Abstract
Background
There has been increasing interest in measuring the productive performance of healthcare services since the mid-1980s.
Objective
By applying bootstrapped data envelopment analysis across the 20 Italian Regional Health Systems (RHSs) for the period 2008–2012, we employed a two-stage procedure to investigate the relationship between care appropriateness and productivity evolution in public hospital services.
Methods
In the first stage, we estimated the Malmquist index and decomposed this overall measure of productivity into efficiency and technological change. In the second stage, the two components of the Malmquist index were regressed on a set of variables measuring per capita health expenditure, care appropriateness, and clinical appropriateness.
Results
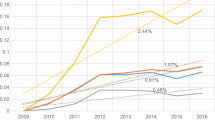
Malmquist analysis shows that no gains in productivity in the health industry have been achieved in Italy despite the sequence of reforms that took place during the 1990s, which were devoted to increasing efficiency and reducing costs. Analysis of the efficiency change index clearly indicates that the source of productivity gain relies on a rationalization of the employed inputs in the Italian RHSs. At the same time, the trend of the technological change index reveals that the health systems in the three macro-areas (North, Central, and South) are characterized by technological regress.
Conclusion
Overall, our results suggest that productivity increases could be achieved in the Italian health system by reducing the level of inputs, improving care and clinical appropriateness, and by counteracting the ‘DRG (diagnosis-related group) creep’ phenomenon.

Similar content being viewed by others
Notes
The number of discharges includes the number of patients discharged from day hospital.
The cmx expresses the average complexity of a diagnosis-related group (DRG) treated in the hospital compared with the average complexity data from a set of reference hospitals (e.g., all Italian hospitals).
2000 replications have been employed. The bootstrap estimates of the indexes are significant at the 5 % values. The confidence intervals are available on request from the authors.
References
Boni S, Malpelli V, De Stefano A, Compagnoni V, Gambino A, Ceccarelli A. I sistemi di governance dei Servizi Sanitari Regionali. Quaderno Formez n. 57. 2007; Formez.
Censis. I modelli decisionali nella sanità locale. Roma: Censis; 2008.
Vainieri M, Nuti S. Performance measurement features of the Italian regional healthcare systems: differences and similarities. In: Smigorski K, editor. Health management-different approaches and solutions. Rijeka: InTech; 2011. http://www.intechopen.com/books/health-management-different-approaches-and-solutions/performance-measurement-features-of-the-italian-regional-healthcare-systems-differences-and-similari. Accessed 9 July 2016.
Francese M, Romanelli M. Healthcare in Italy: expenditure determinants and regional differentials. Banca d’Italia working papers. 2011;828:1–46. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=1880310. Accessed 9 Jul 2016.
Tediosi F, Gabriele S, Longo F. Governing decentralization in health care under tough budget constraint: what can we learn from the Italian experience? Health Policy. 2009;90:303–12.
Italian Ministry of Health. Rapporto annuale sull’attività di ricovero ospedaliero, Dati SDO 2008–12, 2013. http://www.salute.gov.it/portale/documentazione/p6_2_2.jsp?lingua=italiano&area=ricoveriOspedalieri&btnCerca=. Accessed 13 July 2016.
Lavis JN, Anderson GM. Health care delivery: definitions, measurements and policy implications. Can Med Assoc J. 1966;154:321–8.
Bevere F, Dotta F, Fava A, Gentile S, Lauro D, Lauro R, et al. Appropriatezza clinica, strutturale, tecnologica e operativa per la prevenzione, diagnosi e terapia dell’obesità e del diabete mellito. Quaderni del Ministero della Salute 2011;10. ISSN 2038-5293. http://www.salute.gov.it/imgs/C_17_pubblicazioni_1707_allegato.pdf. Accessed 9 Jul 2016.
Siciliani L. Estimating technical efficiency in the hospital sector with panel data. Appl Health Econ Health Policy. 2006;2:99–116.
Liberati P. Fiscal federalism and national health standards in Italy: implication for redistribution. In: Il futuro dei sistemi di welfare nazionali tra integrazione europea e decentramento regionale. Conference of the Società Italiana di Economia Pubblica; 4–5 Oct 2002; Pavia.
Francese M, Romanelli M. Is there room for containing healthcare costs? An analysis of regional spending differentials in Italy. Eur J Health Econ. 2014;15:117–32.
Francese M, Piacenza M, Romanelli M, Turati G. Understanding inappropriateness in health spending: the role of regional policies and institutions in caesarean deliveries. Reg Sci Urban Econ. 2014;43:262–77.
De Nicola A, Gitto S, Mancuso P, Valdmanis VG. Healthcare reform in Italy: an analysis of efficiency based on nonparametric methods. Int J Health Plan Manag. 2014;29:e48–63.
Caves DW, Christensen LR, Diewert WE. The economic theory of index numbers and the measurement of input, output, and productivity. Econometrica. 1982;5:1393–400.
Färe R, Grosskopf S, Lindgren B, Roos P. Productivity changes in Swedish pharmacies 1980–1989: a non parametric approach. J Prod Anal. 1992;3:85–101.
Simar L, Wilson PW. Statistical inference in nonparametric frontier models: recent developments and perspectives. In: Fried H, Lovell K, Schmidt SS, editors. The measurement of productive efficiency and productivity growth. New York: Oxford University Press; 2008.
Thanassoulis E, Portela M, Despic O. Data envelopment analysis: the mathematical programming approach to efficiency analysis. In: Fried H, Lovell K, Schmidt SS, editors. The measurement of productive efficiency and productivity growth. New York: Oxford University Press; 2008.
Shepard RW. Theory of cost and production functions. Princeton: Princeton University Press; 1970.
Färe R, Grosskopf S, Roos P. Productivity and quality changes in Swedish pharmacies. Int J Prod Econ. 1995;39:137–47.
Jacobs R, Smith PC, Street A. Measuring efficiency in health care. New York: Cambridge University Press; 2006.
Simar L, Wilson PW. Estimating and bootstrapping Malmquist indices. Eur J Oper Res. 1999;115:459–71.
Wilson PW. FEAR: a software package for frontier efficiency analysis with R. Socio Econ Plan Sci. 2007;42:247–54.
Worthington A. Malmquist indices of productivity change in Australian financial services. J Int Financ Mark Inst Money. 1999;9:303–20.
Nedelea IC, Fannin JM. Technical efficiency of critical access hospitals: an application of the two-stage approach with double bootstrap. Health Care Manag Sci. 2013;16:27–36.
Baltagi BH. Econometric analysis of panel data. 4th ed. Chichester: Wiley; 2008.
ISTAT (Istituto Nazionale di Statistica). Health for All database. http://www.istat.it/it/archivio/14562. Accessed 9 July 2016.
Loghi M, D’Errico A. Health for All—Italia, an informative health system. Ital J Public Health. 2008;5(2):107–11.
Lo Scalzo A, Donatini A, Orzella L, Cicchetti A, Profili S, Maresso A. Health care systems in transition: Italy. Copenhagen: WHO regional office for Europe on behalf of the European Observatory on Health Systems and Policies; 2009.
De Nicola A, Gitto S, Mancuso P. Evaluating Italian public hospital efficiency using bootstrap DEA and CART. Int J Appl Decis Sci. 2013;6:281–92.
Ferrier GD, Rosko MD, Valdmanis VG. Analysis of uncompensated hospital care using a DEA model of output congestion. Health Care Manag Sci. 2006;9:181–8.
Ozcan YA. Health care benchmarking and performance evaluation: an assessment using data envelopment analysis. New York: Springer; 2008.
O’Neill L, Rauner M, Heidenberger K, Kraus K. A cross-national comparison and taxonomy of DEA-based hospital efficiency studies. Soc Econ Plan Sci. 2008;42:158–89.
Mitropoulos P, Kounetas K, Mitropoulos I. Factors affecting primary health care centers’ economic and production efficiency. Ann Oper Res. doi:10.1007/s10479-015-2056-5 (Epub 12 Nov 2015).
De Nicola A, Gitto S, Mancuso P. Uncover the predictive structure of healthcare efficiency applying a bootstrapped data envelopment analysis. Expert Syst Appl. 2012;39:10495–9.
Grosskopf S, Margaritis D, Valdaminis VG. Competitive effects on teaching hospitals. Eur J Oper Res. 2004;154:515–25.
Mobley LR, Magnussen J. An international comparison of hospital efficiency: does institutional environment matter? Appl Econ. 1998;30:1089–100.
Chowdhury H, Zelenyuk V, Laporte A, Wodchis WP. Analysis of productivity, efficiency and technological changes in hospital services in Ontario: how does case-mix matter? Int J Prod Econ. 2014;150:74–82.
O’Malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health Serv Res. 2005;40:1620–39.
Kahur K. Error DRGs—what are they for? BMC Health Serv Res. 2010;10(Suppl 2):A5.
Simborg DW. DRG creep: a new hospital acquire disease. N Engl J Med. 1981;304:1062–4.
Gibbons L, Belizán JM, Lauer JA, Betrán AP, Merialdi M, Althabe F. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: overuse as a barrier to universal coverage. World Health Report (2010), Background Paper 30. Geneva: WHO; 2010.
ISTAT (Istituto Nazionale di Statistica). Ageing index. 2012. http://noi-italia2012en.istat.it/index.php?id=7&user_100ind_pi1%5Bid_pagina%5D=15&cHash=3af4f87fc1eba1af87e862f57aa97d91. Accessed 9 July 2016.
Daraio C, Simar L. Advanced robust and nonparametric methods in efficiency analysis: methodology and applications. New York: Springer; 2007.
Everitt BS, Torsten H. A handbook of statistical analyses using R. Boca Raton: Chapman and Hall/CRC; 2006.
Hollingsworth B. The measurement of efficiency and productivity of health care delivery. Health Econ. 2008;17:1107–28.
Ferré F, de Belvis AG, Valerio L, Longhi S, Lazzari A, Fattore G, et al. European Observatory on Health System and Policy. Italy: health system review. Health Syst Transit. 2014;16(4):1–168.
Acknowledgments
The authors would like to thank to Tim Wrightson, Editor-in-Chief of Applied Health Economics and Health Policy, and two anonymous referees for their comments and critical remarks, which were very helpful in crafting earlier drafts of this manuscript.
Authors’ contributions
Paolo Mancuso and Vivian Grace Valdmanis evaluated the literature and were equally involved in the model design. Paolo Mancuso built the model and conducted the model analyses. Both authors reviewed and approved the final submitted version of the manuscript. Paolo Mancuso is the guarantor for the overall content.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
No sources of funding were used to prepare this paper. Paolo Mancuso and Vivian Grace Valdmanis have no conflicts of interest that are directly relevant to the content of this paper.
Rights and permissions
About this article
Cite this article
Mancuso, P., Valdmanis, V.G. Care Appropriateness and Health Productivity Evolution: A Non-Parametric Analysis of the Italian Regional Health Systems. Appl Health Econ Health Policy 14, 595–607 (2016). https://doi.org/10.1007/s40258-016-0257-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-016-0257-y