Abstract
Background
Biologic treatments for cancer continue to place a significant economic burden on healthcare stakeholders. Biosimilar therapies may help reduce this burden through cost savings, thereby increasing patient access.
Objectives
The purpose of this study was to collate all published data to assess the weight of available evidence (quantity and quality) for proposed monoclonal antibody biosimilars and intended copies, for the treatment of cancer.
Methods
MEDLINE®, Embase®, and ISI Web of Science® databases were searched to September 2015. Conference proceedings (17) were searched (2012 to July 2015). Searches of the United States National Library of Medicine ClinicalTrials.gov registry were also conducted. Risk of bias assessments were undertaken to assess data strength and validity.
Results
Proposed biosimilars were identified in 23 studies (36 publications) in oncology and ten studies in 14 publications in oncology and chronic inflammatory diseases for bevacizumab, rituximab, and trastuzumab originators. Based on our review of the included published studies, and as inferred from the conclusions of study authors, the identified proposed biosimilars exhibit close similarity to their originators. Published data were also retrieved on intended copies of rituximab. It remains unclear what role these agents may have, as publications on rigorous clinical studies are lacking for these molecules.
Conclusion
While biosimilar products have the potential to improve patient access to important biologic therapies, robust evidence of outcomes for monoclonal antibody biosimilars in treating cancer patients, including data from comparative efficacy and safety trials, is not yet available in the published literature. Significant data gaps exist, particularly for intended copies, which reinforces the need to maintain a clear differentiation between these molecules and true biosimilars. As more biosimilars become available for use, it will be important for stakeholders to understand fully the robustness of overall evidence used to demonstrate biosimilarity and gain regulatory approval.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Monoclonal antibody drugs account for a significant proportion of oncology spending in the USA and are associated with high out-of-pocket costs for patients. Biosimilar therapies have the potential to improve access to these specialist oncology drugs, but knowledge gaps may slow their adoption. |
The degree of biosimilarity is ultimately determined by regulatory authorities and is based on the totality of evidence, which includes data on molecular and functional characterization, other nonclinical data, and the safety, pharmacokinetic, immunogenicity, and efficacy clinical trial data. |
Based on this review of published nonclinical and clinical oncology studies, and as inferred from the conclusions of study authors, proposed biosimilars of bevacizumab, rituximab, and trastuzumab exhibit close similarity to their originators. |
However, at present, robust evidence of outcomes for monoclonal antibody biosimilars in cancer, including data from comparative efficacy and safety trials, is not yet widely available in the published literature. |
1 Introduction
The treatment of cancer continues to place a significant burden on healthcare systems, with the number of cancer cases continuing to rise due to an aging population. Improvements in cancer diagnosis and disease management are now extending survival, and consequently increasing the length of time patients remain on treatment. As a result, there is a need to control current levels of expenditure, which are unsustainable. IMS Health recently reported a snapshot of USA expenditure on cancer medicines:
-
Global spending on oncology and supportive care drugs reached $100 billion in 2014, with targeted therapy expenditures accounting for almost 50% of total spending [1].
-
Spending on oncology medicines in the USA increased 18.0% to $39.1 billion in 2015 [2].
-
The fastest-growing classes of oncology therapy are monoclonal antibodies (mAbs) and protein kinase inhibitors; mAbs account for 35% of oncology spending due to the introduction of new treatments [2].
-
USA sales figures in 2015 for two of the top 20 global products were $6.2 billion for bevacizumab and $5.6 billion for trastuzumab [3].
Given the economic burden of cancer treatments, healthcare systems around the world have devised a range of methods to try to contain these costs, often resulting in seemingly arbitrary access restrictions for patients. Patient access to oncology medicines has been shown to vary significantly even at the regional level [4].
A lack of consensus among healthcare professionals on the most reliable economic drug evaluation methods to employ has led to inconsistency in treatment guidelines. This was demonstrated in a 2015 systematic review by Park et al. that examined the cost-effectiveness of mAb-based orphan drugs [5]. Patient access and reimbursement decisions can vary greatly between regions as a consequence of the different evaluation methods employed by each agency [5].
In the USA, patient out-of-pocket costs for intravenous cancer drugs have increased substantially in recent years, in part due to the integration of small community-based practices into larger hospital systems [1]. Across publicly funded healthcare systems in Europe and other parts of the world, a lack of reimbursement also may limit access to effective oncology medicines, with reimbursement often contingent upon evidence of cost effectiveness.
Biosimilars are biologics that are highly similar to biologics already approved for the treatment of disease. The first biosimilar was authorized for use in the EU in 2006. A greater adoption of biosimilars may help to alleviate the substantial burden on healthcare systems by stimulating price competition and improving patient access to important treatments [6].
Regulatory frameworks for the development of biosimilars were first established by the European Medicines Agency (EMA), followed by the World Health Organization (WHO) and the USA Food and Drug Administration (FDA) [7]. These regulatory frameworks specify the requirements for approval of biosimilars, including important foundational analytical studies to compare the biosimilar with the approved biologic originator product. In addition, comparative nonclinical and clinical studies are required to assess toxicity and pharmacokinetics (PK)/pharmacodynamics (PD), and clinical studies are required to demonstrate an efficacy profile that is comparable to the originator, as well as comparable safety and immunogenicity profiles. Robust evidence of similarity provided from analytical, PK, and nonclinical studies form the foundation to demonstrate the comparability of a biosimilar to the originator and are required to meet regulatory standards and requirements for regulatory approval. It is also important to ensure that these data are made available in the public domain, to facilitate awareness and understanding of biosimilar treatments among physicians and other healthcare professionals.
Intended copies are copies of originator biologics that have not undergone rigorous comparative evaluations as stipulated by major regulatory agencies, but are nevertheless being commercialized by manufacturers in some countries. There is a lack of published information about the efficacy and safety of intended copies compared with the originator. Furthermore, these products may have clinically significant differences in formulation, dosages, efficacy, and safety [8].
A comprehensive systematic literature review (SLR) was undertaken in 2015 to identify, collate, and synthesize all published evidence on named biosimilars and intended copies of originator mAbs and fusion proteins [9]. The aim of that analysis was to summarize the quantity and quality of data available and the number and diversity of publications describing biosimilars for mAbs or fusion proteins across all indications (including chronic inflammatory diseases, oncology, cardiovascular and ophthalmology). Here, we explore the findings for biosimilars indicated for oncology disease in more detail.
2 Methods
2.1 Systematic Literature Review (SLR)
A detailed description of the methods used in this SLR can be found in the manuscript by Jacobs et al. [9].
MEDLINE®/Medline in process and Embase® (searched using the OVIDSP interface), and ISI Web of Science® were searched from database inception to September 3, 2015. The search was executed on April 27, 2015 and repeated on September 3, 2015 to capture more recent full-text publications. The search strategy consisted of the following: (1) terms that captured mAb and fusion protein terms; and (2) terms that included the different terminologies for biosimilar products, such as “biosimilars,” “subsequent entry biologics,” “follow-on biologics,” “follow-on proteins,” “biocomparables,” “biogenerics,” “similar biotherapeutic products,” and “intended copies,” or “biobetters” (which were analyzed separately). Included publications were required to contain both a “mAb” and/or “fusion protein” term and a “biosimilars” term. Proposed biosimilars were differentiated from intended copies, based on them meeting the established rigorous regulatory requirements for biosimilarity, as outlined by major regulatory health authorities such as the EMA, FDA, WHO, Pharmaceuticals Medical Devices Agency/Japan Ministry for Health Labor and Welfare, Health Canada or Korean Ministry of Food and Drug Safety (MFDS). Other markets have issued guidance on biosimilars, although the evaluation of the biosimilar approval pathways by regulatory authorities outside of the major markets is considered beyond the scope of this review. Controlled vocabulary and free-text terms were used, and the search results were filtered using the study designs of interest. Search results from each database were limited to references published in the English language.
In addition, a hand-search of relevant conference proceedings (17 conferences) was conducted for the period January 1, 2012 to July 31, 2015 in order to capture the latest studies not yet published as full-text articles and/or supplement results of previously published studies (Jacobs et al. [9]). Oncology-focused conference proceedings (n = 10) are shown in Supplementary Table S1 (see the electronic supplementary material, online resource 1). For the SLR analysis, conference proceedings of interest included disease-specific (i.e., for oncology), health economics and outcomes research, regulatory-/payer-focused, and manufacturing-/development-themed meetings. In order to identify biosimilars in development that did not appear in the published literature or in the identified congresses, searches were also conducted (on September 21, 2015) using the USA National Library of Medicine ClinicalTrials.gov registry. Hand-screening was used to identify relevant records because of the limited extent of the searches available for ClinicalTrials.gov.
2.2 Components of the SLR
This SLR had two components: the empirical analysis, which focused on peer-reviewed publications of analytical, nonclinical, clinical, pharmacovigilance, and observational empirical data; and the non-empirical analysis, which included opinion pieces or commentaries, publications describing product-related patient support programs, and those on manufacturing and supply issues, which were further classified into general thematic categories to summarize key topics being published on biosimilars. These two components were included to assess the diversity and extent of these types of publications, as well as to identify emergent themes and knowledge gaps in the published literature. Empirical studies were categorized by type into one of the following areas: “human” studies subdivided as randomized controlled trials (RCTs), observational/post-marketing studies, and health economic studies; nonclinical (in vitro/in vivo) studies; and analytical studies. Non-empirical publications were classified into one of the following categories: manufacturing or supply topics and themes, review articles, opinion pieces or commentaries, regulatory-/policy-related content, published descriptions of product-related patient support programs, and any other non-empirical publication type relevant to biosimilars meeting the inclusion criteria.
2.3 Risk of Bias (Quality) Assessment
A risk of bias assessment was undertaken for each classified study (i.e., RCTs, observational studies, studies published in conference proceedings, and animal studies) using a validated tool matched to study type to assess the strength/validity of the empirical data and in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [10, 11]. In cases where multiple publications were retrieved for the same study, quality assessments were only conducted on the first original publication or first full-text publication. The quality of RCTs was assessed using the National Institute for Health and Care Excellence (NICE) single technology appraisal (STA) manufacturer’s template [12] and the Jadad scoring system [13] (Supplementary Table S2; Supplementary Fig. S1).
Non-randomized studies were assessed using the Downs and Black instrument [14] (Supplementary Table S3). The Downs and Black instrument was modified to include only the most critical qualifying parameters (12 of 26) for quality assessment of conference proceeding abstracts (Supplementary Table S4). Detailed parameters related to process were excluded as these data were not available in abstract formats, e.g., suitability of statistical method employed. Animal studies were assessed using SYRCLE’s risk of bias tool [15]. Conference abstracts of analytical/nonclinical studies were not evaluated, as suitable tools were not available at the time of analysis. Analytical and cell-based studies published full-text were also not evaluated for the same reason.
3 Results
3.1 Literature and Conference Search
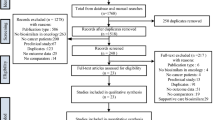
A total of 768 publications relevant to the topic of biosimilars were retained from a total of 1991 publications identified through a title and abstract screen. Of the 768 references, 147 (19%) reported mAb biosimilars for use in oncology. The number of publications included in the analysis is shown in Supplementary Fig. S2. Where encore (or duplicate) publications were retrieved for studies, the information was compared with the original (first published article) and excluded if no additional data were provided. If new data were identified, encore publications were included along with the original publication. However, this did not affect the overall study count. In some instances, a biosimilar was indicated for multiple disorders or diseases. For example, rituximab biosimilar publications were reported for both the oncology and inflammatory disorders categories, where relevant, as rituximab is indicated for both therapeutic areas. Proposed biosimilars or intended copies (i.e., where a unique identifier was provided) were identified in 23 studies (36 publications) in oncology and ten studies in 14 publications in oncology and chronic inflammatory diseases (Fig. 1). In this analysis, biosimilar trials were identified for the following indications: follicular lymphoma, diffuse large B-cell lymphoma (DLBCL), breast cancer (BC), and non-squamous non-small cell lung cancer (NSCLC).
3.2 Preclinical Data
3.2.1 Proposed Bevacizumab Biosimilars
Published preclinical studies of proposed bevacizumab biosimilars are presented in Table 1.
ABP 215 (Amgen) The functional similarity of ABP 215 compared with bevacizumab was assessed in vitro using human umbilical vein endothelial cells (HUVEC) and characterized using analytical methods [16–18]. Binding to vascular endothelial growth factor (VEGF) and VEGF isoforms, neonatal Fc receptor and FcgRIIa, inhibition of proliferation, and composition between the biosimilar and originator were similar.
Hutterer et al. investigated the structural similarity of ABP 215 compared with bevacizumab [19]. Based on results of structural assessment (including higher order structure, impurities, and stability), the authors concluded that ABP 215 was analytically highly similar to bevacizumab.
PF-06439535 (Pfizer) The functional similarity (biological activity or mode of action) of PF-06439535 and bevacizumab were assessed in vitro using cell-based assays [20, 21]. The results of these studies indicated that PF-06439535 was functionally similar to bevacizumab (in HUVEC and another unspecified cell line).
Peraza et al. evaluated the functional similarity of PF-06439535 and bevacizumab in cynomolgus monkeys [21]. The authors reported that PF-06439535 was well tolerated and displayed similar PK properties compared with bevacizumab. Anti-drug antibodies (ADAbs) were not detected.
The charge heterogeneity, post-translational modifications, and hydrodynamic size heterogeneity of PF-06439535 compared with bevacizumab were investigated using various biochemical analytical techniques [20]. The biochemical properties were also confirmed using complementary analyses. The authors reported that PF-06439535 displayed similar structural properties compared with bevacizumab.
Peraza et al. evaluated the analytical (structural) similarity of PF-06439535 compared with the originator [21]. The primary sequence of PF-06439535, bevacizumab-EU, and bevacizumab-USA was reported to be identical, as delineated by liquid chromatography (LC)/mass spectrometry (MS)/MS peptide mapping.
RPH-001 (Alphamab/R-Pharm) Archuadze et al. evaluated the PK profiles of RPH-001 and bevacizumab following a single intravenous administration at three different doses in cynomolgus monkeys [22]. The tested PK parameters were reported to be comparable between RPH-001 and bevacizumab, and neither drug was associated with any toxicity.
3.2.2 Proposed Rituximab Biosimilars
Published preclinical studies of proposed rituximab biosimilars are presented in Table 2.
1B8 (Center of Molecular Immunology) Dorvignit et al. evaluated the functional comparability between 1B8 and rituximab in human Burkitt’s lymphoma, Ramos, Daudi, and Raji cell lines [23]. Similar biological potency was reported [as measured by complement-dependent cytotoxicity (CDC), antibody-dependent cellular cytotoxicity (ADCC), and apoptosis assays].
GP2013 (Sandoz) The pharmacological comparability of GP2013 and the originator rituximab was assessed in a preclinical study of moderate quality (SYRCLE’s risk of bias tool) [24]. The authors reported similar in vitro ADCC potency when compared in a dose-response manner against two lymphoma cell lines using human natural killer (NK) cells [24]. In a separate analysis, in vivo efficacy was demonstrated in mouse xenograft models [25]. PK/PD (CD20 cell depletion) profiles were reportedly comparable based on analysis in cynomolgus monkeys [26].
Visser et al. reported in vitro functional bioequivalence between GP2013 and the originator rituximab in Raji B cells [27]. The Visser et al. study did not undergo quality assessment, because of the unavailability of suitable risk of bias assessment tools for this type of study.
Visser et al. [27] (not assessed) and da Silva et al. [24] (moderate quality using SYRCLE’s risk of bias tool) compared GP2013 with rituximab using combined analytical and characterization methods. Intact mass analysis of GP2013 revealed the same molecular mass to that of rituximab [24–26]. The primary sequence and higher order structure of GP2013 was reported by authors as indistinguishable from the originator. GP2013 and originator rituximab were comparable with regard to post-translational modifications, glycan pattern, purity, and aggregate levels.
PF-05280586 (Pfizer) A comparative nonclinical study of moderate quality (SYRCLE’s risk of bias tool) was conducted with PF-05280586 and rituximab-EU [28–30]. CDC assay results were reported to be similar. As part of the same study, the safety of PF-05280586 and rituximab was also evaluated in cynomolgus monkeys [28–30]. Both molecules were well tolerated at doses up to 20 mg/kg. There were no reported effects on food consumption, body weight, body weight gain, coagulation, urinalysis, or clinical chemistry parameters. No cardiac or ophthalmologic effects were observed in the repeat-dose study (not evaluated in the single-dose study). Emesis was noted in animals administered with either PF-05280586 or rituximab (PF-05280586 vs. control, n = 6 vs. 1; rituximab-EU vs. control, n = 7 vs. 2). The PK and PD profiles for both molecules were purportedly comparable.
Karnik et al. reported biological activity data (from in vitro cell-based assays, cell line unspecified) for PF-05280586 versus rituximab [31]. The reported biological activity was 93–114% for PF-05280586 versus 79–135% for rituximab (combined range for rituximab-EU and rituximab-USA). The Karnik et al. study did not undergo quality assessment, because of the unavailability of suitable risk of bias assessment tools for this type of study at the time of analysis.
As part of a comparative nonclinical assessment study evaluating PF-05280586 versus rituximab, the authors investigated the physicochemical similarity of both products using peptide mapping [reverse-phase (RP) high-performance LC (HPLC)] [28–30]. The identity of each peptide was confirmed by LC/MS using an ultra–high-resolution quadrupole time-of-flight MS. The chromatographic profiles of both products were reported as identical. The totality of the data (including a separate LC/MS analysis) confirmed identical primary sequences.
In a separate study, the primary sequence of PF-05280586 and rituximab were confirmed using proteolytic digests and peptide mapping via LC/MS/MS [31]. Structure, with respect to glycosylation profile and presence of high molecular mass species (0.5–0.7 vs. 0.9–1.6 for PF-05280586 and rituximab-EU/-USA, respectively), was reported as similar. Product purity, charge heterogeneity, post-translational modifications, and hydrodynamic size heterogeneity were reportedly undertaken (individual analyses not shown; Table 2).
RTXM83 (mAbxience) Seigelchifer et al. evaluated the functional comparability of RTXM83 and rituximab-EU in an unspecified cell line and in cynomolgus monkeys [32]. Similar biological potency was reported (as measured by CDC, ADCC, and apoptosis assays). The in vitro binding affinities to neonatal receptors were also described as similar. Data from the in vivo PK/PD study indicated that the area under the curve (AUC), half-life, and maximum serum concentration (C max) of RTXM83 were all within the prespecified 80–120% range of rituximab. The structural similarity between RTXM83 and rituximab was evaluated using mass fingerprinting and MS analysis, ultraviolet circular dichroism spectroscopy, glycan and charge variant analysis, sodium dodecyl sulfate-polyacrylamide gel electrophoresis analysis, and size-exclusion HPLC analysis [32]. The results reportedly indicated similar primary structures, comparable secondary and tertiary structures, and similarity in the extent of post-translational modifications. The level of purity was observed to be comparable between the proposed biosimilar and the originator.
3.2.3 Proposed Trastuzumab Biosimilars
Published preclinical studies of proposed trastuzumab biosimilars are presented in Table 3.
PF-0280014 (Pfizer) Boyle et al. evaluated the biological activity of PF-05280014 as part of a wider analytical characterization study [33]. The mode of action of PF-05280014 was compared with trastuzumab using in vitro cell-binding assays (methods and cell line not described or specified). The biological activity data indicated functional similarity to trastuzumab-USA or trastuzumab-EU. The statistical significance of the results was not reported. The binding kinetics to the ligand and Fc-gamma receptor III, involved in immune-effector functions, were also assessed (individual data not reported). This study did not undergo quality assessment, because no suitable risk of bias assessment tool was available at the time of analysis.
A nonclinical comparability study between PF-05280014 and trastuzumab was conducted using in vitro structural and functional analyses [tumor cell growth inhibition assay in the human epidermal growth factor receptor 2 (HER2) overexpression metastatic breast carcinoma cell line, SKBR-3, and CDC assay], and in vivo PK and immunogenicity assessments in male CD-1 mice [34–37]. Results of the in vitro assessments indicated functional similarity between PF-05280014 and trastuzumab. PK parameters [C max, AUC from time zero to infinity (AUC0–∞), clearance, and steady-state volume of distribution] in mice were reported to be similar and dose dependent. The incidence of ADAbs was reported to be low (~10%) and similar between PF-05280014 and trastuzumab across all dose levels tested. All animals survived to their terminal blood collection (up to 2880 h) with no mAb-related differences in clinical signs, mean body weight, or body weight change. The study by Hurst et al. was considered to be of moderate quality using SYRCLE’s risk of bias tool [34].
An analytical study published by Boyle et al. compared the structural and functional attributes of PF-05280014 with those of trastuzumab [33]. Peptide mapping via LC/MS/MS confirmed identical primary structures for both PF-05280014 versus the licensed products. Charge heterogeneity, major post-translational modifications, hydrodynamic size heterogeneity, and glycan quantification of PF-05280014 versus trastuzumab were evaluated using a combination of biochemical techniques, and all analyses were reported by authors as similar (individual data not reported). High molecular mass species ranged from 0.2–0.4 in the PF-05280014 sample versus 0.3–1.1 in the trastuzumab sample. This study did not undergo quality assessment, because no suitable risk of bias assessment tool was available at the time of analysis.
Hurst and colleagues evaluated the structural attributes of PF-05280014 as part of a wider nonclinical comparability PK/immunogenicity assessment in mice [34–37]. Using peptide mapping, the authors reported structural similarity, with detected peptides constituting ≥98% of the amino acid sequence of trastuzumab. The complete amino acid sequence was obtained from a separate LC/MS analysis at the subunit level, which confirmed structural similarity between PF-05280014 and trastuzumab at the primary sequence level. The study by Hurst et al. was considered to be of moderate quality using SYRCLE’s risk of bias tool [34].
3.3 Pharmacokinetic/Safety Data in Healthy Subjects
3.3.1 Proposed Bevacizumab Biosimilars
Published PK/safety studies of proposed bevacizumab biosimilars in healthy subjects are presented in Table 1.
ABP 215 (Amgen) The PK equivalence of ABP 215 (vs. bevacizumab-EU and bevacizumab-USA) was evaluated in healthy adult male subjects [16, 17]. The authors reported PK equivalence of ABP 215 compared with bevacizumab (within the prespecified equivalence criteria of 80–125%). Similar treatment-related adverse events (AEs) were reported for the ABP 215, bevacizumab-USA, and bevacizumab-EU groups; no subjects developed ADAbs. The study was considered to be of excellent quality.
3.3.2 Proposed Rituximab Biosimilars
No published PK/safety studies in healthy subjects have been reported for proposed biosimilars of rituximab. However, planned and completed PK/safety studies (with published data) have been identified for rituximab biosimilars in rheumatoid arthritis patients [38].
3.3.3 Proposed Trastuzumab Biosimilars
Published PK/safety studies of proposed trastuzumab biosimilars in healthy subjects are presented in Table 3.
FTMB (Allergan/Amgen) FTMB was evaluated and compared with trastuzumab or placebo in a dose-escalation/bioequivalence study in healthy male subjects (n = 118) [39, 40]. The authors reported bioequivalence of FTMB compared with trastuzumab [primary endpoint, AUC0–∞; ratio 0.89; 90% confidence interval (CI) 0.85–0.94]. Nonlinear, target-mediated PK were also observed. FTMB was reported to be well tolerated up to doses of 6.0 mg/kg, with no additional AEs occurring beyond those already documented for trastuzumab. The study was considered to be of excellent quality, as measured by the NICE STA and Jadad scoring tools.
PF-05280014 (Pfizer) The safety and PK properties of PF-05280014 were evaluated and compared with trastuzumab in a study involving 105 healthy male subjects [36, 41–44]. Reported AEs were comparable between treatments. However, the incidence of pyrexia was higher in the PF-05280014 arm [ten participants (28.6%); mild in all but one participant] versus the trastuzumab arms [two to three participants (5.7–8.6%)]. In the context of biosimilar development, a PK similarity study is not necessarily designed for a comparative assessment of safety. This observation appears to be due to chance and not to any inherent difference between PF-05280014 and trastuzumab [43]. Only one subject was ADAb positive (ADAb+) in the trastuzumab-EU group. The authors reported PK similarity between PF-05280014 and trastuzumab-EU and trastuzumab-USA, with a 90% CI of C max, time from 0 to the last time point with quantifiable concentration (AUC0–T), and AUC0–∞ within the prespecified range (80–125%) of PK equivalence. The study was of excellent quality as measured by the NICE STA; however, using the Jadad scoring tool, the study was considered to be only of good quality because the method of randomization and blinding was not described.
3.4 Clinical Evidence in Cancer Patients
3.4.1 Proposed Bevacizumab Biosimilars
Published clinical studies of proposed bevacizumab biosimilars in cancer patients are presented in Table 1.
BCD-021 (Biocad) The PK and safety of BCD-021 were assessed in a comparative trial involving 28 patients with non-squamous NSCLC (stage IIIb/IV) [45]. PK analysis revealed that 90% CIs for the ratio of geometric means of AUC from 0 to 504 h (AUC0–504h) of bevacizumab after single BCD-021 and bevacizumab administrations were 80.01–118.28%. The safety characteristics of BCD-021 and bevacizumab were considered equivalent by authors.
BCD-021 or bevacizumab in combination with paclitaxel and carboplatin was evaluated in a comparative safety/efficacy study in 138 patients with advanced non-squamous NSCLC (stage IIIb/IV) [46]. No statistically significant difference was observed between groups for overall response rate (ORR) as the primary endpoint and other efficacy endpoints [clinical remission (CR), partial remission (PR), stable disease, and progression rate]. The AE profiles of BCD-021 and bevacizumab were declared equivalent, with the majority of incident AEs reportedly associated with chemotherapy. Binding and neutralizing ADAbs were transient and detected only in one patient in each group. Both studies were of excellent quality.
3.4.2 Proposed Rituximab Biosimilars
Published clinical studies of proposed rituximab biosimilars in cancer patients are presented in Table 2.
BCD-020 (Biocad) BCD-020 was evaluated in a comparative safety/efficacy study in 92 patients with non-Hodgkin lymphoma (NHL) and compared with the parameters of rituximab. The study was considered to be of excellent quality [47–49]. ORR on day 50 ± 5 (primary endpoint) in both arms was reported as equivalent (p = 0.8250). The lower limit of the 95% CI for difference in proportion of ORR between arms was –17.81%, exceeding the predefined noninferiority margin (–20%). BCD-020 was considered noninferior to rituximab in all other measured efficacy outcomes. The proportion of AEs (including grades 3–4) was equal across both arms. The PK/PD and immunogenicity profiles of BCD-021 were comparable with that of the originator.
RTXM83 (mAbxience) In a PK and safety study, RTXM83 was evaluated and compared with rituximab in combination with cyclophosphamide, doxorubicin, vincristine, prednisolone (CHOP) chemotherapy in 24 patients with DLBCL; the study was considered to be of good quality [50]. The authors reported comparable PK and (null) immunogenicity profiles across both treatment arms.
SAIT101 (Samsung) The efficacy, safety, and PK/PD parameters of SAIT101 (plus CHOP chemotherapy) were compared with rituximab in a PK/safety study in 24 patients with DLBCL [51]. The study was considered to be of excellent quality. SAIT101 displayed efficacy (tumor response as measured by CR and PR parameters) and safety comparable with rituximab, although one case of mortality (drug-induced pneumonitis) in the SAIT101 group was recorded. Results of the PK/PD assessment indicated a high probability of similarity between SAIT101 and the originator.
3.4.3 Proposed Trastuzumab Biosimilars
Published clinical studies of proposed trastuzumab biosimilars in cancer patients are presented in Table 3.
BCD-022 (Biocad) BCD-022 was evaluated and compared with trastuzumab in a comparative PK substudy in 46 patients with HER2+ metastatic BC [52]. The study was considered to be of excellent quality using the modified Downs and Black instrument. The primary endpoint of the study was AUC0–504h. The authors reported PK equivalence of BCD-022 compared with trastuzumab in accordance with the prespecified equivalence criteria of 80–125%. BCD-022 and trastuzumab were found to be well tolerated, without any significant differences in AE frequency between the groups.
CT-P6 (Celltrion) CT-P6 has been investigated in a PK/safety study in patients with HER2+ metastatic BC (n = 174) [53]. The limits of the 90% CIs for the ratio of AUC at steady-state geometric means were reportedly contained within the established margin (80–125%) required for bioequivalence. There was no reported difference between other studied PK parameters. Serious AEs were reported in 15.8% of CT-P6 and 20.9% of trastuzumab patients; 2.6 and 3.0% were treatment related, respectively. Hypersensitivity, cardiotoxicity, and infection were noted in 1.3, 2.6, and 1.3% of CT-P6 patients and in 1.5, 7.5, and 0% of trastuzumab patients, respectively.
Results of a comparative safety/efficacy study comparing the efficacy and safety of CT-P6 versus trastuzumab in patients (n = 475) with HER2+ metastatic BC were also published [54]. The primary outcome measure was to demonstrate equivalence of CT-P6 and trastuzumab, both given in combination with paclitaxel, in terms of efficacy determined by ORR. A numerically greater number of patients achieved ORR in the trastuzumab group, compared with the CT-P6 group (62 vs. 57%, respectively). The limits of the 95% CIs for the difference in the proportion of responders (from the pooled intention-to-treat population) were reported to be within the range required for bioequivalence (–0.15, 0.15). No significant differences were observed between the two groups in the other measured efficacy parameters. The tolerability and safety of CT-P6 were reported as comparable with those of trastuzumab. Both studies were considered to be of excellent quality.
PF-05280014 (Pfizer) Two clinical studies comparing PF-05280014 with trastuzumab were ongoing at the time of review. One was for first-line treatment of patients (estimated n = 690) with HER2+ metastatic BC and the other for neoadjuvant treatment of operable HER2+ BC (estimated n = 220) [55, 56]. These studies did not undergo quality assessment, as both were found to be trial protocols.
3.5 Preclinical and Clinical Data for Intended Copies of Rituximab: Kikuzubam® and Reditux™
Published preclinical and clinical studies of rituximab intended copies are presented in Table 4.
Kikuzubam ® (Probiomed) Flores-Ortiz et al. validated a series of analytical methods for biosimilar characterization purposes [57]. In vitro comparability assessments (CDC and ADCC) were conducted using cell-based assays (CD20-expressing cells and primary NK cells). Kikuzubam® displayed comparable potency to rituximab (and intended copy Reditux™), as indicated by the results of the CDC and ADCC assays.
The physicochemical properties of Kikuzubam® were evaluated and compared with both Reditux™ and rituximab [57]. The sequence comparability of Kikuzubam® to both comparators was confirmed using peptide mapping (RP-HPLC). Kikuzubam® and rituximab were reported to have the identical glycoform profiles (Reditux™ displayed heterogeneity in theoretical mass due to the C-terminal lysine content). Significant differences were observed among all three products with respect to charge variants, as determined by cation exchange (CEX) and hydrophobic interaction chromatography (HIC). Because the CEX-HPLC technique reportedly revealed nearly two times more acidic variants than standard HPLC methods, the authors urged careful consideration in the chosen analytical methods for comparability studies. The structure [determined by differential scanning calorimetry (DSC) and matrix-assisted lasers (MALS)] and purity [determined by capillary gel electrophoresis (CGE) and size-exclusion chromatography (SEC)] were reportedly similar across all three products evaluated.
Reditux™ (Dr Reddy’s Laboratories) Thakral et al. investigated the biodistribution profile of a radiolabeled immunoconjugate of Reditux™ [177Lu-DOTA-antiCD20 antibody-rituximab (BioSim)] in three patients with B-cell NHL [58]. The study was considered to be of good quality (Downs and Black score). Maximum uptake of the radioimmunoconjugate was reportedly observed in the liver, indicating a favorable biodistribution profile.
A retrospective observational study comparing the efficacy and safety of Reditux™ versus rituximab in patients with DLBCL (n = 223) has been reported, and was considered to be of good quality (Downs and Black score) [59–61]. CR rates were similar between Reditux™ and rituximab originator, and overall survival at 5 years was also reportedly comparable. There were no reported differences in infusion-related reactions or grades 3 and 4 neutropenia and oral mucositis between the two interventions.
A prospective observational study was conducted to determine the causality and factors associated with onset drug reactions during the administration of Reditux™ in patients with cancer (excluding Hodgkin lymphoma and chronic lymphocytic leukemia indications) [62]. The study also assessed patients with chronic inflammatory disease, and the analyses were pooled across indications. Of the total number of patients (n = 133 for combined oncology and chronic inflammatory conditions), only 19 patients experienced AEs, of which the majority were perceived as mild and related to the speed of infusion. The study was considered to be of fair quality (modified Downs and Black score).
Menon et al. evaluated the PK/PD properties of Reditux™ versus rituximab in a prospective observational study in patients (n = 21) with DLBCL [63]. Analyses were undertaken and compared with published data on rituximab. The authors concluded that the PK profile and B-cell kinetics of Reditux™ were comparable with rituximab from the published literature. The study was considered to be of good quality.
Flores-Ortiz et al. compared the physicochemical properties and biological activity of both Reditux™ and Kikuzubam® with rituximab [57]. Biological comparability assessments were conducted in vitro using cell-based assays (CD20-expressing cells and primary NK cells). Reditux™ displayed similar biological effects to rituximab (and Kikuzubam®), as indicated by the results of the CDC and ADCC assays (Table 4). The Florez-Ortiz et al. study did not undergo quality assessment, because of the unavailability of suitable risk of bias assessment tools for this type of study at the time of analysis.
Kumar et al. investigated the suitability (sensitivity and specificity) of complementary assays for immunogenicity assessment in comparative clinical trials for biosimilars, using Reditux™ and rituximab as prototypic agents [64]. The study objectives were not aimed at delineating the comparability of Reditux™ versus rituximab. However, the authors commented that the analytical similarity (as implied by this study) was sufficient to justify the use of biosimilar drug-based assays for immunogenicity assessment. The Kumar et al. study did not undergo quality assessment, because of the unavailability of suitable risk of bias assessment tools for this type of study at the time of analysis.
The immunoreactivity and apyrogenicity of an immunoconjugate of Reditux™ were investigated in vitro using RAMOS cells [58]. The immunoreactivity of the mAb conjugate, as reported by the authors, showed high and specific binding ability to target cells (nonspecific binding showed <2% of the total radioactivity). The immunoreactive fraction was reported as r = R 2 0.9952 = 0.7984, where R = 0.8957. The radiolabeled doses of the mAb conjugate were reported to be pyrogen free. The bacterial endotoxin level was <0.1 EU/mL (the authors reported a permissible limit of <0.5 EU/mL; Table 4). The Thakral et al. study [58] assessed human subjects as well, and thus underwent quality assessment using the Downs and Black instrument. The study was considered to be of good quality.
As described previously, the physicochemical properties of Reditux™ were evaluated and compared with Kikuzubam® and rituximab [57]. The sequence comparability of Reditux™ to both comparators was confirmed using peptide mapping (RP-HPLC). Results of the chemical composition analysis showed heterogeneity of Reditux™ (compared with rituximab and Kikuzubam®) in theoretical mass due to the C-terminal lysine content. Significant differences were observed for both Reditux™ and Kikuzubam® versus rituximab with respect to charge variants, as determined by CEX and HIC. The structure of Reditux™ (determined by DSC and MALS) and purity (determined by CGE and SEC) were said to be similar compared with both the originator and Kikuzubam®.
Mekhssian et al. developed a workflow to aid in a more comprehensive biosimilar comparability assessment using high-resolution MS methodologies [65]. Although this study was not aimed at the characterization of Reditux™, it was utilized as a prototypic agent along with the originator, and some analyses of the data are relevant to this review. Three main glycoforms, G0F, G1F, and G2F, were observed in the mass spectra corresponding to the Fc/2 fragment of both Reditux™ and rituximab, with variations in their corresponding ratios. The authors observed that the C-terminal lysine (heavy chain) was completely clipped for rituximab and only partially clipped for Reditux™. Moreover, the presence of a light chain without N-terminal pyroglutamate formation was identified only in Reditux™. The authors reported on the suitability of IdeS digestion as a method to generate mAb fragments that are more amenable for LC separation. The authors postulated that the addition of guanidine hydrochloride (GdHCl) in turn permits the complete reduction of disulfide bridges.
Results of a comparability study by Lin et al. indicated similar structural profiles for rituximab-US and rituximab-EU [66]. However, significant differences were reported between rituximab-USA/-EU and Reditux™ as delineated by imaged capillary electrophoresis, capillary electrophoresis, and CEX-HPLC methods [66].
3.6 Quality Assessment of the Studies
The quality of analytical and cell-based studies, including abstract publications of analytical and animal studies, could not be evaluated as validated tools to assess the risk of bias for these types of studies or publications were unavailable at the time of the analysis. Thirteen studies were not evaluated [19–23, 27, 31–33, 57, 64–66]. An additional two published abstracts were found to be trial protocols and thus were not eligible for quality assessment [36, 55].
Two RCTs were assessed using the NICE STA manufacturer’s template and Jadad scoring tool (Supplementary Fig. S3) [40, 43]. Both studies were considered to be of excellent quality. Using the NICE STA assessment criteria, although both studies were randomized, only one study provided information to assess the randomization process (Yin et al. [43] did not). Despite the lack of details for randomization in the Yin et al. study, both RCTs were reported as being concealed and blinded. However, details of the blinding method were not provided in Yin et al. [43]. Patient withdrawals, outcome selection, reporting bias, and statistical analyses were appropriately reported in both studies according to the NICE STA criteria.
The two RCTs were also evaluated using the Jadad scoring tool, with Wisman et al. [40] (5 points) reporting on the randomization and method, blinding and methodology, and withdrawals and dropouts (Supplementary Fig. S3), whereas Yin et al. [43] (3 points), as mentioned above, failed to report on the method of randomization and blinding. Two observational studies were assessed using the Downs and Black scoring tool (Supplementary Fig. S4) [58, 60]. Of these, both were considered to be of good quality. Roy et al. scored 16 points from a maximum of 27 points [60], while Thakral et al. scored 13 points [58].
Word count in abstracts from conference proceedings and meetings is restricted, and thus abstracts generally provide limited information on study methodologies and outcomes. For this reason, the Downs and Black instrument was adapted to assess the quality of the 11 identified abstracts for original studies (Supplementary Fig. S5) [16, 45–47, 50–54, 62, 63]. The average score for abstract publications was 8.5 out of a possible 12 points. The total score was fair quality (3–4) for one study [62], good quality (5–8) for two studies [50, 63], and excellent quality (9–12) for eight studies [16, 45–47, 51–54]. The majority of studies published as conference abstracts were of good or excellent quality (90.9%). Three animal studies were assessed using SYRCLE’s risk of bias tool (Supplementary Fig. S6) [24, 29, 34]. The three studies were of moderate quality.
3.7 Weight and Breadth of Evidence for Biosimilarity
The available comparative data from full-text publications of RCTs are currently limited. In addition, the only post-marketing/observational studies that were identified were for intended copy Reditux™. Biosimilarity (based on combined evidence from all related published studies) was graded as identical, highly similar, similar, and dissimilar, which was directly inferred from the conclusions of the study authors (Table 5). For biosimilars, based on study author conclusions from the literature at the time the search was undertaken, the current data from clinical and nonclinical studies suggest a moderate to high degree of similarity between the described biosimilars and their originators (Table 5). The degree of biosimilarity is ultimately determined by regulatory authorities and is based on the totality of evidence, which includes data on molecular and functional characterization, other nonclinical data, and the safety, PK, immunogenicity, and efficacy clinical trial data. However, given that regulatory submissions are not publicly available and the full data set therein cannot be systematically reviewed, the authors have instead based all analysis on information from the peer-reviewed literature.
The total number of studied variables and total reported patient numbers were identified from analytical/nonclinical and clinical studies, respectively. These parameters were then mapped (Fig. 2a, b) against the degree of similarity (as observed by the study author) in order to depict the depth of the research programs and the overall quantity of available evidence for each agent.
Biosimilarity and a total number of healthy subjects or patients for proposed biosimilars and ICs in clinical trials; and b breadth of data for proposed biosimilars and ICs in analytical and nonclinical studies. Totality of evidence from all available published studies (up to September 3, 2015) was used to assess “degree of similarity” for proposed biosimilars and ICs, and is based on the original conclusions made by the study authors. The scale of reference used by each author was not accounted for, as this was not uniformly reported in the literature. * based on author interpretation of study data, Kikuzubam® exhibits, in some cases, dissimilar and, in other cases, identical physicochemical characteristics compared with the originator. BEV bevacizumab, IC intended copy, RTX rituximab, TRA trastuzumab
Studies (n = 16) of the proposed biosimilars and intended copies that were identified included 2514 patients or healthy subjects (Fig. 2a). Biosimilars CT-P6 and PF-05280014 reported the largest combined study populations from PK/safety and comparative efficacy/safety studies [649 and 1015 (two planned studies) patients, respectively]. Based on clinical reports (Fig. 2a), development candidates FTMB and RTXM83 were reported to be similar to their originators. All other development candidates were reported by study authors to be highly similar, based on clinical studies.
The extent of reported information varied greatly across studies when considering the breadth of data available for preclinical studies (based on number of variables reported from structural, functional, and nonclinical studies) for named biosimilars (Fig. 2b). PF-05280586 (rituximab), PF-05280014 (trastuzumab), and GP2013 (rituximab) all had published data on a larger number of investigated variables for analytical and nonclinical biosimilarity (ranging from 29 to 54), compared with the other development candidates, which published on average only five variables across their preclinical programs, as reported in the literature. Findings from Flores-Ortiz et al. [57] revealed heterogeneity with respect to MS and CEX data for intended copy Kikuzubam®. All other variables (DSC analysis, peptide mapping, glycan quantification, etc.) were, however, reported to be the same. Thus the positioning on the x-axis (Fig. 2b) was determined to be both dissimilar and identical across selected variables. Although the conclusions put forward by study authors were that the majority of molecules exhibited biosimilarity to their originator, comparative data were not provided for all attributes studied.
3.8 Non-empirical Data
A limited number of non-empirical publications that referenced a named biosimilar were retrieved overall. These results are shown in Supplementary Table S5. A large percentage of these studies described approaches or methodologies for the characterization and development of biosimilars, as well as how to demonstrate biosimilarity with the originator molecule [67–71]. Additional studies provided examples of biosimilars and opinions on regulatory aspects of biosimilar development [72–80].
3.9 Planned and Ongoing Trials of Bevacizumab, Rituximab, and Trastuzumab Biosimilars
The results of the ClinicalTrials.gov search (conducted September 21, 2015) are presented in Supplementary Table S6. A total of six oncology clinical trials were identified for proposed biosimilars of bevacizumab, one of which was complete at the time of analysis. PF-06439535 represented the most commonly studied bevacizumab biosimilar (two trials identified, one PK/safety study complete). Comparative efficacy and safety studies were reportedly active for ABP 215 and for BCD-021 at the time of analysis. The search also identified additional oncology biosimilars not yet appearing in the published literature. These were bevacizumab biosimilars SB8 (Samsung Bioepis) and BEVZ92 (mAbxience/Laboratorio Elea/ LIBBS).
For proposed biosimilars of rituximab, six trials, all in lymphoma, were reported. CT-P10 (Celltrion) had the highest number of studies (two comparative efficacy and safety trials identified, one actively recruiting). Single comparative efficacy and safety studies were also listed on the ClinicalTrials.gov registry for BCD-020, GP2013, PF-05280586 and RTXM83.
Within oncology and compared across all originator classes, trastuzumab biosimilars appeared most frequently in nine studies (two PK/safety in healthy subjects, one PK/safety study in patients with BC, and six comparative safety/efficacy trials). Of the trastuzumab biosimilars, Pfizer’s PF-05280014 had the most studies listed (one PK/safety study in healthy subjects, and two further studies in BC patients [55, 56]), followed by Celltrion’s CT-P6 (two comparative efficacy/safety studies). The search also identified a novel trastuzumab biosimilar, SB3 (Samsung Bioepis), not yet appearing in the published literature at the time of review.
3.10 Publishing Trends on Biosimilars
3.10.1 Journals
A total of 58 unique journals publishing material on biosimilars in oncology that met our inclusion criteria were identified during this review (23 of which published empirical studies; Supplementary Table S7). The top publishing journal was mAbs, which has published seven articles since 2010, five of which were published between 2013 and 2015. Before 2005, no journal articles relevant to the topic of mAbs or fusion protein biosimilars were published relevant to the field of oncology. The greatest number of articles was published in 2013 (n = 8), of which mAbs, Seminars in Oncology, and Annals of Oncology published two each. Since 2011 (up to and including 2014), the number of publications per year has reached similar totals (n = 5, 5, 8, 4, and 6 for 2011, 2012, 2013, 2014, and 2015, respectively).
The mAbs journal published the greatest number of empirical studies in oncology (n = 7), all of which were published in the years 2011–2015 (three were published between January and September in 2015).
3.10.2 Congresses
A total of 27 unique congresses were identified as publishing abstracts of mAb biosimilars relevant to oncology between 2007 and August 2015. Between January and August 2015, 14 abstracts were identified, highlighting the increasing interest in biosimilars for oncology among academic and industry professionals.
The top three congresses identified with the highest number of published abstracts were the American Association of Pharmaceutical Scientists National Biotechnology Conference (AAPS-NBC) (n = 13), the American Society of Clinical Oncology (ASCO) Annual Meeting (n = 11), and the American Society of Hematology (ASH) Annual Meeting (n = 4). The diverse range of congresses identified [i.e., scientific (analytical), oncology specific, regulatory/payer focused] provides evidence of the importance researchers and manufacturers put on disseminating their data to a broad audience. Before 2007, no congress abstracts relevant to the topic of mAb biosimilars in oncology were identified. Among the top identified congresses (and up to the last complete year, 2014), the highest number of abstracts was published in 2013 (n = 18), a threefold rise from the previous year (n = 6). In 2013, the congress with the greatest number of relevant published abstracts was the AAPS-NBC (n = 6), followed by ASCO (n = 2), the International Society of Pharmacovigilance (n = 2), the European Cancer Congress (n = 2), the American Association for Cancer Research (n = 2), and the European Society for Animal Cell Technology (n = 2) (Supplementary Table S8).
4 Discussion
4.1 Challenges Relevant to Biosimilar Development Identified in the Literature
While biosimilars will eventually play a greater role in the care of patients with cancer, there remain challenges that will temper their immediate impact. We identified several surveys in our review of the literature that highlight some of these challenges. For example, a survey published in 2013 of 400 healthcare professionals (including oncologists, nurses, and pharmacists) demonstrated that most participants had a lack of understanding of the regulatory pathways for biosimilars, as well as a lack of familiarity with biosimilars in the current drug pipeline [81]. A survey of 277 healthcare providers (including physicians, nurses, and pharmacists) conducted by the National Comprehensive Cancer Network (NCCN) showed similar results [6]. When asked about the level of interest in prescribing, dispensing, or administering biosimilars in their practices, 21% of physicians, 31% of nurses, and 26% of pharmacists said they needed more information on biosimilars to make a decision. Among the NCCN recommendations made by the multidisciplinary Biosimilars Working Group was a recommendation for healthcare professionals and policy makers to be educated on biosimilars [6]. The areas that respondents most wanted information on were related to comparative clinical endpoints (safety and efficacy), PK similarity (absorption, distribution, metabolism, and elimination), chemical/physical similarity, and guideline and compendia inclusion.
In addition to the need for robust educational programs on biosimilar therapies, several additional factors may influence integration of biosimilars into oncology practices [82]. These include the choice of patient population for efficacy evaluation, the choice of efficacy endpoints, extrapolation of indication, post-approval safety monitoring for immunogenicity, and interchangeability and automatic substitution. Physicians, payers, and other healthcare stakeholders will all influence the uptake and widespread adoption of biosimilars in clinical practice. As indicated in the NCCN survey, oncologists want access to the data used to support FDA approval of biosimilars, and furthermore, they need to be confident in the evidence supporting biosimilarity [6]. It is therefore incumbent on manufacturers to provide as much transparency in their development programs as possible.
4.2 Biosimilars
The majority of data comparing an investigational biosimilar with the originator in oncology imply a moderate to high degree of similarity compared with the originator products bevacizumab and trastuzumab, as inferred from study author conclusions (Table 5; Fig. 2a, b). This trend appears to be reflected throughout the stages of biosimilar development, showing that the biosimilar of interest showed high similarity at the structural level (as characterized by biochemical methods), displayed acceptable levels of biological activity (i.e., functional similarity) in vitro, and met the required PK thresholds in vivo (usually in mice or monkeys; Table 5; Fig. 2a, b).
The evidence generated in preclinical stages supports progression to clinical stages of development. Of the proposed biosimilars identified in this review, a number of molecules have followed the same logical path, including Amgen’s ABP 215 (bevacizumab), which, at the time of review, was at more advanced stages of clinical development in advanced NSCLC, having shown a high degree of structural similarity to bevacizumab along with achieving the desired outcomes (performing at the level of the originator or better) in animal models and in early safety and PK trials in humans. Pfizer’s PF-06439535 (bevacizumab) was also pursuing the same course, with comparative safety/efficacy trials underway in NSCLC, having satisfied all data requirements during its preclinical phase.
For proposed rituximab biosimilars in development for oncology, GP2013 (Sandoz), PF-05280586 (Pfizer), and RTXM83 (mAbxience) were reportedly in active comparative safety/efficacy studies in lymphoma. Both molecules have shown adequate degrees of similarity to rituximab during preclinical stages of development. Various press releases (in 2012) alluded to the halt in development of SAIT101 (Samsung), owing to concerns over biosimilar regulations in several markets [83]. Results in a PK/safety study of SAIT101 in patients with lymphoma were reported in a single publication in 2014; however, no publications were identified before or since then.
For all proposed biosimilars, it should be noted that the number and quality of studies providing evidence of structural and functional similarity at the preclinical phase may not necessarily be sufficient to predict behaviors or performance in humans. Manufacturers are required to provide high-quality evidence of comparable PK/PD and comparative efficacy and safety outcomes (including a comprehensive immunogenicity assessment) for these biosimilars in well-designed trials if they are to satisfy the requirements of the EMA and FDA for approval.
According to this review, three of Biocad’s molecules [BCD-020 (rituximab), BCD-021 (bevacizumab), and BCD-022 (trastuzumab)] have entered the clinical development phase without published evidence of underlying structural and functional similarity to their originators, for which a preliminary nonclinical assessment is required. While the authors concede that unpublished data may exist for these molecules, the intent of this research was to uncover the gaps in the literature that may contribute to stakeholder uncertainty about the depth and breadth of evidence underpinning these molecules. In the case of the trastuzumab biosimilars, at the time of this review, PF-05280014 (Pfizer) was the only molecule that had published data from all nonclinical and clinical stages. CT-P6 (Celltrion) was being investigated in PK/safety and comparative safety/efficacy trials in metastatic BC; FTMB (Amgen/Allergan/Synthon) had data from PK/safety trials (in healthy subjects), but plans for further trials were not reported; and the aforementioned BCD-022, at the time of the analysis, was being investigated in a comparative safety/efficacy study (in metastatic BC).
4.3 Intended Copies
In addition to the biosimilars identified in the literature, the authors also reviewed available data for intended copies. The extent of available data between proposed biosimilars and intended copies differs between products [7]. Nonclinical studies on intended copy Kikuzubam® (Probiomed) have, thus far, provided some evidence of its structural and functional similarity to rituximab. However, Kikuzubam® was marketed as a biosimilar or “biocomparable” in Mexico, gaining approval without published comparative clinical studies to provide evidence of its safety or efficacy. In 2012, the Mexican Pharmacovigilance Program issued a warning of anaphylactic reactions that occurred in several patients. Subsequently, Kikuzubam® was withdrawn from the market by the regulatory authority, owing to the documented anaphylactic reactions and the lack of clinical data [84]. Some countries are now only just beginning to establish formal regulatory guidelines for the approval of biosimilars to cover requirements for preclinical, clinical, or other analyses that should be used to demonstrate the safety, quality, and effectiveness of a biosimilar (including studies required for immunogenicity and AEs), as well as demonstration of similar modes of action or PD properties to that of the originator. Other countries are yet to provide any guidelines.
Reditux™ (Dr. Reddy’s Laboratories) represents a further example of an intended copy that has been marketed in Latin American markets, India, and Iran, without rigorous data to indicate structural or functional similarity or clinical effectiveness compared with rituximab. Based on the totality of evidence from studies identified during this review, Reditux™ shows heterogeneity with respect to structure, and RCTs are lacking [84, 85]. Although several observational studies have been reported for Reditux™, only one study (retrospective in design) included rituximab as a comparator.
A clear distinction must therefore be made with regard to appropriate terminology for these products, subject to the level and quality of evidence on each, such that they may be easily classified into one of the following categories: “approved biosimilars” (from a regulatory standpoint), “proposed biosimilars” (i.e., they are currently in development, but not yet approved by regulatory authorities), and “intended copies” (i.e., have not undergone rigorous comparative evaluations according to the WHO recommendations, but are being commercialized in some countries). As is evident from this review, manufacturers and researchers do not always clearly state whether they are developing a true biosimilar, or whether they are planning to introduce an intended copy (and appropriately name it as such).
4.4 Knowledge Gaps
Biosimilar products require comprehensive testing to ensure biosimilarity in terms of PK/PD, safety, and efficacy. This is to ensure patients are receiving efficacious treatment and are not being put at unnecessary risk of treatment complications, as has occurred in the case of some intended copies being commercialized in emerging markets without having undergone rigorous comparative evaluations according to the WHO recommendations [84].
A perceived advantage of biosimilars is their potential to reduce the acquisition cost of cancer drugs, thereby increasing affordability and patient access. Thus, economic factors will influence the use of these drugs in clinical practice. It has been estimated that biosimilars will cost 20–40% less in the USA, while in the EU, savings of 10–35% have been reported [7]. This is in contrast to the typical 70–80% discount associated with small-molecule generic drugs [7]. Evaluation of cost and potential cost savings will need to be performed by oncologists, institutions, and payers. From a broader societal impact, cost-effectiveness analyses will need to be performed in order to manage the differences in perceived value of these drugs when comparing the payer’s versus the patient’s and caregiver’s perceptions. In addition, pharmacovigilance and risk management, as well as safety and tolerability considerations, will need to be taken into account when assessing the value of biosimilars.
4.5 Limitations of this SLR
Several limitations of the study should be noted. These include the potential of database searches not capturing all terms related to oncology or mAb biosimilars. Also, the determination of “proposed biosimilar” versus “intended copy” is limited by the inability to discern the intentions of manufacturers with development candidates. The term “proposed biosimilar” is employed in this analysis as a blanket term for all development candidates pending final determination of their status as biosimilars. In addition, a relatively small number of selected conference proceedings were searched. Thus, it is possible that data presented in other conference proceedings may not have been included in this analysis. Furthermore, at the time of analysis, limited outcomes data were available from published conference abstracts only, with no full-text publications available at the time of the review.
The search for clinical trials was done using the ClinicalTrials.gov results database; no other clinical trial registries were used in this analysis. Therefore, it is possible that trials not registered on ClinicalTrials.gov but registered on other clinical trial databases may have been missed.
The degree of biosimilarity, as determined by regulatory authorities, is based on the totality of evidence approach, which includes data on molecular and functional characterization, other nonclinical data, and the safety, PK, immunogenicity, and efficacy clinical trial data. We did not attempt to assess the agents against the criteria used by regulatory authorities, but instead based our analysis on the totality of evidence in the public domain, with biosimilarity determined on the basis of study authors’ conclusions. Consequently, our analysis is based on the scale of reference (i.e., “identical,” “highly similar,” “similar,” or “dissimilar”) used by the study authors. Conclusions on biosimilarity were also drawn collectively from a variety of clinical study types [e.g., RCTs and observational (prospective or retrospective) studies], without accounting for any variation in the overall quality of evidence provided by each study type.
One of the original aims of our research was to identify gaps in the published literature. The results presented therefore contain only the outcomes data and statistical comparisons available from the published abstracts or full-text articles retrieved from the search. Thus, the information collated may not be representative of the full extent of data available for each study, only that which has been published. It should additionally be noted that the search strategy was designed to capture only articles published by MEDLINE® or Embase® indexed journals. Therefore, studies published by non-indexed journals were not included. A full Internet search of all online content was not included in the methodology.
As this review represents a cross-sectional analysis of available published evidence over a defined period, the molecules reviewed were at various stages of development and therefore cannot be compared like for like. Since completion of this review, the authors have identified new biosimilar studies in oncology. These include clinical trials for ABP798 (rituximab; Amgen; CD20+ NHL) and for HLX01 (rituximab; Shanghai Henlius Biotech; CD20+ DLBCL). The JASMINE study is a randomized, double-blind study assessing the safety and efficacy of ABP798 compared with rituximab in patients with CD20+ NHL. The safety and efficacy of HLX01 is being compared with rituximab in combination with CHOP in previously untreated subjects with CD20+ DLBCL.
5 Conclusions
This SLR collates and summarizes all published evidence up to September 2015 on named biosimilars and intended copies of originator mAbs that have been developed in the field of oncology. The review identified biosimilars for the marketed biologics bevacizumab, trastuzumab, and rituximab, and many of these biosimilar molecules are in late-stage clinical development. Intended copies in development for rituximab were also identified.
At present, robust evidence of outcomes for mAb biosimilars in cancer, including data from comparative efficacy and safety trials, is not yet substantially available in the published literature. The authors acknowledge that there are a number of planned and ongoing clinical trials that will help inform the current knowledge gaps. While biosimilar treatments are expected to reduce drug costs and increase patient access to much-needed therapies, the potential impact of these drugs in oncology is currently unclear. Only when oncology biosimilars are approved and adopted in routine clinical practice will their impact be fully recognized.
References
IMS Health. Developments in cancer treatments, market dynamics, patient access and value. Global oncology trend report 2015. 2015 May 2015 [cited 2016 21 June]; Available from: http://keionline.org/sites/default/files/IIHI_Oncology_Trend_Report_2015.pdf.
IMS Health. Medicines use and spending in the U.S. A review of 2015 and outlook to 2020. 2016 April 2016 [cited 2016 21 June]; Available from: https://morningconsult.com/wp-content/uploads/2016/04/IMS-Institute-US-Drug-Spending-2015.pdf.
IMS Health. Top 20 global products 2015. 2015 December 2015 [cited 2016 21 June]; Available from: http://www.imshealth.com/files/web/Corporate/News/Top-Line%20Market%20Data/Top_20_Global_Products_2015.pdf.
Gori S, Di Maio M, Pinto C, Alabiso O, Baldini E, Beretta GD, et al. Differences in the availability of new anti-cancer drugs for Italian patients treated in different regions. Results of analysis conducted by the Italian Society Of Medical Oncology (AIOM). Tumori. 2010;96(6):1010–5.
Park T, Griggs SK, Suh DC. Cost effectiveness of monoclonal antibody therapy for rare diseases: a systematic review. BioDrugs. 2015;29(4):259–74.
Zelenetz AD, Ahmed I, Braud EL, Cross JD, Davenport-Ennis N, Dickinson BD, et al. NCCN biosimilars white paper: regulatory, scientific, and patient safety perspectives. J Natl Compr Cancer Netw. 2011;9(suppl 4):S1–22.
Camacho LH, Frost CP, Abella E, Morrow PK, Whittaker S. Biosimilars 101: considerations for U.S. oncologists in clinical practice. Cancer Med. 2014;3(4):889–99.
Mysler E, Pineda C, Horiuchi T, Singh E, Mahgoub E, Coindreau J, et al. Clinical and regulatory perspectives on biosimilar therapies and intended copies of biologics in rheumatology. Rheumatol Int. 2016;36(5):613–25.
Jacobs I, Petersel D, Shane LG, Ng CK, Kirchhoff C, Finch G, et al. Monoclonal antibody and fusion protein biosimilars across therapeutic areas: a systematic review of published evidence. BioDrugs. 2016;30(6):489–523.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34.
National Institute for Health Care Excellence. Single technology appraisal: user guide for company evidence submission template. 2015 Jan 2015 [cited 2016 21 June]; Available from: http://www.nice.org.uk/article/pmg24.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84.
Hooijmans CR, Rovers MM, de Vries RB, Leenaars M, Ritskes-Hoitinga M, Langendam MW. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. 2014;14:43.
Markus R, Kaur PP, Chow V, Zhang N, Born TL, Huynh Q, et al. Results of functional testing and pharmacokinetics comparing ABP 215 to bevacizumab. J Clin Oncol. 2015;33(15 suppl):711.
Markus RA, Born T, Chow V, Zhang N, Huynh Q, Maher G, et al. Functional similarity and human pharmacokinetic (PK) equivalence of ABP 215 and bevacizumab. J Clin Oncol. 2015;33(15 suppl):e14659.
Born TL, Huynh Q, Mathur A, Velayudhan J, Canon J, Reynhardt K, et al. Functional similarity assessment results comparing bevacizumab to biosimilar candidate ABP 215. Ann Oncol. 2014;25(suppl 4):iv163.
Hutterer K, Liu J, Martinez T, Pace D, Yates Z, Velayudhan J, et al. Analytical similarity assessment of a biosimilar to bevacizumab. In: 19th Symposium on the interface of regulatory and analytical sciences for biotechnology health products (WCBP); 27–29 January 2015; Washington, DC; 2015. p. 146.
Grunder B. Characterization and similarity assessment of bevacizumab and a proposed biosimilar. In: 2014 American Association of Pharmaceutical Scientists (AAPS) annual meeting and exposition; 2–6 November 2014; San Diego; 2014. p. W5349.
Peraza M, Shiue M, Phenix S, Rule K, Finch GL, Thibault S, et al. Comparative nonclinical assessment of the potential biosimilar PF-06439535 and bevacizumab. In: 54th annual meeting of the Society of Toxicology (SOT); 22–26 March 2015; San Diego; 2015. p. Abstr: 129.
Archuadze S, Shipaeva P, Dwivedi Y, Lavrovsky M, Samsonov M, Oshodi T. Pharmacokinetic profile of RPH-001, a recombinant humanized monoclonal antibody to human VEGF following administration by intravenous infusion in the cynomolgus monkey. Toxicologist. 2015;144(1):128.
Dorvignit D, Palacios JL, Merino M, Hernández T, Sosa K, Casaco A, et al. Expression and biological characterization of an anti-CD20 biosimilar candidate antibody: a case study. mAbs. 2012;4(4):488–96.
da Silva A, Kronthaler U, Koppenburg V, Fink M, Meyer I, Papandrikopoulou A, et al. Target-directed development and preclinical characterization of the proposed biosimilar rituximab GP2013. Leuk Lymphoma. 2014;55(7):1609–17.
da Silva A, Kronthaler U, Meyer I, Papandrikopoulou A, Stangler T, Visser JM. Target-directed development of a proposed biosimilar rituximab (GP2013): comparability of antibody-dependent cellular cytotoxicity activity and pre-clinical pharmacokinetics and pharmacodynamics with originator rituximab. In: American College of Rheumatology/Association of Rheumatology Health Professionals (ACR/ARHP) Annual Meeting; 9–14 November 2012; Washington, DC; 2012. p. S911.
da Silva A, Kronthaler U, Meyer I, Fritsch C, Schneiderer T, Stangler T, et al. Physicochemical, functional, and pharmacologic comparability between the proposed biosimilar rituximab GP2013 and originator rituximab as the foundation for biosimilarity. J Clin Oncol. 2013;31(15 suppl):3075.
Visser J, Feuerstein I, Stangler T, Schmiederer T, Fritsch C, Schiestl M. Physicochemical and functional comparability between the proposed biosimilar rituximab GP2013 and originator rituximab. BioDrugs. 2013;27(5):495–507.
Hurst SI, Ryan AM, Ng C-K, Ploch SA, Finch GL, Leach MW. Nonclinical assessments demonstrating the similarity of the proposed biosimilar PF-05280586 and rituximab. Ann Rheum Dis. 2013;72(suppl 3):A198.
Ryan AM, Sokolowski SA, Ng C-K, Shirai N, Collinge M, Shen AC, et al. Comparative nonclinical assessments of the proposed biosimilar PF-05280586 and rituximab (MabThera®). Toxicol Pathol. 2014;42(7):1069–81.
Hurst S, Ryan AM, Ng CK, Thompson M, Plock S, Finch GL, et al. Comparative nonclinical assessments of rituximab-EU (MabThera®) and the potential biosimilar PF-05280586. In: 2013 American Association of Pharmaceutical Scientists (AAPS) national biotechnology conference; 20–23 May 2013; San Diego; 2013. p. M1125.
Karnik S, Thompson M, De Gruttola H, Ferrari S, Gu L, Aggarwal P, et al. Characterization and comparison of PF-05280586—a proposed rituximab biosimilar to the licensed product. In: 2013 American Association of Pharmaceutical Scientists (AAPS) national biotechnology conference; 20–23 May 2013; San Diego; 2013. p. M1038.
Seigelchifer M, Corley E, Fresnillo G, Pesce A, Bes C, Elise M, et al. Development of RTXM83 (a potential rituximab biosimilar): in vitro and in vivo comparability with MabThera. J Clin Oncol. 2014;32(15 suppl):e14020.
Boyle PJ, DeGruttola H, Ferrari S, Gu L, Aggarwal P, Thompson M, et al. Characterization and comparison of PF-05280014—a proposed trastuzumab biosimilar to the licensed product. In: 2013 American Association of Pharmaceutical Scientists (AAPS) National Biotechnology Conference; 20–22 May 2013; San Diego; 2013. p. M1037.
Hurst S, Ryan AM, Ng C-K, McNally JM, Lorello LG, Finch GL, et al. Comparative nonclinical assessments of the proposed biosimilar PF-05280014 and trastuzumab (Herceptin®). BioDrugs. 2014;28(5):451–9.
Hurst S, Ryan A, Ng C, Thompson M, McNally J, Ploch S, et al. Comparative nonclinical assessments of trastuzumab-US and trastuzumab-EU (Herceptin®) and the potential biosimilar PF-05280014. In: 2013 American Association of Pharmaceutical Scientists (AAPS) national biotechnology conference; 20–23 May 2013; San Diego; 2013. p. M1124.
Jacobs IA, Ewesuedo R, Yin D, Li R, Hurst S, Ryan AM, et al. Development of PF-05280014, a potential biosimilar to trastuzumab. In: 2015 American Society of Clinical Oncology (ASCO) annual meeting; 29 May–2 June 2015; Chicago; 2015. p. 618.
Ryan AM, Hurst S, McNally JM, Lorello LG, Finch GL, Leach MW, et al. Comparative pharmacokinetics of trastuzumab-US and trastuzumab-EU and the potential biosimilar trastuzumab-Pfizer in male CD-1 mice. Eur J Cancer. 2012;48(suppl 6):98.
Jacobs I, Petersel D, Isakov L, Lula S, Lea Sewell K. Biosimilars for the treatment of chronic inflammatory diseases: a systematic review of published evidence. BioDrugs. 2016;30(6):525–70.
Wisman L, De Cock E, Reijers J, De Visser I, De Kam M, van Os S, et al. A phase I dose escalation and bioequivalence study of a trastuzumab biosimilar (FTMB) in healthy male volunteers. In: 2012 European Society for Medical Oncology (ESMO) congress; 28 September–2 October 2012; Vienna; 2012. p. ix103–ix4.
Wisman LAB, De Cock EPM, Reijers JAA, Kamerling IMC, Van Os SHG, de Kam ML, et al. A phase I dose-escalation and bioequivalence study of a trastuzumab biosimilar in healthy male volunteers. Clin Drug Investig. 2014;34(12):887–94.
Ricart AD, Zacharchuk C, Reich SD, Meng X, Barker KB, Taylor CT, et al. A phase I pharmacokinetics trial comparing PF-05280014 and trastuzumab in healthy volunteers (REFLECTIONS B327-01). In: 35th Annual Cancer Therapy & Research Center and American Association for Cancer Research (CTRC-AACR) San Antonio Breast Cancer Symposium (SABCS); 4–8 December 2012; San Antonio: Cancer Res; 2012. p. OT1–05.
Yin D, Barker KB, Li R, Meng X, Reich SD, Ricart AD, et al. A phase I pharmacokinetics trial comparing PF-05280014 (a potential biosimilar) and trastuzumab in healthy volunteers (REFLECTIONS B327-01). In: 2013 American Society of Clinical Oncology (ASCO) annual meeting; 31 May–4 June 2013; Chicago; 2013. p. 612.
Yin D, Barker KB, Li R, Meng X, Reich SD, Ricart AD, et al. A randomized phase 1 pharmacokinetic trial comparing the potential biosimilar PF-05280014 with trastuzumab in healthy volunteers (REFLECTIONS B327-01). Br J Clin Pharmacol. 2014;78(6):1281–90.
Yin D, Cai CH, Taylor CT, Zacharchuk CM, Rudin D, Reich SD, et al. Immunogenicity assessment of PF-05280014, a potential biosimilar to trastuzumab, in healthy subjects (REFLECTIONS B327-01). Eur J Cancer. 2013;49(suppl 2):S176–7.
Orlov SV, Burdaeva ON, Nachaeva MP, Kopp MV, Kotiv BN, Sheveleva LP, et al. Pharmacokinetics and safety of BCD-021, bevacizumab biosimilar candidate, compared to Avastin in patients. J Clin Oncol. 2014;32(15 suppl):e13500.
Filon O, Orlov SV, Burdaeva ON, Kopp MlV, Kotiv BN, Alekseev S, et al. Efficacy and safety of BCD-021, bevacizumab biosimilar candidate, compared to Avastin: results of international multicenter randomized double blind phase III study in patients with advanced non-squamous NSCLC. In: 2015 American Society of Clinical Oncology (ASCO) annual meeting; 29 May–2 June 2015; Chicago: J Clin Oncol; 2015. p. 8057.
Alexeev S, Zaritskey A, Volodicheva E, Loginov A, Orlova R, Dvornichenko V, et al. Clinical comparability of BCD-020 to innovator rituximab in patients with indolent non-Hodgkin’s lymphoma. Haematologica. 2014;99(suppl 1):144–5.
Kaplanov K, Zaritskiy A, Alexeev S, Volodicheva E, Loginov A, Orlova R, et al. Key results of international randomized open-label clinical study of BCD-020 (rituximab biosimilar candidate) in patients with B-cell non-Hodgkin’s lymphoma. Blood. 2014;124(21):5467.
Poddubnaya I, Babicheva L, Kaplanov K, Zaritskey A, Volodicheva E, Alexeev S, et al. Comparison of pharmacokinetics and pharmacodynamics of BCD-020 with innovator rituximab to patients with indolent non-Hodgkin lymphoma. J Clin Oncol. 2014;32(15 suppl):e19545.
Florez A, Di Matteo T, Fresnillo G, Tudela C, Seigelchifer M, Corley E, et al. Clinical pharmacokinetic (PK) and safety (immunogenicity) of rituximab biosimilar RTXM83 in combination with chemotherapy CHOP in patients with diffuse large B-cell lymphoma (DLBCL). Blood. 2014;124(21):5472.
Kim SJ, Kim WS, Kang HJ, Kim JS, Choi CW, Lee SI, et al. Safety, pharmacokinetic/pharmacodynamic profiles and efficacy of SAIT101, a biosimilar of rituximab in patients with diffuse large B-cell lymphoma. Haematologica. 2012;97(suppl 1):S317–8.
Stenina MB, Ignatova E, Frolova MA, Burdaeva ON, Nechaeva MP, Kopp MV, et al. Pharmacokinetics and safety of BCD-022, trastuzumab biosimilar candidate, compared to Herceptin in patients. J Clin Oncol. 2014;32(15 suppl):e11576.
Im Y, Krasnozhon D, Bondarenko I, Zvirbule Z, Jung K, Oliynychenko P, et al. Phase I/IIb clinical trial comparing PK and safety of trastuzumab and its biosimilar candidate CT-P6. Breast. 2013;22(suppl 1):S108.
Im Y-H, Odarchenko P, Grecea D, Komov D, Anatoliy CV, Gupta S, et al. Double-blind, randomized, parallel group, phase III study to demonstrate equivalent efficacy and comparable safety of CT-P6 and trastuzumab, both in combination with paclitaxel, in patients with metastatic breast cancer (MBC) as first-line treatment. J Clin Oncol. 2013;31(15 suppl):629.
Ewesuedo R, Barker KB, Taylor CT, Jacobs I. A phase 3 randomized, double-blind trial comparing PF-05280014 + paclitaxel vs. trastuzumab + paclitaxel for treatment of HER2 + metastatic breast cancer. Cancer Res. 2013;73(24 suppl).
Jacobs I, Coiro J, Hilton F, Orazem J, Abbas R, Zacharchuk C. A phase 3 randomized, double-blind trial comparing PF-05280014 + docetaxel and carboplatin vs. trastuzumab + docetaxel and carboplatin for neoadjuvant treatment of operable HER2 + breast cancer. Cancer Res. 2015;75(9 suppl):Abstract OT3-1-02.
Flores-Ortiz LF, Campos-García VR, Perdomo-Abúndez FC, Pérez NO, Medina-Rivero E. Physicochemical properties of rituximab. J Liq Chromatogr Relat Technol. 2014;37(10):1438–52.
Thakral P, Singla S, Yadav MP, Vasisht A, Sharma A, Gupta SK, et al. An approach for conjugation of 177Lu-DOTA-SCN- rituximab (BioSim) & its evaluation for radioimmunotherapy of relapsed & refractory B-cell non Hodgkins lymphoma patients. Indian J Med Res. 2014;139(4):544–54.
Roy PS, John S, Kannan S, Gujral S, Gawande J, B. B, et al. Comparison of efficacy and safety of rituximab (Mabthera) and its biosimilar (Reditux) in diffuse large B cell lymphoma (DLBCL) patients treated with chemo-immunotherapy: a retrospective analysis. In: 53rd National Conference of Indian Society of Hematology & Blood Transfusion (ISHBT); 9–11 November 2012; Puri: Springer; 2012. p. Abstr: 234.
Roy PS, John S, Karankal S, Kannan S, Pawaskar P, Gawande J, et al. Comparison of the efficacy and safety of rituximab (Mabthera™) and its biosimilar (Reditux™) in diffuse large B-cell lymphoma patients treated with chemo-immunotherapy: a retrospective analysis. Indian J Med Paediatr Oncol. 2013;34(4):292.
Roy PS, Sengar M, Menon H, et al. A retrospective single centre analysis of safety, toxicity and efficacy of rituximab (original) and its biosimilar in diffuse large B-cell lymphoma patients treated with chemo-immunotherapy. In: 2012 European Society for Medical Oncology (ESMO) Congress; 28 September–2 October 2012; Vienna; 2012. p. Abstr: ix351.
Aliaga L, Fernandez I, Sanchez M, Saavedra H, Espinoza C. Pharmacovigilance of anti CD 20 monoclonal antibody biosimilar at the Edgardo Rebagliati Martins Hospital-Peru. Drug Saf. 2013;36(9):925.
Menon H, Yadav A, Subramanian PG, Sengar M, Rath S, Kavathiya K, et al. Pharmacokinetic and pharmacodynamic properties of a biosimilar rituximab (Reditux®) are identical to the innovator brand MabThera®—experience from a tertiary cancer centre in Western India. Blood. 2014;124(21):2246.
Kumar V, Vemuri S, Lella RK, Babu MN, Atluri A, Gowravaram M, et al. Suitability of ‘one assay’ for immunogenicity assessment of both proposed biosimilar and innovator rituximab. In: 2014 American Association of Pharmaceutical Scientists (AAPS) national biotechnology conference; 2–6 November 2014; San Diego; 2014. p. M1042.
Mekhssian K, Mess JN, Montalibet J, Garofolo F. Application of complementary HRMS methodologies for a thorough biosimilar comparability assessment. In: 2015 American Association of Pharmaceutical Scientists (AAPS) national biotechnology conference; 8–10 June 2015; San Francisco; 2015. p. T2055.
Lin S, Ramatlapeng D, Hanning J, Bakewell W. Comparability study of monoclonal biosimilar drug products using various analytical methods. In: 18th symposium on the interface of regulatory and analytical sciences for biotechnology health products (WCBP); 28–30 January 2014; Washington, DC; 2014. p. 104.
Beck A, Sanglier-Cianférani S, Van Dorsselaer A. Biosimilar, biobetter, and next generation antibody characterization by mass spectrometry. Anal Chem. 2012;84(11):4637–46.
da Silva A, Grau R, Stangler T, Summer H, Meyer I, Rohde A, et al. Comprehensive target-directed approach for the development of a highly-comparable rituximab biosimilar. Ann Rheum Dis. 2012;71(suppl 3):718.
Ebbers HC, van Meer PJ, Moors EH, Mantel-Teeuwisse AK, Leufkens HG, Schellekens H. Measures of biosimilarity in monoclonal antibodies in oncology: the case of bevacizumab. Drug Discov Today. 2013;18(17–18):872–9.
Kurbanova EK, Chulkova TY, Byrikhina DV, Dano AO, Nikolaeva VA, Gusarov DA. PHARMA-2020: technological aspects of production of some strategical biopharmaceuticals. Russ J Biopharm. 2012;4(3):21–45.
Li E, Subramanian J, Anderson S, Thomas D, McKinley J, Jacobs IA. Development of biosimilars in an era of oncologic drug shortages. Drug Des Dev Ther. 2015;9:3247–55.
What are biosimilars and are they important? Drug Ther Bull. 2013;51(5):57–60.
Cragg MS. CD20 antibodies: doing the time warp. Blood. 2011;118(2):219–20.
Dhingra K. Biosimilars: the industry perspective. J Crohns Colitis. 2009;3(suppl 1):78.
Kay J. Biosimilars: a regulatory perspective from America. Arthritis Res Ther. 2011;13(3):112.
Kudrin A, Knezevic I, Joung J, Kang HN. Case studies on clinical evaluation of biosimilar monoclonal antibody: scientific considerations for regulatory approval. Biologicals. 2015;43(1):1–10.
Nelson KM, Gallagher PC. Biosimilars lining up to compete with Herceptin—opportunity knocks. Expert Opin Ther Pat. 2014;24(11):1149–53.
Rioufol C, Salles G. Biosimilar monoclonal antibodies in lymphoma: a critical appraisal. Expert Rev Anticancer Ther. 2015;15(5):569–78.
Thill M. New frontiers in oncology: biosimilar monoclonal antibodies for the treatment of breast cancer. Expert Rev Anticancer Ther. 2015;15(3):331–8.
Vital EM, Kay J, Emery P. Rituximab biosimilars. Expert Opin Biol Ther. 2013;13(7):1049–62.
Krejcik C. NACCME Releases Results of survey assessing medical education needs in biosimilars [news release]. 2013 May 28 2013 [cited 2016 October 20]; Available from: http://www.prweb.com/releases/2013/5/prweb10769551.htm.
Rugo HS, Linton KM, Cervi P, Rosenberg JA, Jacobs I. A clinician’s guide to biosimilars in oncology. Cancer Treat Rev. 2016;46:73–9.
Macdonald G. Samsung halts biosimilar rituximab trial on regulatory concerns [news release]. 2012 Oct 2012 [cited 2016 21 June]; Available from: http://www.biopharma-reporter.com/Bio-Developments/Samsung-halts-biosimilar-rituximab-trial-on-regulatory-concerns.
Castañeda-Hernández G, González-Ramírez R, Kay J, Scheinberg MA. Biosimilars in rheumatology: what the clinician should know. RMD Open. 2015;1(1):e000010.
Espinosa-de la Garza CE, Perdomo-Abúndez FC, Padilla-Calderón J, Uribe-Wiechers JM, Pérez NO, Flores-Ortiz LF, et al. Analysis of recombinant monoclonal antibodies by capillary zone electrophoresis. Electrophoresis. 2013;34(8):1133–40.
Acknowledgements
The SLR to support this report was sponsored by Pfizer Inc. Medical writing support was provided by Robyn Fowler, PhD, of Engage Scientific Solutions, and was funded by Pfizer Inc. Carole Jones of Envision Pharma Group was involved with the development of the SLR, which was funded by Pfizer Inc.
Author contributions
All authors were involved in drafting the article and revising it critically for important intellectual content. All authors read and approved the final manuscript submitted for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
IJ, RE, and CZ are full-time employees and shareholders of Pfizer. SL is a full-time employee of Envision Pharma Group, who were paid consultants to Pfizer in connection with the development of the SLR report that forms the basis of this manuscript. He was not compensated for his role in the development of this manuscript.
Funding
The SLR to support this manuscript was sponsored by Pfizer Inc.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Jacobs, I., Ewesuedo, R., Lula, S. et al. Biosimilars for the Treatment of Cancer: A Systematic Review of Published Evidence. BioDrugs 31, 1–36 (2017). https://doi.org/10.1007/s40259-016-0207-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-016-0207-0