Abstract
Introduction
This study aimed to investigate the distribution of corneal spherical aberration (CSA) and the relationship between corneal curvature with CSA and anterior chamber parameters in age-related cataract patients with normal axial lengths and shallow anterior chambers.
Methods
Preoperative data of age-related cataract patients were collected in this retrospective comparative study. According to the average corneal curvature, the eyes were divided into groups of Km < 42 diopters (D), 42 D ≤ Km < 45 D, and Km ≥ 45 D. The axial length (AL) and corneal curvature were obtained using IOLMaster. CSA, anterior chamber depth (ACD), anterior chamber volume (ACV), anterior chamber angle (ACA), and corneal diameter (CD) were acquired according to Pentacam. The above parameters were compared among the three groups. Correlation analysis was applied to these parameters.
Results
The average CSA value of 753 eyes was 0.41 ± 0.27 μm, with no significant difference among the three groups. Overall, CSA was significantly correlated with corneal curvature and ACD. The comparison of ACD among the three groups showed significant differences between the Km ≥ 45 D group, Km < 42 D group, and 42 D ≤ Km < 45 D group. Corneal curvature was positively correlated with ACD, and further analysis confirmed that the relationship was significant only in the Km ≥ 45 D group. There were statistically significant differences in CD between the three groups. A significant correlation was found in corneal curvature and CD in all eyes, which was also found in the 42 D ≤ Km < 45 D group and the Km ≥ 45 D group. Concerning ACV and ACA, no correlation with corneal curvature was found. In addition, the mean ACV and ACA of the three groups did not show any significant difference.
Conclusions
CSA was higher in this population and had individual variance. Compared with ACD, ACV and ACA were more stable in different corneal curvatures and more objective in representing the anterior chamber space.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Age-related cataract patients with shallow anterior chambers constitute the majority of cataract patients in China. The specific biological characteristics of this population make it particular and complicated in personalized selection of intraocular lens (IOLs) and surgical treatment. |
What was learned from this study? |
The corneal spherical aberration (CSA) of age-related cataract patients with normal axial length (AL) and shallow anterior chamber was higher than the general population and had individual variance. Although CSA and anterior chamber depth (ACD) increased and corneal diameter (CD) reduced with increasing corneal curvature, the anterior chamber volume (ACV) and anterior chamber angle (ACA) remained relatively stable among the groups. The distribution features of the CSA and the consistency of anterior chamber space in this population were conducive for surgeons to optimize IOL choice and improve surgical outcomes. |
Introduction
Cataract surgery is one of the most successful and sophisticated treatments in all of medicine. During the past few decades, cataracts have already evolved into a refractive surgery era from visual rehabilitation, mainly benefiting from great technological advancements [1]. With the continuous update and improvement of ophthalmic biometric measurement equipment, it is possible to accurately acquire ocular biological parameters, such as axial length (AL), corneal curvature, anterior chamber depth (ACD), and aberration [2,3,4,5]. A previous population-based study showed that the average ACD of Chinese individuals is 2.42 mm, which is significantly shallower than that of Caucasians and is likely to decrease with age [6, 7]. Based on the fact that a shallower anterior chamber is more prone to develop suspicious primary angle closure, using phacoemulsification to avoid the risk of angle closure has become a new trend in clinical treatment for shallow anterior chamber populations over 50 years old [8]. However, such individuals have a relatively good visual history, which makes them pursue the highest quality of visual acuity and contrast sensitivity after surgery. To achieve these targets, a successful operation with an ideal IOL choice is the premise and guarantee.
High-order aberrations of the human eyes are the most important factors affecting visual quality [9,10,11]. Corneal spherical aberration (CSA) is considered as the major high-order aberration that is highly prevalent worldwide and has a crucial impact on visual performance [12, 13]. In recent years, new intraocular lens (IOLs) designs, such as aspheric IOLs, which introduce a negative or zero spherical aberration to the ocular system and compensate for the positive spherical aberration of the cornea by replacing the crystalline lens, have promoted remarkable advances in cataract surgery [14]. Therefore, fully understanding the characteristics and distribution of CSA in different populations is of great importance.
Cataract patients with shallow anterior chambers present special difficulties, such as narrow operating space, high risk of complications, and inaccurate calculation of intraocular lens diopters, which consequently influence postoperative visual outcomes. This is largely due to the particular morphology of the anterior chamber space. Although some researchers have focused on the relationship between the ocular biomechanical parameters in recent years, most studies involve patients with normal ACD [15, 16]. The correlations between these parameters and spherical aberration in shallow anterior chamber cases remain uncertain. Considering the specificity and disparity of the anterior segment in these patients, the safety of cataract surgery or personalized selection of IOLs requires thoughtful consideration. Thus, in the present study, our goals were as follows: (1) to investigate the distribution of CSA and explore correlations of CSA with corneal curvature and other anterior chamber parameters in age-related cataract patients with normal ALs and shallow anterior chambers and (2) to evaluate the characteristics and relationships of anterior chamber parameters in this population.
Patients and Methods
Subjects
Preoperative data of age-related cataract patients who underwent phacoemulsification and IOLs implantation in the Department of Ophthalmology at Peking University International Hospital from March 2019 to December 2021 were collected in this retrospective comparative study. The right eye of each subject was chosen as the study object. The inclusion criteria were age > 50 years and diagnosis of age-related cataract with AL between 22 and 24 mm and ACD less than 2.20 mm. We defined 2.20 mm as the cutoff point for a shallow ACD according to a large population-based study [6] that revealed the mean ACD values for women were 2.42 mm (25th–75th percentile, 2.21–2.63 mm). Exclusion criteria were previous corneal refractive surgery, corneal degeneration and dystrophy, ocular trauma, unsatisfactory intraocular pressure control of glaucoma, uveitis, macular or retinal disease, previous laser or intraocular surgery, and poor image quality. Seven hundred fifty-three eyes (283 male and 470 female) from patients with average age of 75 ± 10 years (range 50–90 years) were included in this study. Based on the results of recent studies about distribution of corneal curvature [7, 17], all eyes were classified into three groups according to the average value of keratometry, i.e., Km < 42 D (63 eyes, 8.37%), 42 D ≤ Km < 45 D (480 eyes, 63.74%), and Km ≥ 45 D (210 eyes, 27.89%). The study adhered to the tenets of the Declaration of Helsinki and was approved by the ethics committee of Peking University International Hospital (2021‐038 (BMR)). All participants were informed of the purpose of the study and signed informed consent forms.
Clinical Observations
Basic information, including the age and sex of the patients, was recorded. All research subjects underwent routine ocular examinations, including visual acuity, intraocular pressure, slit-lamp examination, fundus examination, mydriatic optometry, corneal topography, and corneal endothelium counting. CSA, AL, ACD, corneal diameter (CD), anterior chamber volume (ACV), and anterior chamber angle (ACA) were also measured and recorded.
All data were collected in automode, centered at the corneal apex, with a rotating Scheimpflug camera (Pentacam; Oculus, Wetzlar, Germany) and partial coherence interferometry (IOLMaster500; Carl Zeiss Meditec, Jena, Germany) by one of two skilled examiners to eliminate any latent examiner bias as much as possible. The examination was considered valid only if the quality expressed by the software was “OK”. Each patient’s last acceptable reading was used for the subsequent analysis. AL and corneal curvature were measured using an IOL Master 500 optical biometer. Examinations were performed in the same darkroom. The examined eye was at natural pupil size. The subject was seated with the mandible placed in the mandibular bracket and the forehead close to the forehead bracket. Two eyes were located in the same horizontal position, staring at the indicator. The eye was blinked once before measurement. AL was measured five times and averaged. Corneal curvature was measured three times and averaged. Values with signal-to-noise ratio over 100 were considered to be accurate and reliable. CSA, ACD, ACV, CD, and ACA were measured using the Pentacam. The patient was instructed to maintain steady fixation on the central target for the duration of the scan to avoid acquisition artifacts (such as blinking or motion) and spurious tilt or eye rotation. An automatic acquisition function was applied on the Pentacam, which meant that the operator manually aligned the instrument to the pupil center, but the images were automatically acquired once alignment was achieved. ACD, ACV, CD, and ACA were measured before mydriasis. CSA was measured at pupil diameter of 6 mm. Zernike polynomials are representations of the higher- and lower-order aberrations of the cornea. CSA equal to the primary spherical aberration (Z4(0)) of the total cornea. ACD is defined as the distance from the corneal endothelium to the anterior surface of the lens. ACV is the volume between the corneal endothelium and the surface of the iris and lens. ACA is the angle between the reverse extension lines of the posterior surface of the cornea and the anterior surface of the iris on the 180° horizontal scanning section. Both the nasal and temporal chamber angles were measured, and the minor chamber angle was used for analysis. CD refers to the distance between the temporal limbus and the nasal limbus on the 180° horizontal scanning section.
Statistical Analysis
All statistical analyses were performed by using SPSS software (version 24.0; SPSS Inc., Chicago, IL, USA). The Kolmogorov–Smirnov test was used to assess the normality of the distribution of continuous variables. Values are presented as mean ± standard deviation for data that were normally distributed or median and interquartile range for data that were not. One-way analysis of variance (ANOVA) with post hoc Bonferroni tests and the Kruskal–Wallis test were used to compare data among different groups. Student’s t-test and the Mann–Whitney U test were used to compare data as appropriate. Correlations between corneal curvature, CSA, and other parameters were assessed using Pearson’s correlation test. For all statistical tests, P value less than 0.05 was considered statistically significant.
Results
The study included 753 patients (753 eyes) with mean AL of 22.85 ± 0.67 mm, mean corneal curvature of 44.02 ± 1.53 D, mean CD of 11.30 ± 0.31 mm, mean ACD of 1.95 ± 0.21 mm, mean ACV of 78.45 ± 20.38 mm3, and mean ACA of 25.24° (21.22°, 29.18°). The age and sex distribution were similar among the three groups.
Distribution of CSA and Correlations with Other Parameters
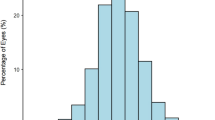
The average value of CSA of 753 eyes was 0.41 ± 0.27 μm with a range of −0.69 to 1.94 μm (Fig. 1; Table 1). The mean CSA in the Km < 42 D group was 0.38 ± 0.14 μm, while in the 42 D ≤ Km < 45 D group and in the Km ≥ 45 D group, it was 0.40 ± 0.31 μm and 0.42 ± 0.25 μm, respectively. Although the difference among the three groups was not significant (P > 0.05), the mean CSA increased with increasing corneal curvature. Further analysis revealed significant positive, yet weak, correlations between CSA and the following parameters: Km (r = 0.17, P = 0.002) and ACD (r = 0.14, P = 0.001) (Fig. 2). No significant correlation was indicated between CSA and other parameters such as age, AL, CD, ACV, and ACA (all P > 0.05).
Correlation analyses between CSA and other parameters. a Correlation between CSA and mean corneal curvature (r = 0.17, P < 0.01). b No significant correlation was found between CSA and age (P > 0.05). c Correlation between CSA and ACD (r = 0.14, P < 0.01). CSA corneal spherical aberration, ACD anterior chamber depth
Correlations of Corneal Curvature with AL and Age
There was a significant difference in AL among the three groups (F = 76.25, P < 0.001; Table 2). Pearson’s analysis showed a statistically significant and moderately negative correlation between corneal curvature and AL in 753 eyes (r = −0.60, P < 0.001). After grouping, the ALs of the three groups all presented a negative correlation with corneal curvature (Table 3). However, there was no significant relationship between age and AL or corneal curvature (r = 0.03, 0.15; P = 0.455, 0.131).
Correlation of Corneal Curvature with ACD
There was a statistical significance in the ACD among the three groups (F = 5.15, P = 0.001; Table 2). Further pairwise comparison showed no significant difference in ACD between the Km < 42 D group and the 42 D ≤ Km < 45 D group (t = 2.04, P = 0.154), while the mean value of the Km ≥ 45 D group was significantly larger than that of the Km < 42 D group (t = 7.89, P = 0.004) and the 42 D ≤ Km < 45 D group (t = 4.59, P = 0.033). Pearson’s correlation analysis revealed that corneal curvature was positively correlated with ACD in 753 eyes (r = 0.26, P = 0.006; Fig. 3). As the corneal curvature increased, the ACD showed a positive shift. Additionally, intragroup analysis showed that a similar positive correlation existed only in the Km ≥ 45 D group (r = 0.23, P = 0.023; Table 3), while no relationship was found in the other two groups. Likewise, there was no significant correlation between age and ACD (r = −0.09, P = 0.078).
Correlation of Corneal Curvature with CD
There was a statistically significant difference in CD among the three groups (F = 85.98, P < 0.001; Table 2). Further comparison of the Km < 42 D group versus the 42 D ≤ Km < 45 D group, the 42 D ≤ Km < 45 D group versus the Km ≥ 45 D group, and the Km < 42 D group versus the Km ≥ 45 D group all showed significant differences in CD value (t = 1.92, 2.97, 2.02; P = 0.030, 0.004, 0.007). Pearson’s analysis revealed that there was a statistically significant and moderately negative correlation between corneal curvature and CD in 753 eyes (r = − 0.52, P < 0.001; Fig. 4). The intragroup analysis revealed a similar relationship in both the 42 D ≤ Km < 45 D group and the Km ≥ 45 D group, except for the Km < 42 D group (Table 3). No significant correlation was found between age and CD (r = − 0.01, P = 0.927).
Correlation of Corneal Curvature with ACV and ACA
Regarding ACV, no significant difference was found among the groups (Table 2). Similarly, as presented in Table 3, no significant correlation was found between corneal curvature and ACV either in a total of 753 eyes or in each group (all P > 0.05). For ACA, neither comparison of the mean values among groups nor the correlation analysis with corneal curvature in all subjects and within groups reached a significant level. Additionally, age was not correlated with ACV or ACA.
Discussion
The current study was the first to analyze the distribution of CSA and the correlation of corneal curvature with spherical aberration and anterior chamber parameters in age‐related cataract patients with normal AL and shallow anterior chamber. Our results indicated that the average value of CSA was 0.41 ± 0.27 μm in this population and showed significant positive, yet weak, statistically correlations with Km and ACD. Moreover, the anterior chamber depth deepened and the corneal diameter decreased with the steepness of corneal curvature, but there was no significant change in ACV or ACA.
Wavefront aberrations, especially spherical aberration (SA), are now widely accepted as vital factors in visual quality [18, 19]. The SA is caused by the inconsistent refracting ability of different positions of the spherical optical system to the light. The paraxial light and the abaxial light fail to converge at the same point after refraction, resulting in SA. The presence of SA in the eye can be considered as a benefit or drawback depending on the visual conditions and requirements. The decrease in SA helps to improve distance visual performance, but, on the contrary, the increase in SA expands the depth of focus [20]. Surgical decisions should be taken considering the possible benefit, drawbacks, and balancing of both sides, in addition to the defocus shift of the highest peak of visual acuity. SA comprises CSA and intraocular SA, which the latter mainly come from the lens [21]. In young eyes, CSAs, which are usually positive, are compensated by internal negative aberrations of the crystalline lens, resulting in few total aberrations and maintaining good visual quality [22]. Owing to age-related changes in the lens, which gradually decrease the negative aberration or transition to positive aberration, ocular SA significantly increases and greatly affects the visual outcome of the elderly individuals. Aspheric IOLs designed with zero or negative SA can reduce or eliminate CSA after removal of the crystalline lenses. To effectively compensate for CSA, we need to understand the distribution of CSA to individualize the choice of IOL. Until recently, numerous studies have been conducted centered on the CSA of cataract patients, with a lack of studies on patients with normal AL and short anterior chambers. In the present research, the results established that the mean value of CSA across this population is 0.41 μm over a 6.0 mm diameter with a range from −0.69 to 1.94 μm. This value is larger than previous results. Wang et al. [23] investigated the corneal aberrations of 228 eyes by using the CTView program and found a mean CSA of 0.281 ± 0.086 μm. Wei et al. [24] measured the higher-order aberrations in the central 6-mm zone of the cornea using an iTrace wavefront analyzer, and found that the CSA ranged from 0.015 to 0.726 μm, with a median value of 0.258 μm. Beiko et al. [25] used the Oculus Easygraph to measure the CSA of 696 healthy subjects and found a mean spherical aberration of 0.270 ± 0.089 μm, with a fluctuation range between +0.041 μm and +0.632 μm. Tarfah et al. [26] applied the Pentacam HR system and revealed a mean CSA of 0.3354 ± 0.1965 μm. The reason for the disparity in results could be attributed to differences in sample type and size. In addition, inconsistent pupil size among studies during measurement might be an explanation for the difference. Furthermore, applying different measuring instruments was another factor. The Pentacam HR system acquired information of the anterior segment more efficiently and quickly with a rotating Scheimpflug camera than corneal topography based on a Placido disc. In the current study, we demonstrated that the total CSA in cataract patients with normal AL and a short anterior chamber was larger than the average level in the general population and had great individual variance. The variations should be taken into consideration to guide the choice of customized IOLs to compensate for CSA in cataract surgery.
To further investigate the characteristics of CSA in this population, we conducted correlation analyses and found a weak but significant positive correlation with both corneal curvature and ACD. In contrast, age seemed to be independent of CSA. Regarding the factors that may affect the CSA, recent studies failed to achieve consensus on the predictors of the CSA. Wang et al. [23] identified that CSA did not vary significantly with age. Lai et al. [27] and Shimozono et al. [28] both reported a negative significant correlation between CSA and AL, Lim and Fam [29] detected no correlations between CSA and other refractive parameters, while Gaku et al. [30] reported a positive correlation between CSA and age. Coincidentally, a large cohort of cataract surgery candidates studied by Rania exhibited a similar relationship with corneal curvature and ACD, but unlike our work, they also proved a similar relationship with age [31]. They believed that changes in the steepest meridian of the cornea with ageing resulted in an increase in corneal asymmetry and aberrations. Based on comparisons with previous studies, we deduced that, in this population, corneal curvature and ACD, which were independent of age, were much more meaningful dynamic parameters for CSA.
The present study revealed a positive correlation between corneal curvature and ACD in age‐related cataract patients with normal AL and a shallow anterior chamber. Further pairwise comparison verified that the trend became obvious only when corneal curvature was over 45 D. Jonas et al. [16] confirmed the positive relationship between corneal curvature and ACD, while Fotedar et al. [17] failed to reduplicate the correlation in a 10-year longitudinal study of Caucasians. We speculated that the explanation for the disparity in results could be attributed to the difference in ethnicity, age, and sample size among studies; for instance, a widely accepted deeper ACD in Caucasians made it less clinically valuable compared with Asians, let alone with a shallow ACD. Furthermore, it should be noted that 91.63% of this population had corneal curvature over 42 D. Considering the negative correlation between corneal curvature and AL in our results, which had been reported previously and believed to be the compensatory mechanism for emmetropia [32], normal or steepened corneal curvature with minor short AL are the main biological characteristics of this population.
Apart from the ACD, the ACV and ACA are vital parameters of the anterior chamber space. However, our study showed that there was no significant correlation between corneal curvature and ACV and ACA in total subjects or in subgroups. This indicated that, although ACD had already deepened when corneal curvature was over 45 D, ACV and ACA were still consistent with the other two groups. Conversely, one previous study reported that ACV and ACA were both positively correlated with corneal curvature by observing the distribution of parameters in 6311 cases in patients 40–64 years of age [33]. To explore the possible reasons for the difference, we compared the CD of groups with different corneal curvatures. Based on the results, we could speculate that the decrease in CD in groups with steeper corneal curvature might be the reason why the ACV and ACA remained the same. In addition, the subjects of this study were patients with age-related cataracts. Changes in the lens, which lead to abnormal location and proportion of intraocular structures, may have an impact on the results.
Shallow and crowded anterior chambers, which are not unusual in the clinic, are commonly present in patients with nanophthalmos, relative anterior microphthalmos (RAM), primary angle-closure glaucoma, and IOL dislocation. Nanophthalmos usually refers to an eye with an AL shorter than 20 mm and hypermetropia between 13 and 18 D, and is mostly accompanied by a small cornea [34]. Primary angle closure glaucoma often shows the anatomical characteristics of elevated intraocular pressure with shallow ACD, narrow ACA, and short AL. Relaxation or rupture of lens zonular may lead to pupillary block, vitreous hernia, secondary glaucoma, and so on owing to the forward movement of the lens. All of the abnormalities mentioned above can easily attract the attention of ophthalmologists, thus adjusting the surgical plan promptly. RAM refers to eyes with normal AL but where the anterior segment shrinks disproportionately. The diagnostic criteria include corneal horizontal diameter less than 11 mm, AL longer than 20 mm, and ACD shallower than 2.20 mm without other morphological abnormalities [35]. Clinically, RAM is easily ignored, which makes the surgery relatively passive. In this study, the Km ≥ 45 D group, with a mean value of 10.89 mm in CD, normal AL, and shallow anterior chamber, was more aligned with the characteristics of RAM. Combined with our previous results, we can reasonably deduce that the extent of crowding in the anterior chamber was nearly identical across groups. Therefore, for patients with a shallow anterior chamber, even if the AL is normal and the IOL diopter is relatively routine, the narrowness of the anterior chamber reminds the surgeon to pay special attention to the safety of operation, including rational use of ultrasound, stability of the anterior chamber, and protection of the corneal endothelium while performing cataract extraction for this population.
This study has some limitations. First, only patients with age-related cataracts were included, and data from younger patients were not available. Consequently, our results are more applicable to patients with age-related cataracts. Second, due to the limitation of retrospective research, this study did not analyze the correlation between lens thickness and anterior chamber parameters, which may be conducive to understanding the mechanism of anterior chamber spatial changes. Finally, the sample size is relatively small. Further large-scale prospective studies of all ages are needed to reinforce our conclusions or identify new correlations between parameters.
Conclusions
This research demonstrates that the mean CSA of age-related cataract patients with normal AL and shallow anterior chamber is higher than that of the general population and has individual variance. Meanwhile, the CSA shows a positive correlation with corneal curvature and ACD. Additionally, the ACD increased and the CD decreased with increasing corneal curvature, while no significant change was found in ACV or ACA. Therefore, for cases with shallow and relatively crowded anterior chambers, ACV and ACA seem to be more objective in reflecting the spatial state of the anterior chamber than the ACD. Surgeons should pay particular attention to the anterior segment data preoperatively, comprehensively evaluate the ocular characteristics of patients, and conduct personalized IOL choice and treatment.
References
Afshari N. Cataract surgery: from couching to femtosecond, look how far we have come! Curr Opin Ophthalmol. 2011;22(1):1.
Lam AK, Chan R, Pang PC. The repeatability and accuracy of axial length and anterior chamber depth measurements from the IOLMaster. Ophthalmic Physiol Opt. 2001;21(6):477–83.
Ferrer-Blasco T, Domínguez-Vicent A, Esteve-Taboada JJ, Aloy MA, Adsuara JE, Montés-Micó R. Evaluation of the repeatability of a swept-source ocular biometer for measuring ocular biometric parameters. Graefes Arch Clin Exp Ophthalmol. 2017;255(2):343–9.
Nemeth G, Szalai E, Hassan Z, Lipecz A, Flasko Z, Modis L. Corneal biomechanical data and biometric parameters measured with Scheimpflug-based devices on normal corneas. Int J Ophthalmol. 2017;10(2):217–22.
Ruiz-Mesa R, Abengózar-Vela A, Ruiz-Santos M. Comparison of a new Scheimpflug imaging combined with partial coherence interferometry biometer and a low-coherence reflectometry biometer. J Cataract Refract Surg. 2017;43(11):1406–12.
He M, Huang W, Zheng Y, Alsbirk PH, Foster PJ. Anterior chamber depth in elderly Chinese: the Liwan eye study. Ophthalmology. 2008;115(8):1286-90.e1-2.
Chen H, Lin H, Lin Z, Chen J, Chen W. Distribution of axial length, anterior chamber depth, and corneal curvature in an aged population in South China. BMC Ophthalmol. 2016;16(1):47.
He M, Jiang Y, Huang S, Chang DS, Munoz B, Aung T, et al. Laser peripheral iridotomy for the prevention of angle closure: a single-centre, randomised controlled trial. Lancet. 2019;393(10181):1609–18.
Porter J, Guirao A, Cox IG, Williams DR. Monochromatic aberrations of the human eye in a large population. J Opt Soc Am A Opt Image Sci Vis. 2001;18(8):1793–803.
Thibos LN, Bradley A, Hong X. A statistical model of the aberration structure of normal, well-corrected eyes. Ophthalmic Physiol Opt. 2002;22(5):427–33.
Levy Y, Segal O, Avni I, Zadok D. Ocular higher-order aberrations in eyes with supernormal vision. Am J Ophthalmol. 2005;139(2):225–8.
Al-Sayyari TM, Fawzy SM, Al-Saleh AA. Corneal spherical aberration in Saudi population. Saudi J Ophthalmol. 2014;28(3):207–13.
Zhang M, Qian D, Jing Q, Chen J, Deng M, Jiang Y. Correlations of corneal spherical aberration with astigmatism and axial length in cataract patients. J Ophthalmol. 2019;2019:4101256.
Holladay JT, Piers PA, Koranyi G, van der Mooren M, Norrby NE. A new intraocular lens design to reduce spherical aberration of pseudophakic eyes. J Refract Surg. 2002;18(6):683–91.
Xu L, Cao WF, Wang YX, Chen CX, Jonas JB. Anterior chamber depth and chamber angle and their associations with ocular and general parameters: the Beijing Eye Study. Am J Ophthalmol. 2008;145(5):929–36.
Jonas JB, Nangia V, Gupta R, Khare A, Sinha A, Agarwal S, et al. Anterior chamber depth and its associations with ocular and general parameters in adults. Clin Exp Ophthalmol. 2012;40(6):550–6.
Fotedar R, Wang JJ, Burlutsky G, Morgan IG, Rose K, Wong TY, et al. Distribution of axial length and ocular biometry measured using partial coherence laser interferometry (IOL Master) in an older white population. Ophthalmology. 2010;117(3):417–23.
Iseli HP, Jankov M, Bueeler M, Wimmersberger Y, Seiler T, Mrochen M. Corneal and total wavefront aberrations in phakic and pseudophakic eyes after implantation of monofocal foldable intraocular lenses. J Cataract Refract Surg. 2006;32(5):762–71.
Rocha KM, Soriano ES, Chalita MR, Yamada AC, Bottós K, Bottós J, et al. Wavefront analysis and contrast sensitivity of aspheric and spherical intraocular lenses: a randomized prospective study. Am J Ophthalmol. 2006;142(5):750–6.
Fernández J, Rodríguez-Vallejo M, Burguera N, Rocha-de-Lossada C, Piñero DP. Spherical aberration for expanding depth of focus. J Cataract Refract Surg. 2021;47(12):1587–95.
Denoyer A, Denoyer L, Halfon J, Majzoub S, Pisella PJ. Comparative study of aspheric intraocular lenses with negative spherical aberration or no aberration. J Cataract Refract Surg. 2009;35(3):496–503.
He JC, Sun P, Held R, Thorn F, Sun X, Gwiazda JE. Wavefront aberrations in eyes of emmetropic and moderately myopic school children and young adults. Vision Res. 2002;42(8):1063–70.
Wang L, Dai E, Koch DD, Nathoo A. Optical aberrations of the human anterior cornea. J Cataract Refract Surg. 2003;29(8):1514–21.
Wei S, Song H, Tang X. Correlation of anterior corneal higher-order aberrations with age: a comprehensive investigation. Cornea. 2014;33(5):490–6.
Beiko GH, Haigis W, Steinmueller A. Distribution of corneal spherical aberration in a comprehensive ophthalmology practice and whether keratometry can predict aberration values. J Cataract Refract Surg. 2007;33(5):848–58.
Al-Sayyari TM, Fawzy SM, Al-Saleh AA. Corneal spherical aberration and its impact on choosing an intraocular lens for cataract surgery. Saudi J Ophthalmol. 2014;28(4):274–80.
Lai YJ, Yeh SI, Cheng HC. Distribution of corneal and ocular spherical aberrations in eyes with cataract in the Taiwanese population. Taiwan J Ophthalmol. 2015;5(2):72–5.
Shimozono M, Uemura A, Hirami Y, Ishida K, Kurimoto Y. Corneal spherical aberration of eyes with cataract in a Japanese population. J Refract Surg. 2010;26(6):457–9.
Lim KL, Fam HB. Ethnic differences in higher-order aberrations: Spherical aberration in the South East Asian Chinese eye. J Cataract Refract Surg. 2009;35(12):2144–8.
Kiuchi G, Hiraoka T, Ueno Y, Mihashi T, Oshika T. Influence of refractive status and age on corneal higher-order aberration. Vis Res. 2021;181:32–7.
Elkitkat RS, Fouad YA, Shams A, Hamza I. Normative values of corneal spherical aberration, pupil size, and other key refractive and topographic parameters in a large cohort of Egyptian cataract surgery candidates. Clin Ophthalmol. 2020;14:4571–7.
Nangia V, Jonas JB, Sinha A, Matin A, Kulkarni M, Panda-Jonas S. Ocular axial length and its associations in an adult population of central rural India: the Central India Eye and Medical Study. Ophthalmology. 2010;117(7):1360–6.
Hashemi H, Khabazkhoob M, Mohazzab-Torabi S, Emamian MH, Shariati M, Dadbin N, et al. Anterior chamber angle and anterior chamber volume in a 40- to 64-year-old population. Eye Contact Lens. 2016;42(4):244–9.
Yang N, Jin S, Ma L, Liu J, Shan C, Zhao J. The pathogenesis and treatment of complications in nanophthalmos. J Ophthalmol. 2020;2020:6578750.
Jung KI, Yang JW, Lee YC, Kim SY. Cataract surgery in eyes with nanophthalmos and relative anterior microphthalmos. Am J Ophthalmol. 2012;153(6):1161-8.e1.
Acknowledgements
The authors thank all the patients for their participation and contributions.
Funding
No funding or sponsorship was received for this study or publication of this article. The journal’s Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work and have given their approval for the version to be published.
Author Contributions
Fei Yang and Yongzhen Bao contributed to the ideas and design of study; Fei Yang collected data, performed the statistical analysis and drafted the manuscript. Yongzhen Bao reviewed and revised the manuscript. Both authors have made a substantial contribution to the work and approved it for publication.
Disclosures
Fei Yang and Yongzhen Bao declare that they have no competing interests.
Compliance with Ethics Guidelines
The studies involving human participants were reviewed and approved by Ethics Committee of Peking University international hospital (2021‐038(BMR)). The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All patients were aware of the collection of their data for this study and signed a consent form at the time of enrollment.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yang, F., Bao, Y. Correlations of Corneal Curvature with Corneal Spherical Aberration and Anterior Chamber Parameters in Eyes with Shallow Anterior Chambers. Ophthalmol Ther 12, 239–249 (2023). https://doi.org/10.1007/s40123-022-00608-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00608-6