Abstract
Purpose
The effectiveness of diabetes self-management interventions has been more generally demonstrated in adults, but there is little evidence of diabetes self-management specific to older adults situated in Iran. The purpose of this study was to evaluate the effectiveness of Persian Diabetes Self-Management Education on self-efficacy, quality of life, self-care activity, depression and loneliness in older adults with type 2 diabetes.
Methods
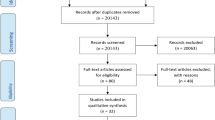
In pilot randomized controlled trial, a total of 34 participants ≥60 years with type 2 diabetes were randomly assigned into intervention (n = 17) and control (n = 17) group in an outpatient diabetes clinic in Tehran. To assess the primary outcome of participant experiences, the Diabetes Management Self-efficacy Scale (DMSES) was the method of measurement. The Diabetes Quality of Life-Basic Clinical Inventory (DQoL-BCI), Patient Health Questionnaire-9 (PHQ-9), Diabetes Self-Management Education Scale (DSMES), and adult Social-Emotional Loneliness Scale Short form (SELSA-S) were used as secondary outcomes. Participants’ evaluations were completed at baseline, while measurements were conducted two and four weeks after allocation, using repeated measurements of Univariate and multivariate ANOVA (adjusted for baseline values) to analyze the data.
Results
In the multivariate model, there was a significant difference between the control and intervention groups regarding reported quality of life (p = 0.04) and the medical-domain’s reported self-efficacy (p = 0.02). However, there were no significant differences in the reported self-management, depression, loneliness, as well as the other domain of self-efficacy; as compared between the two groups before and after intervention.
Conclusion
The study depicts a promising impact on older adults, imparted by the pertinent program. The finding showed PDSME has a positive effect on quality of life and medical control domain of self-efficacy. This pilot study showed that the program is feasible and duly beneficial if delivered to older adults. This pilot proves appealing to begin further testing within a larger sample population.

Similar content being viewed by others
References
International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels: International Diabetes Federation; 2019.
UNDo E. World population prospects: the 2004 revision: volume I: comprehensive tables. United Nations Publications. 2006.
Amos AF, McCarty DJ, Zimmet P. The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diabet Med. 1997;14(S5):S7–S85.
Majeed A, El-Sayed AA, Khoja T, Alshamsan R, Millett C, Rawaf S. Diabetes in the middle-east and North Africa: an update. Diabetes Res Clin Pract. 2014;103(2):218–22.
Esteghamati A, Larijani B, Aghajani MH, Ghaemi F, Kermanchi J, Shahrami A, et al. Diabetes in Iran: prospective analysis from first nationwide diabetes report of national program for prevention and control of diabetes (NPPCD-2016). Sci Rep. 2017;7(1):13461.
Peykari N, Djalalinia S, Qorbani M, Sobhani S, Farzadfar F, Larijani B. Socioeconomic inequalities and diabetes: a systematic review from Iran. J Diabetes Metab Disorders. 2015;14(1):8.
Heisler M, Piette JD, Spencer M, Kieffer E, Vijan S. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care. 2005;28(4):816–22.
Funnell MM. What's new, what's different. Nursing 2017. 2008;38(10):47–9.
Health UDo, Services H. National Diabetes Information Clearinghouse (NDIC). National diabetes statistics. 2011.
National Diabetes Information Clearinghouse. Health statistics. 2008.
Haas L, Maryniuk M, Beck J, Cox CE, Duker P, Edwards L, et al. National standards for diabetes self-management education and support. Diabetes Educator. 2012;38(5):619–29.
Rokach A, Miller Y, Shick S, Abu R, Matot I. Surgery and caregiving: loneliness of the patients and those who care for them. Open J Med Psychol. 2014;3(03):222–34.
Wilson TD. Health literacy and self-efficacy as correlates of self-management of type 2 diabetes in middle-aged and older adults: West Virginia University libraries. 2012.
Educators AAoD. AADE guidelines for the practice of diabetes self-management education and training (DSME/T). Diabetes Educator. 2009;35(3-suppl):85S–107S.
Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet. 2006;368(9529):29–36.
California Healthcare Foundation/American Geriatrics Society Panel in Improving Care for Elders with Diabetes C. Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatrics Soc. 2003;51(5s):265–80.
Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, et al. Diabetes in older adults. Diabetes Care. 2012;35(12):2650–64.
Bell RA, Andrews JS, Arcury TA, Snively BM, Golden SL, Quandt SA. Depressive symptoms and diabetes self-management among rural older adults. Am J Health Behav. 2010;34(1):36–44.
Egede LE, Osborn CY. Role of motivation in the relationship between depression, self-care, and glycemic control in adults with type 2 diabetes. Diabetes Educator. 2010;36(2):276–83.
Katon W, Russo J, Lin EH, Heckbert SR, Karter AJ, Williams LH, et al. Diabetes and poor disease control: is comorbid depression associated with poor medication adherence or lack of treatment intensification? Psychosom Med. 2009;71(9):965–72.
Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–60.
McKellar JD, Humphreys K, Piette JD. Depression increases diabetes symptoms by complicating patients’ self-care adherence. Diabetes Educator. 2004;30(3):485–92.
Pineda Olvera AE, Stewart SM, Galindo L, Stephens J. Diabetes, depression, and metabolic control in Latinas. Cult Divers Ethn Minor Psychol. 2007;13(3):225–31.
Landeiro F, Barrows P, Musson EN, Gray AM, Leal J. Reducing social isolation and loneliness in older people: a systematic review protocol. BMJ Open. 2017;7(5):e013778.
Kim H, Kim K. Health-related quality-of-life and diabetes self-care activity in elderly patients with diabetes in Korea. J Community Health. 2017;42(5):998–1007.
Weinger K, Beverly EA, Smaldone A. Diabetes self-care and the older adult. West J Nurs Res. 2014;36(9):1272–98.
Lakey W, Barnard K, Batch B, Chiswell K, Tasneem A, Green J. Are current clinical trials in diabetes addressing important issues in diabetes care? Diabetologia. 2013;56(6):1226–35.
Nicolaou M, Vlaar E, Van Valkengoed I, Middelkoop B, Stronks K, Nierkens V. Development of a diabetes prevention program for Surinamese south Asians in the Netherlands. Health Promot Int. 2013;29(4):680–91.
Shakibazadeh E, Bartholomew LK, Rashidian A, Larijani B. Persian diabetes self-management education (PDSME) program: evaluation of effectiveness in Iran. Health Promot Int. 2015;31(3):623–34.
Association AD. 2. Classification and diagnosis of diabetes. Diabetes care. 2017;40(Supplement 1):S11–24.
Shrewsbury VA, O'Connor J, Steinbeck KS, Stevenson K, Lee A, Hill AJ, et al. A randomised controlled trial of a community-based healthy lifestyle program for overweight and obese adolescents: the Loozit® study protocol. BMC Public Health. 2009;9(1):119.
McDowell J, Courtney M, Edwards H, Shortridge-Baggett L. Validation of the Australian/English version of the diabetes management self-efficacy scale. Int J Nurs Pract. 2005;11(4):177–84.
Noroozi A, Tahmasebi R. The diabetes management self-efficacy scale: translation and psychometric evaluation of the Iranian version. Nursing Pract Today. 2015;1(1):9–16.
Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–50.
Xu Y, Toobert D, Savage C, Pan W, Whitmer K. Factors influencing diabetes self-management in Chinese people with type 2 diabetes. Res Nurs Health. 2008;31(6):613–25.
Boogar IR, Mohajeri-Tehrani MR, Besharat MA, Talepasand S. The effect of sociostructural and collaborative decision-making on diabetes self-management. Iran J Public Health. 2013;42(3):280.
Burroughs TE, Desikan R, Waterman BM, Gilin D, McGill J. Development and validation of the diabetes quality of life brief clinical inventory. Diabetes Spectrum. 2004;17(1):41–9.
Mirfeizi M, Jafarabadi MA, Toorzani ZM, Mohammadi SM, Azad MD, Mohammadi AV, et al. Feasibility, reliability and validity of the Iranian version of the diabetes quality of life brief clinical inventory (IDQOL-BCI). Diabetes Res Clin Pract. 2012;96(2):237–47.
Kroenke K, Spitzer RL, Williams JB. The phq-9. J Gen Intern Med. 2001;16(9):606–13.
Dadfar M, Kalibatseva Z, Lester D. Reliability and validity of the Farsi version of the patient health Questionnaire-9 (PHQ-9) with Iranian psychiatric outpatients. Trends Psychiat Psychother. 2018;40(2):144–51.
Ditommaso E, Brannen C, Best LA. Measurement and validity characteristics of the short version of the social and emotional loneliness scale for adults. Educ Psychol Meas. 2004;64(1):99–119.
Jowkar B. Psychometric properties of the short form of the social and emotional loneliness scale for adults (SELSA-S). Int J Behavior Sci. 2012;5(4):311–7.
Preumont V, Hermans M, Buysschaert M, Jamart J. Special considerations in the management and education of older persons with diabetes. Diabetes Metab. 2009;35:A60.
Jahromi MK, Ramezanli S, Taheri L. Effectiveness of diabetes self-management education on quality of life in diabetic elderly females. Global J Health Sci. 2015;7(1):10.
Chen SM, Creedy D, Lin H-S, Wollin J. Effects of motivational interviewing intervention on self-management, psychological and glycemic outcomes in type 2 diabetes: a randomized controlled trial. Int J Nurs Stud. 2012;49(6):637–44.
Egede LE, Ellis C. Diabetes and depression: global perspectives. Diabetes Res Clin Pract. 2010;87(3):302–12.
Chen H-Y, Baumgardner DJ, Rice JP. Peer reviewed: Health-related quality of life among adults with multiple chronic conditions in the united states, behavioral risk factor surveillance system, 2007. Prevent Chronic Dis. 2011;8(1):A09.
Goode P. The effect of a diabetes self-management program for African Americans in a faith-based setting: the University of North Carolina at Greensboro. 2016.
Barclay R, Tate RB. Response shift recalibration and reprioritization in health-related quality of life was identified prospectively in older men with and without stroke. J Clin Epidemiol. 2014;67(5):500–7.
Finucane ML, Slovic P, Hibbard JH, Peters E, Mertz C, MacGregor DG. Aging and decision-making competence: an analysis of comprehension and consistency skills in older versus younger adults considering health-plan options. J Behav Decis Mak. 2002;15(2):141–64.
Zheng F, Liu S, Liu Y, Deng L. Effects of an outpatient diabetes self-management education on patients with type 2 diabetes in China: a randomized controlled trial. J Diabetes Res. 2019;2019:1–7.
Martínez de Dávila MG, Moreno Monsiváis MG, Sauceda Flores PF, Vázquez Arreola L, Guadalupe S, Ortíz M, et al. Case management model in patients with type 2 diabetes mellitus. Investigación y Educación en Enfermería. 2006;24(1):58–65.
Glasgow RE, Toobert DJ, Gillette CD. Psychosocial barriers to diabetes self-management and quality of life. Diabetes spectrum. 2001;14(1):33–41.
Zagarins SE, Allen NA, Garb JL, Welch G. Improvement in glycemic control following a diabetes education intervention is associated with change in diabetes distress but not change in depressive symptoms. J Behav Med. 2012;35(3):299–304.
Fortmann AL, Gallo LC, Philis-Tsimikas A. Glycemic control among Latinos with type 2 diabetes: the role of social-environmental support resources. Health Psychol. 2011;30(3):251–8.
Solis JM, Marks G, Garcia M, Shelton D. Acculturation, access to care, and use of preventive services by Hispanics: findings from HHANES 1982-84. Am J Public Health. 1990;80(Suppl):11–9.
Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care. 2003;26(10):2822–8.
De Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63(4):619–30.
Lustman PJ, Clouse RE. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complicat. 2005;19(2):113–22.
Richardson LK, Egede LE, Mueller M, Echols CL, Gebregziabher M. Longitudinal effects of depression on glycemic control in veterans with Type 2 diabetes. General Hospital Psychiat. 2008;30(6):509.
Shakibazadeh E, Larijani B, Shojaeezadeh D, Rashidian A, Forouzanfar M, Bartholomew L. Patients’ perspectives on factors that influence diabetes self-care. Iran J Public Health. 2011;40(4):146–58.
Acknowledgments
The authors extend sincere appreciation to the many people who made this research possible: staff at the Endocrinology and Metabolism Clinical Sciences Institute, Tehran university of Medical science Tehran, Iran. Program managers and facilitators were particularly critical to the data collection. Finally, the participants who attended in the research are thanked for their time and contributions to the evidence required to improve healthcare.
Funding
This study was funded by Shahid Beheshti University of Medical Science (grant number 15847).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saghaee, A., Ghahari, S., Nasli-Esfahani, E. et al. Evaluation of the effectiveness of Persian diabetes self-management education in older adults with type 2 diabetes at a diabetes outpatient clinic in Tehran: a pilot randomized control trial. J Diabetes Metab Disord 19, 1491–1504 (2020). https://doi.org/10.1007/s40200-020-00684-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-020-00684-0