Abstract
Background
There has been an appreciable increase in the prescribing efficiency of proton pump inhibitors, statins, and renin–angiotensin inhibitor drugs in Sweden in recent years. This has been achieved through multiple reforms encouraging the prescription of generics at low prices versus patented drugs in the same class. Generic venlafaxine also presents an opportunity to save costs given the prevalence of depression. However, depression is more complex to treat, with physicians reluctant to change prescriptions if patients are responding to a particular antidepressant.
Objectives
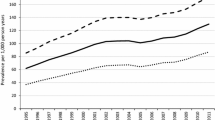
We assessed (a) changes in the utilization pattern of venlafaxine versus other newer antidepressants before and after the availability of generic venlafaxine and before and after the initiation of prescription restrictions for duloxetine limiting its prescription to refractory patients, (b) utilization of generic versus original venlafaxine after its availability, and (c) price reductions for generic venlafaxine and the subsequent influence on total expenditure on newer antidepressants over time.
Methodology
We performed interrupted time series analysis of changes in monthly reimbursed prescriptions using defined daily doses (DDDs) of patients dispensed at least one newer antidepressant from January 2007 to August 2011. DDDs was defined as the average maintenance dose of a drug when used in its major indication in adults. This included 19 months after the availability of generic venlafaxine and before initiation of prescription restrictions for duloxetine to 13 months after prescription restrictions. Total expenditure and expenditure/DDD for venlafaxine were measured over time.
Results
No appreciable change in the utilization pattern for venlafaxine was observed after generic availability when no appreciable demand-side activities by the regions (counties) were implemented to encourage its use. The utilization of venlafaxine significantly increased after prescription restrictions for duloxetine. Generic venlafaxine was dispensed once available, reaching 99.6 % of total venlafaxine (DDD basis) by August 2011. There was an appreciable fall in expenditure for newer antidepressants in Sweden after generic venlafaxine despite increased utilization, helped by a 90 % reduction in expenditure/DDD for venlafaxine by the end of the study versus prepatent loss prices.
Conclusion
Multiple demand-side measures are needed to change physician prescribing habits. Authorities should not rely on a spillover effect between drug classes to effect change. Limited influence of prescription restrictions on the subsequent utilization of duloxetine reflects the complexity of this disease area. This is exacerbated by heterogeneous indications for duloxetine.




Similar content being viewed by others
References
Godman B, Bucsics A, Burkhardt T, Haycox A, Seyfried H, Wieninger P. Insight into recent reforms and initiatives in Austria; implications for key stakeholders. Expert Rev Pharmacoecon Outcomes Res. 2008;8:357–71.
Sermet C, Andrieu V, Godman B, Van Ganse E, Haycox A, Reynier JP. Ongoing pharmaceutical reforms in France; implications for key stakeholder groups. Appl Health Econ Health Policy. 2010;8:7–24.
Coma A, Zara C, Godman B, Augusti A, Diogene E, Wettermark B, Haycox A. Policies to enhance the efficiency of prescribing in the Spanish Catalan region: impact and future direction. Expert Rev Pharmacoecon Outcomes Res. 2009;9:569–81.
Wettermark B, Godman B, Andersson K, Gustafsson LL, Haycox A, Bertele V. Recent national and regional drug reforms in Sweden—implications for pharmaceutical companies in Europe. Pharmacoeconomics. 2008;26:537–50.
Godman B, Wettermark B, Hoffman M, Andersson K, Haycox A, Gustafsson LL. Multifaceted national and regional drug reforms and initiatives in ambulatory care in Sweden; global relevance. Expert Rev Pharmacoecon Outcomes Res. 2009;9:65–83.
Vončina L, Strizrep T, Godman B, Bennie M, Bishop I, Campbell S, Vlahovic Palcevski V, Gustafsson LL. Influence of demand side measures to enhance renin–angiotensin prescribing efficiency in Europe; implications for the future. Expert Rev Pharmacoecon Outcomes Res. 2011;11:469–79.
Godman B, Wettermark B, Bishop I, Burkhardt T, Fürst J, et al. European payer initiatives to reduce prescribing costs through use of generics. GABI. 2012;1:22–7.
Godman B, Shrank W, Andersen M, Berg C, Bishop I, Burkhardt T, et al. Comparing policies to enhance prescribing efficiency in Europe through increasing generic utilisation: changes seen and global implications. Expert Rev Pharmacoecon Outcomes Res. 2010;10:707–22.
Godman B, Shrank W, Andersen M, Berg C, Bishop I, Burkhardt T, Garuoliene K, et al. Policies to enhance prescribing efficiency in Europe: findings and future implications. Front Pharmacol. 2011;1(141):1–16. doi:10.3389/fphar.2010.00141.
OECD (2011) Pharmaceutical expenditure. In: OECD, Health at a Glance 2011: OECD Indicators. OECD Publishing. doi:10.1787/health_glance-2011-63-en. http://www.oecd-ilibrary.org/docserver/download/fulltext/8111101ec063.pdf?expires=1343281688&id=id&accname=guest&checksum=4D4F46B30255998AA81601571E18EE8F. Accessed Dec 2012.
Godman B, Sakshaug S, Berg C, Wettermark B, Haycox A. Combination of prescribing restrictions and policies to engineer low prices to reduce reimbursement costs. Expert Rev Pharmacoecon Outcomes Res. 2011;11:121–9.
Markovic-Pekovic V, Ranko Škrbić R, Godman B, Gustafsson LL. Ongoing initiatives in the Republic of Srpska to enhance prescribing efficiency: influence and future directions. Expert Rev Pharmacoecon Outcomes Res. 2012;5:661–71.
Garuoliene K, Godman B, Gulbinovič J, Wettermark B, Haycox A. European countries with small populations can obtain low prices for drugs: Lithuania as a case history. Expert Rev Pharmacoecon Outcomes Res. 2011;11:343–9.
Godman B, Abuelkhair M, Vitry A, Abdu S, et al. Payers endorse generics to enhance prescribing efficiency; impact and future implications, a case history approach. GABI. 2012;1(2):69–83.
Brkičic L, Vončina L, Sovic S, Godman B, Relja M. Initiatives to improve prescribing efficiency for drugs to treat Parkinson’s disease in Croatia; influence and future directions. Expert Rev Pharmacoecon Outcomes Res. 2012;12:373–84.
Garattini S, Bertele V, Godman B, Haycox A, Wettermark B, Gustafsson LL. Enhancing the rational use of new medicines across European healthcare systems—a position paper. Eur J Clin Pharmacol. 2008;64:1137–8.
McGinn D, Godman B, Lonsdale J, Way R, Wettermark B, Haycox A. Initiatives to enhance the quality and efficiency of statin and PPI prescribing in the UK; impact and implications. Expert Rev Pharmacoecon Outcomes Res. 2010;10:73–85.
Bennie M, Godman B, Bishop I, Campbell S. Multiple initiatives continue to enhance the prescribing efficiency for the proton pump inhibitors and statins in Scotland. Expert Rev Pharmacoecon Outcomes Res. 2012;12:125–30.
Godman B, Burkhardt T, Bucsics A, et al. Impact of recent reforms in Austria on utilisation and expenditure of PPIs and lipid lowering drugs; implications for the future. Expert Rev Pharmacoecon Outcomes Res. 2009;9:475–84.
Godman B, Schwabe U, Selke G, Wettermark B. Update of recent reforms in Germany to enhance the quality and efficiency of prescribing of proton pump inhibitors and lipid lowering drugs. Pharmacoeconomics. 2009;27:435–8.
Godman B, Malmstrom RE, Bennie M, Sakshaug S, Burkhardt T, et al. Prescribing restrictions—a necessary strategy among some European countries to enhance future prescribing efficiency? Rev Health Care. 2012;3:5–16.
Godman B, Bennie M, Baumgärtel C, Sović Brkičić L, et al. Essential to increase the use of generics in Europe to maintain comprehensive healthcare? Farmeconomia Health Econ Ther Pathways. 2012;13(Suppl 3):5–20.
Wladysiuk M, Araszkiewicz A, Godman B, Szabert K, et al. Patient co-payments do influence atypical antipsychotic choice in Poland; implications once generic atypcials are available. Appl Health Econ Health Policy. 2011;9:101–10.
Godman B, Paterson K, Malmstrom R, et al. Improving the managed entry of new drugs: sharing experiences across Europe. Expert Rev Pharmacoecon Outcomes Res. 2012;12:439–41.
Fraeyman J, Van Hal G, Godman B, Beutels P. The potential influence of various initiatives to improve rational prescribing for proton pump inhibitors and statins in Belgium. Expert Rev Pharmacoecon Outcomes Res. 2013;13:141–51.
Bucsics A, Godman B, Burkhardt T, et al. Influence of lifting prescribing restrictions for losartan on subsequent sartan utilisation patterns in Austria; implications for other countries. Expert Rev Pharmacoecon Outcomes Res. 2012;12:809–19.
Norman C, Zarrinkoub R, Hasselström J, Godman B, et al. Potential savings without compromising the quality of care. Int J Clin Pract. 2009;63:1320–6.
Gustafsson LL, Wettermark B, Godman B, Andersén-Karlsson E, Bergman U, et al. The “Wise List”—a comprehensive concept to select, communicate and achieve adherence to recommendations of essential drugs in ambulatory care in Stockholm. Basic Clin Pharmacol Toxicol. 2011;108:224–33.
Wettermark B, Godman B, Neovius M, Hedberg N, et al. Initial effects of a reimbursement restriction to improve the cost-effectiveness of antihypertensive treatment. Health Policy. 2010;94:221–9.
Wettermark B, Pehrsson A, Juhasz-Haverinen M, Veg A, Edlert M, Törnwall-Bergendahl G, Almkvist H, Godman B, et al. Financial incentives linked to self-assessment of prescribing patterns—a new approach for quality improvement of drug prescribing in primary care. Qual Prim Care. 2009;17:179–89.
Andersson K, Sonesson C, Petzold M, et al. What are the obstacles to generic substitution? An assessment of the behaviour of prescribers, patients and pharmacies during the first year of generic substitution in Sweden. Pharmacoepidemiol Drug Saf. 2005;14:341–8.
Pettersson B, Hoffmann M, Wändell P, Levin LA. Utilization and costs of lipid modifying therapies following health technology assessment for the new reimbursement scheme in Sweden. Health Policy. 2012;104:84–91.
Persson U, Svensson J, Pettersson B. A new reimbursement system for innovative pharmaceuticals combining value-based and free market pricing. Appl Health Econ Health Policy. 2012;10:217–25.
Godman B, Gustafsson LL. A new reimbursement systems for innovative pharmaceuticals combining value-based and free market pricing. AHEP. 2013;11:79–82.
Agüera-Ortiz L, Ramos Garcia I. Effectiveness of venlafaxine extended release and conventional antidepressants in elderly patients with depressive disorder. Actas Esp Psiquiatr. 2006;34(3):153–61 (Article in Spanish with English abstract).
Yu-Isenberg KS, Fontes CL, Wan GJ, et al. Acute and continuation treatment adequacy with venlafaxine extended release compared with fluoxetine. Pharmacotherapy. 2004;24(1):33–40.
Baldomero EB, Ubago JG, Cercós CL, et al. Venlafaxine extended release versus conventional antidepressants in the remission of depressive disorders after previous antidepressant failure: ARGOS study. Depress Anxiety. 2005;22(2):68–76.
Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, Watanabe N, Nakagawa A, Omori IM, McGuire H, Tansella M, Barbui C. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373:746–58.
Parikh S. Antidepressants are not all created equal. Lancet. 2009;373:700–1.
Barbui C, Cipriani A. Agomelatine and the brave old world of narrative-based medicine. Evid Based Ment Health. 2012;15:2–3.
Cymbalta (duloxetine) receives restricted reimbursement. TLV Sweden. TLV decision duloxetine. http://www.tlv.se/Upload/Genomgangen/100615-tlv-interim-decision-cymbalta.pdf. Accessed Dec 2012.
Godman B, Buscics A, Burkhardt T, et al. Potential to enhance the prescribing of generic drugs in patients with mental health problems in Austria; implications for the future. Front Pharmacol. 2012;3:198. doi:10.3389/fphar.2012.00198.
Bennie M, Bishop I, Godman B, Barbui C, et al. Are specific initiatives required to enhance the prescribing of generic atypical antipsychotics in Scotland? International implications. Int J Clin Pract. 2013;67(2):170–180.
Usher-Smith J, Ramsbottom T, Pearmain H, Kirby M. Evaluation of the clinical outcomes of switching patients from atorvastatin to simvastatin and losartan to candesartan in a primary care setting: 2 years on. Int J Clin Pract. 2008;62:480–4.
Godman B, Wettermark B, Miranda J, et al. Influence of multiple initiatives in Sweden to enhance ARB prescribing efficiency following generic losartan; findings and implications for other countries. Int J Clin Pract. 2013. doi:10.1111/ijcp.12130.
World Health Organisation (WHO). WHO Collaborating Centre for Drug Statistics Methodology Oslo ATC/DDD index 2012. http://www.whocc.no/atc_ddd_index/. Accessed Dec 2012.
World Health Organization (WHO). Introduction to Drug Utilisation Research. WHO International Working Group for Drug Statistics Methodology, WHO Collaborating Centre for Drug Statistics Methodology, WHO Collaborating Centre for Drug Utilization Research and Clinical Pharmacological Services. ISBN 92 4 156234 X (NLM classification: WB 330). http://www.who.int/medicines/areas/quality_safety/safety_efficacy/Drug%20utilization%20research.pdf.
Rønning M, Blix HS, Harbø BT, Strøm H. Different versions of the anatomical therapeutic chemical classification system and the defined daily dose—are drug utilisation data comparable? Eur J Clin Pharmacol. 2000;56:723–7.
Vlahovic-Palcevski V, Gantumur M, Radosevic N, et al. Coping with changes in defined daily dose in longitudinal drug consumption databases. Pharm World Sci. 2010;32:125–9.
Wettermark B, Godman B, Jacobsson B, Haaijer-Ruskamp F. Soft regulations in pharmaceutical policymaking—an overview of current approaches and their consequences. Appl Health Econ Health Policy. 2009;7:137–47.
McDowall D, et al. Interrupted time series analysis. In: Sage University Papers series on quantitative applications in the social sciences, ps 7–21. Thousand Oaks: Sage Publications Inc.; 1980.
Ross-Degnan D, et al. Examining product risk in context. Market withdrawal of zomepirac as a case study. J Am Med Assoc. 1993;270:1937–42.
Durbin J, Watson GS. Testing for serial correlation in least square regression. Biometrika. 1951;37:409–28.
Brennan P, Croft P. Interpreting the results of observational research: chance is not such a fine thing. BMJ. 1994;309:727–30.
Godman B, Schmitzer M, Burkhardt T, Buscics A, Gustafsson LL. Influence of lifting prescribing restrictions for losartan in Austria; implications for other classes. Pharmacoepidemiol Drug Saf. 2012;21(suppl 3):295–6.
Godman B, Bennett K, Bennie M, Burkhardt T, et al. Are health authorities and health insurance companies taking full advantage of the availability of generic risperidone; implications for the future? Pharmacoepidemiol Drug Saf. 2012;21(suppl 3):55–6.
Signorovitch J, Birnbaum H, Ben-Hamadi R, et al. Increased olanzapine discontinuation and health care resource utilization following a Medicaid policy change. J Clin Psychiatry. 2011;72(6):787–94.
Soumerai SB, Zhang F, Ross-Degnan D, et al. Use of atypical antipsychotic drugs for schizophrenia in Maine Medicaid following a policy change. Health Aff. 2008;3:w185–95.
Acknowledgements
The authors acknowledge the help of Karl Arnberg (TLV) for his helpful comments, especially regarding potential follow-on studies.
Financial disclosure
BW, MP, and JM are employed by Stockholm County Council, Stockholm. The authors have no other conflicts of interest to declare. This work was in part supported by Grants from the Karolinska Institutet, Sweden. No writing assistance was provided for this article.
Author contributions
Brian Godman undertook the analysis of utilization and expenditure data, produced the first draft, and submitted the article following comments. He is the guarantor for the results presented in the article. Marie Persson critiqued the first draft and provided data on expenditure on patented antidepressants in Stockholm County Council. Jamilette Miranda undertook the statistical analysis and critiqued the results. Peter Skiöld provided the rationale behind the study, provided data on the recent reforms regarding generic prices in Sweden, and provided input on the prescription restrictions for duloxetine. Björn Wettermark provided the rationale behind the study and the methodology, provided the data for Sweden and reviewed the results. Corrado Barbui critiqued early drafts especially with respect to the effectiveness and side-effects of the newer antidepressants. Lars L Gustafsson critiqued earlier drafts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Godman, B., Persson, M., Miranda, J. et al. Changes in the Utilization of Venlafaxine after the Introduction of Generics in Sweden. Appl Health Econ Health Policy 11, 383–393 (2013). https://doi.org/10.1007/s40258-013-0037-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-013-0037-x