Abstract
Objectives
The main objective of this study was to derive cost estimates of five major foodborne illnesses (campylobacteriosis, salmonellosis, enterohemorrhagic Escherichia coli (EHEC), yersiniosis and shigellosis) in Sweden. These estimates provide a necessary contribution to perform future cost-benefit analyses aimed at reducing the burden of foodborne disease. A secondary aim was to obtain estimates of the true number of cases that occur in the community, thus providing necessary ground for calculating costs.
Methods
The true number of cases for each foodborne illness was simulated by multiplying the reported number of cases by sequential multipliers, one for each potential source of information loss about a case. This assessment of the true number of cases was then used to estimate the number of cases of sequelae for each illness. An incidence-based analysis was then used to calculate direct medical and non-medical costs, as well as indirect costs. Data for estimating the true number of cases for each illness were primarily based on an expert panel, while the derivation of costs mainly utilized national registries, databases and published literature.
Results
The estimated number of cases was between 7- and 11-fold higher than the reported number of cases, indicating the importance of taking information loss into account when calculating costs. By far the most common pathogen of the five was campylobacter, with an estimated 101,719 (90% credibility interval [CI] 59,640–158,025) human cases occurring annually. For salmonella, 19,678 (90% CI 8394–40,456) cases were estimated to occur each year, while the other three pathogens were less common, with a yearly incidence of approximately 2500–5500 cases each. The total cost for the five pathogens (including sequelae) amounted to €142 million annually. Campylobacter was the most costly pathogen, representing 69% of the total costs. Salmonellosis and EHEC constituted 18 and 9% of these costs, respectively, while yersiniosis and shigellosis represented approximately 2% each. Costs for sequelae were significant and accounted for approximately 50% of the total costs.
Conclusions
Our simulations indicated that campylobacter infection was more common and more costly than salmonella, EHEC, yersinia and shigella combined. Estimated costs for all illnesses were highly influenced by (1) considering potential information losses about cases in the population (which increased costs 7- to 11-fold), and (2) taking account of post-infection sequelae (which doubled the costs).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study estimates the difference between registered and actual number of cases in the community for five major foodborne diseases. Potential post-infection sequelae are included in the analysis. These considerations are crucial in order to assess the actual societal burden of the five pathogens. |
The study also estimates total societal costs and costs per case for the five pathogens, results that can be utilized in future cost-benefit or cost-effectiveness studies. |
1 Introduction
Food-related illnesses result in costs for individuals, industries and society as a whole [1]. Knowing the extent of these costs is pertinent in order to efficiently control the illnesses. Two general methods have been proposed in the literature to quantify disease-related costs in monetary terms. First, the willingness-to-pay (WTP) technique estimates the maximum amount that individuals are prepared to pay in order to reduce the risk of morbidity or mortality caused by specific diseases. These individual costs can then be used to obtain values of statistical cases (VSCs) and statistical lives (VSLs). Multiplying these measures by the number of cases and deaths associated with a particular illness yields an aggregated cost estimate for a disease that can be used in, for example, cost-benefit analyses (CBAs). On the other hand, the cost-of-illness (COI) method uses available statistics to add direct costs (healthcare expenditure) and indirect costs (productivity loss due to unworked days) to obtain a similar cost estimate of an illness. Of these two methods, the COI method is currently the most commonly used to estimate the aggregate economic costs of foodborne illnesses [2].
Since the two methods represent fundamentally different approaches, they do not measure the same thing. The COI method (used in this study) captures direct and indirect costs but disregards intangible costs perceived by individuals, such as pain, suffering and sorrow. COI may therefore be viewed as mainly the financial costs of an illness. In Sweden, COI has previously been calculated for campylobacter and enterohemorrhagic Escherichia coli (EHEC), including a limited number of sequelae [3]. The method has also been used to test whether the Swedish salmonella control program should be modified based on a CBA [4]. On the other hand, the WTP approach includes intangible costs but only considers those parts of the direct and indirect costs that directly affect an individual. Since healthcare can be more or less heavily subsidized, and since sick leave is at least partially covered by compulsory insurance in many countries, there are major parts of direct and indirect costs that do not affect individuals, and will therefore not be included in the WTP measure. Thus, in reality, neither of the two measures will generally cover all costs derived from an illness [5].
One approach that is used to overcome these problems is to combine the two measures, using COI to estimate direct and indirect costs, and WTP to estimate intangible costs [6]. However, this approach can be problematic if the WTP elicitation includes parts of the direct and indirect costs already accounted for by the COI. Therefore, to avoid double-counting errors, care has to be taken so that the WTP measure isolates the intangible costs [5]. In Sweden, the WTP method has previously been employed to calculate WTP and VSCs for salmonella [7].
Both methods described above yield costs per case of an illness. To aggregate this to the national level, it is necessary to know the incidence of an illness, i.e. the number of cases that occur annually. For the five illnesses analyzed in this paper, it is compulsory to report them to the Public Health Agency in Sweden, both for the physician carrying out the examination and the laboratory that performs the tests.
However, the number of reported cases generally underestimates the actual number of cases in the community [8]. This underestimation (UE) of cases is illustrated in terms of a morbidity surveillance pyramid (see Fig. 1). The base of the pyramid holds all infections (both symptomatic and asymptomatic) in the community. At each new level there is a potential loss of information about a case. First, asymptomatic cases and cases with mild symptoms may not seek healthcare at all, and are thus not captured by any surveillance system. This is the underascertainment (UA) part of the UE. The UA may be a particularly severe problem for infectious diseases (IDs) since the self-limiting course of these illnesses may lead to less people seeking care [9]. Second, cases that do seek healthcare may not be reported for a number of reasons: stool samples are not taken, samples are not analyzed for the illness at hand, the test is falsely negative, or a positive result is not reported. This is the underreporting (UR) part of the UE [9]. The fraction between the number of reported cases (the tip) and all infections in the community (the base) is often referred to as the multiplication factor (MF). However, in terms of societal costs, the asymptomatic cases are usually ignored when calculating the MF.
Various methods have been developed in the literature to overcome the UE problem by approximating the true number of cases of IDs. Several studies have utilized community cohorts to obtain sample-based estimates of UE [10,11,12]. When using this method, participants are contacted on a frequent basis and asked whether they have experienced typical ID symptoms such as diarrhea and vomiting. If they have, they are asked further questions and are requested to provide stool samples in order to determine etiology. Thus, the proportion of the cohort that gets infected with different causative agents can be estimated. If the sample is truly representative and if all cases in the cohort can be traced in this manner, the estimates can be scaled up to the entire population where the ‘true’ incidence can thus be calculated. Comparing this estimated incidence with the reported incidence (from national surveillance systems) for each illness makes it possible to calculate the UE and the MF. Various forms of biases (which may lead to unrepresentative samples), as well as difficulties in determining etiology (which may lead to a UE of the number of cases), are factors that need to be carefully considered using this methodology [9].
One variant of the community cohort method is to use serological surveys to measure sero-incidence (the rate of new infections) by testing a cohort for antibody positivity relative to an illness. The method thus measures both symptomatic and asymptomatic cases. By using threshold values for antibody concentration (in cases where these are known), it is also possible to approximate the number of symptomatic cases using this methodology [9]. The method has been used to investigate the effects on the number of cases following a less strict Swedish salmonella control program [13].
Apart from the biases mentioned above, another problem with the community cohort method is that it generally requires large resources to carry out. This problem prevents it from being performed in many countries [14]. An alternative, which is used in this paper, is to use stochastic modeling to obtain values of UE, UR, UA and MF. In short, this method uses available data, literature, and experts to estimate distributions for the probability of information loss at each stage of the morbidity pyramid in Fig. 1. By using stochastic simulation, the joint probability distribution that a case in the community gets reported can be obtained. This method has been used for Sweden in one previous study where the incidences of seven pathogens in seven European countries were examined [14]. However, some of the distribution parameters used in that study were based on very small samples and contradicted parameter values of all other countries. Furthermore, some parameters could only be roughly approximated by using non-Swedish samples. In the present study, all parameters have been estimated using native experts and published literature with large Swedish samples.
To summarize, the objective of this paper was to provide credible cost estimates of five of the most common food-related illnesses in Sweden using the COI methodology. To obtain this aim, we carefully took into account the two factors discussed above. Thus, we first created a model that accounted for UR errors by simulating the magnitude of various possible sources of information loss. The main merit of this approach is that UR factors are adapted to specific Swedish conditions and to each illness separately, which has not previously been made. Second, we estimated COI, not only for the main illnesses but also for four different sequelae that may follow from them. In conclusion, this approach is likely to yield a much more reliable cost estimation of these illnesses than has previously been available. Furthermore, it provides an essential basis for finding cost-efficient measures to reduce the health burden of these illnesses in the future.
2 Methods
2.1 Reconstructing the Morbidity Pyramids for the Main Illnesses
Most of the notation used in this section is provided in Fig. 2. Let the total number of reported cases (hospitalized and non-hospitalized) per year of illness, \(p\), be denoted by \(L_{p}\), and let the number of reported hospitalized cases be denoted by \(M_{p}\). Both \(L_{p}\) and \(M_{p}\) were calculated as averages for the years 2012–2016 [15, 16]. To account for UE, five different stages were identified where information about a symptomatic case in the population may disappear (see Fig. 2): (i) the carrier does not visit a general practitioner (GP); (ii) a sample is not taken; (iii) the sample is not analyzed for the particular illness at hand; (iv) the sample analysis does not detect the illness; and (v) positive test results are not reported. Note that the asymptomatic cases have been exempted from Fig. 2 (compared with Fig. 1) in accordance with the discussion in Sect. 1.
Variables and calculations related to the reconstruction of the morbidity pyramids. Variables A–F denote the following general probabilities, which are common for all pathogens: A probability of visiting a GP if having bloody diarrhea; B probability of having to submit a stool sample to a GP if having bloody diarrhea; C probability of visiting a GP if having non-bloody diarrhea; D probability of having to submit a stool sample to a GP if having non-bloody diarrhea; E probability of submitting a stool sample if hospitalized; F probability that a positive test result is reported. Variables G–J denote the following pathogen-specific probabilities: G probability of the submitted stool sample being analyzed (GP); H probability of the submitted stool sample being analyzed (hospital); I probability that the test will detect pathogen; J probability of having bloody diarrhea. p denotes an indexation of the pathogens. GP general practitioner
The different probabilities in Fig. 2 (A–J) were estimated using a Monte Carlo simulation methodology. The model ran 10,000 iterations, and for each iteration the probabilities were obtained by drawing randomly from constructed or fitted probability distributions (details are provided in Online Resource 1). In general, the distributions were based on expert opinion and published literature. The simulations were performed using an add-in to Microsoft Excel called RiskAMP©.
As depicted in Fig. 2, the probability of a carrier visiting a GP for illness \(p\) was calculated as a weighted average of the probability of visiting a GP if you experience bloody diarrhea (\(A\)) and non-bloody diarrhea (\(C\)). Notably, the probability of experiencing bloody diarrhea for illness \(p\), (\(J_{p}\)) was modeled by beta distributions that were fitted based on outbreak data. Most of the outbreak studies that were used were taken from a literature search made in a previous article [14]. Some further Swedish studies were then added before the distributions were fitted (see Online Resource 1 for details). The beta distributions were fitted using an add-in to Microsoft Excel called @Risk 5.0©.
A carrier who visits a GP may or may not be referred to a hospital for further examination. Since routines may differ between hospitals and outpatient departments, the model in some cases assumes different probability distributions for patients in those two types of institutions. This is reflected in Fig. 2, with the left part of the pyramid displaying probabilities for GP patients who are referred to a hospital, and the right part displaying probabilities for patients who only visit a GP. For example, hospitals generally have a higher proportion of severe cases and more routinely require stool samples. In the case of non-referrals, stool samples are mostly requested if a patient has bloody diarrhea. Thus, in Fig. 2, probability \(E\) is generally higher and independent of the presence of bloody diarrhea, while its GP-only counterpart is generally lower and calculated as a weighted average that depends on the presence of bloody diarrhea.
To obtain an estimation of the real number of patients who visit a GP with illness \(p\), referred to below as \({\text{RGP}}_{p}\), the reported number of cases is divided by the relevant probabilities of no information loss:
Similarly, to find an estimate of the real number of patients with illness \(p\) who are referred to a hospital \(\left( {{\text{RH}}_{p} } \right)\), the reported number of hospitalized patients is divided by the relevant probabilities of no information loss:
By adding \({\text{RGP}}_{p}\) and \({\text{RH}}_{p}\), we obtain the total number of carriers that seek care. By dividing this sum with the probability that carriers (with symptoms) seek care, we get an estimate of the total number of symptomatic cases in the population with illness \(p\) (\({\text{TC}}_{p}\)), which is what we need as an input into the COI calculations:
By dividing the actual number of cases by the reported number of cases for illness \(p\), we also obtain the multiplication factor of illness \(j\) (\({\text{MF}}_{p}\)):
2.2 Estimating Outcome Classes for the Main Illnesses
The symptoms of an illness may differ quite markedly between different carriers; some only experience mild and self-limiting symptoms, while others get much more severe and long-lasting problems and may require hospital care. These differences obviously also get reflected in the costs, which will vary with severity and duration. To take these differences into account, the model divides the total number of symptomatic cases \(({\text{TC}}_{p} )\) into four different outcome classes: no care, GP only, GP and hospital (no death), and GP and hospital (death). Note that in the Swedish health system, patients usually first visit a GP, who may or may not refer the patient to a hospital. It is therefore assumed that all hospitalized cases have also visited a GP. The calculations made to estimate the number of carriers in the different outcome classes are visualized in Fig. 3.
Calculations related to estimating outcome classes for the main pathogens. Description of variables used: \({\text{TC}}_{p} :\)total number of symptomatic cases in the population with illness \(p\), \({\text{RGP}}_{p}\): real number of patients who visit a GP with illness \(p\), \({\text{RH}}_{p}\): real number of patients with illness \(p\) who are referred to a hospital, \(K_{p}\): probability of death due to illness \(p\). GP general practitioner
The outcome class no care is calculated by simply subtracting the number of carriers seeking care from the total number of cases. The class GP only is calculated according to the previous section, while those cases that are referred to a hospital have been divided into two separate classes—those who survive and those who die.
2.3 Incidence and Event Trees for Sequelae
Four different post-infection sequelae were accounted for in this study: irritable bowel syndrome (IBS), reactive arthritis (ReA), hemolytic uremic syndrome (HUS) and Guillain–Barré syndrome (GBS). Based on several epidemiological studies and two systematic reviews, the first two of these illnesses were assumed to be possible sequelae of all main illnesses, while HUS and GBS were expected sequelae of only EHEC and campylobacter, respectively [17,18,19,20,21,22,23]. See Online Resource 1 for details of how the number of sequelae was determined in the model.
The incidences of post-infectious ReA, IBS, and HUS were calculated as proportions of the number of cases of the main illnesses. For ReA, these proportions were determined for each illness individually by using unique pathogen-specific beta distributions. The parameters of these beta distributions were all taken from a study of ReA as a post-infection sequela in the US and Canada [17]. Since IBS is rather common in the population, there was a need to explicitly account for background risk when calculating the proportion of post-infectious IBS. For this reason, attributable risk (AR) was used for these calculations [19]. Parameters for the calculations were taken from five different studies, and the final AR measure was calculated as a weighted average of the ARs obtained from these studies based on the number of observations in each [24,25,26,27,28]. The proportion of EHEC cases that led to HUS was based on a BetaPert distribution with parameters taken from two different studies: one Swedish study of sequelae to bacterial illnesses in general [29], and one study of HUS as a sequela to EHEC in children between 0 and 10 years of age [30].
The incidence of campylobacter-related GBS was calculated in three distinct ways: (1) by multiplying the number of GBS cases according to official statistics from hospitals by the proportion of GBS cases that are preceded by a campylobacter infection according to various studies [31,32,33,34]; (2) by multiplying the number of GBS cases as estimated in various studies [35] by the same proportion as in (1); and (3) by multiplying the estimated number of campylobacter cases (as given by the simulations) by the proportion of these cases that typically develop GBS according to results in the literature [34, 36]. The results from these three methods were then translated into a BetaPert distribution over the number of campylobacter-related GBS cases.
Like the five main illnesses, the total number of each sequela was divided into different events in order to simplify later COI calculations. For ReA and IBS, the event trees consisted of the three events: (i) no care; (ii) GP only; and (iii) GP and hospitalization. HUS may require dialysis, therefore the events for this illness are (i) no dialysis; (ii) dialysis, survive; and (iii) dialysis, death. The illness is generally severe and it was thus assumed that all patients were hospitalized. Finally, for GBS, the use of ventilation determines the three events: (i) no ventilation; (ii) ventilation, survive; and (3) ventilation, death. Again, due to the severity of the illness, all patients were assumed to having received hospital care.
2.4 Calculation of Costs Using Cost of Illness (COI)
COI is an estimation of the direct costs (medicine, transport, GP visits, hospitalization, and rehabilitation) and indirect costs (production losses due to sick leave) due to a particular illness. All costs were calculated in Swedish krona (SEK) using 2016 prices, and were then converted to Euros (€1.00 = SEK9.40) according to the exchange rate as of 1 July 2016.
2.4.1 Direct Costs: Main Pathogens
The data sources used to estimate direct costs are specified in Online Resource 2. In short, costs for GP visits, hospitalizations, medication, and transport were estimated for the main illnesses. The costs for GP visits and hospitalizations were obtained from a Swedish national registry where healthcare costs are related to individual patients rather than to the institutions where they arise. Since the registry only indicates costs per visit, ID numbers for each post were matched to obtain costs per patient. For a few records, the ID numbers were missing, therefore these costs were not included in the estimates. The costs for medicine and transport were taken from a study on the number of gastrointestinal illnesses and costs in Sweden [37]. All medical and transport costs were recalculated to the price level of 2016 according to relevant consumer price indices. Direct costs for GP visits and hospitalizations were calculated for outcome classes 2–4 and 3–4, respectively. Costs for medication and transport were calculated for all outcome classes.
2.4.2 Direct Costs: Sequelae
For ReA, direct costs were estimated for outpatient visits to doctors at hospitals and healthcare centers, visits to physiotherapists and occupational therapists, inpatient stays, radiographs, laboratory tests for disease-modifying antirheumatic drug (DMARD) monitoring, and medication. The costs used were based on a prospective study in southern Sweden of costs of early inflammatory joint disease [38]. For outcome class 3, all these costs were applied, but for outcome class 2, it was assumed that costs for inpatient stays, radiographs, and laboratory tests for DMARD monitoring were not applicable. For outcome class 1, no direct costs were expected.
Direct costs for IBS included costs for GP visits, hospitalizations, transport, and medication. The data sources used for calculating these costs were the same as for the main illnesses. Two studies were identified where the cost of medication relative to the cost of GP visits was provided [39, 40]. To calculate the cost of medication, a BetaPert distribution was used, with the results of these studies used as parameters of the distribution. The number of GP visits was assumed to be three in total for outcome classes 2 and 3, based on a study of long-term prognosis of IBS in the US [41]. The majority of these visits (85%) were assumed to occur within the first year of the illness based on a Dutch study of the disease burden of foodborne pathogens [42]. The rest of the visits were assumed to occur evenly for the remaining duration of the illness. Costs for these visits were adjusted using an annual discount rate of 4%. Based on the Dutch study discussed above, it was assumed that all these visits occurred within the first year of the illness. For outcome class 1, no direct costs were estimated.
For EHEC-related HUS, direct costs were calculated based on the same national registries as for the main illnesses. Costs were included for GP visits, less severe hospitalized cases (‘innerfall’), and severe hospitalized cases (‘ytterfall’). It was assumed that the severe cases included dialysis treatment, therefore the costs for these were applied to outcome classes 2 and 3. The costs for less severe cases were applied to outcome class 1. Since HUS is such a serious illness, it was assumed that all cases included GP visits and were being hospitalized. Costs for medication and transport could not be found in the literature and were thus not included for HUS.
The direct costs for campylobacter-related GBS included GP visits, hospitalization, and rehabilitation. Medication and transport costs were not found in the literature and were thus excluded from the calculations. Like HUS, hospitalization costs in the national registry were divided into less severe cases (‘innerfall’) and severe cases (‘ytterfall’). It was assumed that severe cases were equivalent to the need for ventilation, and these costs were thus applied to outcome classes 2 and 3. Costs for less severe hospitalization cases were applied to outcome classes 1 and 2, while costs for GP visits were assumed to apply for all cases. The data sources used for calculating costs for GP visits and hospitalizations were the same as for HUS and the main illnesses. To calculate rehabilitation costs, results from a Dutch study of the costs of campylobacter and sequelae were used [35]. In that study, the proportion between hospitalization costs and rehabilitation costs was calculated for three outcome classes: less severe cases, severe cases, and deaths. To apply the results to the present study, where the outcome classes are slightly different, the author of the Dutch study made new calculations upon request, where the severe cases were divided into ventilated/non-ventilated cases.
2.4.3 Indirect Costs: General
Indirect costs in this context consist of productivity losses that are forgone as the result of an adverse health outcome [43]. The productivity losses may result either from an employee’s own illness or from an employee staying at home to take care of a sick child. The size of the production loss is largely determined by two factors: its duration in days and the daily productivity loss.
To determine the duration of productivity losses, one of two competing methods can be used—the friction cost method and the human capital method [44]. In this study, the friction cost method was used, with a friction period of 90 days, which was the median duration of 46 published productivity cost studies [45]. A sensitivity analysis of this assumption is provided in Sect. 4. Since the data used to estimate illness duration for the main illnesses were different from that for the sequelae, the latter are discussed under separate headings below.
In accordance with neoclassical wage theory, the daily productivity loss was calculated as the gross wage per day, including social benefits for employees who stay home due to their illness [44]. For adults, the gross wages, including social benefits, for different age/sex combinations was calculated using data from Statistics Sweden. Gross wages were adjusted for labor force participation and for non-working days such as weekends. For children, it was assumed that one parent was at home during the illness until the child was aged 12 years (after which the parent needs to prove that the child has particular needs in order to receive compensation). The age of the parent staying at home was based on publicly available data over the number of mothers who gave birth at different ages in Sweden. To each age was added the average age of children 0–11 years who contracted a particular illness, using age data from the Public Health Agency of Sweden. This distribution was then divided into the different age categories used in the study. The distribution of men and women staying at home was taken from a Swedish study stating that approximately 64% of parents staying home with sick children are women [46]. Due to a lack of data, it was assumed that the age distribution of men staying at home were the same as that calculated for women.
2.4.4 Illness Duration: Main Illnesses
The average number of days at home due to one of the main illnesses was assumed to depend on which of the four outcome classes a certain case belonged to. For outcome classes 1 (no care) and 2 (GP only), data from a large population-based cohort study in England were used [8]. The illness duration was assumed to be the same for all illnesses in outcome class 1, but not in outcome class 2. For yersiniosis, two additional sources were used to estimate a BetaPert distribution for the illness duration in outcome class 2 [47, 48] (for details, see Online Resource 1). For outcome class 3 (GP and hospital), the number of days in hospital care per patient was added to the number of days in outcome class 2. For outcome class 4, the assumed friction period of 90 days was used.
2.4.5 Illness Duration: Sequelae
The illness duration for the four sequelae was assumed to correlate with the outcome class severity. For ReA, it was assumed that cases in outcome class 1 (no care) had no sick leave due to having only mild symptoms [49]. The illness duration in outcome classes 2 and 3 was modeled to be between 26 and 53 days based on results in the literature [38, 49].
IBS is an illness that can last several years, with relapses of diarrhea, constipation, and other gastrointestinal problems. In different studies, the illness duration has been estimated to be between 0.5 and 6 years [50,51,52,53,54,55]. It was thus assumed that the illness duration would always be longer than the 90-day friction period. The relatively mild symptoms of IBS imply that most persons will generally go to work despite the illness, but that the efficiency at work is somewhat reduced. In one study, it was estimated that work absence due to IBS was only 1.3%, but that the efficiency at the workplace was reduced by 15% on average [56]. These results were incorporated into the modeling framework.
In most cases, GBS is both a severe and a prolonged illness. Based on a Dutch study, productivity losses were assumed to last for the entire friction period of 90 days for all three outcome classes [49]. For HUS, data on the length of hospitalizations were combined with unpublished data from Italy on the period that people with HUS stay at home [57]. The illness durations were thus estimated to be 13 and 30 days for patients in outcome classes 1 and 2, respectively.
3 Results
3.1 General Parameters
Mean values and 90% credibility intervals (CIs) of the general parameters (parameters common for all main illnesses) are displayed in Table 1. Notably, the probability of visiting a GP and the probability of submitting a stool sample are markedly higher for cases with bloody diarrhea. For details regarding the underlying uncertainty distributions, see Online Resource 1.
3.2 Pathogen-Specific Parameters
Table 2 summarizes mean values and CIs (where applicable) for the various pathogen-specific parameters used in the model. The reported annual mean number of cases was highest for campylobacteriosis (8901) and salmonellosis (2500), followed by EHEC (536), shigellosis (306), and yersiniosis (268). The risk of having bloody diarrhea differs significantly between the main pathogens. The mean risk was highest for EHEC (74%), followed by yersiniosis (39%), salmonellosis (35%), shigellosis (29%), and campylobacteriosis (19%). The 90% CIs were markedly wide for these risks. The probability of death ranged from 0.03% (1 in every 3333 cases) for salmonellosis to 0.004% (1 in every 25,000 cases) for campylobacteriosis.
3.3 Reconstruction of the Morbidity Surveillance Pyramids
In Table 3, the different segments of the morbidity surveillance pyramids are reconstructed for the five main pathogens. The mean MF was highest for campylobacteriosis at 11.43 (90% CI 6.70–17.75), followed by EHEC (10.46, 90% CI 4.21–24.05), yersiniosis (10.00, 90% CI 5.05–18.29), shigellosis (10.08, 90% CI 3.77–21.57), and salmonellosis (7.87, 90% CI 3.36–16.18). The main reason for the high MF for campylobacter infections is the low risk of having bloody diarrhea and the resulting low probability of visiting a GP.
The high number of reported cases for campylobacteriosis in combination with the high MF implies that the estimated mean number of symptomatic cases is distinctly higher than for the other illnesses, with a mean of 101,719 (90% CI 59,640–158,025) cases occurring annually. The estimated mean number of cases in the community was second highest for salmonellosis (19,678, 90% CI 8394–40,456), followed by EHEC (5611, 90% CI 2256–12,898), shigellosis (3084, 90% CI 1154–6602), and yersiniosis (2676, 90% CI 1351–4896).
3.4 Event Trees of the Main Pathogens and Sequelae
In Table 4, we present an overview of the simulation results of the event trees for the five main pathogens and their sequelae. Each column in the table describes the event tree for a particular pathogen. Thus, for example, the total number of EHEC cases amount to 5611 (90% CI 2256–12,898). These cases are distributed into one of the four possible outcome classes defined in Sect. 2, with, for example, 2327 (90% CI 1243–4200) cases belonging to outcome class 2 (GP only). Below the event tree for each pathogen, the number of cases of each sequelae (and event trees for each of these) are provided. Thus, for example, a mean of 509 (90% CI 191–1184) cases of ReA occur as a direct consequence of first having had an episode of EHEC.
The proportion of main pathogen cases that lead to ReA varies between 9% (for EHEC) and 16% (for yersiniosis), while the proportion of main pathogen cases that lead to IBS was 9% for all the main pathogens. The incidences of campylobacter-related GBS and EHEC-related HUS are much smaller, with 38 and 165 cases, respectively, estimated to occur each year; however, many of these cases have very serious outcomes and are therefore important to consider.
3.5 COI
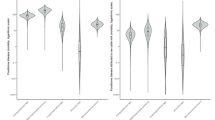
Table 5 summarizes the direct and indirect costs from the simulations. In total, the mean COI for the five pathogens and their sequelae amounts to over €142 million annually. Campylobacter (including sequelae) is by far the costliest of the pathogens, with annual direct and indirect costs of €97.7 million (90% CI 64.8–142.1), followed by salmonella (€25.3 million, 90% CI 14.2–45.0), EHEC (€12.5 million, 90% CI 5.5–26.3), shigella (€3.7 million, 90% CI 1.8–7.0), and yersinia (€3.3 million, 90% CI 1.9–5.6). Approximately 50% of the total costs are due to the main illness, while the remaining costs are due to the various sequelae.
For the main illnesses, as well as for IBS and ReA, the majority of direct costs were due to GP visits, which accounted for approximately 50–60%. Hospitalization accounted for approximately 30–40% of costs, while transportation and medicine, where applicable, represented 2–6%. For GBS, only 1% of direct costs were due to GP visits, while the majority of costs arose because of hospital visits (61%) and rehabilitation (39%). Finally, for HUS, as much as 97% of direct costs were due to hospitalizations. The majority of these hospital costs (87% of the total direct costs) were due to very expensive treatments for the more severe cases in outcome classes 2 and 3.
The annual costs per case was highest for EHEC at €2360 (90% CI 1669–3313), followed by salmonella (€1374, 90% CI 1057–1756), yersinia (€1273, 90% CI 949–1678), shigella (€1262, 90% CI 961–1634), and campylobacter (€979, 90% CI 843–1138).
4 Discussion
This is the first study to estimate direct and indirect costs for five major foodborne diseases in Sweden. The results were derived from simulations based on expert opinion, primary data from various sources, and available literature. The estimated total costs amount to over €142 million each year, with campylobacter representing almost 70% of the total costs. As a comparison, it has been estimated that the total cost of all gastrointestinal illnesses in Sweden amount to approximately €1 billion, based on a cohort study with 3241 participants [58]. Annual COI estimates have also been reported for other illnesses in Sweden, such as rheumatoid arthritis (€600 million) [59], breast cancer (€330 million) [60] and atrial fibrillation (€708 million) [61].
The estimations of the true number of cases of each illness were calculated by multiplying the number of reported cases by a pathogen-specific MF. To obtain this MF, simulations were performed based mainly on expert opinion regarding the magnitude of potential information loss about a case in the community. Other studies have presented higher MFs [62], similar MFs [10], and lower MFs [63]. Using other multipliers would alter the estimated number of cases as well as the COI for these cases (although costs per case would not be affected). More precisely, a certain percentage change in an MF would imply a similar percentage change of the costs associated with a certain illness and its sequelae.
However, UR relies heavily on healthcare systems, which vary widely between countries. Therefore country-specific MFs should be used if possible [14, 64, 65]. The MFs estimated in this paper are the only ones available based on Swedish data, and these are therefore considered to be the most accurate estimates available. Nevertheless, the main results for each illness are very dependent on the estimated MF and on the sequential multipliers that are used to calculate it. To account for the uncertainty related to these multipliers, as well as other uncertain parameters in the model, distributions rather than point estimates were used for most individual parameters in all simulations. As a consequence, CIs that incorporate the uncertainty of the estimates were obtainable for all results.
Of particular interest from an uncertainty perspective are the pathogen-specific distributions for parameter \(J\), the probability of having bloody diarrhea. As described in Sect. 2, this probability affects both the probability of seeking care and the probability of having a stool sample taken by a GP. From Table 2, it is evident that the estimates of this parameter are very uncertain, with wide CIs for all five pathogens. A sensitivity analysis further indicates that a 10% change in this probability would lead to a change of between 6 and 15% (in the opposite direction) for the estimated number of cases of the illnesses (and thus a corresponding change in the total costs). This substantial impact of \(J\) on the main results means that obtaining less ambiguous estimates of this probability would be one of the major sources of potential improvements in future studies.
Costs for certain sequelae were also accounted for (ReA and IBS for all pathogens, GBS for campylobacter, and HUS for EHEC). Including IBS as a post-ID is somewhat uncommon in COI studies. The underlying mechanisms between an initial infection and IBS are not fully understood, but it has been demonstrated that the odds of having IBS are considerably higher after an episode of gastrointestinal infection, and that the risk remains higher for at least 2–3 years [23]. Thus, it seemed reasonable to include IBS as a sequela in the analysis. Some studies have also found evidence of other sequelae, including IBD [66] and meningitis [67]. However, at least in the case of IBD, the number of cases triggered by any of the five main illnesses seem to be very limited and including them should not qualitatively change any results.
Neither VSLs nor VSCs were included in the estimates of the total costs of the illnesses. There are no principle problems in adding these costs, although one should be aware of double counting, as discussed in Sect. 1. However, both VSLs and VSCs are very sensitive to the contexts in which they are estimated, and transferability of values between countries and/or sectors should thus be avoided if possible [68]. Furthermore, even values from studies within Sweden related to food-related illnesses vary considerably depending on the methods used to elicit them [7, 69]. Considering the very limited number of relevant food-illness-related VSC and VSL estimations in Sweden, a choice was thus made to exclude these costs from the calculations.
The costs related to VSCs and VSLs may potentially constitute a major part of the total costs [70] and excluding them probably leads to a considerable UE of the total societal costs. One study, in which the remaining life expectancy of persons who die as a result of salmonella infection was considered, found that including VSLs had only a minor impact on expected costs [4]. Although this study used VSL values that decrease proportionately with age, which is not supported by most studies [71], it nevertheless provides an indication of how much VSL costs would increase if age is considered for the main illnesses (for which the average age of cases that do not survive is rather high). To see the impact of assuming an average (age-independent) VSL value, simulations were run in which a static VSL value of €2.6 million was applied to all mortal cases. This value is based on a stated preference study that has been estimated in, and is used by, the transport sector in Sweden for many years [72]. Assuming this approach increased overall costs by €66 million (46%), with the largest increases for HUS (€23 million), salmonella (€18 million), and campylobacter and EHEC (€10 million each). Despite problems with, for example, benefit transfers between sectors, this sensitivity analysis clearly indicates that including a constant VSL for all cases of mortality would probably lead to an appreciable increase in total costs.
To conclude, it was regarded as reasonable to exclude VSC and VSL values pending more consistent estimates. The implications of this exclusion are considered to be substantial, and the costs estimated in the current paper should thus be regarded as lower-bound estimates of the total costs for the respective illnesses when performing, for example, CBAs.
Indirect costs were calculated using the friction cost approach rather than the human capital approach. There are arguments for and against both approaches [73,74,75]. The main implication of using the friction cost approach is that the indirect costs calculated should also be seen as a lower bound. The impact depends heavily on the characteristics of the various illnesses, with a higher mortality and longer illness duration leading to greater differences between the two approaches. According to a previous Swedish study, the increase in costs using the human capital approach to calculate indirect costs would be approximately 6% for salmonella, 0% for ReA, and 140% for IBS [4]. The estimated mortality rates (see Table 2) indicate that for yersinia, campylobacter, and shigella, the increase in total costs would be less than the 6% for salmonella, while for EHEC this increase would be higher. For GBS and HUS, which both have relatively high mortality rates, the human capital approach would probably increase the estimated costs considerably more.
A friction period of 90 days was assumed as a point estimate throughout the study, based on the median value of a systematic review of productivity costs in various countries [45]. The friction period should ideally be based on macroeconomic characteristics of the country where the approach is applied [73]. Data for such an estimation were unfortunately not available. Since the assumption of 90 days is uncertain, a sensitivity analysis was performed in which the lowest (70 days) and highest (183 days) values in the systematic review were applied in the simulations. Using 70 days decreased the total costs of the five illnesses (including sequelae) by €3.2 million (2%), while using 183 days increased the costs by €12.9 million (9%). Almost all changes in costs were due to changed costs for IBS, for which all outcome classes were affected by the altered friction period.
The main objective of this paper was to produce cost estimates that can be used to evaluate various policy interventions that affect the level of food safety. Various potential interventions have been suggested for different stages of the food supply chain [76]. At the farm level, possible risk-reducing measures include using boot dips or fly screens, or to disinfect equipment and vehicles. Feed additives such as probiotics, bacteriophage, and bacteriocins have also been suggested. At the slaughter stage, interventions such as forced air chill, electrolyzed oxidizing water, and crust freezing are possible. At the consumer stage, various information on labels or through information campaigns could also be assessed and compared with the COI estimated in this article.
The discussion has demonstrated that the estimated costs associated with the five illnesses and their sequelae should be seen as lower bounds of the actual costs. This should be kept in mind when using the results for policy evaluation purposes. If evaluation of a food safety improvement should result in benefits (in terms of a lower number of human cases) outweighing the costs of the improvement, one can safely conclude that there is a positive net present value of the improvement. However, if costs should outweigh benefits, there is still uncertainty about the net result (since benefits may be higher than this study indicates).
With future studies producing more reliable estimates of intangible costs that could be added to the costs in this study, even more policy alternatives may be evaluated using cost-benefit methodologies.
References
Buzby JC, Roberts T. The economics of enteric infections: human foodborne disease costs. Gastroenterology. 2009;136(6):1851–62.
Ahmed S. Measuring the benefit of reducing food-borne illness. Ottawa: University of Ottawa; 2014.
Toljander J, Dovärn A, Andersson Y, Ivarsson S, Lindqvist R. Public health burden due to infections by verocytotoxin-producing Escherichia coli (VTEC) and Campylobacter spp. as estimated by cost of illness and different approaches to model disability-adjusted life years. Scand J Public Health. 2012;40(3):294–302.
Sundström K, Wahlström H, Ivarsson S, Lewerin SS. Economic effects of introducing alternative salmonella control strategies in Sweden. PloS One. 2014;9(5):e96446.
Soguel N, Griethuysen PV. Cost of illness and contingent valuation: controlling for the motivations of expressed preferences in an attempt to avoid double-counting, vol. 12. Marseille: Institut d’économie publique (IDEP); 2004.
Hughes G, Lovei M. Economic reform and environmental performance in transition economies, vol. 446. Washington, DC: World Bank Publications; 1999.
Andersson H, Hammitt JK, Sundström K. Willingness to pay and QALYs: what can we learn about valuing foodborne risk? J Agric Econ. 2015;66(3):727–52.
Wheeler JG, Sethi D, Cowden JM, Wall PG, Rodrigues LC, Tompkins DS, et al. Study of infectious intestinal disease in England: rates in the community, presenting to general practice, and reported to national surveillance. BMJ. 1999;318(7190):1046–50.
Gibbons CL, Mangen MJJ, Plass D, Havelaar AH, Brooke RJ, Kramarz P, et al. Measuring underreporting and under-ascertainment in infectious disease datasets: a comparison of methods. BMC Public Health. 2014;14(1):147.
Adak GK, Long SM, O’Brien SJ. Trends in indigenous foodborne disease and deaths, England and Wales: 1992 to 2000. Gut. 2002;51(6):832–41.
Tam CC, Rodrigues LC, Viviani L, Dodds JP, Evans MR, Hunter PR, et al. Longitudinal study of infectious intestinal disease in the UK (IID2 study): incidence in the community and presenting to general practice. Gut. 2012;61(1):69–77.
de Wit MA, Koopmans M, Kortbeek L, Wannet W, Vinje J, Van Leusden F, et al. Sensor, a population-based cohort study on gastroenteritis in the Netherlands: incidence and etiology. Am J Epidemiol. 2001;154(7):666–74.
Wahlström H, Lewerin SS, Sundström K, Ivarsson S. Estimation of the expected change in domestic human Salmonella cases in Sweden in 2010, given a hypothetical relaxation of the current Salmonella control programme. PloS One. 2014;9(3):e89833.
Haagsma J, Geenen P, Ethelberg S, Fetsch A, Hansdotter F, Jansen A, et al. Community incidence of pathogen-specific gastroenteritis: reconstructing the surveillance pyramid for seven pathogens in seven European Union member states. Epidemiol Infect. 2012;1(1):1–15.
The Public Health Agency of Sweden, online database. http://www.folkhalsomyndigheten.se/amnesomraden/statistik-och-undersokningar/sjukdomsstatistik/. Accessed 20 Oct 2017.
The National Board of Health and welfare, dataset from the National Patient Registry database. http://www.socialstyrelsen.se/english. Accessed 8 Oct 2017.
Townes JM, Deodhar AA, Laine ES, Smith K, Krug HE, Barkhuizen A, et al. Reactive arthritis following culture-confirmed infections with bacterial enteric pathogens in Minnesota and Oregon: a population-based study. Ann Rheum Dis. 2008;67(12):1689–96.
Parfenov AI, Ruchkina IN, Atauilakhanov RI, Belaya OF, Chikunova BZ, Pichugin AV. Postinfection irritable bowel syndrome. Terapevticheskii Arkhiv. 2009;81(2):39–45.
Haagsma JA, Siersema PD, De Wit NJ, Havelaar AH. Disease burden of post-infectious irritable bowel syndrome in The Netherlands. Epidemiol Infect. 2010;138(11):1650–6.
Mangen MJJ, Van Duynhoven Y, Van Pelt W, Kemmeren J, Havelaar AH. Priority setting of (foodborne) pathogens. Eur J Public Health. 2006;16(Suppl 1):11.
Noris M, Remuzzi G. Hemolytic uremic syndrome. J Am Soc Nephrol. 2005;16(4):1035–50.
Ajene AN, Walker CLF, Black RE. Enteric pathogens and reactive arthritis: a systematic review of Campylobacter, Salmonella and Shigella-associated reactive arthritis. J Health Popul Nutr. 2013;31(3):299.
Thabane M, Kottachchi DT, Marshall JK. Systematic review and meta-analysis: the incidence and prognosis of post-infectious irritable bowel syndrome. Aliment Pharmacol Ther. 2007;26(4):535–44.
Mearin F, Perez-Oliveras M, Perello A, Vinyet J, Ibanez A, Coderch J, et al. Dyspepsia and irritable bowel syndrome after a Salmonella gastroenteritis outbreak: one-year follow-up cohort study. Gastroenterology. 2005;129(1):98–104.
Parry SD, Stansfield R, Jelley D, Gregory W, Phillips E, Barton JR, et al. Does bacterial gastroenteritis predispose people to functional gastrointestinal disorders? A prospective, community-based, case-control study. Am J Gastroenterol. 2003;98(9):1970–5.
Jung IS, Kim HS, Park H, Lee SI. The clinical course of postinfectious irritable bowel syndrome a five-year follow-up study. J Clin Gastroenterol. 2009;43(6):534–40.
Rodriguez LAG, Ruigomez A. Increased risk of irritable bowel syndrome after bacterial gastroenteritis: cohort study. Br Med J. 1999;318(7183):565–6.
Wang LH, Fang XC, Pan GZ. Bacillary dysentery as a causative factor of irritable bowel syndrome and its pathogenesis [published erratum appears in Gut. 2004;53(9):1390]. Gut. 2004;53(8):1096–101.
Ternhag A, Törner A, Svensson A, Ekdahl K, Giesecke J. Short- and long-term effects of bacterial gastrointestinal infection. Emerg Infect Dis. 2008;14(1):143–8.
Tarr PI, Gordon CA, Chandler WL. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet. 2005;365(9464):1073–86.
Mishu B, Blaser MJ. Role of infection due to Campylobacter jejuni in the initiation of Guillain–Barré syndrome. Clin Infect Dis. 1993;17(1):104–8.
Jacobs B, Rothbarth P, Van der Meché F, Herbrink P, Schmitz P, De Klerk M, et al. The spectrum of antecedent infections in Guillain–Barré syndrome: a case-control study. Neurology. 1998;51(4):1110–5.
Havelaar A, van Koningsveld R, van Kempen E. Health burden in the Netherlands due to infection with thermophilic Campylobacter spp. Epidemiol Infect. 2000;125(3):505–22.
Allos BM. Association between Campylobacter infection and Guillain–Barré syndrome. J Infect Dis. 1997;176(Suppl 2):S125–8.
Mangen MJ, de Wit G, Havelaar AH. Campylobacteriosis in the Netherlands: estimating the cost-of-illness and the disease burden. IJMM Int J Med Microbiol. 2003;293(Suppl 35):27.
McCarthy N, Giesecke J. Incidence of Guillain–Barré syndrome following infection with Campylobacter jejuni. Am J Epidemiol. 2001;153(6):610–4.
Hansdotter FI, Magnusson M, Kühlmann-Berenzon S, Hulth A, Sundström K, Hedlund K-O, et al. The incidence of acute gastrointestinal illness in Sweden. Scand J Public Health. 2015;43(5):540–7.
Soderlin MK, Kautiainen H, Jonsson D, Skogh T, Leirisalo-Repo M. The costs of early inflammatory joint disease: a population-based study in southern Sweden. Scand J Rheumatol. 2003;32(4):216–24.
Akehurst RL, Brazier JE, Mathers N, O’Keefe C, Kaltenthaler E, Morgan A, et al. Health-related quality of life and cost impact of irritable bowel syndrome in a UK primary care setting. Pharmacoeconomics. 2002;20(7):455–62.
Leong SA, Barghout V, Birnbaum HG, Thibeault CE, Ben-Hamadi R, Frech F, et al. The economic consequences of irritable bowel syndrome: a US employer perspective. Arch Intern Med. 2003;163(8):929–35.
Owens DM, Nelson DK, Talley NJ. The irritable-bowel-syndrome: long-term prognosis and the physician-patient interaction. Ann Intern Med. 1995;122(2):107–12.
Haagsma JA, van der Zanden BP, RTariq L, van Pelt W, van Duynhoven YTPH, Havelaar AH. Disease burden and costs of selected foodborne pathogens in the Netherlands, 2006. National Institute for Public Health and the Environment; 2006.
Kuchler F, Golan EH. Assigning values to life: comparing methods for valuing health risks. United States Department of Agriculture, Economic Research Service; 1999.
Drummond M, McGuire A. Economic evaluation in health care: merging theory with practice. Oxford: Oxford University Press; 2001.
Kigozi J, Jowett S, Lewis M, Barton P, Coast J. Estimating productivity costs using the friction cost approach in practice: a systematic review. Eur J Health Econ. 2016;17(1):31–44.
Eriksson H. Är det verkligen ekonomin som styr? En studie av ekonomiska drivkrafter vid vård av barn. Working Papers in Social Insurance, Försäkringskassan; 2009.
Ostroff SM, Kapperud G, Lassen J, Aasen S, Tauxe RV. Clinical features of sporadic yersinia-enterocolitica infections in Norway. J Infect Dis. 1992;166(4):812–7.
Lee LA, Taylor J, Carter GP, Quinn B, Farmer JJ, Tauxe RV. Yersinia-Enterocolitica o-3: an emerging cause of pediatric gastroenteritis in the United States. J Infect Dis. 1991;163(3):660–3.
Mangen MJ, Havelaar A, Bernsen R, Van Koningsveld R, De Wit G. The costs of human Campylobacter infections and sequelae in the Netherlands: A DALY and cost-of-illness approach. Food Econ Acta Agric Scand Sect C. 2005;2(1):35–51.
Gwee KA, Graham JC, McKendrick MW, Collins SM, Marshall JS, Walters SJ, et al. Psychometric scores and persistence of irritable bowel after infectious diarrhoea. Lancet. 1996;347(8995):150–3.
McKeown ES, Parry SD, Stansfield R, Barton JR, Welfare MR. Postinfectious irritable bowel syndrome may occur after non-gastrointestinal and intestinal infection. Neurogastroenterol Motil. 2006;18(9):839–43.
Ji S, Park H, Lee D, Song YK, Choi JP, Lee SI. Post-infectious irritable bowel syndrome in patients with Shigella infection. J Gastroenterol Hepatol. 2005;20(3):381–6.
Marshall JK, Thabane M, Garg AX, Clark WF, Salvadori M, Collins SM, et al. Incidence and epidemiology of irritable bowel syndrome after a large waterborne outbreak of bacterial dysentery. Gastroenterology. 2006;131(2):445–50.
Kim HS, Kim MS, Ji SW, Park H. The development of irritable bowel syndrome after Shigella infection: 3 year follow-up study [in Korean]. Korean J Gastroenterol. 2006;47(4):300–5.
Neal KR, Barker L, Spiller RC. Prognosis in post-infective irritable bowel syndrome: a six year follow up study. Gut. 2002;51(3):410–3.
Dean BB, Aguilar D, Barghout V, Kahler KH, Frech F, Groves D, et al. Impairment in work productivity and health-related quality of life in patients with IBS. Am J Manag Care. 2005;11(1 Suppl):S17–26.
Scavia G. HUS Registry in Italy 1988–2008, personal communication with Gaia Scavia, HUS registry coordinator in Italy.
Edelstein M, Merk H, Deogan C, Carnahan A, Wallensten A. Quantifying the incidence and cost of acute gastrointestinal illness in Sweden, 2013–2014. Epidemiol Infect. 2016;144(13):2831–9.
Kalkan A, Hallert E, Bernfort L, Husberg M, Carlsson P. Costs of rheumatoid arthritis during the period 1990–2010: a register-based cost-of-illness study in Sweden. Rheumatology. 2013;53(1):153–60.
Lidgren M, Wilking N, Jönsson B. Cost of breast cancer in Sweden in 2002. Eur J Health Econ. 2007;8(1):5–15.
Ericson L, Bergfeldt L, Björholt I. Atrial fibrillation: the cost of illness in Sweden. Eur J Health Econ. 2011;12(5):479–87.
Mead PS, Slutsker L, Dietz V, McCaig LF, Bresee JS, Shapiro C, et al. Food-related illness and death in the United States. Emerg Infect Dis. 1999;5(5):607–25.
de Jong B, Ekdahl K. The comparative burden of salmonellosis in the European Union member states, associated and candidate countries. BMC Public Health. 2006;6:4.
Havelaar A, Ivarsson S, Löfdahl M, Nauta M. Estimating the true incidence of campylobacteriosis and salmonellosis in the European Union, 2009. Epidemiol Infect. 2012;1(1):1–10.
Falkenhorst G, Simonsen J, Ceper TH, van Pelt W, de Valk H, Sadkowska-Todys M, et al. Serological cross-sectional studies on salmonella incidence in eight European countries: no correlation with incidence of reported cases. BMC Public Health. 2012;12(1):523.
Kahng LS. Infection, inflammation, and homeostasis in inflammatory bowel disease. Gastroenterology. 2009;137(2):415–8.
CDC. Reported isolates of Salmonella from CSF in the United States, 1968–1979. J Infect Dis. 1981;143:504–56.
Brouwer R, Bateman IJ. Benefits transfer of willingness to pay estimates and functions for health-risk reductions: a cross-country study. J Health Econ. 2005;24(3):591–611.
Andersson H, Hole AR, Svensson M. Valuation of small and multiple health risks: a critical analysis of SP data applied to food and water safety. J Environ Econ Manag. 2016;75:41–53.
Henson S. Consumer willingness to pay for reductions in the risk of food poisoning in the UK. J Agric Econ. 1996;47(3):403–20.
Aldy JE, Viscusi WK. Adjusting the value of a statistical life for age and cohort effects. Rev Econ Stat. 2008;90(3):573–81.
SIKA PM. 2008:3 Samhällsekonomiska principer och kalkylvärden för transportsektorn: ASEK 4. 2008. https://www.trafikverket.se/contentassets/d7cf7d727fb2488aab9fa9d24387c7c8/externa-rapporter/asek_4_samhallsekonomiska_principer_och_kalkylvarden_for_transportsektorn.pdf .
Koopmanschap MA, Rutten FFH, Vanineveld BM, Vanroijen L. The friction cost method for measuring indirect costs of disease. J Health Econ. 1995;14(2):171–89.
Johannesson M, Karlsson G. The friction cost method: a comment. J Health Econ. 1997;16(2):249–55.
Koopmanschap MA, Rutten FFH, van Ineveld BM, van Roijen L. Reply to Johanneson’s and Karlsson’s comment. J Health Econ. 1997;16(2):257–9.
MacRitchie L, Hunter CJ, Strachan N. Consumer acceptability of interventions to reduce Campylobacter in the poultry food chain. Food Control. 2014;35(1):260–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was provided for this study.
Conflict of interest
Kristian Sundström has no conflicts of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sundström, K. Cost of Illness for Five Major Foodborne Illnesses and Sequelae in Sweden. Appl Health Econ Health Policy 16, 243–257 (2018). https://doi.org/10.1007/s40258-017-0369-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-017-0369-z