Abstract
Introduction
We investigated the long-term outcomes of pediatric cataract surgeries performed with modern surgical techniques involving in-the-bag implantation of a foldable intraocular lens (IOL).
Methods
Data were retrospectively collected from 42 eyes in 30 patients who underwent surgery at 6 years and younger (average 2.5 ± 2.3 years) and were followed up for an average of 12.2 ± 2.4 years (10–17 years). Surgical procedures included anterior continuous curvilinear capsulorhexis (CCC), lens removal, posterior CCC, anterior vitrectomy, and in-the-bag IOL implantation. There were 18 unilateral (2.7 ± 2.3 years) and 12 bilateral cases (2.3 ± 2.3 years), with no significant age difference between groups (p = 0.462).
Results
The mean best-corrected visual acuity (BCVA) at the final visit was 0.453 ± 0.488 (logMAR), correlating significantly with the age at surgery (r = −0.307, p = 0.048). The unilateral group had a worse BCVA (0.658 ± 0.615) than the bilateral group (0.298 ± 0.294) (p < 0.001). On average, eyes showed a myopic shift of −6.0 ± 6.3D, which significantly correlated with surgical age (r = 0.402, p = 0.008). While the myopic shift was −8.2 ± 6.1 D in the unilateral group and −4.9 ± 6.4 D in the bilateral group, the net shift for unilateral cases (comparing pseudophakic and fellow eyes) was −4.8 D. Three eyes (7.1%) exhibited suspected glaucoma (increased intraocular pressure), but no glaucoma or other severe complications were noted. IOL exchange surgery was necessary in two eyes (4.8%) due to pronounced myopic drift and significant IOL decentration. Three eyes (7.1%) required surgery for significant visual axis opacification.
Conclusions
Contemporary surgical strategies appear to yield promising long-term outcomes in patients with infantile cataracts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
As in adult cataract surgeries, advancements in pediatric cataract surgeries have been observed over the recent decades. |
However, longitudinal outcomes of pediatric cataract surgeries, employing current technology and refined techniques, are not fully elucidated. |
What was learned from the study? |
We analyzed the 10-year surgical outcomes of pediatric surgical interventions, incorporating both anterior and posterior continuous curvilinear capsulorhexis, anterior vitrectomy, and in-the-bag implantation of an acrylic foldable intraocular lens. |
Contemporary surgical approaches offer encouraging long-term results in patients with infantile cataracts, with a reduced risk of complications such as glaucoma and visual axis opacification. |
Introduction
Technological and technical advances in adult cataract surgery have consistently emerged, encompassing improvement in microsurgical procedures, advanced instrumentation, sophisticated ophthalmic viscosurgical devices, more secure in-the-bag placement of an intraocular lens (IOL), and a refined approach to manage postoperative inflammation. Although these advancements have also benefitted pediatric cataract surgeries, overall surgical and visual outcomes for children remain suboptimal when compared to adults [1]. Pediatric cataract surgeries face challenges due to the less mature nature of children’s eyes, potential for a more severe postoperative inflammatory response, and a greater propensity for complications both during and after surgery.
Long-term analysis of surgical outcomes is crucial for all surgical procedures, but it is particularly vital for pediatric cataract surgeries. Several studies have examined the long-term (> 10 years) results of infantile cataract surgeries, both with and without IOL implantation employing traditional surgical techniques [2,3,4,5,6,7]. There is a paucity of research, however, on the long-term outcomes after modern surgical procedures that incorporate anterior and posterior continuous curvilinear capsulorhexis (CCC), anterior vitrectomy, and in-the-bag implantation of a single-piece foldable IOL.
In Japan, the governmental restriction on IOL use in children was lifted in 2011. This paper presents 10-year outcomes of cataract surgeries with IOL implantation, which included anterior and posterior CCC and anterior vitrectomy, in the pediatric demographic.
Methods
Patients
We conducted a retrospective review of the medical records of patients who underwent pediatric cataract surgery at the Department of Ophthalmology, University of Tsukuba. Inclusion criteria were patients operated on at age 6 years or younger, with a follow-up duration of at least 10 years postoperatively. Cases of traumatic cataract or cataract secondary to other ocular diseases were excluded. Given the challenges in distinguishing between congenital and developmental cataract, both clinical entities were considered for this study. While eyes of infants with systemic and ocular comorbidities were included, those with congenital glaucoma were excluded.
The study was conducted in adherence to the tenets of the Declaration of Helsinki, and the institutional review board of Tsukuba University Hospital approved the study protocol (R04-162, December 2022). The institutional review board of Tsukuba University Hospital committee waived the need for patient informed consent for the use of their medical record data, in line with the regulations of the Japanese Guidelines for Epidemiologic Study issued by the Japanese Government. Due to the observational nature of the study, clinical trial registration was not mandated.
Surgery
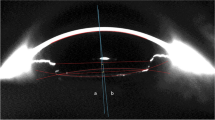
A single surgeon (TO) performed all the surgical procedures. After creating a 2.4-mm scleral tunnel incision at the superior location, an anterior CCC was fashioned using forceps. The lens material was aspirated with an irrigation/aspiration device. A posterior CCC was manually crafted using forceps through the scleral incision, followed by a 25-gauge bimanual anterior vitrectomy conducted via two side ports located at the limbus. A single-piece hydrophobic acrylic foldable IOL (AcrySof, SA60AT or SA30AT, Alcon Laboratories, Inc., Fort Worth, TX, USA) was then implanted into the capsular bag using an injector. The scleral incision was securely sutured with a 10-0 nylon, while the 25-gauge side ports remained unsutured.
The IOL power was determined using the SRK/T formula, based on data obtained from hand-held keratometry and contact ultrasound biometry performed immediately before surgery. An anticipated postoperative myopic shift was factored in, and empirical guidelines were employed to set the target refraction [8], with the IOL power capped at 30 D.
Data Collection and Interpretation
Glaucoma and suspected glaucoma classifications were based on previously established definitions for childhood glaucoma [9,10,11]. In summary, glaucoma was diagnosed using a combination of criteria, including intraocular pressure (IOP) exceeding 21 mmHg, abnormal corneal enlargement greater than 11 mm, progressive increase in cup–disc ratio, cup–disc asymmetry of 0.2 when optic discs were of similar size, focal rim thinning, requirement for medication to lower IOP, and undergoing surgery specific to glaucoma. Suspected glaucoma was identified if the IOP was above 21 mm Hg, but other definitive criteria for glaucoma were absent. In instances where abnormal glaucomatous changes or increased IOP were observed, consultations with glaucoma specialists within our hospital were initiated to ascertain the diagnosis of either glaucoma or suspected glaucoma.
Statistical Analysis
Numerical data are presented as mean ± standard deviation (SD) unless otherwise noted. Numerical data were compared between groups using the Mann–Whitney U-test. Correlations between two parameters were tested with the Pearson correlation test. For categorical data, the chi-square test and Fisher’s exact test for trend were used to assess the incidence rates. All statistical tests were two-sided, and a p-value of ≤ 0.05 was considered significant. Statistical analysis was performed using SPSS software version 29 (IBM Corp, Armonk, NY, USA).
Results
A total of 42 eyes of 30 patients met the inclusion criteria, and their medical records were analyzed. The average age at the time of cataract surgery was 2.5 ± 2.3 years (1 month–6 years) (Fig. 1), and the follow-up duration averaged 12.2 ± 2.4 years (10–17 years). Preoperative axial length was 21.19 ± 2.01 mm (16.61–26.32 mm). Preoperatively, systemic and ocular complications were observed: two patients had trisomy 21, two had Lowe syndrome, two presented with developmental disorders, one was diagnosed with Cornelia de Lange syndrome, two eyes manifested nanophthalmos, and one eye exhibited persistent fetal vasculature.
Among the patients, 18 cases had unilateral cataract and 12 cases had bilateral cataract. The average age at the time of surgery for unilateral and bilateral patients were 2.7 ± 2.3 years and 2.3 ± 2.3 years, respectively, with no significant difference between them (p = 0.462). Previous studies indicated that the critical periods for surgical treatment to minimize the effects of visual deprivation in congenital cataract were 6 weeks for unilateral cases and 8 to12 weeks for bilateral cases [12,13,14,15]. In our cohort, 17% (3/18) of the patients with unilateral cataracts and 33% (4/12) of the patients with bilateral cataracts underwent surgery within this critical period for visual development.
The mean best-corrected visual acuity (BCVA) at the final visit was 0.453 ± 0.488 (logMAR) for all cases. There was a significant correlation between the final visual acuity and the patient’s age at the time of surgery (r = −0.307, p = 0.048). The unilateral cataract group showed a significantly poorer BCVA (0.658 ± 0.615) than the bilateral cataract group (0.298 ± 0.294) (p < 0.001). Their distributions are depicted in Fig. 2.
Over the course of the follow-up period, the eyes underwent an average myopic shift of −6.0 ± 6.3 diopters (D). There was a significant correlation between the patient’s age at the time of surgery and the magnitude of the myopic shift (r = 0.402, p = 0.008) (Fig. 3). The myopic shift tended to be larger in patients with unilateral cataracts (−8.2 ± 6.1 D) than in patients with bilateral cataracts (−4.9 ± 6.4 D), but the difference was not significantly different between groups (p = 0.213). Since the non-cataract eye in the unilateral group also showed a considerable myopic shift during the same period (−3.4 ± 2.4 D), the net myopic shift (the difference between the eyes in this group, −4.8 D) was similar to that observed in the bilateral cataract group.
There were some postoperative complications as summarized in Table 1. Three eyes (7.1%) developed suspected glaucoma (increased IOP), but glaucoma was not seen in any cases. There were no cases of retinal detachment, pupillary membrane, pupillary closure, persistent iritis, or other serious complications. IOL exchange surgery was conducted in two eyes (4.8%): one in the unilateral group due to pronounced myopic drift and one in the bilateral group due to significant IOL decentration. Three eyes (7.1%) in the bilateral group underwent a secondary surgical intervention for significant visual axis opacification.
Discussion
During our study's follow-up period of over 10 years, no cases developed glaucoma, although there were three cases (7.1%) that exhibited suspected glaucoma. Prior long-term studies indicated a frequent occurrence of glaucoma-related complications following infantile cataract removal [3, 7]. On the other hand, more recent reports utilizing modern surgical techniques revealed a reduced incidence of glaucoma in pseudophakic eyes, indicating that primary IOL implantation combined with anterior vitrectomy does not elevate the risk of secondary glaucoma [16,17,18,19]. In addition, other large-scale analyses underscored that primary IOL implantation serves as a protective factor against glaucoma development after congenital cataract surgery [20,21,22,23]. To rationalize how primary IOL implantation in pediatric patients with cataracts might reduce glaucoma incidence, two hypotheses have been proposed [20, 23]. Firstly, the chemical theory conjectures that harmful vitreous chemical components might damage the trabecular meshwork in an aphakic eye. The presence of the IOL in a pseudophakic eye might limit or lessen this exposure. The second hypothesis, termed the mechanical theory, proposes that the loss of support to the trabecular meshwork in aphakia may lead to its disorganization or even collapse. This would compromise its function both as a filter and an active metabolic tissue. Implanting a posterior chamber IOL at the time of cataract removal could potentially counteract this loss of support. The validity of these theories, however, remains a subject for future investigations.
After cataract extraction with primary IOL implantation in children, visual axis opacification is the most common complication requiring reoperation [16, 17, 19]. In a 5-year follow-up study after cataract surgery among children younger than 13 years, the cumulative incidence of significant visual axis opacification was reported as 33% for bilateral pseudophakia and 34% for unilateral pseudophakia [16]. For children who underwent cataract removal and IOL implantation before reaching 2 years of age, 10.3% experienced visual axis opacification requiring surgical intervention over a 5-year follow-up period [24]. Within 5 years following cataract surgery and primary IOL implantation in children aged 2 years or younger, visual axis opacity was observed in 39% of bilateral cases and 40% of unilateral cases [25]. In our study, 7.1% of eyes needed a secondary surgical procedure to clear visual axis opacification. While the previous studies and ours differ in terms of patient age and follow-up duration, our research indicated a lower incidence of visual axis opacification. This decreased incidence might be due to the thorough anterior vitrectomy performed during cataract surgery and the utilization of newer IOLs with advanced materials, designs, and surface finishes.
Progressive myopia is a common sequela after pediatric cataract surgery. The magnitude of this refractive shift can vary based on factors such as the patient’s age at surgery and the length of follow-up [1, 7, 26]. In our study, the average myopic shift observed was −6.0 ± 6.3 D, which was found to significantly correlate with the patient’s age at surgery. The myopic drift for bilateral cases was −4.9 D, and the net myopic shift (difference between the pseudophakic and the fellow eyes) in unilateral cases was −4.8 D. For pediatric patients operated on before reaching 13 years of age, the median 5-year change in spherical equivalent refractive error was reported to be −1.63 D for bilateral pseudophakic eyes and −1.94 D for unilateral pseudophakic eyes [16]. Another study noted that, among infants who underwent cataract extraction and primary IOL implantation before 1 year of age, the myopic shift at 10 years postoperatively ranged from −21.88 D to −3.75 D, averaging −11.62 ± 5.14 D [26]. A younger age at surgery was associated with a greater magnitude of myopic shift [26]. In another cohort, patients who underwent pediatric cataract surgery at an average age of 2.4 months (ranging from 1.0 to 6.8 months) demonstrated a mean refractive shift of −8.97 D at age 5 years for those operated at 1 month and −7.22 D for those treated at 6 months [27]. Predicting the long-term refractive outcomes after pediatric cataract surgery remains challenging. Based on available evidence, researchers advocate for an under-correction when implanting an IOL in young children, anticipating a likely myopic progression in the future [8, 28].
In pediatric eyes, small-incision cataract surgery would be preferred to minimize the degree of surgical invasion to the eye. To this end, we used hydrophobic acrylic single-piece IOLs in all cases. This approach is in line with previous studies that indicate the advantages of hydrophobic acrylic IOLs over polymethyl methacrylate IOLs in pediatric populations [29,30,31,32,33]. In terms of overall IOL size and optic diameter, smaller dimensions might be more suitable for particularly immature pediatric eyes. However, there are limited options available in practice. Determining the appropriate IOL power in pediatric cataract surgery is challenging due to increasing axial length and changing corneal refraction postoperatively. Therefore, under-correction and hyperopic outcomes at the time of cataract surgery are usually recommend to prevent excessive myopic shifts in the long run [33]. In our study, we considered an anticipated a postoperative myopic shift and followed empirical guidelines to set the target refraction [8], ensuring the IOL power did not exceed 30 D.
This study has several limitations. First, the absence of a control group (aphakia group) is notable because, in adherence to our treatment policy, we implanted an IOL in every case. If congenital cataract was diagnosed at a very early age, we opted to wait until the limit of “critical period for visual development” [12,13,14,15], and then proceeded with cataract surgery and IOL implantation into the capsular bag. Second, determination of the exact age of onset for childhood cataract is challenging; thus, both congenital and developmental cataracts were included in our cohort. Third, our analysis was restricted to patients who completed a 10-year postoperative follow-up. We lack data on individuals who were lost to follow-up during the study period. It may be that those with a less favorable prognosis might have discontinued their regular check-ups.
Conclusions
We retrospectively analyzed long-term outcomes of pediatric cataract surgery. Younger patients at the time of surgery tended to have poorer BCVA at their final visit. The unilateral group's BCVA was inferior to that of the bilateral group. A substantial myopic shift was observed overall, yet its magnitude in the bilateral group paralleled the net shift seen in the unilateral group (comparing pseudophakic and fellow eyes). While three eyes (7.1%) showed suspected glaucoma (increased intraocular pressure), there were no confirmed cases of glaucoma or any other significant complications. Only a handful of eyes required secondary surgical interventions, such as IOL exchange or procedures to clear visual axis opacification. The advancements in modern surgical technologies and techniques could further enhance the long-term surgical outcomes for pediatric patients with cataracts.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Lenhart PD, Lambert SR. Current management of infantile cataracts. Surv Ophthalmol. 2022;67:1476–505.
Plager DA, Bothun ED, Freedman SF, Wilson ME, Lambert SR. Complications at 10 years of follow-up in the Infant Aphakia Treatment Study. Ophthalmology. 2020;127:1581–3.
Murphy M, Murtagh P, McAnena L, Eldouri A, Kirwan C, O’Keefe M. Secondary glaucoma and visual axis opacification in aphakic and pseudophakic patients following congenital cataract surgery: a 28-year longitudinal case series. Eur J Ophthalmol. 2020;30:1370–80.
McClatchey SK, McClatchey TS, Cotsonis G, Nizam A, Lambert SR, Infant Aphakia Treatment Study Group. Refractive growth variability in the Infant Aphakia Treatment Study. J Cataract Refract Surg. 2021;47:512–5.
Lambert SR, Nizam A, DuBois L, Cotsonis G, Weakley DR Jr, Wilson ME, Infant Aphakia Treatment Study Group. The myopic shift in aphakic eyes in the Infant Aphakia Treatment Study after 10 years of follow-up. Eye Contact Lens. 2021;47:108–12.
Freedman SF, Beck AD, Nizam A, Vanderveen DK, Plager DA, Morrison DG, Drews-Botsch CD, Lambert SR, Infant Aphakia Treatment Study Group. Glaucoma-related adverse events at 10 years in the infant aphakia treatment study: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol. 2021;139:165–73.
Weakley DR Jr, Nizam A, VanderVeen DK, Wilson ME, Kruger S, Lambert SR, Infant Aphakia Treatment Study Group. Myopic shift at 10-year follow-up in the Infant Aphakia Treatment Study. Ophthalmology. 2022;129:1064–5.
Awner S, Buckley EG, DeVaro JM, Seaber JH. Unilateral pseudophakia in children under 4 years. J Pediatr Ophthalmol Strabismus. 1996;33:230–6.
Solebo AL, Russell-Eggitt I, Cumberland PM, Rahi JS, British Isles Congenital Cataract Interest Group. Risks and outcomes associated with primary intraocular lens implantation in children under 2 years of age: the IoLunder2 cohort study. Br J Ophthalmol. 2015;99:1471–6.
Thau A, Lloyd M, Freedman S, Beck A, Grajewski A, Levin AV. New classification system for pediatric glaucoma: implications for clinical care and a research registry. Curr Opin Ophthalmol. 2018;29:385–94.
Freedman SF, Kraker RT, Repka MX, Wallace DK, de Alba Campomanes A, Yanovitch TL, Orge FH, Gearinger MD, Pediatric Eye Disease Investigator Group (PEDIG). Incidence and management of glaucoma or glaucoma suspect in the first year after pediatric lensectomy. JAMA Ophthalmol. 2020;138:71–5.
Birch EE, Stager DR. The critical period for surgical treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci. 1996;37:1532–8.
Gelbart SS, Hoyt CS, Jastrebski G, Marg E. Long-term visual results in bilateral congenital cataracts. Am J Ophthalmol. 1982;93:615–21.
Lambert SR, Lynn MJ, Reeves R, Plager DA, Buckley EG, Wilson ME. Is there a latent period for the surgical treatment of children with dense bilateral congenital cataracts? J AAPOS. 2006;10:30–6.
Birch EE, Cheng C, Stager DR Jr, Weakley DR Jr, Stager DR Sr. The critical period for surgical treatment of dense congenital bilateral cataracts. J AAPOS. 2009;13:67–71.
Repka MX, Dean TW, Kraker RT, Li Z, Yen KG, de Alba Campomanes AG, Young MP, Rahmani B, Haider KM, Whitehead GF, Lambert SR, Kurup SP, Kraus CL, Cotter SA, Holmes JM, Pediatric Eye Disease Investigator Group. Visual acuity and ophthalmic outcomes 5 years after cataract surgery among children younger than 13 years. JAMA Ophthalmol. 2022;140:269–76.
Yen KG, Repka MX, Sutherland DR, Haider KM, Hatt SR, Kraker RT, Galvin JA, Li Z, Cotter SA, Holmes JM, Pediatric Eye Disease Investigator Group. Complications occurring through 5 years following primary intraocular lens implantation for pediatric cataract. JAMA Ophthalmol. 2023;141(8):705–14.
Bothun ED, Repka MX, Kraker RT, Wu R, Leske DA, Hatt SR, Li Z, Freedman SF, Astle WF, Cotter SA, Holmes JM, Pediatric Eye Disease Investigator Group. Incidence of glaucoma-related adverse events in the first 5 years after pediatric lensectomy. JAMA Ophthalmol. 2023;141:324–31.
Liu Y. Some lessons regarding intraocular implantation following pediatric cataract surgery. JAMA Ophthalmol. 2023. https://doi.org/10.1001/jamaophthalmol.2023.2672.
Asrani S, Freedman S, Hasselblad V, Buckley EG, Egbert J, Dahan E, Gimbel H, Johnson D, McClatchey S, Parks M, Plager D, Maselli E. Does primary intraocular lens implantation prevent “aphakic” glaucoma in children? J AAPOS. 2000;4:33–9.
Yagev R, Khatib N, Barrett C, Lior Y, Lifshitz T, Tsumi E. Intraocular lens implantation as an isolated risk factor for secondary glaucoma in pediatric patients. Can J Ophthalmol. 2019;54:621–5.
Balekudaru S, Agarkar S, Guha S, Mayee RC, Viswanathan N, Pandey A, Singh M, Lingam V, George R. Prospective analysis of the predictors of glaucoma following surgery for congenital and infantile cataract. Eye (Lond). 2019;33:796–803.
Wang J, Wu X, Wang Q, Zhou F, Chen H, Chen W, Lin D, Zhang X, Wang R, Chen J, Liu Z, Lin Z, Li X, Li J, Han Y, Liu Y, Lin H, Chen W. Incidence of and risk factors for suspected and definitive glaucoma after bilateral congenital cataract surgery: a 5-year follow-up. Br J Ophthalmol. 2023. https://doi.org/10.1136/bjo-2022-322589.
Vasavada AR, Vasavada V, Shah SK, Praveen MR, Vasavada VA, Trivedi RH, Rawat F, Koul A. Five-year postoperative outcomes of bilateral aphakia and pseudophakia in children up to 2 years of age: a randomized clinical trial. Am J Ophthalmol. 2018;193:33–44.
Solebo AL, Cumberland P, Rahi JS, British Isles Congenital Cataract Interest Group. 5-year outcomes after primary intraocular lens implantation in children aged 2 years or younger with congenital or infantile cataract: findings from the IoLunder2 prospective inception cohort study. Lancet Child Adolesc Health. 2018;2:863–71.
Chan JJT, Wong ES, Lam CPS, Yam JC. Ten-year refractive and visual outcomes of intraocular lens implantation in infants with congenital cataract. Hong Kong Med J. 2023;29:22–30.
Weakley DR Jr, Lynn MJ, Dubois L, Cotsonis G, Wilson ME, Buckley EG, Plager DA, Lambert SR, Infant Aphakia Treatment Study Group. Myopic shift 5 years after intraocular lens implantation in the Infant Aphakia Treatment Study. Ophthalmology. 2017;124:822–7.
Lambert SR. Changes in ocular growth after pediatric cataract surgery. Dev Ophthalmol. 2016;57:29–39.
Wilson ME, Elliott L, Johnson B, et al. AcrySof acrylic intraocular lens implantation in children: clinical indications of biocompatibility. J Am Assoc Pediatr Ophthalmol Strabismus. 2001;5:377–80.
Küchle M, Lausen B, Gusek-Schneider GC. Results and complications of hydrophobic acrylic vs PMMA posterior chamber lenses in children under 17 years of age. Graefes Arch Clin Exp Ophthalmol. 2003;241:637–41.
Vasavada AR, Nath VC, Trivedi RH. Anterior vitreous face behavior with AcrySof in pediatric cataract surgery. J Am Assoc Pediatr Ophthalmol Strabismus. 2003;7:384–8.
Rowe N, Biswas S, Lloyd I. Primary IOL implantation in children: a risk analysis of foldable acrylic v PMMA lenses. Br J Ophthalmol. 2004;88:481–5.
Mohammadpour M, Shaabani A, Sahraian A, Momenaei B, Tayebi F, Bayat R, Mirshahi R. Updates on managements of pediatric cataract. J Curr Ophthalmol. 2018;31:118–26.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Dr. Tetsuro Oshika conceived and designed the study. Drs. Tetsuro Oshika and Gaku Kiuchi collected the data. Dr. Tetsuro Oshika analyzed the data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Tetsuro Oshika received compensation as a consultant from Alcon, Johnson & Johnson Vision, Santen Pharmaceutical, HOYA, Topcon, and Logic and Design. He receives research support from Santen Pharmaceutical, Tomey, Alcon, Senju Pharmaceutical, Johnson & Johnson Vision, HOYA, KOWA Pharmaceutical, Otsuka Pharmaceutical, Novartis, Topcon, Tomey, and Chugai Pharmaceutical. Dr. Gaku Kikuchi does not have any conflict of interest.
Ethical Approval
The study was conducted in adherence to the tenets of the Declaration of Helsinki, and the institutional review board of Tsukuba University Hospital approved the study protocol (R04-162, December 2022). The institutional review board of Tsukuba University Hospital committee waived the need for patient informed consent for the use of their medical record data, in line with the regulations of the Japanese Guidelines for Epidemiologic Study issued by the Japanese Government. Due to the observational nature of the study, clinical trial registration was not mandated.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Oshika, T., Kiuchi, G. 10-Year Outcomes of Pediatric Cataract Surgery with Foldable Intraocular Lens Implantation and Posterior Continuous Curvilinear Capsulorhexis. Ophthalmol Ther 12, 3337–3345 (2023). https://doi.org/10.1007/s40123-023-00826-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00826-6