction, even if elements of guidance from different jurisdictions are similar in practice. Similarities in guidance between jurisdictions result partly from a shared view of the relevant science, but also because collaborations between regulators are now routine and often subject to formal arrangements.Footnote 4 Paradoxically, the emulation of guidance on biosimilars between different jurisdictions has resulted in guidance from individual regulators that suggests that each biologic licensed locally is different, analytically and clinically, from the same originator product licensed in other jurisdictions.Footnote 5 Some jurisdictions accept the use of FACs without bridging studies, provided that the FAC used is adequately qualified in other ways. The fact that some regulators show flexibility, within the biosimilars paradigm, as to the requirement for bridging studies between an FAC and its locally licensed equivalent suggests that the requirement for bridging studies, in those jurisdictions that require them, is a matter of regulatory policy rather than of any essential scientific rigor.
The EMA was the first major authority to publish guidelines for the development of biosimilars, and is generally regarded as the leader in many aspects of their regulation. The guideline (see Table 1) from the European Union (EU) permits the use of an FAC, preferably licensed in a country that has adopted the guidelines of the International Conference on Harmonization (ICH) [4]. However, the guideline does not point out that the simplest and most obvious means for an Applicant to demonstrate that a non-EEA (European Economic Area) licensed comparator is representative of an EEA-licensed reference is usually by substantiating their shared development history and data.
In the US, the Food and Drug Administration’s (FDA) guidance appears to require bridging studies, and states that “As a scientific matter, the type of bridging data needed will always include data from analytical studies (e.g., structural and functional data) that directly compare all three products (i.e., the proposed biosimilar product, the US-licensed reference product, and the non-US-licensed comparator product), and is likely to also include bridging clinical PK and/or PD study data for all three products”. The statement that three-way comparative studies are required without exception (“always”) appears to preclude the possibility that the FDA might accept other evidence that the FAC is materially representative of its US-licensed version. However, elsewhere in the same guidance, the FDA states “A sponsor may submit publicly available information regarding the non-US-licensed comparator product to justify the extent of comparative data needed to establish a bridge to the US-licensed reference product”. This suggests that there may be situations when the FDA would not require the full panoply of bridging data.
3 Biosimilar Comparator Bridging Studies Unnecessarily Consume Time and Resources
The objective costs of conducting bridging studies of FACs and the RBP can be estimated in financial terms.
Although bridging studies may represent a small fraction of the total costs of a typical biosimilar development, they are not trivial in absolute terms. In practice, the sourcing of product batches of different ages from different markets for development purposes may present significant difficulties and incur costs that are multiples of the cost of the product for medical use in its local market. Given the extensive development of new and improved technologies for analytical characterization of biologics, the panel of analytical comparisons of the FAC and the RBP for each jurisdiction will typically comprise evaluations of 20–40 separate variables for multiple (typically, at least 7–10) batches of the RBP from each jurisdiction to be compared. In vivo nonclinical studies will require the acquisition, maintenance, and use of additional laboratory animals, perhaps including primates. Clinical comparisons (e.g., pharmacokinetic studies), which are often required, will necessitate the inclusion of an additional group (typically, 10–40 per study) of patients or volunteers. Not to be casually dismissed, the inclusion of human subjects in these studies of doubtful necessity is also ethically questionable as it exposes them to strictly avoidable and unnecessary risks.Footnote 6
Clearly, there is variability between the resources required by different biosimilar development programs, but we estimate the financial costs of comparator bridging studies for each jurisdiction to be within a range of several hundred thousand to 1–2 million US dollars, depending upon the requirement for clinical studies. Further, these same studies will be repeated independently by each sponsor who is developing a biosimilar for any given biologic, so that there is an important, often uncounted, multiplier for all costs. The inability of biosimilar sponsors to rely upon a single version of the reference product as globally representative leads to the gross inefficiency of the replication of the same data by each sponsor, along with multiplication of costs that will inevitably eventually be passed to the market.
4 Different Jurisdiction, Same Reference Biologic
Due to the functional sensitivity of biologics to the specific processes by which they are manufactured, innovative biologics are developed and first manufactured at a single facility. Per ICH guidelines, regulators require that pivotal clinical studies of new biologics are conducted with investigational material that is fully representative of the to-be-commercialized drug. Product from the first facility is used in the clinical studies that are conducted for registration in the first market, and the same clinical studies are included in the marketing applications to most other jurisdictions, either concurrently or subsequently. Table 2 illustrates this practice by showing that the same major clinical data were used for the authorizations of the representative biologics in multiple jurisdictions. Moreover, the product’s nonclinical, quality, and manufacturing data are also necessarily largely the same across multiple jurisdictions. When the commercial strategy in a particular jurisdiction requires a variation from the original data, complementary studies are conducted and included in the marketing application, but the core data remain the same as were submitted in the first market(s). While there are exceptions to this rule, and while the burden remains on the sponsor to make the case, this commonality of data can effectively vitiate the need for new bridging studies between product versions.
A common representation by some regulators and the innovator biologic industryFootnote 7 is that reference product bridging studies are necessary because differences in critical quality attributes (CQAs) between an FAC and an RBP might be introduced or exacerbated by manufacturing changes to either or both of them after their approvals in their respective jurisdictions. A related argument is that data from bridging studies promote realistic acceptance ranges for the biosimilar. A third argument is that bridging studies are necessary because comparison of biosimilar candidates to the local version of the innovator biologic is required by regulatory text. In our view, these positions generally do not bear examination.
As preamble, it should be clear that, even if small differences in CQAs, within their acceptance limits, were to be introduced, there is no associated clinical safety or effectiveness issue arising from choosing either the FAC or the RBP as a biosimilar comparator, because both of these products must remain true to the clinical profiles described in their marketing applicationsFootnote 8 [5]. In this sense, bridging studies are not necessary; while the careful comparison of CQAs is important in establishing the ‘high similarity’ of a biosimilar candidate to its comparator, there is no additional risk to patients from choosing the FAC or the RBP as comparator as both are approved with the expectation of the same clinical outcomes.
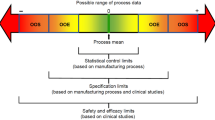
Manufacturing changes to biologics are always justified by data showing that the pre- and post-change products are comparable, as described in the ICH Q5E guideline [6]. While most changes are supported only by analytical comparability data,Footnote 9 occasionally regulators require nonclinical or clinical (pharmacokinetic or even safety and efficacy) comparability data. The huge collective experience with this approach has allowed individual biologics to maintain adequate consistency to remain on the market despite multiple manufacturing changes [2, 7]. While data from bridging studies demonstrate the analytical differences between the FAC and the RBP, their clinical properties, which are the ultimate ‘litmus test’ for accepting a biosimilar candidate as similar to its reference, are explicitly the same. Logically, therefore, these data in common between the FAC and the RBP are sufficient for bridging; no biosimilar candidate has failed to be approved just because the analytical data of the FAC and the RBP were discrepant if there were not also evident differences in their clinical profiles. Consequently, it is possible to define circumstances in which a manufacturing change to a biologic that is approved in one jurisdiction, based upon comparability data, can equally be accepted by the other jurisdictions applying the same guidelines, without a requirement for additional data. Because regulators in the different jurisdictions have similar technical experience and are applying the same principles of comparability (via shared guidelines [6]), and because the changed products in each of their jurisdictions have a common origin and share the same core data describing their structure and functions, the material representivity of the FAC for the RBP is preserved—any quality differences between the two product versions can be considered inconsequential as regards their use as comparators for biosimilar development. Indeed, any such differences simply broaden the ‘goal posts’ [8] (the design spaceFootnote 10) for the biosimilar.
Whether or not comparator bridging studies have been conducted, the inconsequentiality of any quality differences between the FAC and the RBP is confirmed unequivocally by the fact that biosimilars are routinely expected to be, and have been, approved as biosimilar to the local RBP in different jurisdictions (see Table 3). This closes the logical circle on the concept that, when a reference product satisfies the criteria that we propose (see below), the versions of it approved in different jurisdictions cannot be differentiated as reference comparators for biosimilar development. If this were not the case, sponsors would potentially have to develop and manufacture a product variant for each jurisdiction, which would completely deny the purpose of the biosimilars model. It can be concluded that, as a practical matter, it is generally redundant to conduct bridging studies of the FAC and the RBP—there is, effectively, only a single reference comparator approved globally.
As to the argument that bridging data are necessary to satisfy textual requirements to compare biosimilars to the local version of the originator’s product, we have justified above our position that the data in common between the FAC and the RBP are adequate for this purpose as a scientific matter. We note that regulators have very large discretion in such mattersFootnote 11; in the absence of a strong scientific basis for a requirement, there is ample precedent for regulators either waiving it or effecting a change in regulations or guidance.
5 A Proposal
Based upon the shared development history and data of many versions of individual biologics approved independently in different jurisdictions, and their consequent lack of significant differences as comparators for biosimilar development, we propose that regulators accept that a single reference version of the originator biologic may be selected for global biosimilar development if the following criteria are met, and that, as a consequence, bridging studies between the local reference and other versions of it approved in different jurisdictions will not be required:
-
The chosen reference has been approved in a jurisdiction that has formally adopted the guidelines of the ICH. This criterion ensures that any comparability studies that have been conducted to support manufacturing changes of the reference have been conducted according to an internationally accepted process and standard, and also that the reviewing authority is experienced in operating to this standard.
-
The formulation of the chosen reference has the same pharmaceutical form and route of administration as the RBP; the same content of active pharmaceutical ingredient (API) as a presentation of the RBP; and the same composition of excipients as the RBP; or, if the compositions of excipients in the products are different, there are data to show that the differences are without clinical effects.
-
There is substantial evidence in the public domain that the chosen reference and the RBP have been approved in their respective jurisdictions on the basis of essentially the same original data, including clinical safety and effectiveness data.
If regulators accept this proposal, we recommend that they amend their guidelines to clarify the circumstances under which bridging studies will, or will not, generally be required. Guidelines should not appear to require the performance of new bridging studies as the preferred or ‘default’ means of justifying the use of an FAC, but should expressly encourage compliance with simpler criteria for which the scientific basis is clear. In the absence of local regulatory guidelines reflecting the proposal, biosimilar sponsors may still choose to discuss our proposals, and specifically the applicability of all or any of the three criteria above, with regulators.
We recognize that there are a few biologics for which the reference bridging criteria above will not be appropriate, and that regulators will wish to evaluate the suitability of this approach on a case-by-case basis. However, we believe the approach is applicable to the majority of biologics, and that the adoption of the ‘global reference’ approach will significantly improve the efficiency of biosimilar development.
6 Interchangeability
The US is alone in demarcating an additional category of biosimilar products called ‘interchangeable biologics’. As defined in the biosimilars’ law [10], these are biosimilars that:
-
(a)
“can be expected to produce the same clinical result as the reference product in any given patient; and
-
(b)
for a biological product that is administered more than once to an individual, the risk in terms of safety or diminished efficacy of alternating or switching between use of the biological product and the reference product is not greater than the risk of using the reference product without such alternation or switch” [11].
In contrast, although they have no formal legal authority to designate biosimilars as interchangeable, in the sense of that term as applied in the US, European regulators are acknowledging extensive experience showing that clinical outcomes with biosimilars are the same as with their references, and going so far as to state “Our conclusion is that biosimilars licensed in the EU are interchangeable” [12].
Legally, biosimilars in the US are ‘highly similar’ to their reference products, whereas a designation of interchangeability by the FDA means that the Agency has determined that, subject to state law, it is safe for a pharmacist to substitute the interchangeable biologic for its reference biologic without the original prescriber’s knowledge. The question may be asked, if the originator product from a jurisdiction outside the US can act as the global comparator for biosimilar development, can it also act as the comparator in a study to support designation of a biosimilar as interchangeable?
The FDA’s initial guidance on this question stated: “At this time, as a scientific matter, it is unlikely that clinical comparisons with a non-US-licensed product would be an adequate basis to support the additional criteria required for a determination of interchangeability with the US-licensed reference product” [13]. In recent guidance, the FDA has continued to support this view, but has not excluded the possibility that the Agency might accept clinical data generated with an FAC [14]. Approval of a licensed biosimilar as interchangeable rests upon a demonstration that its clinical properties (safety and effectiveness) are not degraded by alternating its administration with that of its reference product, due to excess immunogenicity. The FDA already requires data from transition studies from the reference to the biosimilar for the initial approval of a biosimilar [15], so clinicians have evidence that biosimilars are safe and effective to use in patients who have received the reference product, but not vice versa.
The FDA has argued that, when a biologic or its biosimilar is dosed repeatedly, the human immune system can be sensitive to differences in molecular structure and conformation that cannot be discriminated reliably with current analytical methods [14]. On the other hand, it must be noted that an instance of excess immunogenicity at a population level triggered by switching between a ‘rigorously reviewed’Footnote 12 biologic and its ‘rigorously reviewed’ biosimilar has yet to be recorded, and it remains possible that the FDA’s concern is entirely theoretical. While it is true that “absence of evidence is not evidence of absence”, in the spirit of Eichler et al. [1], continued absence of evidence of immunogenicity triggered by switching should lead to a reevaluation of the evidence required to support applications for interchangeability designations, potentially resulting in a less burdensome requirements and a simpler application process. The other implications for the use of comparability data also have to be considered.
Consequently, we recommend that our proposal for selection of a reference comparator for the establishment of biosimilarity should not necessarily be used if the sponsor’s intention is also to use the resulting data for the establishment of interchangeability in the US, unless the chosen global reference is the US-licensed originator biologic, but neither should it be excluded a priori [16]. A careful choice may enable the data to be used to support marketing applications for the product as a biosimilar both in the US and in other jurisdictions, and to support an application for interchangeability designation in the US.
7 Conclusion
Our proposal is based upon the documented reliability of the comparability approach, as practiced in major regulatory jurisdictions, with its established sharing of development data for the approvals of versions of a biologic in different jurisdictions, as well as the routine approvals of the same biosimilars in multiple jurisdictions as similar to the local version of the originator. We have shown that new bridging studies between the local and foreign versions of the originator, in order to qualify the use of a foreign version as an FAC, are usually redundant. Instead, we have proposed a much simplified, but scientifically rigorous, basis for selection of a reference product that avoids the unjustified and replicated costs of these bridging studies for biosimilar sponsors.
That these studies are of questionable value is evident from the reality that each biosimilar is routinely expected to be, and is, approved in multiple jurisdictions as similar to the local version of the reference biologic that itself is a global product. Efficient regulation will also consider the effect of regulatory requirements as instruments of regulatory policy in the overall context of global public health. Many biologics have been transformative of the standard of clinical care for the conditions for which they are indicated, offering unprecedented relief to patients, but at high, and often unsustainable, cost. Biosimilars provide a potent means of reducing the cost of care, and add surety of supply. This opportunity is shared by all healthcare systems and, as such, all regulators share a mission to make pragmatic but scientifically justified and consistent choices about approval requirements in order to maximize biosimilars’ rapid development and availability to patients, even those outside their own jurisdictions. To quote Eichler et al. [1], “Good drug regulation is more than just minimizing risks; it is about maximizing gains in public health”. We contend that insistence by a jurisdiction on new bridging studies between FACs and an RBP, when available information supports the material representivity of the FAC for the RBP, is no less than the gratuitous application of a precautionary principle. It does not contribute whatsoever to the local patient’s experience, nor to scientific rigor, but does add substantial unnecessary development time and cost for biosimilar sponsors, particularly since the same data are required from each sponsor, and by multiple jurisdictions. As such, it is contrary to the very trust that societies vest in regulators.
Change history
02 August 2017
An erratum to this article has been published.
Notes
In the US, pressure on the FDA to revise its process for Compassionate Use applications and state Right-to-Try laws are clear evidence of a perception of regulatory delays compromising individual patients’ access to new medicines—see https://www.fda.gov/NewsEvents/PublicHealthFocus/ExpandedAccessCompassionateUse/default.htm and http://www.righttotry.org.
As represented by the FDA’s Guidance Concerning Demonstration of Comparability of Human Biological Products, Including Therapeutic Biotechnology-Derived Products (FDA, April, 1996) and equivalent guidelines in other jurisdictions (see https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm122879.htm).
Analytical ‘high similarity’ was already established as a regulatory matter by ICH Q5E, which evolved from the FDA’s comparability guidance of 1996 (see http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Quality/Q5E/Step4/Q5E_Guideline.pdf).
For example, several authorities have signed bilateral memoranda of understanding to discuss their evaluations of marketing applications and to collaborate on regulatory approaches. See also the International Pharmaceutical Regulators Forum at https://www.i-p-r-f.org.
For example, the adoption of EU guidelines by the Australian authority, and even the language of some US guidances is clearly adopted from the corresponding EU guidelines.
See ICH Guideline E6 on Good Clinical Practice: “A trial should be initiated and continued only if the anticipated benefits justify the risks”. http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R1_Guideline.pdf.
See, for example, public statements of industry groups on requirements for bridging studies in the US (https://www.bio.org/sites/default/files/2012-04-16%20Scientific%20Considerations%20-%20FINAL.pdf) and the EU (http://www.europabio.org/healthcare-biotech/publications/ema-strengthens-biosimilars-pathway-europe).
The only example of which we are aware when such a clinical difference emerged between versions of a biologic licensed in different jurisdictions was Eprex® (epoetin alfa). In the EU, there was an increase in immunogenicity of the product after a reformulation to remove human serum albumen, per new regulations, resulting in cases of pure red cell aplasia (PRCA). Documented by Casadevall et al. [9] (also, see http://www.ema.europa.eu/docs/en_GB/document_library/Presentation/2009/11/WC500011064.pdf). Note that the version of Eprex licensed in the EU would not have been accepted as an FAC to the US version under our proposed conditions for selecting a biosimilar development comparator.
Dr. Janet Woodcock, Deputy Commissioner and Chief Medical Officer, FDA testified before the US Congress House Committee on Oversight and Government Reform on ‘Follow-on Protein Products’, March 26, 2007 (testimony at https://www.fda.gov/NewsEvents/Testimony/ucm154070.htm). During the question-and-answer session, Dr Woodcock stated that, in the FDA’s experience, when biologics’ sponsors use a comparability approach to justify manufacturing changes to biologics, clinical data are required in not more than 1–2% of cases, if that.
ICH Q8, 9, 10, https://www.fda.gov/drugs/guidancecomplianceregulatoryinformation/guidances/ucm313087.htm and EMA/FDA Quality by Design approaches, https://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/UCM248526.pdf.
This is true even in the US where, while the biosimilars’ law requires that a biosimilar be shown to be similar to its locally licensed originator (that is, a product approved under Sect. 351(a) of the Public Health Service Act of 1942, as amended), it also expressly gives the FDA discretion to vary the information required to establish biosimilarity [See 42 USC 262(k)(2)(A)(ii)]. Therefore, there is no legal impediment to the Agency deciding that other information that establishes a bridge between an FAC and the RBP can replace data from new bridging studies.
‘Rigorously reviewed’ means that the product has been licensed based on a full complement of quality, nonclinical and clinical data per ICH guidelines, and reviewed by expert scientists.
References
Eichler H-G, Bloechl-Daum B, Brasseur D, Breckenridge A, Leufkens H, Raine J, Salmonsen T, Schneider CK, Rasi G. The risks of risk aversion in drug regulation. Nature Reviews Drug Discovery. 2013;1–10. published online 15 November 2013.
Vezér B, Buzás Z, Sebeszta M, Zrubka Z. Authorized manufacturing changes for therapeutic monoclonal antibodies (mAbs) in European Public Assessment Report (EPAR) documents. Curr Med Res Opin. 2016. doi:10.1185/03007995.2016.1145579.
Webster C, Copmann T, Garnick R, Green J, Hayes M, Landis J, Lubiniecki A, Murano G, Seamon K, Zezza D, Woollett G. Biologics: can there be abbreviated applications, generics, or follow-on products? BioPharm International. 2003. 28–37. http://www.biopharminternational.com/biologics-can-there-be-abbreviated-applications-generics-or-follow-products. Accessed 17 May 2017.
The International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH). http://www.ich.org. Accessed 17 May 2017.
Questions and Answers on Biosimilar Medicines, European Medicines Agency, 27 September 2012, EMA/837805/2011. 2012. http://www.ema.europa.eu/docs/en_GB/document_library/Medicine_QA/2009/12/WC500020062.pdf. Accessed 17 May 2017.
ICH Harmonised Tripartite Quality Guideline 5E (Q5E)—Comparability of biotechnological/biological products subject to changes in their manufacturing process at. http://www.ich.org/products/guidelines/quality/quality-single/article/comparability-of-biotechnologicalbiological-products-subject-to-changes-in-their-manufacturing-proc.html. Accessed 17 May 2017.
Schiestl M, Stangler T, Torella C, Cepeljnik T, Toll H, Grau R. Acceptable changes in quality attributes of glycosylated biopharmaceuticals. Nat Biotechnol. 2011;29(4):310–2.
McCamish M, Woollett G. Worldwide experience with biosimilar development. mAbs. 2011;3(2):209–217. http://www.tandfonline.com/doi/full/10.4161/mabs.3.2.15005. Accessed 17 May 2017.
Casadevall N, Eckardt K-U, Rossert J. Epoetin-induced autoimmune pure red cell aplasia. J Am Soc Nephrol. 2005;16(3):S67–S69. http://jasn.asnjournals.org/content/16/3_suppl_1/S67.long. Accessed 17 May 2017.
The Biologics Price Competition and Innovation Act of 2009 (BPCIA) is Title VII, Subtitle A of the Patient Protection and Affordable Care Act (PPACA) of 2010. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/UCM216146.pdf. Accessed 17 May 2017.
Title 42 of United States Code, Part 262 (k)(4)(A), (B).
Kurki P, van Aerts L, Wolff-Holz E, Giezen T, Skibeli V, Weise M. Interchangeability of biosimilars: a European perspective. BioDrugs. 2017. doi:10.1007/s40259-017-0210-0.
Draft Guidance for Industry: Biosimilars: Questions and Answers Regarding Implementation of the Biologics Price Competition and Innovation Act of 2009; FDA, February, 2012:8. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM444661.pdf. Finalized Apr 2015.
Draft Guidance for Industry: Considerations in Demonstrating Interchangeability With a Reference Product; FDA, January, 2017, p. 16. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM537135.pdf. Accessed 17 May 2017.
See transcripts of Advisory Committee meetings for etanercept (Erelzi®) and adalimumab (Amjevita®)— https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ArthritisAdvisoryCommittee/UCM518367.pdf and https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ArthritisAdvisoryCommittee/UCM520028.pd. Accessed 17 May 2017.
McCamish M, Pakulski J, Sattler C, Woollett G. Toward interchangeable biologics. Clin Pharmacol Ther. 2015;97:215–7. doi:10.1002/cpt.39.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received by the authors for writing this paper.
Conflict of interest
No conflicts of interest exist for Dr. Christopher Webster or for Dr. Gillian Woollett.
Additional information
The original version of this article was revised due to a retrospective Open Access order.
An erratum to this article is available at https://doi.org/10.1007/s40259-017-0236-3.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, a link is provided to the Creative Commons license and any changes made are indicated.
About this article
Cite this article
Webster, C.J., Woollett, G.R. A ‘Global Reference’ Comparator for Biosimilar Development. BioDrugs 31, 279–286 (2017). https://doi.org/10.1007/s40259-017-0227-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-017-0227-4