Abstract
Background
Genome-based precision medicine strategies promise to minimize premature graft loss after renal transplantation, through precision approaches to immune compatibility matching between kidney donors and recipients. The potential adoption of this technology calls for important changes to clinical management processes and allocation policy. Such potential policy change decisions may be supported by decision models from health economics, comparative effectiveness research and operations management.
Objective
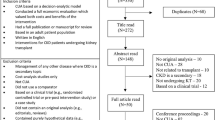
We used a systematic approach to identify and extract information about models published in the kidney transplantation literature and provide an overview of the status of our collective model-based knowledge about the kidney transplant process.
Methods
Database searches were conducted in MEDLINE, Embase, Web of Science and other sources, for reviews and primary studies. We reviewed all English-language papers that presented a model that could be a tool to support decision making in kidney transplantation. Data were extracted on the clinical context and modelling methods used.
Results
A total of 144 studies were included, most of which focused on a single component of the transplantation process, such as immunosuppressive therapy or donor-recipient matching and organ allocation policies. Pre- and post-transplant processes have rarely been modelled together.
Conclusion
A whole-disease modelling approach is preferred to inform precision medicine policy, given its potential upstream implementation in the treatment pathway. This requires consideration of pre- and post-transplant natural history, risk factors for allograft dysfunction and failure, and other post-transplant outcomes. Our call is for greater collaboration across disciplines and whole-disease modelling approaches to more accurately simulate complex policy decisions about the integration of precision medicine tools in kidney transplantation.
Graphical abstract


Similar content being viewed by others
References
Zelmer JL. The economic burden of end-stage renal disease in Canada. Kidney Int. 2007;72(9):1122–9. https://doi.org/10.1038/sj.ki.5002459 (published Online First: 2007/08/19).
Liyanage T, Ninomiya T, Jha V, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385(9981):1975–82. https://doi.org/10.1016/S0140-6736(14)61601-9 (published Online First: 20150313).
Canadian Organ Replacement Register. Canadian Institute for Health Information. Treatment of End-Stage Organ Failure in Canada, 2010 to 2019 2020. https://www.cihi.ca/en/organ-replacement-in-canada-corr-annual-statistics-2020. Accessed 21 Apr 2022.
Sussell J, Silverstein AR, Goutam P, et al. The economic burden of kidney graft failure in the United States. Am J Transplant. 2020;20(5):1323–33. https://doi.org/10.1111/ajt.15750 (published Online First: 20200204).
Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11(10):2093–109. https://doi.org/10.1111/j.1600-6143.2011.03686.x (published Online First: 20110830).
Wiebe C, Rush DN, Nevins TE, et al. Class II eplet mismatch modulates tacrolimus trough levels required to prevent donor-specific antibody development. J Am Soc Nephrol. 2017. https://doi.org/10.1681/ASN.2017030287 (published Online First: 2017/07/22).
Wiebe C, Pochinco D, Blydt-Hansen TD, et al. Class II HLA epitope matching-a strategy to minimize de novo donor-specific antibody development and improve outcomes. Am J Transplant. 2013;13(12):3114–22. https://doi.org/10.1111/ajt.12478 (published Online First: 2013/10/30).
Senev A, Coemans M, Lerut E, et al. Eplet Mismatch load and De novo occurrence of donor-specific anti-HLA antibodies, rejection, and graft failure after kidney transplantation: an observational cohort study. J Am Soc Nephrol. 2020. https://doi.org/10.1681/ASN.2020010019 (published Online First: 2020/08/09).
Sapir-Pichhadze R, Tinckam K, Quach K, et al. HLA-DR and -DQ eplet mismatches and transplant glomerulopathy: a nested case-control study. Am J Transplant. 2015;15(1):137–48. https://doi.org/10.1111/ajt.12968.
Kosmoliaptsis V, Mallon DH, Chen Y, et al. Alloantibody responses after renal transplant failure can be better predicted by donor-recipient hla amino acid sequence and physicochemical disparities than conventional HLA matching. Am J Transplant. 2016;16(7):2139–47. https://doi.org/10.1111/ajt.13707 (published Online First: 20160301).
Kausman JY, Walker AM, Cantwell LS, et al. Application of an epitope-based allocation system in pediatric kidney transplantation. Pediatr Transplant. 2016;20(7):931–8. https://doi.org/10.1111/petr.12815 (published Online First: 20160924).
Sapir-Pichhadze R, Zhang X, Ferradji A, et al. Epitopes as characterized by antibody-verified eplet mismatches determine risk of kidney transplant loss. Kidney Int. 2019. https://doi.org/10.1016/j.kint.2019.10.028 (published Online First: 2020/02/16).
Himmelfarb J, Vanholder R, Mehrotra R, et al. The current and future landscape of dialysis. Nat Rev Nephrol. 2020;16(10):573–85. https://doi.org/10.1038/s41581-020-0315-4 (published Online First: 20200730).
Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR). 2020 Annual Data Report. 2022. http://srtr.transplant.hrsa.gov/annual_reports/Default.aspx. Accessed 21 Apr 2022.
Kidney foundation of Canada. Facing the Facts. 2020. https://kidney.ca/KFOC/media/images/PDFs/Facing-the-Facts-2020.pdf. Accessed 21 Apr 2022.
Winkelmayer WC, Weinstein MC, Mittleman MA, et al. Health economic evaluations: the special case of end-stage renal disease treatment. Med Decis Making. 2002;22(5):417–30. https://doi.org/10.1177/027298902236927.
Senanayake S, Graves N, Healy H, et al. Cost-utility analysis in chronic kidney disease patients undergoing kidney transplant; what pays? A systematic review. Cost Eff Resour Alloc. 2020;18:18. https://doi.org/10.1186/s12962-020-00213-z (published Online First: 20200519).
Chung R, Howard K, Craig JC, et al. Economic evaluations in kidney transplantation: frequency, characteristics, and quality-a systematic review. Transplantation. 2014;97(10):1027–33. https://doi.org/10.1097/TP.0000000000000079.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097. https://doi.org/10.1371/journal.pmed.1000097 (published Online First: 20090721).
Husereau D, Drummond M, Petrou S, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Value Health. 2013;16(2):e1-5. https://doi.org/10.1016/j.jval.2013.02.010.
Gharibi Z, Ayvaci MUS, Hahsler M, et al. Cost-effectiveness of antibody-based induction therapy in deceased donor kidney transplantation in the United States. Transplantation. 2017;101(6):1234–41. https://doi.org/10.1097/TP.0000000000001310.
Muduma G, Shaw J, Hart WM, et al. Cost utility analysis of immunosuppressive regimens in adult renal transplant recipients in England and Wales. Patient Prefer Adherence. 2014;8:1537–46. https://doi.org/10.2147/PPA.S69461 (published Online First: 20141104).
Muduma G, Odeyemi I, Pollock RF. Evaluating the economic implications of non-adherence and antibody-mediated rejection in renal transplant recipients: the role of once-daily tacrolimus in the UK. J Med Econ. 2015;18(12):1050–9. https://doi.org/10.3111/13696998.2015.1074584 (published Online First: 20150826).
Whiting JF, Kiberd B, Kalo Z, et al. Cost-effectiveness of organ donation: evaluating investment into donor action and other donor initiatives. Am J Transplant. 2004;4(4):569–73. https://doi.org/10.1111/j.1600-6143.2004.00373.x.
Tilden DP, Chapman J, Davey PJ, et al. A decision-analytic economic evaluation of valaciclovir prophylaxis for the prevention of cytomegalovirus infection and disease in renal transplantation. Clin Transplant. 2004;18(3):312–20. https://doi.org/10.1111/j.1399-0012.2004.00168.x.
Tedesco Silva Jr H, EvansGavaghan RWMB, et al. A cost-effectiveness analysis of organ preservation methods for deceased donor kidneys at high risk for delayed graft function in Brazil. Transplant Proc. 2018;50(10):3121–7. https://doi.org/10.1016/j.transproceed.2018.06.024 (published Online First: 20180626).
Felipe C, Tedesco-Silva H, Ferreira Brigido A, et al. Cost-effectiveness analysis of everolimus versus mycophenolate in kidney transplant recipients receiving no pharmacological prophylaxis for cytomegalovirus infection: a short-term pharmacoeconomic evaluation (12 Months). Value Health Reg Issues. 2017;14:108–15. https://doi.org/10.1016/j.vhri.2017.08.009 (published Online First: 20171109).
Cleemput I, Kesteloot K, Vanrenterghem Y, et al. The economic implications of non-adherence after renal transplantation. Pharmacoeconomics. 2004;22(18):1217–34. https://doi.org/10.2165/00019053-200422180-00006.
Howard K, Salkeld G, White S, et al. The cost-effectiveness of increasing kidney transplantation and home-based dialysis. Nephrology (Carlton). 2009;14(1):123–32. https://doi.org/10.1111/j.1440-1797.2008.01073.x.
Scott N, Snell G, Westall G, et al. Cost-effectiveness of transplanting lungs and kidneys from donors with potential hepatitis C exposure or infection. Sci Rep. 2020;10(1):1459. https://doi.org/10.1038/s41598-020-58215-z (published Online First: 20200129).
Hornberger JC, Best JH, Garrison LP Jr. Cost-effectiveness of repeat medical procedures: kidney transplantation as an example. Med Decis Making. 1997;17(4):363–72. https://doi.org/10.1177/0272989X9701700401.
Haller M, Gutjahr G, Kramar R, et al. Cost-effectiveness analysis of renal replacement therapy in Austria. Nephrol Dial Transplant. 2011;26(9):2988–95. https://doi.org/10.1093/ndt/gfq780 (published Online First: 20110210).
Moradpour A, Hadian M, Tavakkoli M. Economic evaluation of end stage renal disease treatments in Iran. Clini Epidemiol Glob Health. 2020;8(1):199–204.
Schweitzer EJ, Perencevich EN, Philosophe B, et al. Estimated benefits of transplantation of kidneys from donors at increased risk for HIV or hepatitis C infection. Am J Transplant. 2007;7(6):1515–25. https://doi.org/10.1111/j.1600-6143.2007.01769.x.
Mutinga N, Brennan DC, Schnitzler MA. Consequences of eliminating HLA-B in deceased donor kidney allocation to increase minority transplantation. Am J Transplant. 2005;5(5):1090–8. https://doi.org/10.1111/j.1600-6143.2005.00802.x.
Matas AJ, Schnitzler M. Payment for living donor (vendor) kidneys: a cost-effectiveness analysis. Am J Transplant. 2004;4(2):216–21. https://doi.org/10.1046/j.1600-6143.2003.00290.x.
Axelrod DA. Economic and financial outcomes in transplantation: whose dime is it anyway? Curr Opin Organ Transplant. 2013;18(2):222–8. https://doi.org/10.1097/MOT.0b013e32835f0757.
Nguyen HD, Wong G, Howard K, et al. Modeling the benefits and costs of integrating an acceptable HLA mismatch allocation model for highly sensitized patients. Transplantation. 2014;97(7):769–74. https://doi.org/10.1097/01.TP.0000438639.36838.ac.
Muntinghe FL, Vegter S, Verduijn M, et al. Using a genetic, observational study as a strategy to estimate the potential cost-effectiveness of pharmacological CCR5 blockade in dialysis patients. Pharmacogenet Genom. 2011;21(7):417–25. https://doi.org/10.1097/FPC.0b013e3283472990.
Luan FL, Kommareddi M, Ojo AO. Universal prophylaxis is cost effective in cytomegalovirus serology-positive kidney transplant patients. Transplantation. 2011;91(2):237–44. https://doi.org/10.1097/TP.0b013e318200000c.
Puttarajappa CM, Mehta RB, Roberts MS, et al. Economic analysis of screening for subclinical rejection in kidney transplantation using protocol biopsies and noninvasive biomarkers. Am J Transplant. 2021;21(1):186–97. https://doi.org/10.1111/ajt.16150 (published Online First: 20200715).
McLaughlin K, Manns B, Nickerson P. The routine use of high-resolution immunological screening of recipients of primary deceased donor kidney allografts is cost-effective. Transplantation. 2006;81(9):1278–84. https://doi.org/10.1097/01.tp.0000205797.05544.e5.
Liem YS, Kock MC, Ijzermans JN, et al. Living renal donors: optimizing the imaging strategy–decision- and cost-effectiveness analysis. Radiology. 2003;226(1):53–62. https://doi.org/10.1148/radiol.2261011893.
de Vries EF, Rabelink TJ, van den Hout WB. Modelling the cost-effectiveness of delaying end-stage renal disease. Nephron. 2016;133(2):89–97. https://doi.org/10.1159/000446548 (published Online First: 20160608).
Lee CP, Chertow GM, Zenios SA. A simulation model to estimate the cost and effectiveness of alternative dialysis initiation strategies. Med Decis Making. 2006;26(5):535–49. https://doi.org/10.1177/0272989X06290488.
McLaughlin K, Manns B, Culleton B, et al. An economic evaluation of early versus late referral of patients with progressive renal insufficiency. Am J Kidney Dis. 2001;38(5):1122–8. https://doi.org/10.1053/ajkd.2001.28619.
Villa G, Sanchez-Alvarez E, Cuervo J, et al. Cost-effectiveness analysis of timely dialysis referral after renal transplant failure in Spain. BMC Health Serv Res. 2012;12:257. https://doi.org/10.1186/1472-6963-12-257 (published Online First: 20120816).
Yen EF, Hardinger K, Brennan DC, et al. Cost-effectiveness of extending Medicare coverage of immunosuppressive medications to the life of a kidney transplant. Am J Transplant. 2004;4(10):1703–8. https://doi.org/10.1111/j.1600-6143.2004.00565.x.
Shelton BA, Sawinski D, Linas BP, et al. Population level outcomes and cost-effectiveness of hepatitis C treatment pre- vs postkidney transplantation. Am J Transplant. 2018;18(10):2483–95. https://doi.org/10.1111/ajt.15040 (published Online First: 20180830).
Simon DG. A cost-effectiveness analysis of cyclosporine in cadaveric kidney transplantation. Med Decis Making. 1986;6(4):199–207. https://doi.org/10.1177/0272989X8600600403.
Shimizu U, Saito S, Lings Y, et al. Cost-effectiveness achieved through changing the composition of renal replacement therapy in Japan. J Med Econ. 2012;15(3):444–53. https://doi.org/10.3111/13696998.2011.653512 (published Online First: 20120207).
Rodina-Theocharaki A, Bliznakova K, Pallikarakis N. Markov Chain Monte Carlo simulation for projection of end stage renal disease patients in Greece. Comput Methods Programs Biomed. 2012;107(1):90–6. https://doi.org/10.1016/j.cmpb.2011.09.012 (published Online First: 20111022).
Groen H, Moers C, Smits JM, et al. Cost-effectiveness of hypothermic machine preservation versus static cold storage in renal transplantation. Am J Transplant. 2012;12(7):1824–30. https://doi.org/10.1111/j.1600-6143.2012.04030.x (published Online First: 20120511).
Eckman MH, Talal AH, Gordon SC, et al. Cost-effectiveness of screening for chronic hepatitis C infection in the United States. Clin Infect Dis. 2013;56(10):1382–93. https://doi.org/10.1093/cid/cit069 (published Online First: 20130207).
Axelrod DA, Schnitzler MA, Xiao H, et al. An economic assessment of contemporary kidney transplant practice. Am J Transplant. 2018;18(5):1168–76. https://doi.org/10.1111/ajt.14702 (published Online First: 20180331).
McEwan P, Dixon S, Baboolal K, et al. Evaluation of the cost effectiveness of sirolimus versus tacrolimus for immunosuppression following renal transplantation in the UK. Pharmacoeconomics. 2006;24(1):67–79. https://doi.org/10.2165/00019053-200624010-00006.
Abecassis MM, Seifeldin R, Riordan ME. Patient outcomes and economics of once-daily tacrolimus in renal transplant patients: results of a modeling analysis. Transplant Proc. 2008;40(5):1443–5. https://doi.org/10.1016/j.transproceed.2008.03.090.
Earnshaw SR, Graham CN, Irish WD, et al. Lifetime cost-effectiveness of calcineurin inhibitor withdrawal after de novo renal transplantation. J Am Soc Nephrol. 2008;19(9):1807–16. https://doi.org/10.1681/ASN.2007040495 (published Online First: 20080618).
Eckman MH, Woodle ES, Thakar CV, et al. Cost-effectiveness of using kidneys from HCV-viremic donors for transplantation into HCV-uninfected recipients. Am J Kidney Dis. 2020;75(6):857–67. https://doi.org/10.1053/j.ajkd.2019.11.005 (published Online First: 20200217).
Kadatz M, Gill JS, Gill J, et al. Economic evaluation of extending medicare immunosuppressive drug coverage for kidney transplant recipients in the current era. J Am Soc Nephrol. 2020;31(1):218–28. https://doi.org/10.1681/ASN.2019070646 (published Online First: 20191108).
Orme ME, Jurewicz WA, Kumar N, et al. The cost effectiveness of tacrolimus versus microemulsified cyclosporin: a 10-year model of renal transplantation outcomes. Pharmacoeconomics. 2003;21(17):1263–76. https://doi.org/10.2165/00019053-200321170-00003.
Snowsill TM, Moore J, Mujica Mota RE, et al. Immunosuppressive agents in adult kidney transplantation in the National Health Service: a model-based economic evaluation. Nephrol Dial Transplant. 2017;32(7):1251–9. https://doi.org/10.1093/ndt/gfx074.
Jassal SV, Krahn MD, Naglie G, et al. Kidney transplantation in the elderly: a decision analysis. J Am Soc Nephrol. 2003;14(1):187–96. https://doi.org/10.1097/01.asn.0000042166.70351.57.
Kadatz M, Klarenbach S, Gill J, et al. Cost-effectiveness of using kidneys from hepatitis C nucleic acid test-positive donors for transplantation in hepatitis C-negative recipients. Am J Transplant. 2018;18(10):2457–64. https://doi.org/10.1111/ajt.14929 (published Online First: 20180614).
Morton RL, Howard K, Webster AC, et al. The cost-effectiveness of induction immunosuppression in kidney transplantation. Nephrol Dial Transplant. 2009;24(7):2258–69. https://doi.org/10.1093/ndt/gfp174 (published Online First: 20090417]).
Hua DK, Howard K, Craig JC, et al. Cost-effectiveness of cidofovir treatment of polyomavirus nephropathy in kidney transplant recipients. Transplantation. 2012;93(2):188–94. https://doi.org/10.1097/TP.0b013e31823e7b0e.
de Wit GA, Ramsteijn PG, de Charro FT. Economic evaluation of end stage renal disease treatment. Health Policy. 1998;44(3):215–32. https://doi.org/10.1016/s0168-8510(98)00017-7.
Cavallo MC, Sepe V, Conte F, et al. Cost-effectiveness of kidney transplantation from DCD in Italy. Transplant Proc. 2014;46(10):3289–96. https://doi.org/10.1016/j.transproceed.2014.09.146.
Bianic F, Campbell R, Damera V, et al. Cost-effectiveness of everolimus plus reduced tacrolimus in de novo liver-recipients in the Italian setting. J Med Econ. 2016;19(9):866–73. https://doi.org/10.1080/13696998.2016.1179199 (published Online First: 20160512).
Zhang Y, Briggs D, Lowe D, et al. A new data-driven model for post-transplant antibody dynamics in high risk kidney transplantation. Math Biosci. 2017;284:3–11. https://doi.org/10.1016/j.mbs.2016.04.008 (published Online First: 20160514).
Keizer KM, de Klerk M, Haase-Kromwijk BJ, et al. The Dutch algorithm for allocation in living donor kidney exchange. Transplant Proc. 2005;37(2):589–91. https://doi.org/10.1016/j.transproceed.2004.12.096.
Kim BS, Kim YS, Kim SI, et al. Outcome of multipair donor kidney exchange by a web-based algorithm. J Am Soc Nephrol. 2007;18(3):1000–6. https://doi.org/10.1681/ASN.2006101071 (published Online First: 20070131).
Kaplan I, Houp JA, Montgomery RA, et al. A computer match program for paired and unconventional kidney exchanges. Am J Transplant. 2005;5(9):2306–8. https://doi.org/10.1111/j.1600-6143.2005.00991.x.
Hanto RL, Reitsma W, Delmonico FL. The development of a successful multiregional kidney paired donation program. Transplantation. 2008;86(12):1744–8. https://doi.org/10.1097/TP.0b013e3181909035.
Constantino M, Klimentova X, Viana A, et al. New insights on integer-programming models for the kidney exchange problem. Eur J Oper Res. 2013;231(1):57–68.
Kurt M, Roberts M, Schaefer A, et al. Valuing prearranged paired kidney exchanges: a stochastic game approach. Boston College Department of Economics; 2011.
Davis AE, Mehrotra S, Friedewald JJ, et al. Improving geographic equity in kidney transplantation using alternative kidney sharing and optimization modeling. Med Decis Making. 2015;35(6):797–807. https://doi.org/10.1177/0272989X14557696 (published Online First: 20141110).
Ahmadvand S, Pishvaee MS. An efficient method for kidney allocation problem: a credibility-based fuzzy common weights data envelopment analysis approach. Health Care Manag Sci. 2018;21(4):587–603. https://doi.org/10.1007/s10729-017-9414-6 (published Online First: 20170809).
Alalouf A, David I, Pliskin J. Computing the probabilities of HLA-like matching. Ann Oper Res. 2014;221(1):33–45. https://doi.org/10.1007/s10479-011-1049-2.
Bohmig GA, Fidler S, Christiansen FT, et al. Transnational validation of the Australian algorithm for virtual crossmatch allocation in kidney paired donation. Hum Immunol. 2013;74(5):500–5. https://doi.org/10.1016/j.humimm.2013.01.029 (published Online First: 20130201).
Schaafsma M, van der Deijl W, Smits JM, et al. Decision tables and rule engines in organ allocation systems for optimal transparency and flexibility. Transpl Int. 2011;24(5):433–40. https://doi.org/10.1111/j.1432-2277.2011.01221.x (published Online First: 20110203).
Sousa LC, Filho HL, Von Glehn CQ, et al. EpHLA: an innovative and user-friendly software automating the HLAMatchmaker algorithm for antibody analysis. Transpl Immunol. 2011;25(4):210–6. https://doi.org/10.1016/j.trim.2011.08.008 (published Online First: 20110910).
Su X, Zenios SA, Chakkera H, et al. Diminishing significance of HLA matching in kidney transplantation. Am J Transplant. 2004;4(9):1501–8. https://doi.org/10.1111/j.1600-6143.2004.00535.x.
Anderson R, Ashlagi I, Gamarnik D, et al. Finding long chains in kidney exchange using the traveling salesman problem. Proc Natl Acad Sci. 2015;112(3):663–8. https://doi.org/10.1073/pnas.1421853112.
Ross LF, Parker W, Veatch RM, et al. Equal Opportunity Supplemented by Fair Innings: equity and efficiency in allocating deceased donor kidneys. Am J Transplant. 2012;12(8):2115–24. https://doi.org/10.1111/j.1600-6143.2012.04141.x (published Online First: 20120615).
Fumo DE, Kapoor V, Reece LJ, et al. Historical matching strategies in kidney paired donation: the 7-year evolution of a web-based virtual matching system. Am J Transplant. 2015;15(10):2646–54. https://doi.org/10.1111/ajt.13337 (published Online First: 2015/05/26).
Sonmez et al. Enhancing the Efficiency of and Equity in Transplant Organ Allocation via Incentivized Exchange SSRN: https://ssrncom/abstract=2551344 or http://dxdoiorg/https://doi.org/10.2139/ssrn2551344. 2015
Li Y, Song PX, Zhou Y, et al. Optimal decisions for organ exchanges in a kidney paired donation program. Stat Biosci. 2014;6(1):85–104. https://doi.org/10.1007/s12561-013-9082-0.
Klimentova X, Pedroso JP, Viana A. Maximising expectation of the number of transplants in kidney exchange programmes. Comput Opera Res. 2016;73(C):1–11. https://doi.org/10.1016/j.cor.2016.03.004.
Offermann G. HLA-based local donor/recipient matching in renal transplantation: a microcomputer program. Int J Biomed Comput. 1988;22(3):251–7. https://doi.org/10.1016/0020-7101(88)90079-7.
Ashlagi I, Gilchrist DS, Roth AE, et al. Nonsimultaneous chains and dominos in kidney-paired donation-revisited. Am J Transplant. 2011;11(5):984–94. https://doi.org/10.1111/j.1600-6143.2011.03481.x.
Bray M, Wang W, Rees MA, et al. KPDGUI: An interactive application for optimization and management of a virtual kidney paired donation program. Comput Biol Med. 2019;108:345–53. https://doi.org/10.1016/j.compbiomed.2019.03.013 (published Online First: 20190316).
Bertsimas D, Farias VF, Trichakis N. Fairness, efficiency, and flexibility in organ allocation for kidney transplantation. Oper Res. 2013;61(1):73–87.
Lonze BE, Dagher NN, Simpkins CE, Locke JE, Segev DL, Singer AL, Hiller J, Collins V, Montgomery RA. 100 kidney transplants performed via kidney paired donation at the Johns Hopkins hospital. Transplantation Journal. 2010;90:60.
Dickerson JP. Robust dynamic optimization with application to kidney exchange. In: Proceedings of the 2014 international conference on Autonomous agents and multi-agent systems 2014 May 5, pp. 1701–1702.
Abraham DJ, Blum A, Sandholm T. Clearing algorithms for barter exchange markets: Enabling nationwide kidney exchanges. In: Proceedings of the 8th ACM conference on Electronic commerce 2007 Jun 11, pp. 295–304.
Awasthi P, Sandholm T. Online stochastic optimization in the large: Application to kidney exchange. In: Twenty-first international joint conference on artificial intelligence 2009 Jun 24.
Segev DL, Gentry SE, Melancon JK, et al. Characterization of waiting times in a simulation of kidney paired donation. Am J Transplant. 2005;5(10):2448–55. https://doi.org/10.1111/j.1600-6143.2005.01048.x.
Devi SP, Kumar SS, Rao KS. Evaluation of kidney transplantation programmes using system simulation. J Med Syst. 2012;36(3):1117–31. https://doi.org/10.1007/s10916-010-9574-0 (published Online First: 20100901).
Taranto SE, Harper AM, Edwards EB, Rosendale JD, McBride MA, Daily OP, Murphy D, Poos B, Reust J, Schmeiser B. Developing a national allocation model for cadaveric kidneys. In: Proceedings of the 2000 Winter Simulation Conference Proceedings (Cat. No. 00CH37165) 2000 Dec 10, vol. 2, pp. 1971–1977. IEEE.
Zenios SA, Chertow GM, Wein LM. Dynamic allocation of kidneys to candidates on the transplant waiting list. Oper Res. 2000;48(4):549–69.
Harvey C. The kidney transplant process model (KTPM) simulation tool for the transplant process. In: Proceedings of the summer computer simulation conference 2016 Jul 24, pp. 1–8.
Santos N, Tubertini P, Viana A, et al. Kidney exchange simulation and optimization. J Oper Res Soc. 2017;68(12):1521–32. https://doi.org/10.1057/s41274-016-0174-3.
Yahav I, Shmueli G. Outcomes matter: estimating pre-transplant survival rates of kidney-transplant patients using simulator-based propensity scores. Ann Oper Res. 2014;216(1):101–28. https://doi.org/10.1007/s10479-013-1359-7.
Bolger PG, Davies R. Simulation model for planning renal services in a district health authority. BMJ. 1992;305(6854):605–8. https://doi.org/10.1136/bmj.305.6854.605.
Davies H, Davies R. A simulation model for planning services for renal patients in Europe. J Oper Res Soc. 1987;38(8):693–700. https://doi.org/10.1057/jors.1987.118.
Dominguez J, Harrison R, Atal R, et al. A new kidney allocation policy in Chile: computer-based simulations. Transplant Proc. 2013;45(4):1313–5. https://doi.org/10.1016/j.transproceed.2013.01.012.
Roderick P, Davies R, Jones C, et al. Simulation model of renal replacement therapy: predicting future demand in England. Nephrol Dial Transplant. 2004;19(3):692–701. https://doi.org/10.1093/ndt/gfg591.
Dominguez J, Harrison R, Contreras D. Effectiveness of different kidney exchange mechanisms to improve living donor transplantation in Chile. Transplant Proc. 2011;43(6):2283–7. https://doi.org/10.1016/j.transproceed.2011.06.001.
Jacquelinet C, Audry B, Golbreich C, et al. Changing kidney allocation policy in France: the value of simulation. AMIA Annu Symp Proc. 2006;2006:374–8.
Wujciak T, Opelz G. Computer analysis of cadaver kidney allocation procedures. Transplantation. 1993;55(3):516–21.
Yuan Y, Gafni A, Russell JD, et al. Development of a central matching system for the allocation of cadaveric kidneys: a simulation of clinical effectiveness versus equity. Med Decis Making. 1994;14(2):124–36. https://doi.org/10.1177/0272989X9401400205.
Saidman SL, Roth AE, Sönmez T, et al. Increasing the opportunity of live kidney donation by matching for two- and three-way exchanges. Transplantation. 2006;81(5):773–82. https://doi.org/10.1097/01.tp.0000195775.77081.25.
Su X, Zenios SA, Chertow GM. Incorporating recipient choice in kidney transplantation. J Am Soc Nephrol. 2004;15(6):1656–63. https://doi.org/10.1097/01.asn.0000127866.34592.60.
Roth AE, Sönmez T, Unver MU, et al. Utilizing list exchange and nondirected donation through “chain” paired kidney donations. Am J Transplant. 2006;6(11):2694–705. https://doi.org/10.1111/j.1600-6143.2006.01515.x (published Online First: 20060918).
Segev DL, Gentry SE, Warren DS, et al. Kidney paired donation and optimizing the use of live donor organs. JAMA. 2005;293(15):1883–90. https://doi.org/10.1001/jama.293.15.1883.
Ding Y, Ge D, He S, et al. A nonasymptotic approach to analyzing kidney exchange graphs. Oper Res. 2018;66(4):918–35.
Anderson R, Ashlagi I, Gamarnik D, et al. Kidney exchange and the alliance for paired donation: operations research changes the way kidneys are transplanted. INFORMS J Appl Analyt. 2015;45(1):26–42. https://doi.org/10.1287/inte.2014.0766.
Ata B, Skaro A, Tayur S. OrganJet: overcoming geographical disparities in access to deceased donor kidneys in the United States. Manag Sci. 2016;63(9):2776–94. https://doi.org/10.1287/mnsc.2016.2487.
Davis A, Mehrotra S, Friedewald J, Ladner D. Characteristics of a simulation model of the national kidney transplantation system. In: Proceedings of the 2013 Winter Simulations Conference (WSC) 2013 Dec 8, pp. 2320–2329. IEEE.
Sabouri A, Huh WT, Shechter SM. Screening strategies for patients on the kidney transplant waiting list. Oper Res. 2017;65(5):1131–46. https://doi.org/10.1287/opre.2017.1632.
Motohashi Y, Nishi S. Prediction of end-stage renal disease patient population in Japan by system dynamics model. Int J Epidemiol. 1991;20(4):1032–6. https://doi.org/10.1093/ije/20.4.1032.
Zhao L, Shi J, Shearon TH, et al. A Dirichlet process mixture model for survival outcome data: assessing nationwide kidney transplant centers. Stat Med. 2015;34(8):1404–16. https://doi.org/10.1002/sim.6438 (published Online First: 20150126).
Gheorghian A, Schnitzler M, Axelrod D, Salvalaggio P, Xiao H, Segev D, Gentry S, Lentine K. The economic value of preemptive living donor kidney transplantation. In: American Journal of Transplantation 2010;10:66–6. Commerce place, 350 main st, Malden 02148, MA USA: Wiley-Blackwell Publishing, Inc.
Su X, Zenios SA. Patient choice in kidney allocation: a sequential stochastic assignment model. Oper Res. 2005;53(3):443–55. https://doi.org/10.1287/opre.1040.0180.
Van Arendonk KJ, Chow EK, James NT, Orandi BJ, Ellison TA, Smith JM, Colombani PM, Segev DL. Choosing the order of deceased donor and living donor kidney transplantation in pediatric recipients: a Markov decision process model. Transplantation. 2015;99(2):360-66.
Chow EK, Massie AB, Muzaale AD, et al. Identifying appropriate recipients for CDC infectious risk donor kidneys. Am J Transplant. 2013;13(5):1227–34. https://doi.org/10.1111/ajt.12206.
Ortiz F, Finne P, Sandholm U, Roennholm K. Effectiveness of the finnish model of adolescent transition to adult care in kidney transplant recipients. In: Transplant international 2015;28:115–115. 111 RIVER ST, HOBOKEN 07030-5774, NJ USA: WILEY-BLACKWELL.
Martínez-Camblor P, de Uña-Álvarez J, Corte CD. Expanded renal transplantation: a competing risk model approach. J Appl Stat. 2015;42(12):2539–53. https://doi.org/10.1080/02664763.2015.1043866.
Begun A, Icks A, Waldeyer R, et al. Identification of a multistate continuous-time nonhomogeneous Markov chain model for patients with decreased renal function. Med Decis Making. 2013;33(2):298–306. https://doi.org/10.1177/0272989x12466731 (published Online First: 20121228).
Couchoud C, Dantony E, Elsensohn MH, et al. Modelling treatment trajectories to optimize the organization of renal replacement therapy and public health decision-making. Nephrol Dial Transplant. 2013;28(9):2372–82. https://doi.org/10.1093/ndt/gft204 (published Online First: 20130619).
Roth AE, Sönmez T, Utku ÜM. Pairwise kidney exchange. Journal of Economic Theory. 2005;125(2):151–88. https://doi.org/10.1016/j.jet.2005.04.004.
Massie AB, Boyarsky BJ, Werbel WA, et al. Identifying scenarios of benefit or harm from kidney transplantation during the COVID-19 pandemic: a stochastic simulation and machine learning study. Am J Transplant. 2020;20(11):2997–3007. https://doi.org/10.1111/ajt.16117[publishedOnlineFirst:20200715].
Zenios SA. Optimal control of a paired-kidney exchange program. Manag Sci. 2002;48(3):328–42.
Ge R, Liu S, Duan XD. A queuing model of time waiting based on kidney transplantation. In: Proceedings of the 21st annual international conference on Chinese Control and Decision Conference 2009 Jun 17. pp. 1509–1514.
Elalouf A, Perlman Y, Yechiali U. A double-ended queueing model for dynamic allocation of live organs based on a best-fit criterion. Appl Math Model. 2018;60:179–91. https://doi.org/10.1016/j.apm.2018.03.022.
Abellán JJ, Armero C, Conesa D, et al. Analysis of the renal transplant waiting list in the País Valencià (Spain). Stat Med. 2006;25(2):345–58. https://doi.org/10.1002/sim.2217.
Su X, Zenios S. Patient choice in kidney allocation: the role of the queueing discipline. Manuf Serv Oper Manag. 2004;6(4):280–301. https://doi.org/10.1287/msom.1040.0056.
Alta B, Ding Y, Zenios S. KDPI-dependent ranking policies: shaping the allocation of deceased-donor kidneys in the new era. Stanford: Stanford Graduate School of Business; 2017.
Bandi C, Trichakis N, Vayanos P. Robust multiclass queuing theory for wait time estimation in resource allocation systems. Manag Sci. 2018;65(1):152–87. https://doi.org/10.1287/mnsc.2017.2948.
Su X, Zenios SA. Recipient choice can address the efficiency-equity trade-off in kidney transplantation: a mechanism design model. Manag Sci. 2006;52(11):1647–60. https://doi.org/10.1287/mnsc.1060.0541.
Reinaldo F, Rahman MA, Alves CF, Malucelli A, Camacho R. Machine learning support for kidney transplantation decision making. In: Proceedings of the international symposium on biocomputing 2010 Feb 15. pp. 1–4.
Brown TS, Elster EA, Stevens K, et al. Bayesian modeling of pretransplant variables accurately predicts kidney graft survival. Am J Nephrol. 2012;36(6):561–9. https://doi.org/10.1159/000345552 (published Online First: 20121205).
Mark E, Goldsman D, Keskinocak P, Gurbaxani B. Using Machine Learning and Simulation to Compare High Risk Kidney Transplant Survival to Waiting for a Non High Risk Organ. In: American Journal of Transplantation 2018;18:532–32. 111 RIVER ST, HOBOKEN 07030-5774, NJ USA: WILEY.
Dovgan E, Gradišek A, Luštrek M, et al. Using machine learning models to predict the initiation of renal replacement therapy among chronic kidney disease patients. PLoS ONE. 2020;15(6): e0233976. https://doi.org/10.1371/journal.pone.0233976.
Caruso V, Daniele P. A network model for minimizing the total organ transplant costs. Eur J Oper Res. 2018;266(2):652–62.
Desai VCA, Ferrand Y, Cavanaugh TM, et al. Comparative effectiveness of tacrolimus-based steroid sparing versus steroid maintenance regimens in kidney transplantation: results from discrete event simulation. Med Decis Making. 2017;37(7):827–43. https://doi.org/10.1177/0272989X17700879 (published Online First: 20170406).
Djebli N, Rousseau A, Hoizey G, et al. Sirolimus population pharmacokinetic/pharmacogenetic analysis and bayesian modelling in kidney transplant recipients. Clin Pharmacokinet. 2006;45(11):1135–48. https://doi.org/10.2165/00003088-200645110-00007.
Frobel AK, Karlsson MO, Backman JT, et al. A time-to-event model for acute rejections in paediatric renal transplant recipients treated with ciclosporin A. Br J Clin Pharmacol. 2013;76(4):603–15. https://doi.org/10.1111/bcp.12121.
Jassal SV, Lok CE, Walele A, et al. Continued transplant immunosuppression may prolong survival after return to peritoneal dialysis: results of a decision analysis. Am J Kidney Dis. 2002;40(1):178–83. https://doi.org/10.1053/ajkd.2002.33927.
Saint-Marcoux F, Debord J, Undre N, et al. Pharmacokinetic modeling and development of Bayesian estimators in kidney transplant patients receiving the tacrolimus once-daily formulation. Ther Drug Monit. 2010;32(2):129–35. https://doi.org/10.1097/FTD.0b013e3181cc70db.
Sy SK, Heuberger J, Shilbayeh S, et al. A Markov chain model to evaluate the effect of CYP3A5 and ABCB1 polymorphisms on adverse events associated with tacrolimus in pediatric renal transplantation. AAPS J. 2013;15(4):1189–99. https://doi.org/10.1208/s12248-013-9528-9 (published Online First: 20130830).
Liem YS, Wong JB, Winkelmayer WC, et al. Quantifying the benefit of early living-donor renal transplantation with a simulation model of the Dutch renal replacement therapy population. Nephrol Dial Transplant. 2012;27(1):429–34. https://doi.org/10.1093/ndt/gfr294 (published Online First: 20110523]).
Chang Y, Gallon L, Shetty K, et al. Simulation modeling of the impact of proposed new simultaneous liver and kidney transplantation policies. Transplantation. 2015;99(2):424–30. https://doi.org/10.1097/TP.0000000000000270.
Levy AR, Briggs AH, Johnston K, et al. Projecting long-term graft and patient survival after transplantation. Value Health. 2014;17(2):254–60. https://doi.org/10.1016/j.jval.2014.01.001.
Choudhury RA, Prins K, Dor Y, et al. Uncontrolled donation after circulatory death improves access to kidney transplantation: a decision analysis. Clin Transplant. 2020;34(7): e13868. https://doi.org/10.1111/ctr.13868.
McLean DR, Jardine AG. A simulation model to investigate the impact of cardiovascular risk in renal transplantation. Transplant Proc. 2005;37(5):2135–43. https://doi.org/10.1016/j.transproceed.2005.03.057.
Anunciacao FA, Sousa LC, da Silva AS, et al. EpViX: a cloud-based tool for epitope reactivity analysis and epitope virtual crossmatching to identify low immunologic risk donors for sensitized recipients. Transpl Immunol. 2015;33(3):153–8. https://doi.org/10.1016/j.trim.2015.09.006 (published OnlineFirst: 20151101).
Tsai WC, Wu HY, Peng YS, et al. Risk Factors for development and progression of chronic kidney disease: a systematic review and exploratory meta-analysis. Medicine (Baltimore). 2016;95(11): e3013. https://doi.org/10.1097/MD.0000000000003013.
Caulfield T, Murdoch B, Sapir-Pichhadze R, et al. Policy challenges for organ allocation in an era of “Precision Medicine.” Can J Kidney Health Dis. 2020;7:2054358120912655. https://doi.org/10.1177/2054358120912655 (published Online First: 20200320).
Noordzij M, Leffondre K, van Stralen KJ, et al. When do we need competing risks methods for survival analysis in nephrology? Nephrol Dial Transplant. 2013;28(11):2670–7. https://doi.org/10.1093/ndt/gft355 (published Online First: 20130824).
Sapir-Pichhadze R, Pintilie M, Tinckam KJ, et al. Survival analysis in the presence of competing risks: the example of waitlisted kidney transplant candidates. Am J Transplant. 2016;16(7):1958–66. https://doi.org/10.1111/ajt.13717 (published Online First: 20160303).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Genome BC (Genome Canada 273AMR) and the Canadian Institutes of Health Research (CIHR GP1-155871).
Conflicts of interest
None.
Ethics approval
The Can-Prevent AMR study was approved by the University of British Columbia’s Research Ethics Board (H18-00090).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
MY, LE, SB, SS, MDW, RSP and PK designed the study. MDW designed and performed the database searches. MY and LE reviewed the studies and extracted the data. SB, MY, LE, SC and SS analysed the results. All authors contributed to drafting the manuscript and preparing it for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yaghoubi, M., Cressman, S., Edwards, L. et al. A Systematic Review of Kidney Transplantation Decision Modelling Studies. Appl Health Econ Health Policy 21, 39–51 (2023). https://doi.org/10.1007/s40258-022-00744-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-022-00744-x