Abstract
Introduction
Refractive lens exchange (RLE) patients represent a unique population with a different baseline and set of expectations compared to their cataract counterparts. Visual outcomes and patient satisfaction following RLE with bilateral implantation of a trifocal intraocular lens (IOL) were assessed in a cohort of patients with presbyopia and without cataract.
Methods
Charts of patients with presbyopia who underwent femtosecond laser-assisted RLE with bilateral implantation of the PanOptix trifocal IOL (toric and non-toric) at a single-surgeon, private practice center from September 2019 to August 2020 were retrospectively reviewed. Eyes with prior keratorefractive surgery, amblyopia, or underlying pathology were excluded. Primary endpoints included corrected and uncorrected visual acuity at distance (CDVA and UDVA), intermediate (DCIVA and UIVA), and near (DCNVA and UNVA) at 6 months. Secondary endpoints included residual refractive error, patient-reported satisfaction, spectacle independence, and visual disturbance profile as assessed by a validated questionnaire at 6 months.
Results
Seventy-eight eyes of 39 patients (mean age 56 ± 6 years; 79% female) were included. Most eyes were hyperopic (mean SE 2.35 ± 1.81). Postoperatively, 100% and 92% of eyes were within ± 1.00 D and ± 0.50 D of emmetropia, respectively. One hundred percent, 97%, and 97% of patients achieved UDVA, UNVA, and UIVA of logMAR 0.1 or better. Starbursts were the most frequent (67%) and bothersome (41%) visual disturbance cited, but nearly half (41%) of patients rated them as absent or “not bothersome at all.” Overall, 77% of patients reported achieving complete spectacle independence with 87% and 90% of patients stating they were satisfied with their vision and would recommend the same procedure to others, respectively.
Conclusions
RLE with bilateral implantation of the PanOptix IOL is a safe and effective procedure with good patient satisfaction. Because of their relatively clear native lenses and visually demanding needs compared to their cataract counterparts, surgeons should take extra precautions to counsel RLE patients on the limitations of trifocal technology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Why carry out this study? |
The AcrySof IQ PanOptix (Alcon Fort Worth, TX, USA) is the first and only trifocal IOL approved by the US Food and Drug Administration, and allows for increased spectacle independence at distance, intermediate, and near. |
Research has shown safe and effective outcomes for PanOptix implantation in mostly cataract and mixed cataract + RLE cohorts, but studies evaluating non-cataractous, RLE-only populations are limited. |
RLE patients represent a unique subset with a different baseline and often higher set of expectations compared to their cataract counterparts and warrant further study. |
What was learned from this study? |
Bilateral RLE with the PanOptix trifocal IOL results in good unaided vision at distance, intermediate, and near with good patient satisfaction and an acceptable visual disturbance profile. |
Because of their visually demanding needs and relatively clear native lenses compared to their cataract counterparts, surgeons should take extra precautions to counsel RLE patients on the limitations of trifocal technology, including the likelihood of photic phenomena and possible need for spectacles postoperatively. |
Introduction
Presbyopia is the natural and irreversible loss of the eye’s accommodation due to aging and is the most common cause of decreased near vision in adults older than age 40 [1]. Presbyopia has been found to have a negative impact on quality of life in adults because of the limitations it poses on near vision activities [1]. As the global population’s life expectancy continues to rise, the proportion of individuals older than 40 and presbyopic will continue to grow and is predicted to be 1.8 billion by 2050 [1].
Current treatments for presbyopia are divided between optical correction, with spectacles or contact lenses, and refractive surgery. The keratorefractive surgical techniques to correct presbyopia including monovision laser in situ keratomileusis (LASIK) and corneal inlays [3,4,5] treat the symptoms but not the underlying cause of presbyopia, specifically the crystalline lens dysfunction. More recently, refractive lens exchange (RLE) which consists of replacing a non-cataractous lens with a presbyopia-correcting intraocular lens (IOL) has gained increasing popularity [2,3,4]. However, multifocal IOLs with only two focal points at distance and near do not provide optimal intermediate vision [5]. Moreover, the increased range of vision is not without adverse effects, such as increased photic phenomena or reduced contrast sensitivity [6,7,8].
To improve intermediate vision without impairing distance and near visual acuity, trifocal IOLs were designed to provide three useful focal distances: near, intermediate, and far [9,10,11]. The AcrySof IQ PanOptix (Alcon Fort Worth, TX, USA) is the first and only trifocal IOL to be approved by the US Food and Drug Administration (FDA), and allows for increased spectacle independence at distance, intermediate (60 cm), and near (40 cm). At a pupil diameter of 3.0 mm, approximately 40% of the light energy is directed to distance, with approximately 25% at near and 22% at intermediate. When the pupil dilates to 6.0 mm, the light energy at distance is increased to 70% with 10% each at near and intermediate [12]. Studies have shown safe and effective outcomes for PanOptix implantation amongst cataract and mixed cataract + RLE study populations, but similar studies evaluating outcomes in non-cataractous, RLE-only cohorts are limited. Because of their visually demanding needs and relatively clear native lenses, RLE patients may experience notable differences in their satisfaction, spectacle independence, and photic phenomena levels compared to their cataract counterparts. To our knowledge, this is the first significant case series describing the outcomes of RLE with bilateral PanOptix IOL implantation specifically in patients without cataract in the USA, where it is considered an “off-label” procedure.
Methods
This was a retrospective, non-interventional case series (i.e., chart review) performed at a single-surgeon, private practice center. The charts of all patients who underwent femtosecond laser-assisted RLE with bilateral implantation of the Acrysof IQ PanOptix trifocal IOL (Alcon Fort Worth, TX, USA) between September 1, 2019 and August 31, 2020 were reviewed. Inclusion criteria were patients with presbyopia, as defined by distance corrected near vision (DCNVA) of 0.3 logMAR (20/40) or worse, with healthy eyes and clinically insignificant intraocular lens and media opacity with best-corrected visual acuity of 0.0 logMAR (20/20) or better. Eyes with prior keratorefractive surgery, amblyopia, or any underlying ocular pathology including significant ocular surface disease and abnormal corneal higher order aberrations were excluded.
The study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the ethical committee of the Salus Institutional Review Board.
All patients provided written informed consent after explanation of the “off label” nature and possible consequences of the procedure. Patients then underwent a comprehensive preoperative ophthalmic examination including an anterior segment slit lamp exam with fluorescein corneal staining and assessment of the tear breakup time (TBUT) as well as a posterior dilated fundus exam. Additional testing included preoperative uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), uncorrected near visual acuity (UNVA), and DCNVA as well as manifest refraction, optical biometry (Carl Zeiss IOL Master 500, Germany), corneal tomography (Oculus Pentacam Oculus Optikgerate GmbH, Wetzlar, Germany), endothelial cell count (Konan SP-9000, Hyogo, Japan), and optical coherence tomography of the macula and optic nerve (Optovue). IOL calculations were performed with the Barrett II Universal formula (Holladay IOL consultant, Houston, TX, USA and www.apacrs.org/barrett_universal2). The A constant of 119.1 was used. Targeted postoperative refraction was plano for both eyes. All patients received extensive counseling on the risks, benefits, and alternatives of undergoing RLE with a trifocal IOL.
Femtosecond laser-assisted RLE surgery was performed using the LensAR (LensAR Inc, Winter Park, FL, USA) to complete a 5.0-mm capsulotomy, lens fragmentation, arcuate incisions for mild corneal astigmatism correction (a toric IOL was used for greater than 0.75 D against-the-rule and 1.00 D with-the-rule astigmatism), and a 2.75-mm clear corneal incision. All cases were performed under topical anesthesia and oral sedation with MKO melt (midazolam, ketamine, ondansetron compound) (Melt Pharmaceuticals, TN, USA). Phacoemulsification was completed with the Centurion (Alcon Laboratories, Fort Worth, TX, USA). Postoperatively, all patients received a combined antibiotic, NSAID, and steroid drop four times a day on a tapering schedule for 4 weeks. Patients returned for follow-up at 1 day, 1 week, 4 weeks, 3 months, and 6 months or more visits as needed.
At the 6-months follow-up visit, the monocular UDVA, binocular uncorrected intermediate visual acuity (UIVA) at 66 cm, and binocular UNVA at 40 cm were collected along with the monocular CDVA and binocular DCIVA and DCNVA. A careful manifest refraction and assessment of spherical equivalent were completed. Validated patient questionnaires assessing visual disturbances within the past 7 days (QUVID) along with spectacle independence, quality of vison under dim and bright lighting, and patient satisfaction (IOLSAT) were administered to emmetropic (− 0.25 ≤ SE ≤ 0.75 and cyl ≤ 0.75) patients at the 6-months visit [12]. Patients with significant residual refractive error or posterior capsular opacity at any time during the follow-up period were treated with keratorefractive surgery and YAG laser capsulotomy, respectively, prior to questionnaire administration.
Statistical analyses were performed using MATLAB (Natick, Massachusetts: The MathWorks Inc.). Visual acuity was converted to logarithm of the minimum angle of resolution (logMAR) and compared using a two-tailed Student t test, with significance corresponding to p < 0.05.
Results
A total of 78 eyes of 39 patients were included in the analysis. The mean age was 56 ± 6 years, and 79% (30) of patients were female. Most patients were hyperopic with mean preoperative spherical equivalent + 2.35 ± 1.81 diopters (D) and sphere ranging from − 5.00 to 8.00 D; only six patients (15%) were myopic preoperatively. Mean preoperative cylinder was 0.75 ± 1.79 D with refractive astigmatism ranging from 0.00 to 5.50 D. Patient demographics and preoperative monocular UDVA and binocular UNVA are demonstrated in Table 1. UIVA data was unavailable from the chart review. Mean follow-up time was 8.9 months (range 5.8–16.0 months).
Best-Corrected Visual Acuity
The postoperative CDVA, DCIVA, and DCNVA at 6 months are summarized in Fig. 1a.
The mean postoperative monocular CDVA was 0.00 logMAR (20/20). Ninety-nine percent (38) and 100% (39) of patients achieved monocular CDVA of 0.00 logMAR (20/20) and 0.10 logMAR (20/25) or better, respectively. Binocularly, the mean CDVA improved to − 0.01 logMAR (approximately 20/20), with 100% (39) of patients achieving binocular CDVA 0.00 logMAR (20/20) or better.
At near, the mean postoperative binocular DCNVA was 0.02 logMAR (approximately 20/20), with 90% (35), 97% (37), and 100% (39) of patients achieving binocular DCNVA of 0.00 logMAR (20/20), 0.10 logMAR (20/25), and 0.20 logMAR (20/30) or better, respectively.
At intermediate, the mean postoperative binocular DCIVA was 0.03 logMAR (approximately 20/20), with 69% (27), 97% (37), and 100% (39) of patients achieving binocular DCIVA of 0.00 logMAR (20/20), 0.10 logMAR (20/25), and 0.20 logMAR (20/30) or better, respectively.
Uncorrected Visual Acuity
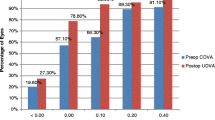
Table 2 and Fig. 1b summarize the improvement in UDVA and UNVA at 6 months after surgery.
The mean postoperative monocular UDVA was 0.02 logMAR (approximately 20/20), with 81% (32), 97% (37), and 99% (38) of patients achieving monocular UDVA of 0.00 logMAR (20/20), 0.10 logMAR (20/25), and 0.20 logMAR (20/30) or better, respectively.
Binocularly, this improved to 97% (37) and 100% (39) of patients achieving UDVA of 0.00 logMAR (20/20) and 0.10 logMAR (20/25) or better, respectively.
The mean postoperative binocular UNVA was 0.04 logMAR (approximately 20/20), with 87% (34), 97% (37), and 97% (37) of patients achieving binocular UNVA of 0.00 logMAR (20/20), 0.10 logMAR (20/25), and 0.20 logMAR (20/30) or better, respectively.
The mean postoperative binocular UIVA was 0.04 logMAR (approximately 20/20), with 64% (25), 97% (37), and 97% (37) of patients achieving binocular UIVA of 0.00 logMAR (20/20), 0.10 logMAR (20/25), and 0.20 logMAR (20/30) or better, respectively.
Refractive Outcomes
Table 2 shows a statistically significant improvement in reduction of sphere, cylinder, and spherical equivalent at 6 months post-RLE surgery. The mean postoperative spherical equivalent was 0.23 ± 0.19 D. Overall, 100% (78) and 92% (72) of eyes were within ± 1.00 D and ± 0.50 D of emmetropia, respectively. Three (4%) eyes underwent LASIK enhancements before their final exams for small residual refractive errors.
Patient-Reported Outcomes
Visual Disturbances (QUVID Questionnaire)
The frequency of patient-reported visual disturbances within the past 7 days of survey administration at their 6-month postoperative visit is summarized in Fig. 2a. The most commonly reported visual disturbances were starbursts (67%, N = 26) followed by glare (62%, N = 24), haloes (51%, N = 20), blurred vision (36%, N = 14), hazy vision (23%, N = 9), and a “dark area” (i.e., negative dysphotopsia; 13%, N = 5). There were no complaints about double vision. For positive dysphotopsias, the greatest reported frequency for haloes and glare was “never” (49%, N = 19 and 38%, N = 15, respectively), while the most commonly reported frequency for starbursts was “always” (41%, N = 16) followed by “never” (33%, N = 13). Still, over one-third of patients reported “never” experiencing any positive dysphotopsias at all.
The severity of patient-reported visual disturbances is summarized in Fig. 2b. Of those patients who experienced starbursts, haloes, and glare, the majority rated those symptoms to be moderate and severe. More patients rated starbursts (59%, N = 23) as “moderate” or “severe” compared to haloes (44%, N = 17) and glare (41%, N = 16) (p < 0.05). However, when patients were asked to rate the “bothersomeness” of their dysphotopsias, the greatest proportion of patients reported “none” or “not bothered at all” for starbursts (41%, N = 16), haloes (51%, N = 20), and glare (44%, N = 17) (Fig. 2c). Starbursts were cited as most bothersome with 41% (16) of patients reporting that they were “bothered quite a bit” or “very much” compared to haloes (28%, N = 11) and glare (29%, N = 11) (p < 0.05).
Spectacle Independence (IOLSAT Questionnaire)
At the 6 months postoperative visit, most patients (77%, N = 30) reported “never” needing glasses to see at any distance in the past 7 days. Only 15% (6) of patients stated that they needed glasses to see “sometimes” and 3% (1) “rarely” (Fig. 3a). Overall, 82% (32), 90% (35), and 87% (34) of patients reported never needing glasses to see at distance, intermediate, and near, respectively, in general lighting (Fig. 3b). To gauge their preoperative expectation levels for spectacle independence, patients were asked how often they were expecting to need glasses after surgery; 77% reported “never.”
Quality of Vision (IOLSAT Questionnaire)
In bright lighting, most patients described their vision as “good” or “very good” at distance (66%, N = 25), intermediate (77%, N = 30), and near (70%, N = 27). Fewer patients reported “very good” quality of vision in dim lighting, but most patients still described their vision as “good” or “very good” at distance (67%, N = 26), intermediate (82%, N = 32), and near (72%, N = 28) (Supplementary Material).
Patient Satisfaction (IOLSAT Questionnaire)
Overall, 87% (34) of patients reported being “satisfied” or “very satisfied” with their vision following RLE. Thirteen percent (5) of patients reported being “neither satisfied nor dissatisfied,” and no patients reported being “dissatisfied” or “very dissatisfied” (Fig. 4a). The most common reasons cited for unhappiness included nighttime visual disturbances, inability to see fine print up-close, and symptoms related to ocular surface disease. When asked if they would have the same lens implanted again, 85% (33) of patients responded affirmatively with 90% (35) of patients willing to recommend the same surgery to friends or family (Fig. 4b).
Adverse Events
No intraoperative complications were seen. One eye lost 1 line of CDVA at their final visit due to presumed tear film disturbance. All eyes gained statistically significant lines of UCVA, UIVA, and UNVA (p < 0.01). A total of 18 eyes (23%) developed significant posterior capsular opacities during the follow-up period and were successfully treated with a Nd:YAG laser capsulotomy procedure. Three (4%) eyes underwent uncomplicated LASIK enhancements for small residual refractive errors. No IOL exchanges were required.
Discussion
RLE with implantation of presbyopia-correcting IOLs is being increasingly performed in patients seeking greater spectacle independence. In addition to objective visual and refractive outcomes following RLE, this study also assessed patient-reported outcomes including spectacle independence, visual disturbances, and patient satisfaction using detailed validated questionnaires from the original PanOptix FDA studies. To our knowledge, this is the first study in the USA to evaluate outcomes of PanOptix IOL implantation in RLE-only patients (no patients with cataract included). This is an important distinction because compared to patients with cataract, RLE patients are likely to have higher expectations and greater sensitivity to postoperative visual disturbances, which warrants further characterization in this unique population. Only one other study has analyzed the visual outcomes of bilateral PanOptix implantation in RLE patients alone, but spectacle independence and visual disturbances were not addressed in detail [19]. Overall in our study, we found RLE with PanOptix implantation to be a safe and effective procedure in our patients mostly with hyperopia, presbyopia, and without cataract, similar to prior studies evaluating PanOptix IOL outcomes in cataract and mixed cataract + RLE study cohorts (Table 3) [13, 15,16,17,18,19,20,21,22,23,24]. However, a few key differences based on a literature review will be highlighted below.
Refractive and Visual Outcomes
Refractive predictability was excellent in our study as 92% of patients fell within ± 0.50 D of emmetropia. The PanOptix trifocal IOL delivered great vision at all three focal points as 100%, 97%, and 97% of patients achieved UDVA, UIVA, and UNVA of 0.1 logMAR (20/25) or better. Femtosecond laser arcuate incisions were used to treat low levels of astigmatism in this study, which has been shown to yield more precise refractive outcomes especially with presbyopia-correcting IOLs [25]. With correction, all patients achieved CDVA, DCIVA, and DCNVA of 0.20 logMAR (20/30) or better with mean 0.01 logMAR, 0.03 logMAR, and 0.02 logMAR, respectively. These results are comparable to what prior bilateral PanOptix studies have reported with binocular CDVA ranging from − 0.1 to 0.03 logMAR, DCIVA from − 0.11 to 0.12 logMAR, and DCNVA from − 0.07 to 0.08 logMAR [13, 14].
Spectacle Independence
The rate of complete spectacle independence reported in the literature for combined cataract and RLE PanOptix studies range from 75% to 100%, with a recent large meta-analysis reporting a complete spectacle independence rate of 90% in patients with cataract [13, 26, 27]. Our study’s rate of complete spectacle independence was 77% and falls in the lower end of this range. This is likely because our study focused solely on RLE patients, who tend to be younger (mean age 56 years old in this study) and are likely to have more visually demanding needs across all distances for their day-to-day work especially at near (e.g., jeweler, electrician, etc.) compared to relatively older patients with cataract, many of whom are retired. A high level of spectacle independence is the main driving factor for why RLE patients seek surgery in the first place, unlike patients with cataract whose primary motivation is usually to seek improved visual quality from cataract removal with spectacle independence as a secondary gain. This selection bias inherent to RLE patients can make it more difficult for the surgeon to meet those patients’ expectations in regards to spectacle independence compared to their cataract counterparts. Still, 100%, 97%, and 97% of the patients in our study demonstrated uncorrected Snellen visual acuity of 20/25 or better at distance, intermediate, and near, respectively, suggesting good overall unaided vision across all distances.
Another reason for the disconnect between the excellent uncorrected visual acuities and the lower-than-expected degree of spectacle independence reported by patients in our study may be secondary to the decreased contrast sensitivity inherent to the PanOptix trifocal and all diffractive multifocal IOLs, which can significantly impact visual function under dim lighting conditions commonly encountered in the “real world.” Thus, while our study demonstrated excellent uncorrected visual acuity at all working distances in a controlled, high-contrast clinical setting, it is not representative of our RLE patients’ true quality of vision and level of function in real-life settings. This decreased contrast sensitivity is partly reflected by the small proportion of patients in our study who reported experiencing “hazy vision.” Indeed, the patients in our study reported better quality of vision under bright lighting compared to dim lighting, but the majority of patients still reported good or very good quality of vision across all distances, with the highest level of spectacle independence (90%) achieved at the intermediate range similar to previous studies [27].
Visual Disturbances
Photic phenomena are common with diffractive IOLs and can significantly impact patients’ visual quality, function, and satisfaction. We used the same validated questionnaires from the original PanOptix FDA studies [12] to perform a detailed assessment of the visual disturbance profile of RLE patients in our study. More than half of our patients reported experiencing some frequency of starbursts, haloes, and/or glare. In contrast, several PanOptix studies previously reported lower rates of dysphotopsias. For example, Nicula et al. cited a positive dysphotopsia rate of only 18.8% in their RLE patients, but their self-developed survey was limited and queried only about postoperative “halos and glittering” [19]. Another PanOptix study described only 1 out of 55 patients who reported “disturbing haloes,” but again their questionnaire was non-standardized, and their population included both RLE patients and patients with cataract [28]. In general, it is difficult to compare the frequency of reported visual disturbances amongst different PanOptix studies in the literature because of the variety of non-standardized questionnaires used. It is also possible that RLE patients may be more sensitive to postoperative dysphotopsias because of their relatively normal baseline visual function compared to patients with cataract, which may skew RLE-only studies towards a higher incidence of photic phenomena compared to prior studies that included patients with cataract in their analyses.
Overall, studies have mostly reported on a wide range of halos frequency (15–95%) after PanOptix IOL implantation with limited or absent information on other types of positive dysphotopias including glare and starbursts [14, 18, 21, 29]. Interestingly, starbursts were the most common and bothersome visual disturbance type reported by more than half of the patients in our study. Still, the greatest proportion of patients in our study rated each visual disturbance as absent or “not bothersome at all,” and overall patient satisfaction remained high. Because of the wide variation of visual disturbance outcomes seen amongst patients and inability to predict which patients will be most affected, it is important to counsel all patients on the possibility of photic phenomena after implantation of a presbyopia-correcting IOL, especially in RLE patients who may be more susceptible.
Other Trifocal IOLs and Patient Satisfaction
Trifocal IOLs have been available in the global market since 2010. The AT Lisa and FineVision IOL are not available in the USA but have similarly been implanted with good refractive outcomes and patient satisfaction in non-presbyopes and presbyopic hyperopes and emmetropes abroad [30, 31]. These studies further highlight the utility of trifocal IOLs in addressing the needs of patients without cataract. A major difference between the AT Lisa and FineVision trifocal IOLs and the PanOptix is that the intermediate focus distance is farther at 80 cm in the former two compared to 60 cm with the PanOptix [12]. The few existing studies that have directly compared the PanOptix with other trifocal IOLs have found favorable visual and refractive outcomes in all [1]. Spectacle independence has also been shown to be higher with the PanOptix trifocal than with bifocal or extended depth of focus (EDOF) IOLs [32,33,34]. Synergy, a newer mixed EDOF and multifocal IOL, has been shown to deliver a high level of spectacle independence at near, intermediate, and distance. There is even some evidence showing that the Synergy may deliver better near visual acuity and mesopic contrast sensitivity compared to the PanOptix, which may improve patient satisfaction amongst myopes and patients who desire stronger near vision [35]. Few myopes were included in this study, but one patients with baseline myopia did report lower satisfaction due to the inability to see fine print up close postoperatively, while all other myopes reported good or very good satisfaction with the PanOptix IOL. The visual disturbance profile inherent to all trifocal and multifocal IOLs remains a limitation for widespread use of any one IOL for RLE, and further head-to-head studies are needed.
Overall, the RLE patients in this study reported a good level of patient satisfaction (87%) with bilateral PanOptix implantation. Prior PanOptix studies have reported satisfaction rates as high as 97% [22], but again, these cohorts included patients with cataract in their analyses, who are typically easier to please. RLE patients, on the other hand, tend to have higher expectations in regards to their vision and spectacle independence. Indeed, the vast majority (77%) of patients in our study reported expecting to “never” have to use glasses for any distance postoperatively despite thorough preoperative counseling that occasional reading glasses would likely be needed for every patient. In addition to the periodic need for glasses to see fine print up-close, the most common reasons cited for lower satisfaction in this study were due to positive dysphotopsias and symptoms related to ocular surface disease. This highlights the critical importance of screening out frequent nighttime (or early morning) drivers, counseling on the high likelihood of visual disturbances, and optimizing the ocular surface before and after RLE surgery.
Limitations
Limitations of this study include the relatively small sample size, retrospective nature, and that all surgeries were performed by a single surgeon, thus potentially limiting the applicability of these results to a different population. There was no head-to-head comparison of RLE patients versus patients with cataract, which could have provided additional valuable information. Moreover, no formal testing of contrast sensitivity was performed, but subjective visual quality under dim and bright lighting conditions was assessed. Strengths of this study include the use of validated questionnaires with detailed assessment of visual disturbance profiles and quality of vision under different lighting conditions, minimum 6-month duration of follow-up, and the specific inclusion of RLE patients alone.
Conclusion
This study provides valuable insights into a unique population of patients with a different baseline and potentially higher set of expectations from those undergoing cataract extraction. While several studies have demonstrated excellent outcomes for PanOptix IOL implantation in mainly cataract or mixed cataract + RLE cohorts, this study highlights its utility specifically as a refractive procedure for RLE patients. Our results show the PanOptix IOL to be a safe and effective option for RLE patients seeking spectacle independence with good patient satisfaction and an acceptable visual disturbance profile. Compared to their cataract counterparts, surgeons should take greater precautions to set realistic expectations with RLE patients and counsel them on the limitations of trifocal technology, including the possibility of photic phenomena and potential need for spectacles postoperatively.
References
Goertz AD, Stewart WC, Burns WR, Stewart JA, Nelson LA. Review of the impact of presbyopia on quality of life in the developing and developed world. Acta Ophthalmol. 2014;92(6):497–500. https://doi.org/10.1111/aos.12308.
Javitt J, Brauweiler HP, Jacobi KW, et al. Cataract extraction with multifocal intraocular lens implantation: clinical, functional, and quality-of-life outcomes. Multicenter clinical trial in Germany and Austria. J Cataract Refract Surg. 2000;26(9):1356–66. https://doi.org/10.1016/s0886-3350(00)00636-2.
Alió JL, Grzybowski A, Romaniuk D. Refractive lens exchange in modern practice: when and when not to do it? Eye Vis. 2014;1:10. https://doi.org/10.1186/s40662-014-0010-2.
Vingolo EM, Grenga P, Iacobelli L, Grenga R. Visual acuity and contrast sensitivity: AcrySof ReSTOR apodized diffractive versus AcrySof SA60AT monofocal intraocular lenses. J Cataract Refract Surg. 2007;33(7):1244–7. https://doi.org/10.1016/j.jcrs.2007.03.052.
Alfonso JF, Fernández-Vega L, Baamonde MB, Montés-Micó R. Prospective visual evaluation of apodized diffractive intraocular lenses. J Cataract Refract Surg. 2007;33(7):1235–43. https://doi.org/10.1016/j.jcrs.2007.03.034.
de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12(12): CD003169. https://doi.org/10.1002/14651858.CD003169.pub4.
Zeng M, Liu Y, Liu X, et al. Aberration and contrast sensitivity comparison of aspherical and monofocal and multifocal intraocular lens eyes. Clin Experiment Ophthalmol. 2007;35(4):355–60. https://doi.org/10.1111/j.1442-9071.2007.01452.x.
Wang SY, Stem MS, Oren G, Shtein R, Lichter PR. Patient-centered and visual quality outcomes of premium cataract surgery: a systematic review. Eur J Ophthalmol. 2017;27(4):387–401. https://doi.org/10.5301/ejo.5000978.
Vryghem JC, Heireman S. Visual performance after the implantation of a new trifocal intraocular lens. Clin Ophthalmol. 2013;7:1957–65. https://doi.org/10.2147/OPTH.S44415.
Jonker SMR, Bauer NJC, Makhotkina NY, Berendschot TTJM, van den Biggelaar FJHM, Nuijts RMMA. Comparison of a trifocal intraocular lens with a +3.0 D bifocal IOL: results of a prospective randomized clinical trial. J Cataract Refract Surg. 2015;41(8):1631–40. https://doi.org/10.1016/j.jcrs.2015.08.011.
Mojzis P, Kukuckova L, Majerova K, Liehneova K, Piñero DP. Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J Refract Surg. 2014;30(10):666–72. https://doi.org/10.3928/1081597X-20140903-06.
Laboratories A. AcrySof® IQ PanOptix® Trifocal Intraocular Lens (Model TFNT00) and AcrySof® IQ PanOptix® Toric Trifocal Intraocular Lens (Models TFNT30, TFNT40, TFNT50, TFNT60).
Bissen-Miyajima H, Ota Y, Hayashi K, Igarashi C, Sasaki N. Results of a clinical evaluation of a trifocal intraocular lens in Japan. Jpn J Ophthalmol. 2020;64(2):140–9. https://doi.org/10.1007/s10384-019-00712-4.
Kohnen T, Titke C, Böhm M. Trifocal intraocular lens implantation to treat visual demands in various distances following lens removal. Am J Ophthalmol. 2016;161:71–7.e1. https://doi.org/10.1016/j.ajo.2015.09.030.
Carreño E, Carreño EA, Carreño R, Carreño M, López V, Potvin R. Refractive and visual outcomes after bilateral implantation of a trifocal intraocular lens in a large population. Clin Ophthalmol. 2020;14:369–76. https://doi.org/10.2147/OPTH.S238841.
Ramamurthy D, Vasavada A, Padmanabhan P, et al. Clinical outcomes after bilateral implantation of a trifocal presbyopia-correcting intraocular lens in an Indian population. Clin Ophthalmol. 2021;15:213–25. https://doi.org/10.2147/OPTH.S279001.
Alfonso JF, Fernández-Vega-Cueto L, Fernández-Vega L, Montés-Micó R. Visual function after implantation of a presbyopia-correcting trifocal intraocular lens. Ophthalmic Res. 2020;63(2):152–64. https://doi.org/10.1159/000500834.
Lawless M, Hodge C, Reich J, et al. Visual and refractive outcomes following implantation of a new trifocal intraocular lens. Eye Vis. 2017;4:10. https://doi.org/10.1186/s40662-017-0076-8.
Nicula CA, Popescu R, Rednik AM, Nicula D, Bulboaca AE, Stanescu I. Refractive lens exchange in hyperopic presbyopes with the Acrysof IQ Panoptix intraocular lens: one-year results and analysis of the literature. Ther Clin Risk Manag. 2020;16:1125–37. https://doi.org/10.2147/TCRM.S279065.
Alió JL, Plaza-Puche AB, Alió Del Barrio JL, et al. Clinical outcomes with a diffractive trifocal intraocular lens. Eur J Ophthalmol. 2018;28(4):419–24. https://doi.org/10.1177/1120672118762231.
Kohnen T, Herzog M, Hemkeppler E, et al. Visual performance of a quadrifocal (trifocal) intraocular lens following removal of the crystalline lens. Am J Ophthalmol. 2017;184:52–62. https://doi.org/10.1016/j.ajo.2017.09.016.
García-Pérez JL, Gros-Otero J, Sánchez-Ramos C, Blázquez V, Contreras I. Short term visual outcomes of a new trifocal intraocular lens. BMC Ophthalmol. 2017;17(1):72. https://doi.org/10.1186/s12886-017-0462-y.
Donmez O, Asena BS, Kaskaloglu M, Akova YA. Patients satisfaction and clinical outcomes of binocular implantation of a new trifocal intraocular lens. Int Ophthalmol. 2020;40(5):1069–75. https://doi.org/10.1007/s10792-020-01390-9.
Kim T-I, Chung T-Y, Kim MJ, Lee K, Hyon JY. Visual outcomes and safety after bilateral implantation of a trifocal presbyopia correcting intraocular lens in a Korean population: a prospective single-arm study. BMC Ophthalmol. 2020;20(1):288. https://doi.org/10.1186/s12886-020-01549-z.
Wortz G, Gupta PK, Goernert P, et al. Outcomes of femtosecond laser arcuate incisions in the treatment of low corneal astigmatism. Clin Ophthalmol. 2020;7(14):2229–36. https://doi.org/10.2147/OPTH.S264370.
Ribeiro FJ, Ferreira TB. Comparison of visual and refractive outcomes of 2 trifocal intraocular lenses. J Cataract Refract Surg. 2020;46(5):694–9. https://doi.org/10.1097/j.jcrs.0000000000000118.
Zhu D, Ren S, Mills K, Hull J, Dhariwal M. Rate of complete spectacle independence with a trifocal intraocular lens: a systematic literature review and meta-analysis. Ophthalmol Ther. 2023. https://doi.org/10.1007/s40123-023-00657-5.
Donmez O, Asena BS, Aydin AY. Subjective and objective clinical outcomes of a new trifocal toric intraocular lens and effect of femtosecond laser cataract surgery. Eur J Ophthalmol. 2022;32(4):2225–33. https://doi.org/10.1177/11206721211046496.
Böhm M, Hemkeppler E, Herzog M, et al. Comparison of a panfocal and trifocal diffractive intraocular lens after femtosecond laser-assisted lens surgery. J Cataract Refract Surg. 2018;44(12):1454–62. https://doi.org/10.1016/j.jcrs.2018.07.060.
Fernández-García JL, Llovet-Rausell A, Ortega-Usobiaga J, et al. Unilateral versus bilateral refractive lens exchange with a trifocal intraocular lens in emmetropic presbyopic patients. Am J Ophthalmol. 2021;223:53–9. https://doi.org/10.1016/j.ajo.2020.09.044.
Djodeyre MR, Ortega-Usobiaga J, Beltran J, Druchkiv V, Baviera-Sabater J, Bouza-Miguens C. Bilateral refractive lens exchange with trifocal intraocular lens for hyperopia in patients younger than 40 years: a case-control study. J Refract Surg. 2021;37(8):524–31. https://doi.org/10.3928/1081597X-20210518-01.
Sezgin AB. Visual and refractive outcomes, spectacle independence, and visual disturbances after cataract or refractive lens exchange surgery: comparison of 2 trifocal intraocular lenses. J Cataract Refract Surg. 2019;45(11):1539–46. https://doi.org/10.1016/j.jcrs.2019.06.005.
Cochener B, Boutillier G, Lamard M, Auberger-Zagnoli C. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg. 2018;34(8):507–14. https://doi.org/10.3928/1081597X-20180530-02.
Hovanesian JA, Jones M, Allen Q. The PanOptix Trifocal IOL vs the ReSTOR 2.5 active focus and ReSTOR 3.0-add multifocal lenses: a study of patient satisfaction, visual disturbances, and uncorrected visual performance. Clin Ophthalmol. 2021;15:983–90. https://doi.org/10.2147/OPTH.S285628.
Moshirfar M, Stapley SR, Corbin WM, et al. Comparative visual outcome analysis of a diffractive multifocal intraocular lens and a new diffractive multifocal lens with extended depth of focus. J Clin Med. 2022;11(24):7374. https://doi.org/10.3390/jcm11247374.
Acknowledgements
Funding
This study was supported by an investigator-initiated trial research grant issued by Alcon (Fort Worth, TX, USA), which was used to fund study activities as well as the journal’s Rapid Service Fee. Alcon did not materially participate in the design, data collection, analysis, interpretation, or writing of any study-related activities.
Author Contributions
Dagny C. Zhu oversaw and provided supervision over the study conception and design. Material preparation, data collection and analysis were performed by Cindi K. Yim, Amisha Dave, Alyx Strawn, Jeffrey Chan, Irene Zhou, and Dagny C. Zhu. The first draft of the manuscript was written by Cindi K. Yim and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Prior Presentation
Data from this manuscript was presented at the American Society of Cataract and Refractive Surgery Annual Meeting in Las Vegas, USA, July 2021.
Disclosures
Dagny C. Zhu, MD is a consultant for Alcon, Inc. Alcon, Inc has provided research grant support for this investigator-initial trial including funding for the journal’s Rapid Service Fee, but did not materially participate in the design, data collection, analysis, interpretation, or writing of any study-related activities. Cindi K. Yim, Amisha Dave, Alyx Strawn, Jeffrey Chan, and Irene Zhou have no competing interests.
Compliance with Ethics Guidelines
The study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the ethical committee of the Salus Institutional Review Board. All patients provided written informed consent after explanation of the nature and possible consequences of the procedure.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yim, C.K., Dave, A., Strawn, A. et al. Visual Outcomes and Patient Satisfaction After Bilateral Refractive Lens Exchange with a Trifocal Intraocular Lens in Patients with Presbyopia. Ophthalmol Ther 12, 1757–1773 (2023). https://doi.org/10.1007/s40123-023-00708-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00708-x