Abstract
Introduction
This study assessed 5-year results of rotationally asymmetric multifocal intraocular lens (IOL) with +1.5 diopters (D) near addition (Lentis Comfort LS-313 MF15, Teleon Surgical B.V., Spankeren, Netherlands).
Methods
In 38 eyes of 20 patients (76.8 ± 4.6 years) who were examined at both 1 and 5 years after surgery, clinical data were retrospectively collected.
Results
Corrected and uncorrected distance visual acuity (5 m) and uncorrected and distance-corrected intermediate visual acuity (70 cm) were excellent, with no significant differences between 1 and 5 years after surgery. Uncorrected and distance-corrected near visual acuity (30 cm) remained lower. Contrast sensitivity was within the normal range at both 1 and 5 years. The percentage of patients who reported “never or hardly use spectacles” for far, intermediate, and near vision was 95.0%, 85.0%, and 35.0%, respectively. Glare and halo were slightly increased from 1 to 5 years after surgery, but the severity remained none or mild. All patients reported “very high” or “high” level of overall satisfaction. There were no notable postoperative complications.
Conclusions
During 5 years after surgery, low-add-power segmented multifocal IOL maintained excellent distance and intermediate visual acuity as well as good contrast sensitivity. Glare and halo symptoms were mild, and patients’ satisfaction level was high.
Trial Registration
University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) identifier UMIN000048353.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
There have been no reports on the long-term clinical results of the low-add-power segmented rotationally asymmetrical intraocular lens (IOL) |
The stability of a plate-haptic IOL within the eye may differ from that of an open-loop IOL, and concerns remain about their long-term stability as a result of insufficient data |
What was learned from the study? |
This lens maintained its performance with excellent far and intermediate vision over 5 years after surgery |
Contrast sensitivity was also good and disturbing photic phenomena were minimal |
There have been no cases of IOL-related complications, including tilt, decentration, dislocation, opacification, or calcification |
Introduction
Growing attention has been directed to intermediate vision, which is important for daily activities such as using computers and tablets, cooking, and viewing car instrument panels. Several designs of intraocular lenses (IOLs) have been introduced to provide useful intermediate vision after cataract surgery without compromising distant image quality. One such IOL is the rotationally asymmetric, refractive segmented IOL with +1.5 diopter (D) addition (Lentis Comfort LS-313 MF15, Teleon Surgical B.V., Spankeren, Netherlands). This is a non-diffractive multifocal IOL that is designed to boost intermediate performance while suppressing disturbing photic phenomena [1,2,3,4,5,6,7,8]. This IOL does not compromise contrast sensitivity of patients, and the frequency and degree of glare and halo are comparable to those of monofocal IOLs [4,5,6,7,8]. While short-term clinical results have been documented [1,2,3,4,5,6,7,8], the long-term outcomes have not yet been reported. While open-loop-style IOLs have a well-established long track record, concerns may remain about the mid- to long-term stability of plate-haptic-type IOLs as a result of insufficient data. To address this, we conducted the current study to evaluate 5-year clinical results of this IOL.
Methods
Patients
We recruited patients who had undergone phacoemulsification and implantation of Lentis Comfort for age-related cataract and had been examined at both 1 and 5 years postoperatively. At the time of cataract surgery, none of the eyes had any history of previous ocular surgery, ocular diseases that could affect surgical outcomes, or corneal astigmatism greater than 1.5 D.
Three surgeons from three surgical sites performed surgeries, using a standard technique of phacoemulsification with a self-sealing 2.3- or 2.4-mm incision placed on the temporal side. After removal of nucleus and cortex through anterior capsulorrhexis of approximately 5.0 mm in diameter, the IOL was implanted into the capsular bag using an injector.
Examinations
At 1 and 5 years postoperatively, ocular examinations were carried out including manifest refraction, uncorrected (UDVA) and corrected (CDVA) distance visual acuity at 5 m, uncorrected (UIVA) and distance-corrected (DCIVA) intermediate visual acuity measured at 70 cm, uncorrected (UNVA) and distance-corrected (DCNVA) near visual acuity measured at 30 cm, and contrast sensitivity. Intermediate and near visual acuity was measured using the C-Landolt near and intermediate visual acuity chart (TMI-V5, T.M.I. Company, Limited, Saitama, Japan). Contrast sensitivity was assessed using the CSV-1000 chart (Vector Vision, Greenville, OH, USA) at 3, 6, 12, and 18 cycles per degree (cpd). The test was performed at a distance of 2.5 m with refractive correction, and the background illumination for the translucent chart was provided by the fluorescent luminance source that was automatically calibrated to 85 cd/m2.
The subjective severity of photic phenomena was assessed at 1 and 5 years postoperatively. The intensity of glare and halo was graded from none, mild, moderate, to severe. The degree of difficulty in night vision was categorized from none, mild to moderate, to severe. The overall satisfaction with surgical outcomes was assessed using a 4-point scale (very high, high, medium, and low).
At 5 years postoperatively, patients were asked about their dependency on spectacles for far, intermediate, and near vision. Spectacle dependency was evaluated using a 4-point scale: “never or hardly use,” “occasionally use,” “sometimes use,” and “usually or always use.” In the questionnaire, “far” was defined to be distance for driving or outdoor activity, “intermediate” was defined to be computer work or housework distance, and “near” was defined as distance for books or smartphone.
Any episode of postoperative adverse effects was recorded throughout the study period.
The study protocol was approved by the Nihonbashi Sakura Clinic Research Ethics Committee and each patient gave informed consent in a written form or oral agreement. This study adhered to the tenets of the Declaration of Helsinki, the good clinical practice guide for medical devices in Japan (Pharmaceuticals and Medical Devices Agency: PMDA clinical trial identifier TC2), and the Ethical Guidelines for Medical and Biological Research Involving Human Subjects. This study was registered at University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) UMIN000048353 (https://center6.umin.ac.jp/cgi-open-bin/ctr/ctr_view.cgi?recptno=R000055111). This study was funded by Santen Pharmaceutical Co., Ltd.
Statistical Analysis
Numerical data are expressed as mean ± standard deviation. Statistical comparisons between two paired measurements were performed using the paired t test after verifying the normal distribution of the data with the Kolmogorov–Smirnov test. For categorical data, the chi-square test and Fisher’s exact test for trend were used to assess the difference in incidence rates. Correlations between two numerical parameters were tested using the Pearson correlation coefficient. Statistical analysis was performed using SPSS Statistics for Windows software (version 28, IBM Corp., Armonk, NY, USA). In all cases, the level of significance was a p value less than 0.05.
Results
Data were collected from 38 eyes of 20 patients who underwent ophthalmic examinations at both 1 and 5 years postoperatively. There were 3 male and 17 female patients, and their age at the final visit was 76.8 ± 4.6 (69–86) years old.
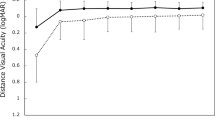
Manifest refraction spherical equivalent became slightly myopic from 1 to 5 years postoperatively (− 0.07 ± 0.41 D to − 0.18 ± 0.45 D), but the difference was not statistically significant (p = 0.102). There was no significant change in the amount of refractive astigmatism from 1 year (0.35 ± 0.42 D) to 5 years (0.53 ± 0.51 D) (p = 0.131). Visual acuity is shown in Fig. 1. At both 1 and 5 years, good distance visual acuity was obtained, with UDVA and CDVA of approximately 20/20 and 20/16, respectively. Intermediate visual acuity was also satisfactory, with UIVA and DCIVA of around 20/25 after surgery. On the other hand, near visual acuity was suboptimal, being lower compared with distance and intermediate visual acuity. UNVA and DCNVA were at the level of around 20/60. The difference between 1 and 5 years after surgery was not statistically significant for UDVA (p = 0.580), CDVA (p = 0.305), UIVA (p = 0.488), and DCIVA (p = 0.221). However, UNVA (p < 0.001) and DCNVA (p < 0.001) were significantly better at 5 years than at 1 year postoperatively (Fig. 1). At 5 years postoperatively, manifest refraction spherical equivalent showed a significant correlation with UNVA (r = 0.715, p < 0.001) and DCNVA (r = 0.552, p < 0.001).
Visual acuity at 1 and 5 years. Uncorrected (UDVA) and corrected (CDVA) distance visual acuity, and uncorrected (UIVA) and distance-corrected (DCIVA) intermediate visual acuity remained at a high level through 5 years postoperatively. Near visual acuity was suboptimal, but both uncorrected (UNVA, *p < 0.001) and distance-corrected (DCNVA, *p < 0.001) near visual acuity significantly improved from 1 to 5 years after surgery
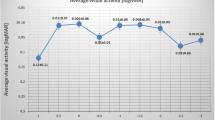
Contrast sensitivity measured at 1 and 5 years postoperatively is plotted in Fig. 2. The results were within the range of age-considered normal controls as reported in the literature [9]. There was no difference between 1 and 5 years for all spatial frequencies; 3 cpd (p = 0.219), 6 cpd (p = 0.745), 12 cpd (p = 0.709), and 18 cpd (p = 0.959).
Incidence and intensity of glare and halo are summarized in Table 1. The degree of glare (p < 0.001) and halo (p < 0.001) significantly increased from 1 to 5 years, but most patients reported none to mild symptoms. Very few patients reported difficulty in night vision at both 1 and 5 years, with no difference between the two points (Table 2). The majority of patients rated their overall satisfaction as very high or high (Table 3), but the level of satisfaction decreased significantly from 1 to 5 years postoperatively (p < 0.001).
Spectacle independence at 5 years postoperatively is shown in Fig. 3. While most patients did not use spectacles for far and intermediate vision, reading glasses were necessary for near vision in approximately two-third of patients.
Eight eyes (21.1%) developed posterior capsule opacification (PCO), which was evident on slit-lamp microscopic examination. Among these, three eyes (7.9%) were treated with YAG laser posterior capsulotomy at 3 months, 3 years, and 5 years postoperatively. The presence of PCO was not correlated with the severity of glare (p = 0.555, Table 4), halo (p = 0.615, Table 4), and difficulty in night vision (p = 0.428, Table 5) at 5 years postoperatively. There were no other postoperative complications, such as IOL decentration, tilt, opacification, and calcification.
Discussion
At 1 year after implantation of a rotationally asymmetric multifocal IOL with +1.5 D near addition, good distance (UDVA and CDVA) and intermediate visual acuity (UIVA and DCIVA) was obtained, but near visual acuity (UNVA and DCNVA) remained at a lower level, ranging from 20/60 to 20/70. These results are consistent with previous studies [4, 7, 8]. In the longer-term, while distance and intermediate visual acuity remained stable over years, near visual acuity significantly improved from 1 to 5 years after surgery. During this time, manifest refraction showed a slight myopic shift (− 0.07 ± 0.41 D to − 0.18 ± 0.45 D). Since the spherical equivalent showed a significant correlation with UNVA at 5 years postoperatively, the improvement of UNVA appears to be attributable to the minor myopic shift in refraction. However, this shift was not large enough to influence distance and intermediate vision. On the other hand, improvement in DCNVA cannot be explained by myopic changes because DCNVA was measured with refractive correction. Other factors, such as age-related miosis, increases in corneal wavefront aberration, and changes in corneal multifocality, which are among the known factors that are associated with the amplitude of apparent accommodation in pseudophakic eyes [10,11,12,13], may have played a role. However, the current retrospective study cannot provide a conclusive explanation for these results, as it lacks data on anterior chamber depth, pupillary diameter, corneal topography, and optical aberrations. Further studies are necessary to clarify these points.
Previous studies have reported that Lentis Comfort LS-313 MF15 did not compromise contrast sensitivity compared with monofocal IOLs [4,5,6,7,8]. In this study, contrast sensitivity assessed at 1 and 5 years postoperatively was within the range of age-considered normal controls, and there was no difference between the two time points. Since contrast sensitivity was measured with refractive correction, the myopic shift mentioned earlier did not affect the measurement results. Overall, our results indicate that optical quality of this IOL was maintained throughout the 5-year follow-up period.
In the current study, at both 1 and 5 years, none of the patients complained of severe disturbing photic phenomena, and most patients reported no or minor symptoms of glare and halo. The level of satisfaction was very high or high in all patients. Similar results were reported previously. Kim et al. [5] showed that low-power-added multifocal IOLs yielded better intermediate and near vision as well as greater overall satisfaction without increasing optical phenomena compared to monofocal IOLs. Vounotrypidis et al. [3] indicated that patient satisfaction was very high, and few patients reported disturbing photic phenomena after implantation of Lentis Comfort LS-313 MF15. Yoo et al. [1] demonstrated that there were fewer glare and halo symptoms with Lentis Comport (+ 1.5 D add) than with Lentis M plus (+ 3.0 D add). Song et al. [6] concluded that dysphotopsia symptoms were comparable between Lentis Comfort LS-313 MF15 and conventional monofocal IOLs.
Patients’ evaluation of these parameters, however, significantly worsened from 1 to 5 years postoperatively (Tables 1 and 3), despite far and intermediate visual acuity as well as contrast sensitivity being maintained at a very high level for 5 years after surgery. Near visual acuity even improved from 1 to 5 years postoperatively. Several hypothesized mechanisms may underlie the discrepancy between the subjective and objective assessments; the subclinical age-related changes in a patient’s vision system including the cornea, retina, nerve, and brain over time. The presence of PCO was not correlated with the severity of glare, halo, and difficulty in night vision at 5 years postoperatively. Psychological factors might be involved. The impact of visual recovery after surgery may have diminished over time. Comparison of subjective parameters at two separate time points is challenging, particularly when the evaluation is conducted several years apart and involves elderly patients, as in this study.
Spectacle independence is one of the important issues which are closely related to the success of multifocal IOLs. In this study, very few patients used glasses for far and intermediate vision, while approximately two-third of patients depended on reading glasses for near vision. These results are in line with the concept of low-power-added multifocal IOLs. Kim et al. [5] found that spectacle use at intermediate working distance was significantly less frequent with Lentis Comfort than with conventional monofocal IOLs. Pedrotti et al. [4] also revealed that Lentis Comfort offered good intermediate spectacle independence with a high quality of vision.
This study has several limitations. First, there was no control group, such as patients implanted with a monofocal IOL. Second, no data were collected between 1 and 5 years after surgery. Third, the number of subjects is small. Fourth, several important data are missing in this retrospective study, such as anterior chamber depth, pupillary diameter, corneal topography, and wavefront aberrations.
Conclusion
The low-add-power segmented rotationally asymmetrical IOL maintained its performance with excellent far and intermediate vision over 5 years after surgery. Contrast sensitivity was also good and disturbing photic phenomena were minimal.
References
Yoo A, Kwag JY, Song IS, et al. Comparison of visual function after implantation of inferior sector-shaped intraocular lenses: low-add +1.5 D vs +3.0 D. Eur J Ophthalmol. 2016;26:607–11.
Kretz FT, Khoramnia R, Attia MS, Koss MJ, Linz K, Auffarth GU. Clinical evaluation of functional vision of +1.5 diopters near addition, aspheric, rotational asymmetric multifocal intraocular lens. Korean J Ophthalmol. 2016;30:382–9.
Vounotrypidis E, Diener R, Wertheimer C, et al. Bifocal nondiffractive intraocular lens for enhanced depth of focus in correcting presbyopia: clinical evaluation. J Cataract Refract Surg. 2017;43:627–32.
Pedrotti E, Mastropasqua R, Bonetto J, et al. Quality of vision, patient satisfaction and long-term visual function after bilateral implantation of a low addition multifocal intraocular lens. Int Ophthalmol. 2018;38:1709–16.
Kim KH, Kim WS. Visual outcome and patient satisfaction of low-power-added multifocal intraocular lens. Eye Contact Lens. 2018;44:60–7.
Song X, Liu X, Wang W, et al. Visual outcome and optical quality after implantation of zonal refractive multifocal and extended-range-of-vision IOLs: a prospective comparison. J Cataract Refract Surg. 2020;46:540–8.
Oshika T, Arai H, Fujita Y, et al. One-year clinical evaluation of rotationally asymmetric multifocal intraocular lens with +1.5 diopters near addition. Sci Rep. 2019;9:13117.
Oshika T, Negishi K, Noda T, et al. Prospective assessment of plate-haptic rotationally asymmetric multifocal toric intraocular lens with near addition of + 1.5 diopters. BMC Ophthalmol. 2020;20:454.
Hashemi H, Khabazkhoob M, Jafarzadehpur E, Emamian MH, Shariati M, Fotouhi A. Contrast sensitivity evaluation in a population-based study in Shahroud, Iran. Ophthalmology. 2012;119:541–6.
Fukuyama M, Oshika T, Amano S, Yoshitomi F. Relationship between apparent accommodation and corneal multifocality in pseudophakic eyes. Ophthalmology. 1999;106:1178–81.
Oshika T, Mimura T, Tanaka S, et al. Apparent accommodation and corneal wavefront aberration in pseudophakic eyes. Investig Ophthalmol Vis Sci. 2002;43:2882–6.
Kamiya K, Kawamorita T, Uozato H, Kasugai H, Shimizu K. Effect of astigmatism on apparent accommodation in pseudophakic eyes. Optom Vis Sci. 2012;89:148–54.
Yamamoto T, Hiraoka T, Oshika T. Apparent accommodation in pseudophakic eyes with refractive against-the-rule, with-the-rule and minimum astigmatism. Br J Ophthalmol. 2016;100:565–71.
Acknowledgements
Funding
This study was funded by Santen Pharmaceutical Co., Ltd., who also funded the journal's Rapid Service Fee.
Author Contributions
Dr. Tetsuro Oshika conceived and designed the study. Drs. Hiroyuki Arai, Yasushi Inoue and Yoshifumi Fujita collected the data. Dr. Oshika analyzed the data and drafted the manuscript. All authors read and approved the final manuscript.
Disclosures
Tetsuro Oshika is a consultant for Santen Pharmaceutical Co., Ltd. Hiroyuki Arai, Yasushi Inoue and Yoshifumi Fujita have nothing to disclose.
Compliance and Ethics Guidelines
The study protocol was approved by the Nihonbashi Sakura Clinic Research Ethics Committee and each patient gave informed consent in a written form or oral agreement. This study adhered to the tenets of the Declaration of Helsinki, the good clinical practice guide for medical devices in Japan (Pharmaceuticals and Medical Devices Agency: PMDA clinical trial identifier TC2), and the Ethical Guidelines for Medical and Biological Research Involving Human Subjects. This study was registered at University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) UMIN000048353; https://center6.umin.ac.jp/cgi-open-bin/ctr/ctr_view.cgi?recptno=R000055111.
Data Availability
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Oshika, T., Arai, H., Inoue, Y. et al. Five-Year Clinical Outcomes of Low-Add-Power Segmented Rotationally Asymmetrical Intraocular Lens. Ophthalmol Ther 12, 1649–1656 (2023). https://doi.org/10.1007/s40123-023-00703-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00703-2