Abstract
Introduction
This study compared the surgical outcomes in eyes with myopic foveoschisis (MF) according to the recently developed ATN classification system.
Methods
This was an observational case series of 64 consecutive eyes that underwent vitrectomy for MF. Eyes were classified into severe myopic maculopathy (MM) (n = 43) and non-severe MM (n = 21) groups according to the ATN classification system. The primary outcome measures constituted best-corrected visual acuity (BCVA) and anatomical changes.
Results
In total, BCVA improved from 0.97 to 0.53 (P < 0.001) after surgery. The ATN score was significantly lower in the eyes with vision improvement than those without vision improvement (P < 0.001). In the subgroup, BCVA improved from 0.79 to 0.28 in the non-severe MM group (P < 0.001), and improved from 1.05 to 0.65 in the severe MM group (P = 0.001) after surgery. The non-severe MM group achieved better postoperative BCVA (P = 0.001) and were more likely to gain vision improvement (P < 0.001) after surgery compared with the severe MM group. Anatomical success was achieved in 62 of the 64 eyes (96.88%). Two eyes with anatomical failure developed full-thickness macular holes postoperatively; both were in the severe MM group.
Conclusions
For patients with MF, different severity of MM based on ATN classification could lead to a significantly different prognosis after surgery. For patients with high ATN scores, the operative decision should be made cautiously for the worse anatomical and visual prognosis. ATN system is instructive in making operative proposals for MF.
Plain Language Summary
On the basis of the newly developed ATN classification system, we found significant differences in postoperative visual acuity, the rate of vision improvement, and the rate of primary retinal reattachment after vitrectomy between the severe and non-severe myopic maculopathy groups in patients with myopic foveoschisis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Vitrectomy is a proven approach to treating progressive myopic foveoschisis (MF). However, postoperative visual outcome varies greatly after anatomical resolution of the foveoschisis. |
Previous MF grading systems could not predict the postoperative outcomes well. Recently, a new classification system—the ATN system—was proposed and proven to be a reliable tool for classifying patients with myopic maculopathy. |
The present study aimed to investigate the postoperative anatomical and visual outcomes of MF based on the ATN system and to explore whether the ATN classification system is instructive in making operative proposals and judging the prognosis. |
What was learned from the study? |
On the basis of the newly developed ATN classification system, we found significant differences in postoperative structural and functional outcomes between the severe and non-severe myopic maculopathy groups in patients with myopic foveoschisis. Patients with high ATN scores were more likely to have a worse anatomical and visual prognosis. |
The ATN classification and grading system is instructive in making operative proposals and judging the prognosis for patients with MF. The operative decisions should be made cautiously for patients with high ATN scores. |
Introduction
Myopic foveoschisis (MF) is a common sight-threatening complication of pathologic myopia (PM), characterized by intraretinal splitting in the macula region. It affects 8–34% of highly myopic patients with posterior staphyloma [1, 2]. MF can be slowly progressive at the initial stage. In contrast, severe cases may develop serious complications such as foveal detachment (FD) and full-thickness macular hole (MH), leading to substantial vision impairment.
For progressive MF, pars plana vitrectomy (PPV) is a proven approach to improve macular anatomy [3]. However, postoperative visual outcome varies greatly after anatomical resolution of the foveoschisis [4,5,6]. Identifying factors that can be used to predict postoperative visual function would be clinically valuable. Previous studies [4, 6] have revealed preoperative FD, epiretinal membrane, and photoreceptor layer defects as predictive factors of poor postoperative outcomes. However, these optical coherence tomography (OCT)-based findings mainly focus on the tractional changes in MF and do not include accompanying atrophy and neovascular maculopathy. Eyes with severe atrophy and neovascular lesions are at high risk for poor visual outcomes regardless of the presence or resolution of MF.
Recently, Ruiz-Medrano et al. [7] proposed a new classification system—the ATN system—to assess myopic maculopathy (MM), which integrated atrophy (A), traction (T), and neovascularization (N) components. This new classification system has been proven to be an accurate and reliable tool for classifying patients with PM [8, 9]. Although many studies have analyzed the surgical outcomes of MF based on OCT, no research has been conducted to comprehensively analyze the surgical outcomes based on the ATN classification system. The present study aimed to investigate the postoperative anatomical and visual outcomes of MF based on the ATN system and to explore whether the ATN classification system is instructive in making operative proposals and judging the prognosis.
Methods
This study involved human participants and was approved by the Institutional Review Board of Shenzhen Eye Hospital (Shenzhen, China), and was conducted in accordance with the World Medical Association Declaration of Helsinki. The medical records of patients with MF who underwent vitrectomy and perfluoropropane tamponade performed by a single surgeon (SZ) between January 2012 and January 2022 were retrospectively reviewed. The surgical indication was when the patient’s vision decreased even after full correction or when the patient complained of metamorphopsia with corresponding changes on the OCT. Exclusion criteria were (1) eyes with any associated or concomitant retinopathy that could confound the retinal interpretation of OCT images and fundus photographs; (2) unclear image of OCT, which was defined as insufficient visualization of the retinal pigment epithelium line in the macular area; (3) patients with a postoperative follow-up period less than 6 months; (4) patients who exhibited MF with MH and/or macular hole retinal detachment were excluded because it is right to operate unconditionally in such cases. As a result, 64 eyes of 56 consecutive patients were ultimately included in this study.
All the surgeries were done under retrobulbar or general anesthesia. All eyes underwent 25-gauge transconjunctival pars plana vitrectomy. After core vitrectomy, the manual posterior vitreous detachment was induced. The internal limiting membrane (ILM) was stained with 0.1 ml of indocyanine green solution at a concentration of 0.5%. If epiretinal membrane was present, it was removed first; then the ILM was peeled entirely within the vascular arcades. Finally, fluid–air exchanges were performed, followed by 16% perfluoropropane tamponade. After surgery, all the patients were told to keep a face-down position for more than 2 weeks.
All patients underwent a comprehensive ophthalmological examination, including refractometry using an autorefractor (KR-8800, Topcon, Tokyo, Japan), IOL Master (Carl Zeiss Meditec, Jena, Germany), fundus photographs (Visucam, Carl Zeiss Meditec, Jena, Germany) or ultrawide-field imaging (Optomap 200Tx, Optos pls), and OCT. OCT images were obtained with a spectral-domain OCT (Spectralis OCT; Heidelberg Engineering GmbH, Heidelberg, Germany; Optovue Inc., Fremont, California, USA). Vertical and horizontal scans, passing through the center of the fovea and radial scans, covering all the macular complications, were obtained in each eye. All data were fully anonymized before access by our researchers. Two experienced retinal specialists (SZ and LC) read all the OCT images, and agreement by the two specialists was needed to determine the severity of MM. Another specialist would be enrolled if there was disagreement, and a diagnosis was provided according to the majority rule.
The ATN classification system was adopted to compare clinical outcomes in the present study. This grading system includes three myopic alterations: the atrophic component (A), the tractional component (T), and the neovascular component (N) (Table 1). Patients were considered to present severe MM if either A or T components were ≥ 3 and/or N was ≥ 2; others were classified as non-severe MM [8]. Anatomical success was defined as complete foveal reattachment and the absence of foveoschisis. Among them, eyes with well-attached retina without retinoschisis after surgery were classified as “primary retinal reattachment,” and eyes with extrafoveal or perivascular retinoschisis without aggravation were classified as “secondary retinal reattachment.” Eyes that displayed either aggravated foveoschisis or postoperative development of MH or FD were defined as anatomical failure. A postoperative gain or loss of at least two lines of best corrected visual acuity (BCVA) (0.3 logMAR units) was considered improvement or deterioration; otherwise it was defined as stable vision.
Snellen visual acuity (VA) was converted to the logarithm of the minimum angle of resolution (logMAR). Hand motion and counting fingers were converted into logMAR 2.3 and logMAR 2.0 according to previous studies [10, 11]. Continuous variables between severe and non-severe MM groups were compared using independent sample t tests or Mann–Whitney U tests. One-way analysis of variance (ANOVA) or the Kruskal–Wallis test was used to compare the clinical characteristics among the different grades of MM. Multiple comparisons between different groups were adjusted by the Bonferroni test. Analysis of the BCVA changes before and after surgery was performed using paired t test. A P value of less than 0.05 was considered statistically significant. All data were analyzed using the SPSS 19.0 software (SPSS Inc., Chicago, IL, USA).
Results
Clinical Characteristics and Surgical Outcomes of the Whole Cohort
A total of 64 eyes of 56 consecutive patients with MF were enrolled. Baseline characteristics of the study population are summarized in Table 2. The patients comprised 32 women and 24 men with a mean age of 53.00 ± 11.00 years old, ranging from 25 to 76 years old. The mean axial length was 29.37 ± 1.69 mm, ranging from 26.34 to 33.22 mm. The mean follow-up period was 34.17 ± 19.58 months. Before surgery, most of the eyes (84.38%) were phakic. Among the 54 phakic eyes, 49 underwent cataract surgery with vitrectomy or after vitrectomy due to cataract progression during the follow-up period; five did not (non-severe MM, n = 2; severe MM, n = 3). Spherical equivalent of preoperative refractive errors in phakic eyes were − 14.83 ± 5.13 diopters (D) (range − 32.00 to − 7.00 D).
Among the total population, there was significant BCVA improvement after surgery (preoperative 0.97 ± 0.57; postoperative 0.53 ± 0.44; P < 0.001). Vision improvement was achieved in 37 of 64 eyes (57.81%). Central retinal thickness (CFT) also showed a significant reduction (preoperative CFT 573.54 ± 250.18 mm to postoperative CFT 122.05 ± 48.70 mm, P < 0.001). Anatomical success was achieved in 62 of the 64 eyes (96.88%), of which 41 eyes achieved primary retinal reattachment and 21 eyes achieved secondary retinal reattachment. The two eyes with anatomical failure developed full-thickness MH postoperatively.
Surgical Outcomes According to the ATN Classification System
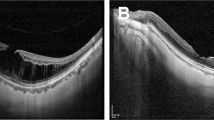
Mean ATN grades for each component were as follows: ATN = 5.11 ± 1.35 (2.00–8.00), A = 1.95 ± 0.79 (1.00–4.00), T = 2.31 ± 0.81 (1.00–3.00), and N = 0.84 ± 0.44 (0.0–2.0). Significantly lower ATN scores were found in the eyes with vision improvement than those without vision improvement (4.54 ± 1.28 vs. 5.89 ± 1.01, P < 0.001). Similarly, eyes with primary retinal reattachment got lower ATN scores than those without primary retinal reattachment (4.80 ± 1.40 vs. 5.65 ± 1.07, P = 0.019). Representative images of MF eyes in this study according to the ATN classification system are shown in Fig. 1.
Representative images of myopic foveoschisis by corresponding ATN categories. Each column consists of preoperative fundus photographs (A1–E1), preoperative optical coherence tomography (OCT) scans (A2–E2), and postoperative OCT scans (A3–E3) of the same person. First row, fundus of the right eye of a 53-year-old woman with an axial length of 28.80 mm (A1T2N1). Fundus photograph (A1) showed a tessellated fundus with lacquer cracks (LCs) in the macular area; preoperative OCT image (A2) revealed inner and outer retinoschisis; and postoperative OCT image (A3) revealed anatomically satisfactory restoration 12 months after surgery. The best corrected visual acuity (BCVA) improved from 0.4 to 0.8 (Snellen). Second row, fundus of the left eye of a 62-year-old woman with an axial length of 31.60 mm (A2T3N1). Fundus photograph (B1) revealed diffuse chorioretinal atrophy with LCs in the edge of chorioretinal atrophy; preoperative OCT image (B2) displayed foveal retinal detachment, vitreomacular traction, and inner lamellar hole; postoperative OCT image (B3) showed completely retinoschisis resolution 25 months after surgery, the inner surface remained unsmooth even after a long time after surgery. The BCVA improved from 0.3 to 0.7 (Snellen). Third row, fundus of the right eye of a 55-year-old woman with an axial length of 26.34 mm (A3T3N1). Patchy chorioretinal atrophy with LCs in macula was noted on the fundus photograph (C1); preoperative OCT image (C2) showed extensive foveal retinal detachment with posterior vitreous detachment. Postoperative OCT image (C3) revealed completely retinoschisis resolution 27 months after surgery. The BCVA improved from 0.15 to 0.4 (Snellen). Fourth row, fundus of the left eye of a 55-year-old woman with an axial length of 31.70 mm (A3T3N1). Fundus photograph (D1) revealed patchy chorioretinal atrophy at the edge of posterior staphyloma. Around the lesion was diffuse chorioretinal atrophy. Preoperative OCT image (D2) showed foveal retinal detachment, vitreomacular traction, and inner lamellar hole. Twenty-three months after vitrectomy, OCT (D3) revealed that the central part of the macula was well attached. Still, retinoschisis remained on the edge of posterior staphyloma, i.e., where the patchy chorioretinal atrophy was located. The BCVA improved from 0.2 to 0.3 (Snellen). Fifth row, fundus of the left eye of a 48-year-old woman with an axial length of 31.32 mm (A4T3N1). Fundus photograph (E1) revealed macular atrophy at baseline. Around the lesion was patchy chorioretinal atrophy. Preoperative OCT image (E2) showed tractional retinal detachment. The sclera was bowed posteriorly. Thirty-seven months after surgery, OCT (E3) revealed that macular hole developed, which is one of two cases with anatomical failure in the enrolled group. The BCVA decreased from 0.1 to 0.05 (Snellen)
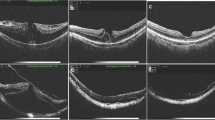
There were 43 (67.19%) eyes in the severe MM group and 21 (32.81%) in the non-severe MM group. The non-severe MM group exhibited BCVA improvement from 0.79 ± 0.47 to 0.28 ± 0.18 (P < 0.001), whereas the severe MM group exhibited BCVA improvement from 1.05 ± 0.60 to 0.65 ± 0.48 (P < 0.001). The postoperative BCVA of the severe MM group was inferior to that of the non-severe MM group (P = 0.001). The proportion of patients with vision improvement was 90.48% in the non-severe MM group, whereas it was only 41.86% in the severe MM group (P < 0.001) (Table 2, Fig. 2).
Postoperative structural and functional outcomes of non-severe myopic maculopathy (MM) and severe MM group. A Different postoperative logMAR BCVA between two groups (0.28 ± 0.18 vs. 0.65 ± 0.48, P = 0.001). B Different postoperative CFT between two groups (139.81 ± 51.73 vs. 113.38 ± 45.26, P = 0.057). C Changes of BCVA after surgery compared to baseline in two groups (90.48%, 9.52%, 0% vs. 41.86%, 55.81%, 2.33%, P < 0.001). D Different postoperative anatomical outcome between two groups (85.71%, 14.29%, 0% vs. 53.49%, 41.86%, 4.65%, P = 0.029). MM myopic maculopathy, Post-op postoperative, BCVA best corrected visual acuity, CFT central foveal thickness, logMAR logarithm of the minimum angle of resolution. Asterisk denotes statistical significance at P < 0.05
A subgroup analysis yielded no statistically significant difference in axial length, preoperative CFT, postoperative CFT, and CFT changes between the non-severe MM and severe MM groups (P = 0.823, P = 0.121, P = 0.057, P = 0.055) (Table 2). In terms of postoperative anatomical prognosis, anatomical success was achieved in 21 of 21 eyes (100%) in the non-severe MM group, among which 18 eyes (85.71%) achieved primary retinal reattachment and 3 eyes (14.29%) achieved secondary reattachment. In the severe MM group, 41 of 43 (95.35%) eyes achieved anatomical success, among which 23 eyes (53.49%) achieved primary retinal reattachment and 18 eyes (41.86%) achieved secondary reattachment. The difference was statistically significant in the primary retinal reattachment rate (P = 0.029) but not significant in the rate of anatomical success (P = 1.00) between the two groups (Fig. 2). There were two eyes with anatomical failure; both were in the severe MM group, with MH that developed after surgery. Preoperatively, both cases exhibited FD with severe atrophy fundus (A3/A4).
Surgical Outcomes According to the Tractional Component (T)
In terms of tractional component, there were 14 (21.88%) eyes in T1, 16 (25.00%) in T2, and 34 (53.13%) in T3 (Table 3). For each subgroup, postoperative CFT was significantly reduced compared with preoperative CFT (383.09 ± 151.18 vs. 150.79 ± 61.17, P < 0.001; 604.89 ± 220.88 vs. 117.78 ± 33.77, P < 0.001; 637.21 ± 261.29 vs. 112.23 ± 45.57, P < 0.001). Postoperative BCVA was significantly improved compared with preoperative BCVA (0.88 ± 0.64 vs. 0.51 ± 0.43, P = 0.012; 0.83 ± 0.52 vs. 0.45 ± 0.49, P = 0.003; 1.07 ± 0.57 vs. 0.58 ± 0.43, P < 0.001) in each group.
Preoperative CFT became significantly thicker with the increasing severity of MF in T1–T3 (P = 0.002). With surgery, the changes in CFT increased dramatically with the increasing severity of MF in T1–T3 (P = 0.001). However, the differences were not significant in postoperative BCVA (P = 0.301), the proportion of vision improvement (P = 0.155), the ratio of anatomical success (P = 0.105), and primary retinal reattachment (P = 0.058) between the eyes with different T grades (Table 3).
Surgical Outcomes According to the Atrophic Component (A)
In terms of atrophic component, there were 21 (32.81%) eyes in A1, 25(39.06%) in A2, 15 (23.44%) in A3, and 3 (4.69%) in A4 (Table 4). As a result of the limited cases in the A4 group, we combined A3 and A4 groups for statistical analysis. For each subgroup, postoperative CFT was evidently reduced compared with preoperative CFT (552.37 ± 224.89 vs. 144.14 ± 53.00, P < 0.001; 629.89 ± 301.42 vs. 122.76 ± 35.84, P < 0.001; 519.97 ± 189.56 vs. 95.31 ± 48.06, P < 0.001). Postoperative BCVA was significantly improved compared with preoperative BCVA in A1 and A2 (0.83 ± 0.58 vs. 0.31 ± 0.37, P < 0.001; 0.91 ± 0.45 vs. 0.41 ± 0.24, P < 0.001). However, no significant difference was found between preoperative and postoperative BCVA in A3/A4 (1.19 ± 0.66 vs. 0.95 ± 0.46, P = 0.443).
With the increasing severity of MAM in A1–A3/A4, axial length increased (P = 0.017), and refractive error became more myopic (P = 0.013). The preoperative BCVA gradually decreased with the increasing severity of MAM in A1 to A3/A4. However, the difference was not significant (0.83 ± 0.58, 0.91 ± 0.45, 1.19 ± 0.66; P = 0.120). After surgery, CFT became evidently thinner, and BCVA became significantly worse with the increasing severity of MAM in A1–A3/A4 (P = 0.013, P < 0.001). Statistically, a significant difference was yielded in the proportion of vision improvement between different grades of MAM (76.19%, 72.00%, 16.67%; P < 0.001). No significant difference was found in anatomical success (P = 0.076) or primary retinal reattachment (P = 0.139) among different MAM grades (Table 4).
For the neovascular component, the majority were in N1, presenting lacquer cracks in the macula (50 eyes, 78.13%). There were 12 eyes (18.75%) without myopic choroidal neovascularization (CNV) (N0), and only two cases presented CNV scar (N2s). There was no case with active CNV (N2a).
Discussion
To the best of our knowledge, this work is the first study to investigate the surgical outcomes in patients with MF using the newly developed ATN classification system. On the basis of the ATN classification system, the eyes were divided into severe and non-severe MM groups in the current study. The non-severe MM group achieved better BCVA and was more likely to improve vision after surgery than the severe MM group. Moreover, eyes with vision improvement got significantly lower ATN scores than those without vision improvement, and eyes with primary retinal reattachment achieved lower ATN scores than those without. These findings suggest that for patients with MF who require surgical treatment, different severity of MM based on ATN classification could lead to a significantly different prognosis after surgery. ATN classification system is instructive in making operative proposals and judging the prognosis.
As the gold standard for diagnosing MF, OCT has long been the primary tool for assessing clinical severity and the prognosis. Recently, Parolini et al. [12,13,14,15,16,17] proposed a new myopic traction maculopathy staging system based on OCT, which provided practice diagnostic and management strategies for MF. However, taking accompanying atrophy and neovascular maculopathy into consideration on the basis of OCT changes could better account for the numerous macular changes of MF [5, 18,19,20]. To comprehensively evaluate myopic MM, Ruiz-Medrano [7] proposed the ATN classification system that integrates these three factors. Previous studies [8, 9] proved that the ATN system is an accurate and reliable tool to classify patients with PM for its excellent interobserver rate and high reproducibility. However, the ATN system has not been used to assess postoperative outcomes in MF. The present research revealed significant differences in postoperative visual acuity, the rate of vision improvement, and the rate of primary retinal reattachment between the severe and non-severe MM groups based on ATN scores. Moreover, eyes with worse postoperative anatomical or functional outcomes achieved significantly lower ATN scores at baseline. Thus, it is essential to comprehensively assess MM based on the ATN system before surgical intervention. For patients with high ATN scores, the operative decision should be made with caution because of the worse anatomical and visual outcomes.
In the present study, two cases developed MH after surgery. Both cases came from the severe MM group and presented a high ATN score at baseline, which displayed FD with severe atrophy fundus before surgery. Similarly, Huang et al. [21] found that preoperative FD is a risk factor for the development of MH retinal detachment after vitrectomy for MF. The outcome may suggest that patients with FD are more vulnerable to surgical trauma such as ILM peeling and are more likely to develop MH postoperatively. For these cases, fovea-sparing ILM peeling might help reduce the risk of postoperative complications, and intraoperative OCT can be a practical tool for intraoperative observation.
In 2015, Ohno-Matsui et al. [22] performed the international META analysis for PM and proposed a grading system. The ATN system adopted this atrophy-centered system as the atrophy component. Kim et al. [23] found that atrophy MM severity was correlated with postoperative BCVA for MF. Similarly, we found that with the increasing severity of atrophy MM, the postoperative central foveal thickness became thinner, and the postoperative BCVA became worse. The proportion of vision improvement was significantly lower in A3/A4 compared with A1 and A2. However, no difference was found in the proportion of foveoschisis resolution among different grades of atrophy MM. In these cases, the critical factor that limited postoperative functional outcomes was the atrophy component rather the tractional component like foveaschisis. The preoperative traction can be resolved after surgery, whereas the preoperative atrophy cannot be corrected by surgery, resulting in poor vision improvement potential. ln the ATN system, the tractional components were divided into six grades: no macular schisis (T0); inner or outer foveoschisis (T1); inner and outer foveoschisis (T2); FD (T3); full-thickness MH (T4); and MH retinal detachment (T5). Among different grades of T component, we found no evident difference in postoperative BCVA, the proportion of vision improvement, and the proportion of anatomical success. However, previous studies [19] reported that eyes with FD had much worse postoperative BCVA than eyes without FD. The inconsistency between different studies might result from uncontrolled confounding factors like atrophy MM. Further research with controlled confounding factors and a larger sample size is warranted.
There are some limitations in our study. First, subgroup analysis of the neovascular components was not conducted here. In our research, most of the cases (78.13%) presented macular lacquer cracks (N1), only two cases of CNV scar (N2s), and there was no active CNV. The uneven data distribution limited further analysis. Further investigations would be required to explore the role of neovascular components in MF surgical outcomes. Second, the sample size of the current study is relatively small. To minimize bias associated with surgical procedures, we enrolled cases operated on by a single skilled surgeon. However, this would also result in a relatively small sample size. Research with a larger sample size would have provided more substantial statistical power for analysis.
Conclusion
The present study is the first to adopt the new ATN classification system to assess the surgical outcomes of MF. For patients with MF who require surgical treatment, different severity of MM could lead to a significantly different prognosis after surgery. The operative decisions should be made cautiously for patients with high ATN scores because of the worse anatomical and visual prognosis and higher possibility of MH development in these cases. It is imperative to incorporate all three types of MM before surgical intervention, providing dependable guidance in hierarchical management and prognosis evaluation for MF.
References
Baba T, Ohno-Matsui K, Yoshida T, et al. Optical coherence tomography of choroidal neovascularization in high myopia. Acta Ophthalmol Scand. 2002;80:82–7.
Baba T, Ohno-Matsui K, Futagami S, et al. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol. 2003;135:338–42.
Rizzo S, Giansanti F, Finocchio L, et al. Vitrectomy with internal limiting membrane peeling and air tamponade for myopic foveoschisis. Retina. 2019;39:2125–31.
Shin JY, Yu HG. Visual prognosis and spectral-domain optical coherence tomography findings of myopic foveoschisis surgery using 25-gauge transconjunctival sutureless vitrectomy. Retina. 2012;32:486–92.
Lee DH, Moon I, Kang HG, et al. Surgical outcome and prognostic factors influencing visual acuity in myopic foveoschisis patients. Eye (Lond). 2019;33:1642–8.
Lim LS, Ng WY, Wong D, et al. Prognostic factor analysis of vitrectomy for myopic foveoschisis. Br J Ophthalmol. 2015;99:1639–43.
Ruiz-Medrano J, Montero JA, Flores-Moreno I, Arias L, Garcia-Layana A, Ruiz-Moreno JM. Myopic maculopathy: current status and proposal for a new classification and grading system (ATN). Prog Retin Eye Res. 2019;69:80–115.
Ruiz-Medrano J, Flores-Moreno I, Ohno-Matsui K, Cheung CMG, Silva R, Ruiz-Moreno JM. Validation of the recently developed ATN classification and grading system for myopic maculopathy. Retina. 2020;40:2113–8.
Ruiz-Medrano J, Flores-Moreno I, Ohno-Matsui K, Cheung CMG, Silva R, Ruiz-Moreno JM. Correlation between atrophy-traction-neovascularization grade for myopic maculopathy and clinical severity. Retina. 2021;41:1867–73.
Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities “hand motion” and “counting fingers” can be quantified with the freiburg visual acuity test. Invest Ophthalmol Vis Sci. 2006;47:1236–40.
Lange C, Feltgen N, Junker B, Schulze-Bonsel K, Bach M. Resolving the clinical acuity categories “hand motion” and “counting fingers” using the Freiburg Visual Acuity Test (FrACT). Graefes Arch Clin Exp Ophthalmol. 2009;247:137–42.
Palmieri M, Frisina R, Finzi A, Besozzi G, Parolini B. The role of the outer lamellar macular hole in the surgical management of myopic traction maculopathy. Ophthalmologica. 2021;244:229–36.
Parolini B, Palmieri M, Finzi A, Frisina R. Proposal for the management of myopic traction maculopathy based on the new MTM staging system. Eur J Ophthalmol. 2021;31:3265–76.
Parolini B, Palmieri M, Finzi A, et al. The new myopic traction maculopathy staging system. Eur J Ophthalmol. 2021;31:1299–312.
Frisina R, Gius I, Palmieri M, Finzi A, Tozzi L, Parolini B. Myopic traction maculopathy: diagnostic and management strategies. Clin Ophthalmol. 2020;14:3699–708.
Parolini B, Palmieri M, Finzi A, Besozzi G, Frisina R. Myopic traction maculopathy: a new perspective on classification and management. Asia Pac J Ophthalmol (Phila). 2021;10:49–59.
Frisina R, Besozzi G, Finzi A, Pinackatt SJ, Palmieri M, Parolini B. Inter-observer and intra-observer reliability of the myopic traction maculopathy staging system. Eur J Ophthalmol. 2022;32:1577–83.
Dolar-Szczasny J, Swiech-Zubilewicz A, Mackiewicz J. A review of current myopic foveoschisis management strategies. Semin Ophthalmol. 2019;34:146–56.
Hattori K, Kataoka K, Takeuchi J, Ito Y, Terasaki H. Predictive factors of surgical outcomes in vitrectomy for myopic traction maculopathy. Retina. 2018;38(Suppl 1):S23-s30.
Ohno-Matsui K, Wu PC, Yamashiro K, et al. IMI pathologic myopia. Invest Ophthalmol Vis Sci. 2021;62:5.
Huang Y, Huang W, Ng DSC, Duan A. Risk factors for development of macular hole retinal detachment after pars plana vitrectomy for pathologic myopic foveoschisis. Retina. 2017;37:1049–54.
Ohno-Matsui K, Kawasaki R, Jonas JB, et al. International photographic classification and grading system for myopic maculopathy. Am J Ophthalmol. 2015;159:877-83.e7.
Kim CY, Kim MS, Kim KL, Woo SJ, Park KH. Prognostic factors related with surgical outcome of vitrectomy in myopic traction maculopathy. Korean J Ophthalmol. 2020;34:67–75.
Acknowledgements
Funding
Supported by the Natural Science Foundation of Guangdong Province (2021A1515011090), the Shenzhen Outstanding Science and Technology Innovation Talents Training Program (RCBS20210706092347043), the Sanming Project of Medicine in Shenzhen (SZSM202011015), Shenzhen Science and Technology Program (KCXFZ20211020163813019) and the National Natural Science Foundation of China (81900877). The journal’s Rapid Service Fee was funded by the Sanming Project of Medicine in Shenzhen (SZSM202011015).
Authorship
All authors conform to the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, account for the integrity of the whole work, and have approved the version to be published.
Author Contributions
Dong Fang contributed to the study design and wrote the manuscript; Jia Liang contributed to the clinical data collection, data analyses and manuscript polishing; Sheng Chen and Canfeng Huang assisted in clinical data collection; Kunke Li and Xingxing Mao contributed to the manuscript preparation; Xiaofeng Hou and Ting Xie assisted in data analyses; Pengxue Wei assisted in article revision. Lu Chen contributed to the conception of the study, study design and manuscript polishing; Shaochong Zhang contributed to the conception, design, data acquisition, writing, statistical analysis, interpretation of data, original draft preparation. All authors read and approved the final manuscript.
Disclosures
All named authors confirm that they have no financial or conflicting interests to disclose.
Compliance with Ethics Guidelines
Ethics approval for this study was granted by the Institutional Review Board of Shenzhen Eye Hospital (Shenzhen, China). All data were anonymized prior to the analysis. The research adhered to the principles of the Declaration of Helsinki and its later amendments.
Data Availability
Dong Fang and Jia Liang had full access to all the data in the research and account for the integrity of the data and the accuracy of the data analysis. The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fang, D., Liang, J., Chen, S. et al. Surgical Outcomes of Myopic Foveoschisis According to the ATN Classification System. Ophthalmol Ther 12, 71–85 (2023). https://doi.org/10.1007/s40123-022-00582-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00582-z