Abstract
Purpose
COVID-19, a disease that can be transmitted from person to person and with serious health problems, can be associated with mental health disorders. In this study, we evaluated the prevalence and severity of depression, anxiety, stress, and stress perception among a group of patients with COVID-19 who were hospitalized.
Methods
In this cross-sectional study, 106 inpatients with COVID-19 who had stable clinical conditions were evaluated psychologically by two questionnaires: Depression, Anxiety and Stress Scales-21 (DASS-21) and Perceived Stress Scale (PSS-4).
Results
More than one third of patients had underlying disease. Overall, 97.2% of patients with COVID-19 had some degree of depression. Severity of depression, according to the DASS questionnaire, was 85.8%. All patients (100%) had severe (0.9%) and very severe (99.1%) anxiety. Regarding to stress levels, 97.1% of patients had some degree of stress. In the severity of stress category, 84.9% of patients had severe and very severe stress. In terms of perceived stress, 73.6% of patients had high levels and 22.6% had moderate levels. A positive strong correlation was found between depression and perceived stress (Coefficient: 0.33, P-value: 0.001). Correlation between anxiety and perceived stress was statistically significant (Coefficient: 0.2, P-value: 0.04).
Conclusions
The existence of such a high prevalence and severity of psychiatric disorders among hospitalized patients with COVID-19 underscores the need for serious attention to the mental health status of these patients. It seems that health policymakers need to have coherent plans for screening cases and managing related situations.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the cause of the transmission of the novel coronavirus disease-19 (COVID-19), which is associated with the ability to transmit the disease from humans to humans. The disease is associated with serious health problems and can be fatal [1]. As some authors have suggested, severe acute respiratory syndrome (SARS) caused by coronavirus, as the first outbreak of an infectious disease in the 21st century, was not the last one and COVID-19 was introduced as a pandemic earlier this century [2].
The outbreak was described by the World Health Organization as Public Health Emergency of International Concern (PHEIC) [3]. The disease has, in recent times, been associated with social disruptions and worrying economic consequences. These points, along with the risk of stigmatization and discrimination, can lead to mental health disorders for public and especially in patients with the disease [4,5,6].
With the increase in the number of infected patients and their deaths, many patients may experience psychological distress and physical problems [7]. Unpredictability and uncertainty of the disease condition of different aspects of epidemiology and effective methods of treatment, puts people exposed to stressful situations [8]. Fear of the consequences of a deadly disease, combined with severe anxiety and mental distress, which can coincide with insomnia and the physical effects of the disease, can create unfavorable conditions for patients due to the aggravation of mental health disorders [9,10,11].
Early in the SARS epidemic, hospitalized patients raised concerns such as fear, loneliness, fatigue, and anger. They experienced anxiety as a result of fever and the effects of insomnia. [12]. Anxiety is seen as a significant effect of epidemics with high levels of involvement and risk of death, both among people who are directly involved in the disease and among the masses. This can be accompanied by depression and other psychological problems [13].
Duan et al., noting that the epidemic of diseases can have negative effects on individuals, emphasize the existence of psychological distress following the spread of the COVID-19 and the need for active and appropriate intervention in this area [14]. In this regard Zheng noted the high prevalence of psychiatric disorders among survivors of the SARS-CoV-2 epidemic, including depression and post-traumatic stress disorder, and emphasized the importance of prevention, screening and treatment of associated psychiatric disorders during the COVID-19 pandemic [15].
In this study, we examined the mental health status of patients with COVID-19 who were hospitalized. After becoming clinically stable, these patients were evaluated for some psychiatric symptoms such as depression, anxiety, stress, and perceived stress.
This study also has investigated the possible impact of occupational, economic and social status of patients on their mental health following the spread of COVID-19. Examining the impact of demographic differences such as marital status in this area is another point of discussion. Due to the interaction of some underlying diseases such as hypertension and diabetes and psychiatric disorders [16, 17], in this study, we also investigated the relationship between these diseases and related psychiatric disorders in patients with COVID-19.
Method
Study design
This study was a cross-sectional study conducted in one of the largest referral centers for patients with COVID-19 requiring hospitalization in Alborz, Iran. Three psychiatric nurses performed initial screening of patients based on inclusion criteria to select patients to enter the project. These patients were selected from inpatients in isolated treatment wards. All psychiatric nurses had complete personal protective equipment during screening. All information collected was transmitted electronically. Patients were consulted and, if desired, entered the study after obtaining informed consent. Participants were told that in addition to receiving the required medical services, if they needed psychological or psychiatric services during the project, they would be provided free of charge if they wished.
Inclusion and exclusion criteria
Participants in the project were adults who, based on medical records, were diagnosed with COVID-19 and were clinically stable and willing to participate in the research project. Being over the age of 18 was one of the criteria for entering the study. If the patient did not want to continue the cooperation at any stage of the project, he/she would be excluded from the study.
Data Collection
Patients ‘demographic information was collected as much as possible through patients’ medical records and were checked with the patient. These included gender, age, marital status, employment status, and education. Patients were assessed through two questionnaires, the Depression, Anxiety and Stress Scales-21 (DASS − 21) and Perceived Stress Scale-4 (PSS-4).
Procedure
The Site
The project site is one of the largest educational hospital centers in Alborz province, Iran, where patients go for screening and treatment of COVID-19 disease or are referred to this center through primary care centers. Patients admitted to the isolated ward with COVID-19 diagnosis were evaluated.
Selection of Participants
In this study, according to the inclusion criteria, 120 patients were evaluated and finally 106 patients were included in the study.
Scales
The Depression, Anxiety and Stress Scales-21(DASS-21)
DASS-21 is a suitable tool for measuring depression, anxiety and stress, for research and clinical purposes and for such a purpose, is a validated tool among various ethnicity and population groups [18]. This tool has been evaluated in Iran in terms of reliability and validity and its persian version has satisfactory psychometric properties and can be used by the Iranian population [19]. They reported the Cronbach’s alpha as 0.94 for the total scales of the questionnaire, and 0.85, 0.85, and 0.87 for depression, anxiety, and stress scales, respectively. This tool has 3 scales, each containing 7 questions. The final score is also obtained through the sum of the scores. Each question varies from zero (“it doesn’t apply to me at all”) to 3 (“it applies to me completely”). Since this questionnaire is a shortened form of the main scale (42 questions), the final score of each subscale must be doubled. Each of the subscales is divided into 4 categories based on the score obtained: normal, moderate, severe and very severe [20].
Perceived Stress Scale-4 (PSS-4)
PSS is one of the most widely used tools for measuring psychological stress in clinical and non-clinical situations. Its internal consistency and validity have been shown in various studies [21]. In Iran, Persian versions of its various versions (including pss-4) have been evaluated and have satisfactory psychometric properties. In a study in Iran, the Cronbach’s alpha coefficients for it was 0.77 [22]. Version 4 (PSS-4) has 2 positive and 2negative phrases and its score range is from 0 to 16, and it has a triple classification based on intensity as high, moderate, and low [23].
Statistical analysis
The obtained information was entered into the SPSS version 23. Continuous and categorical variables are expressed as mean (standard deviation (SD)) and frequency (percentage) respectively. Chi-square was used to investigate the association between qualitative variables with mental health status. Pearson correlation test was used to assess correlation between scales of DASS-21 and PSS-4 questionnaires. A P-value less than 0.05 was considered as statistically significant.
Ethical considerations
The Ethics Committee of Alborz University of Medical Sciences, Iran, has approved this research. (IR.ABZUMS.REC.1399.011, date: 06-04-2020). In the case of each of the patients under study, who needed further evaluation in terms of psychiatric issues, the possibility of relevant psychiatric evaluations was provided to the patient so that, if desired, appropriate treatment could be performed. These facilities were provided free of charge and only if the patient so wished. Given that the research data were based on human participants, the study was conducted according to Helsinki rules. Participants were informed of the objectives of the study and its nature. They were assured that the information obtained from them would remain confidential.
Result
The total number of participants in the study was 106 patients and all of the questionnaires were filled completely (response rate 100%). The mean age of the patients was 55 (SD = 16.92) years. 51.9% were men and 48.1% were women. 86.8% of the participants were married and the rest were single. In terms of job status, 37.7% were house-worker and 24.5%were unemployed. 20.8% were employees and 15.1% were retired. 39.6% were illiterate and equally had a diploma and the rest had a university degree. (Table 1) None of the patients had a history of alcohol consumption and 2.8%were smoker. 0.8% of patients had a history of substance use. Among the patients studied, 39 patients) 36.8%( had a history of psychiatric disorders, and 5 of them (4.7%) had a history of taking psychiatric medications. Anxiety, depression and somatization were the most common disorders.
The prevalence of underlying diseases in hospitalized patients with COVID-19 in our study was as follows: hypertension (38.7%), diabetes mellitus (31.1%), hyperlipidemia (31.1%), ischemic heart disease (25.5%), asthma (7.5%), renal disease (6.6%), cerebrovascular accident (5.7%), chronic obstructive pulmonary disease (3.8%), cancer (1.9%) and rheumatological diseases (1.9%). Also, 11.3% of patients were taking corticosteroids.
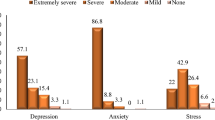
Average subclass scores based on the overall score of the DASS-21 and PSS-4 questionnaires on depression was 29.94 (SD = 8.25), anxiety was 31.53 (SD = 4.22), stress was 30.34 (SD = 5.95), and the perceived stress was 10.29 (SD = 3.17) (Fig. 1).
Overall, 97.2% of patients with COVID-19 had some degree of depression. Severity of depression, according to the DASS questionnaire, was 85.8%. All patients (100%) had severe (0.9%) and very severe (99.1%) anxiety. Regarding to stress levels, 97.1% of patients had some degree of stress. In the severity of stress category, 84.9% of patients had severe and very severe stress. In terms of perceived stress, 73.6% of patients had high levels and 22.6% had moderate levels (Fig. 2).
There was no statistically significant association between gender and age with depression, anxiety, stress and perception of stress. There was a statistically significant relationship between job status and the severity of depression among patients admitted with COVID-19 ) P-value: 0.006(.The highest prevalence of patients with severe and very severe depression was in the group of patients with freelancers.
There was also a significant statistical association between education level and severity of depression (P-value: 0.001). The highest prevalence of patients with severe and very severe depression was observed in the group of patients with diploma and illiteracy education. Being married in patients was associated with increased anxiety) P-value: 0.010). Having rheumatological disease was statistically associated with stress (P-value < 0.001).
Correlation between Scales of DASS-21 and PSS-4 questionnaires of hospitalized patients with COVID-19 is presented in Table 2. A positive strong correlation was found between depression and perceived stress (Coefficient: 0.33, P-value: 0.001). A similar correlation was found between anxiety and perceived stress (Coefficient: 0.2, P-value: 0.04).
Discussion
The average age of patients in our study was 55) Std. Deviation = 16.92) years. In some other studies, most hospitalized patients with COVID-19 were in the age range of 31–70 years (75.97%) [24].
Regarding the relationship between socioeconomic status and psychiatric disorders, in our study, the highest rate of depression was in the group of patients with diploma degree and illiterate and then in the group of people with bachelor’s degree. In various studies, there is a difference of opinion between the relationship between socio-economic levels and education with depression, but most studies point to the inverse relationship between them [25]. Also, in our study, people with a long history of freelancers and house workers were more likely to be depressed than retired people and government employees. The existence of economic problems and attention to economic prospects after the COVID-19 pandemic has raised concerns in the general public about meeting the essential needs and economic stability. This can be accompanied by mental health disorders, including depression, especially in people with occupations more likely to be affected by these economic conditions [26, 27]. Managing existing resources, paying attention to positive international experiences and using the potential of social capital can be effective steps in this regard [28, 29].
Regarding the relationship between marital status and perceived stress, some studies have suggested a protective role for marriage in this area as well as in anxiety [30]. Due to the uncertainty of the conditions of the COVID-19 [8]. the study of the effectiveness of common protective factors in this field requires further research. The role of environmental and social factors in this regard seems important. Given the complexity of the conditions associated with COVID-19, an accurate interpretation of the relationship between marriage and anxiety and stress among these patients requires further evaluation in other related studies.
One of the points of our study was the high number of patients with underlying diseases among the COVID-19 patients. These underlying diseases and their prevalence in our study were hypertension (38.7%), diabetes mellitus (31.1%), hyperlipidemia (31.1%), ischemic heart disease (25.5%), asthma (7.5%) and more, respectively. In a systematic review and meta-analysis, the prevalence of these underlying diseases or conditions in people infected with SARS-CoV-2 in hospitalized patients, respectively, has been as follows: hypertension (16.37%), cardiovascular disease (12.11%), smoking history (7.63%) and diabetes (7.87%) [31]. There is a similarity between our study and other studies in terms of the type of underlying disease associated with the COVID-19 .However, due to differences in the number of populations studied, it is not possible to compare the prevalence. In general, having physical illnesses that weaken the immune system and physical strength is a factor that exacerbate COVID-19 disease [32]. Given the purpose of this study, which assesses patients with COVID-19 in terms of depression, anxiety and stress, it is important to pay attention to this issue. Correlation of physical and mental illnesses is an important challenge in modern medicine and is associated with a great deal of interaction [33]. In our study, there was no significant relationship between underlying diseases and psychiatric disorders in patients. Summarizing this result requires larger studies, preferably multicenter samples with larger sample sizes.
Lim et al. described the first COVID-19 tertiary transmission cases in South Korea. They described a 54-year-old man with no history of physical or mental illness, smoking or drugs. During his hospitalization and isolation, he developed depression, insomnia, and suicidal ideation while his treatment eventually progressed satisfactorily. Also, the patient experienced stress in the context of people’s reactions to patients with COVID-19, which he received through media reports. The patient was subsequently consulted by a psychiatrist and received medication for the problem. The authors cited disease-related isolation as one of the major causes of psychological symptoms in patients [34]. According to various sources, quarantine conditions for various reasons have negative psychological effects. These reasons include long-term quarantine, insufficient information, frustration, and stigmatization. Some experts also talk about its long-term negative effects. They have advised that the course of quarantine be as short as possible and that appropriate information be provided to patients [35].
On the other hand, one of the points that has been considered in recent years is the relationship between infections caused by respiratory viruses and subsequent mood disorders. As an example ,in one study, the relationship between seropositivity for influenza and coronavirus with history of mood disorders was reported [36]. This focuses on the biological aspects of the relationship between coronavirus disease and mood disorders. Definite conclusions in this regard also need to pay attention to various factors affecting this field and conduct more extensive studies. Examples of this group of possible connections can be seen in some scientific points of view [37, 38].
Other studies have highlighted high levels of anxiety as a form of psychological stress, especially following isolation to treat COVID-19 disease [39]. In our study, all patients who were hospitalized and isolated had some degree of anxiety, and the severity of all cases was severe and very severe. Anxiety symptoms may be mild at first, but there is a risk that they will suddenly worsen over the course of a few days [33]Due to the severity of anxiety symptoms in hospitalized and isolated patients, and especially due to the anticipation of anxiety disorders among hospitalized patients, it seems that the use of psychological and psychiatric counseling methods, in person or through online hospital systems, can be an effective way to control patients’ clinical condition. The use of other anxiety reduction techniques, such as progressive muscle relaxation, has been suggested by some researchers [39].
More than one-third of the patients studied had a history of psychiatric disorders. It is important to pay attention to various aspects of the psychiatric condition of patients with a history of mental health disorders [40]. At the time of hospitalization and after clinically stability, all patients revealed anxiety and other psychiatric manifestations. According to a review study, the overall prevalence of psychiatric disorders in the general population in Iran was 31.03% [41]. In another study, the prevalence of mental health disorders was 23.4%. The prevalence of anxiety and somatization syndrome was higher than other disorders [42]. In a study conducted to assess the prevalence of 310 diseases and injuries in Iran and neighboring countries between 1990 and 2015, one of the most significant changes was increasing the effect of mental disorder, in years lived with disability(YLD). Meanwhile, major depressive disorder has been one of the main causes of YLD among the Iranian population [43]. Also in a study in Iran, the prevalence of depression among patients with diabetes was estimated at 54% [43]. In another study examining the prevalence of depression and anxiety among patients with maxillofacial trauma as an acute event, the prevalence of some degrees of depression and anxiety was 24% and 32.5%, respectively [44]. They reported a higher prevalence of depression and anxiety in this group than in the control group.
According to the studies conducted in recent years in Iran, the prevalence of mental health disorders in Iran is increasing. On the other hand, according to various studies, during the hospitalization of patients, due to acute or chronic diseases, there is an increase in the prevalence of depression with anxiety among patients. These results are consistent with the results of our study, in which degrees of depression and anxiety were seen in 97.1% and 100% of hospitalized patients, respectively.
Rossely et al. examined a group of hospitalized patients, noting the high level of anxiety and depression among these patients compared to other individuals, and emphasized the need for screening for psychiatric distress during hospitalization in different hospital wards [45]. What we see in patients in our study is that patients with COVID-19 have a high severity of depression, anxiety, and stress, along with high levels of perceived stress and it is very important to pay attention to their mental health status in addition to their medical status.
IsHak et al. investigated a group of hospitalized patients and reported that the prevalence of depression among these patients was between 5 and 60 percent and an average of 33 percent. They suggested that hospitalized patients be screened for depression. Depression among hospitalized patients has been associated with poorer functional outcomes, worse physical health, and re-hospitalization [46]. As noted, in our study, 97.1% of patients had some degree of depression during hospitalization. In addition, DASS severity of depression scale, had severe and very severe results, in 85.8% of them, indicating a high prevalence of depression and its severity in patients. Given the serious health concerns of patients with COVID-19, screening and the effective treatment of depression in these patients, along with proper follow-up after discharge, may play an effective role in improving their physical health.
In a study conducted by Zatzick et al., the status of post-traumatic stress disorder, depression, and their relationship to the patient’s subsequent occupational performance were assessed 12 months after the trauma event, and each of these was associated with a marked functional decline. They emphasized the need for early acute interventions in order to provide possible access to appropriate occupational performance in patients [47]. Given the economic problems associated with the COVID-19 pandemic, it seems that the therapeutic aspects of these patients in terms of mental health disorders may have a positive effect on improving their job performance.
Lee et al. examined the stress and psychological stress levels of 79 and 96 patients in two hospitals during the outbreak of SARS and one year thereafter. They had higher stress levels at the time of outbreak compared to the control group. The important point in their study is that one year after this study, in both groups, the scores of this test showed that the level of stress in these patients remained high. In addition, a year after the outbreak, they still showed worrying levels of depression, anxiety, and post-traumatic stress [48]. Given the similarities between the causative agent and the outbreak conditions of SARS and COVID-19 (although according to many experts, COVID-19 is more worrying in terms of severity and extent than SARS[49]), concerns about the persistence of these demonstrations are also present among these patients.
In a study conducted 30 months after the outbreak of SARS on treated SARS survivors, the cumulative incidence of psychiatric disorders was 58.9%, and the prevalence of any psychiatric disorders at the time of the study was 33.3%. PTSD and subsequent depressive disorders were the most common disorders. Accordingly, they described SARS’ outbreak as a mental health catastrophe and stressed the need for planning to identify and treat psychiatric disorders during other infectious epidemics [50]. Given all the available evidence and the results of our study, it is important to pay serious attention to the mental health disorders of patients with COVID-19 in order to better control possible psychiatric disorders in future.
Also, a review article on SARS outbreak reported clear clinical symptoms among patients, between 17% and 43% for depression, and 23–48% for nonspecific anxiety. They reported a high prevalence of psychiatric disorders among patients, and emphasized the need to prevent and follow up on similar conditions [51].
In another study, Chua et al. used the Perceived Stress Scale (PSS) questionnaire to examine the mental health status of hospitalized patients with SARS diagnosis. They reported a significantly higher level of stress among patients compared to the control group. They identified a clear link between stress and negative psychological effects [52]. In our study, there is, in a similar situation, a significant positive statistical relationship between depression and perceived stress, as well as a positive statistical relationship between anxiety and perceived stress. There was also a positive statistical relationship between anxiety and stress. And among the group of patients with very severe depression, the highest number of patients with high perceived stress was present.
Conclusions
Depression, anxiety, stress and perceived stress were highly prevalent among patients with COVID-19 under study. There was also a high correlation between depression and anxiety with perceived stress. The high prevalence and severity of these psychiatric disorders among patients with COVID-19 emphasizes the need to pay more attention to their mental health status. It seems that health policymakers need to have coherent plans for screening cases and managing related situations.
Summary
In this study, we evaluated the psychiatric status of patients with COVID-19 who were hospitalized. About one-third of these patients had other underlying illness, the most common of which were hypertension, diabetes, hyperlipidemia, and ischemic heart disease. The prevalence of depression, anxiety and stress among patients was very high and also had a high severity. The level of perceived stress was also high in most patients. There was a strong association between depression and anxiety with patients’ perceived stress.
The existence of such a high prevalence and severity of psychiatric disorders among hospitalized patients with COVID-19 underscores the need for serious attention to the mental health status of these patients. It seems that health policymakers need to have coherent plans for screening cases and managing related situations. Also, following the process of patients’ psychiatric treatments and implementing related educational programs can be effective at the community level, given the extent of the disease.
Limitations
Due to the high distribution of the disease, in order to achieve more complete results, it is recommended to conduct larger studies with a larger sample size and in a multicenter manner.
Data availability
All study data and materials are available.
References
Li W, et al. Progression of Mental Health Services during the COVID-19 Outbreak in China. Int J Biol Sci. 2020;16(10):1732.
Database2020b, Database2020a. World Health Organization, speeches, March 11,2020. Available from https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020..
Database2020a, Database2020k. World Health Organization, speeches, January30,2020. Available from https://who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov).
Ransing R, et al. Early career psychiatrists’ perspectives on the mental health impact and care of the COVID-19 pandemic across the world. Asian J Psychiatry, 2020:102085.
Badrfam R, Zandifar A. Stigma Over COVID-19; New conception beyond individual sense. Arch Med Res. 2020;51(6):593–4.
Badrfam R, Zandifar A. COVID-19 and melancholia; Different perception of the concept of stigma and loss. Iran J Psychiatry. 2020;15(3):264–5.
Bo HX, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. 2020. https://doi.org/10.1017/S0033291720000999.
Zandifar A, Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J Psychiatry. 2020;51:101990.
Xiang Y-T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–9.
Zandifar A, Badrfam R, Khonsari NM, Assareh M, Karim H, Azimzadeh M, et al. COVID-19 and medical staff’s mental health in educational hospitals in Alborz Province, Iran. Psychiatry Clin Neurosci. 2020. https://doi.org/10.1111/pcn.13098.
Zandifar A, et al. Prevalence and associated factors of posttraumatic stress symptoms and stigma among health care workers in contact with COVID-19 patients. Iran J Psychiatry. 2020;15(4):355–65.
Maunder R, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Cmaj. 2003;168(10):1245–51.
Lima CKT, et al. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res. 2020;287:112915.
Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):300–2.
Zheng W. Mental health and a novel coronavirus (2019-nCoV) in China. J Affect Disord. 2020;269:201–2.
Sandström YK, et al. Psychiatric comorbidities in patients with hypertension–a study of registered diagnoses 2009–2013 in the total population in Stockholm County, Sweden. J Hypertens. 2016;34(3):414–20.
Lankarani MM, Assari S. Association between number of comorbid medical conditions and depression among individuals with diabetes; race and ethnic variations. J Diabetes Metab Disord. 2015;14(1):56.
Norton PJ. Depression Anxiety and Stress Scales (DASS-21): Psychometric analysis across four racial groups. Anxiety Stress Coping. 2007;20(3):253–65.
Asghari A, Saed F, Dibajnia P. Psychometric properties of the Depression Anxiety Stress Scales-21 (DASS-21) in a non-clinical Iranian sample. Int J Psychol. 2008;2(2):82–102.
Antony MM, et al. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess. 1998;10(2):176.
Leung DY, Lam T-h, Chan SS. Three versions of Perceived Stress Scale: validation in a sample of Chinese cardiac patients who smoke. BMC Public Health. 2010;10(1):513.
Maroufizadeh S, Zareiyan A, Sigari N. Psychometric properties of the 14, 10 and 4-item “Perceived Stress Scale” among asthmatic patients in Iran. Payesh (Health Monitor). 2014;13(4):457–65.
Cohen S. Perceived stress in a probability sample of the United States. 1988.
Cao C, Li Y, Liu S, Fan H, Hao L. Epidemiologic features of 135 patients with coronavirus disease (COVID-19) in Tianjin, China. Disaster Med Public Health Prep. 2020;1:1–5. https://doi.org/10.1017/dmp.2020.63.
Lorant V, et al. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157(2):98–112.
Torales J, et al. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–20.
Gupta M, Abdelmaksoud A, Jafferany M, Lotti T, Sadoughifar R, Goldust M. COVID-19 and economy. Dermatol Ther. 2020;33:e13329. https://doi.org/10.1111/dth.13329.
Zandifar A, Badrfam R. Fighting COVID-19 in Iran; Economic challenges ahead. Arch Iran Med. 2020;23(4):284.
Mohammadi MR, et al. Social capital in general population of Tehran province in comparison with other provinces of Iran. J Iran Med Counc. 2019;2(3):26–34.
Ta VP, et al. Stress of singlehood: Marital status, domain-specific stress, and anxiety in a national US sample. J Soc Clin Psychol. 2017;36(6):461–85.
Emami A, et al. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8(1):e35.
Covid C, et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. Morb Mortal Wkly Rep. 2020;69(13):382.
Sartorious N. Comorbidity of mental and physical diseases: a main challenge for medicine of the 21st century. Shanghai Arch Psychiatry. 2013;25(2):68.
Lim J, et al. Case of the index patient who caused tertiary transmission of COVID-19 infection in Korea: the application of lopinavir/ritonavir for the treatment of COVID-19 infected pneumonia monitored by quantitative RT-PCR. J Korean Med Sci. 2020;35(6):e79.
Brooks SK, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20.
Okusaga O, et al. Association of seropositivity for influenza and coronaviruses with history of mood disorders and suicide attempts. J Affect Disord. 2011;130(1–2):220–5.
Zandifar A, Badrfam R. COVID-19; considering the prevalence of schizophrenia in the coming decades. Psychiatry Res. 2020;288:112982.
Badrfam R, Zandifar A. From encephalitis lethargica to COVID-19: Is there another epidemic ahead? Clin Neurol Neurosurg. 2020;196:106065.
Liu K, et al. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Ther Clin Pract. 2020;39:101132.
Seshadri S, Chatterjee BCM, Mukherjee A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian J Psychiatry. 2020;51:102071. Available online.
Mirghaed MT, Gorji HA, Panahi S. Prevalence of psychiatric disorders in Iran: A systematic review and meta-analysis. Int J Prev Med. 2020;11:21.
Noorbala AA, et al. Mental health survey of the Iranian adult population in 2015. Arch Iran Med. 2017;20(3):128–34.
Pashaki MS, et al. The prevalence of comorbid depression in patients with diabetes: A meta-analysis of observational studies. Diabetes Metab Syndr Clin Res Rev. 2019;13(6):3113–9.
Gandjalikhan-Nassab S-A-H, et al. Depression and anxiety disorders in a sample of facial trauma: A study from Iran. Med Oral Patol Oral Cir Bucal, 2016;21(4):e477-e482.
Rosselli M, et al. Screening of distress among hospitalized patients in a department of internal medicine. Asian J Psychiatry. 2015;18:91–6.
IsHak WW, et al. Screening for depression in hospitalized medical patients. J Hosp Med. 2017;12(2):118–25.
Zatzick D, et al. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg. 2008;248(3):429–37.
Lee AM, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007;52(4):233–40.
Peeri NC, et al. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020;49:717–26.
Mak IWC, et al. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31(4):318–26.
Davydow DS, et al. Psychiatric morbidity in survivors of the acute respiratory distress syndrome: a systematic review. Psychosom Med. 2008;70(4):512–9.
Chua SE, et al. Stress and psychological impact on SARS patients during the outbreak. Can J Psychiatry. 2004;49(6):385–90.
Acknowledgements
We would like to thank all the patients who participated in this study. We would also like to thank the medical staff who are responsible for the care and treatment of patients with COVID-19. We thank all those who contributed to the various stages of this project.
Funding
This study was conducted with the financial support of Alborz University of Medical Sciences. (IR.ABZUMS.REC.1399.011(.
Author information
Authors and Affiliations
Contributions
All authors had the same role in the various stages of preparing this article.
Corresponding author
Ethics declarations
Conflicts of interest/Competing interests
There is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zandifar, A., Badrfam, R., Yazdani, S. et al. Prevalence and severity of depression, anxiety, stress and perceived stress in hospitalized patients with COVID-19. J Diabetes Metab Disord 19, 1431–1438 (2020). https://doi.org/10.1007/s40200-020-00667-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-020-00667-1