Abstract
Introduction
The aim of this nationwide, prospective post-marketing surveillance was to assess the safety and effectiveness of up to 52 weeks of adalimumab treatment in patients with noninfectious intermediate, posterior, or panuveitis in Japanese clinical practice.
Methods
This post-marketing surveillance was conducted at 60 medical facilities in Japan from October 2016 to June 2020. Patients with noninfectious intermediate, posterior, or panuveitis who were administered adalimumab (Humira®, AbbVie Inc.) for the first time were eligible. Subcutaneous adalimumab was initially administered at 80 mg, followed by 40 mg 1 week later, then 40 mg every 2 weeks. Safety measures included the incidence of adverse events (AEs) and adverse drug reactions (ADRs; primary endpoint). Effectiveness measures included visual acuity, anterior chamber cell grade, vitreous haze, macular edema, foveal retinal thickness, uveitis recurrence rate, and oral corticosteroid dose. Health-related quality of life was evaluated using the 25-item National Eye Institute Visual Function Questionnaire (VFQ-25).
Results
During 52 weeks of surveillance, AEs and ADRs occurred in 70 (27.9%) and 47 (18.7%) of 251 patients, respectively. The most common ADR was infection (21/251 patients; 8.4%), including serious infections in eight (3.2%) patients. ADRs were more frequent in patients ≥ 65 years of age, those with concurrent diseases, and those with past medical history. Four patients developed tuberculosis. The uveitis recurrence rate was 24.8% (61/246 patients). All effectiveness measures tended to improve from baseline to week 52, and mean corticosteroid doses decreased. Clinically meaningful changes were observed for most VFQ-25 subscales.
Conclusions
The safety profile of adalimumab was generally consistent with previous reports, and no new safety concerns were identified.
Trial registration
ClinicalTrials.gov: NCT02916017.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Adalimumab is an anti-tumor necrosis factor-α monoclonal antibody approved for the treatment of noninfectious intermediate, posterior, or panuveitis; however, the long-term use of adalimumab in routine clinical practice needs to be evaluated prospectively in nationwide studies involving large numbers of patients. |
This nationwide, prospective post-marketing surveillance study was conducted to assess the safety and effectiveness of up to 52 weeks of adalimumab treatment in 251 patients with noninfectious intermediate, posterior, or panuveitis in Japanese clinical practice. |
What was learned from the study? |
The safety profile of adalimumab was similar to that reported in clinical trials and in smaller, retrospective real-world studies, sustained improvements in uveitis symptoms and quality of life were achieved, and a corticosteroid-sparing effect was observed. |
These results support the long-term use of adalimumab in Japanese patients with noninfectious uveitis. |
Introduction
Noninfectious uveitis, which is common in Japan [1], is an ocular inflammatory condition associated with a number of systemic immune disorders, including sarcoidosis, Vogt-Koyanagi-Harada (VKH) disease, and Behçet’s disease [2, 3]. Chronic inflammation from uveitis damages ocular structures and threatens vision, especially in patients with panuveitis. The standard initial treatment for noninfectious uveitis is oral or intravenous corticosteroids; however, long-term use of corticosteroids in patients with recurring uveitis can lead to serious side effects [4, 5]. Once inflammation subsides, corticosteroid doses can be tapered. In patients who experience recurrent flares after corticosteroid tapering or who require long-term control of inflammation, addition of immunosuppressants can further control inflammation without increasing the corticosteroid dose (“corticosteroid-sparing”) [2, 4, 5]. However, some patients become refractory to or intolerant of corticosteroid and immunosuppressant therapy or have uveitis such as Behçet’s disease where immediate use of immunosuppressants is warranted; for these patients, biologic drugs provide a molecularly targeted therapy as an effective, corticosteroid-sparing alternative [6].
Inhibitors of the proinflammatory cytokine tumor necrosis factor-α (TNF-α) are a major class of biologic drugs used to control inflammation in a range of diseases, including noninfectious uveitis. For example, the anti-TNF-α monoclonal antibody infliximab has been shown to suppress ocular inflammatory attacks in patients with Behçet’s disease [7]. Adalimumab is a fully human anti-TNF-α monoclonal antibody that was approved for the treatment of noninfectious intermediate, posterior, or panuveitis in 2016 [8], including in Japan. Two global, randomized, placebo-controlled trials established the safety and efficacy of adalimumab for active (VISUAL I) and inactive (VISUAL II) noninfectious uveitis [9, 10]. In both trials, adalimumab significantly reduced the risk of treatment failure (a composite outcome based on changes in visual acuity, anterior chamber cell grade, and vitreous haze grade, and the appearance of new retinal lesions) compared with placebo [9, 10]. Adverse events (AEs) in the adalimumab group were consistent with those observed for other indications, although VISUAL I reported a higher incidence of AEs with adalimumab than placebo, mainly due to injection site reactions. However, a small number of cases of tuberculosis and malignancy were noted in both trials, consistent with the known effects of TNF-α inhibitors on opportunistic infections [11, 12] and the potential risk for their influence on malignancies [8].
The long-term (150 weeks) safety and efficacy of adalimumab were confirmed in VISUAL III, an open-label extension study of VISUAL I and II [13]. Although the long-term use of adalimumab (or a biosimilar) in routine clinical practice has been evaluated in mainly retrospective studies conducted at ≤ 5 medical centers [14,15,16,17,18,19,20,21], larger, nationwide, prospective studies are needed. Such studies would include patients with complex treatment and medical histories who would have been excluded from clinical trials. In addition, it is important to assess the safety of adalimumab in Japan, where tuberculosis is more common than in most European and North American countries [22]. This nationwide, prospective post-marketing surveillance study was conducted to assess the safety and effectiveness of up to 52 weeks of adalimumab treatment in patients with noninfectious intermediate, posterior, or panuveitis in Japanese clinical practice.
Methods
Study Design
This was an open-label, noncontrolled, multicenter, post-marketing surveillance conducted at 60 medical facilities in Japan from October 2016 to June 2020 (ClinicalTrials.gov identifier: NCT02916017). The surveillance was conducted in accordance with Good Post-marketing Study Practices for Drugs, and Japanese regulatory and legal requirements. The protocol was approved by the Pharmaceuticals and Medical Devices Agency of Japan. Patients provided written informed consent before any surveillance-specific procedures.
Study Population
Patients who were diagnosed with noninfectious intermediate uveitis, posterior uveitis, or panuveitis and who were administered adalimumab (Humira®, AbbVie Inc.) for the first time were eligible to register for this surveillance.
Treatment Protocol
Patient registration was managed by a central registration system (EPS Corporation, Tokyo, Japan). Patients received adalimumab by subcutaneous injection at 80 mg as an initial dose, followed by 40 mg 1 week later, and then 40 mg once every 2 weeks. As recommended by the Japanese Ocular Inflammation Society [23], patients were screened for serious infections, including tuberculosis and hepatitis B infection, before being administered adalimumab. The surveillance consisted of a 52-week treatment period (observational period). Patients who discontinued during the treatment period were observed until discontinuation; patients who had AEs were followed for up to 70 days after discontinuation. All data were entered into an electronic data capture system (Fujitsu FIP Corporation, now Fujitsu Japan Limited, Tokyo, Japan) by the investigators.
Outcome Measures
Information about patient demographics, disease characteristics (including primary disease underlying uveitis), medical history (including any concurrent diseases present at the time of first adalimumab administration and past medical history [diseases, conditions, procedures, etc.] that is no longer present at the time of first adalimumab administration), and treatment history was collected. Safety was evaluated by the incidence of AEs and adverse drug reactions (ADRs; primary endpoint). AEs were coded using version 23.0 of the Medical Dictionary for Regulatory Activities/Japanese version (MedDRA/J). ADRs were defined as AEs for which a causal relationship with adalimumab could not be ruled out. The incidence of ADRs was also assessed in subgroups of patients with sarcoidosis, VKH disease, and Behçet’s disease, which are three of the most common diseases underlying noninfectious uveitis in Japan [1]. Following the risk management plan for adalimumab, incidence rates of ADRs of interest and other important potential risks were assessed. ADRs of interest were specified from safety results of clinical studies and post-marketing surveillance studies in noninfectious uveitis and other indications and included infections, hepatitis B reactivation, tuberculosis, demyelinating diseases, lupus-like syndromes, serious allergic reactions, interstitial pneumonia, serious blood disorders, and fulminant hepatitis/liver disorders/jaundice/hepatic failure. Important potential risks are adverse events that are suspected to be related to adalimumab but that lack sufficient clinical data to be confirmed; these include malignancy, psoriasis or psoriasis aggravation, and sarcoidosis deterioration.
Effectiveness was evaluated at pre-dose (except uveitis recurrence rate) and all examination time points from treatment start (week 0) to week 52 or discontinuation. Effectiveness outcomes included visual acuity, anterior chamber cell grade by slit-lamp microscopy (Standardization of Uveitis Nomenclature [SUN] criteria [24]), vitreous haze by indirect ophthalmoscopy (National Eye Institute [25]/SUN working group [26] criteria), macular edema and foveal retinal thickness by optical coherence tomography, recurrence rate of uveitis, and oral corticosteroid dose as prednisolone equivalent.
Health-related quality of life (HR-QoL) was evaluated using the 25-item National Eye Institute Visual Function Questionnaire (VFQ-25; [27]) at pre-dose and week 52 or discontinuation. The VFQ-25 consists of 25 items in 12 subscales. Each item is assessed on a Likert scale from 0 to 100, with higher scores indicating better HR-QoL. Individual item scores are averaged to obtain subscale and total composite scores. Changes of approximately 4 points in the total score and 4–6 points in subscale scores have been suggested to be clinically meaningful [28].
Statistical Analysis
A target sample size of 250 patients was set to provide at least 216 patients for the safety analysis, accounting for patient withdrawals, assuming an incidence rate of serious infections of approximately 2.3% (95% confidence interval ± 2.0%) based on previous safety data. All patients who met registration criteria were included in the safety analysis set. Of these, patients in whom effectiveness was evaluated at least once were included in the effectiveness analysis set. Data are summarized as numbers and percentages for categorical variables and mean ± standard deviation (SD) for continuous variables. Missing data were not imputed. A chi-square test was used to compare incidence rates between patient subgroups. Effectiveness outcomes are presented as descriptive statistics at baseline and last observation. Statistical analyses were performed using SAS® version 9.2 or later (SAS Institute, Cary, NC, USA).
Results
Patient Disposition and Characteristics
Of 259 patients registered, case report forms were collected for 256 patients; 251 and 246 patients were included in the safety and effectiveness analysis sets, respectively (Fig. 1). Of 251 patients, 199 (79.3%) completed the 52-week treatment period and 52 (20.7%) discontinued participation. The most common reasons for discontinuation were AEs (n = 19), hospital transfer or not visiting a hospital (n = 13), lack of effectiveness (n = 8), and symptom improvement (n = 6).
Most patients were female (61.0%), aged from 40 to 64 years (49.8%), and had concurrent diseases (55.0%); 22.7% had a past medical history (Table 1). The most common primary diseases were Behçet’s disease (27.5%), VKH disease (25.5%), and sarcoidosis (11.6%); 22.3% of patients had idiopathic noninfectious uveitis. A small percentage of patients (12.0%) had received previous treatment with infliximab; in contrast, most patients (94.8%) had been treated with other medications (Table 1). Approximately half (55.0%) of patients had at least one concurrent disease; the most common concurrent diseases were glaucoma (n = 29), hypertension (n = 26), diabetes mellitus (n = 19), cataract (n = 17), ocular hypertension (n = 10), hyperlipidemia (n = 9), rheumatoid arthritis (n = 8), osteoporosis (n = 6), dyslipidemia (n = 5), and dry eye (n = 5). Almost a quarter (22.7%) of patients had a past medical history, most commonly cataract (n = 13), gastric ulcer (n = 3), pneumonia, uterine leiomyoma, drug hypersensitivity, gout, asthma, cholecystitis, drug eruption, injection site reaction, open globe injury, and intraocular lens insertion (n = 2 each). Most patients were screened for tuberculosis (n = 234; 93.2%) and hepatitis B (n = 244; 97.2%; surface antigen test [HBsAg]: 92.8%, core antibody test [HBcAb]: 81.3%, surface antibody test [HBsAb]: 79.7%) at the first visit. The mean ± SD total VFQ-25 at baseline was 60.4 ± 21.1, with mean subscale scores ranging from 44.0 (general health) to 81.8 (color vision). Chest imaging was performed in 242 (96.4%) patients (X-ray: n = 183 [72.9%]; computed tomography: n = 131 [52.2%]).
Safety Outcomes
During the surveillance period, 70 of 251 patients (27.9%) reported at least one AE and 24 (9.6%) reported at least one serious AE (Table 2). Forty-seven patients (18.7%) reported at least one ADR and 14 (5.6%) reported at least one serious ADR (Table 2). The most common ADR was an infection (any infection: 21 patients, 8.4%; serious infection: eight patients, 3.2%) (Table 2, Table S1). Among the three most common primary diseases, the incidence of ADRs was higher in patients with sarcoidosis (any: 27.6%; serious: 13.8%) than in those with VKH disease (any: 18.8%; serious: 4.7%) or Behçet’s disease (any: 15.9%; serious: 2.9%) (Table S2). Infection was the most common ADR in all three primary disease groups. The incidence rate of ADRs was significantly higher in patients aged ≥ 65 years than in those < 65 years, in patients with concurrent diseases than in those without concurrent diseases, and in patients with a past medical history than in those without a past medical history (Table 3).
Serious infections, tuberculosis, and interstitial pneumonia were reported ADRs of interest (Table 2). Four patients developed active tuberculosis during the surveillance period (tuberculosis in two patients, miliary tuberculosis in one patient, and brain tuberculoma in one patient); of these, three patients had tested negative and one patient’s test was inconclusive (interferon-γ release assay test) before treatment. As important potential risks, two patients (0.8%) had a serious malignancy (colon cancer, breast cancer) and one patient (0.4%) had nonserious psoriasis aggravation (Table 2). One patient died because of a putaminal hemorrhage that was considered treatment-related. The patient was refractory to treatment with prednisolone, methotrexate, and cyclosporine and received adalimumab after a negative tuberculosis screen was confirmed. An adverse reaction of personality change occurred after the start of adalimumab administration, which was then discontinued. Subsequently, the patient was diagnosed with intracranial tuberculoma and died of putaminal hemorrhage.
Effectiveness Outcomes
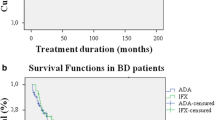
The recurrence rate of uveitis was 24.8% (61/246 patients) (Table 4). Recurrence rates were 37.0% in patients with sarcoidosis, 28.1% in patients with VKH disease, 23.5% in patients with Behçet's disease, and 21.4% in patients with idiopathic uveitis.
Visual acuity and foveal retinal thickness tended to be improved at final observation compared with pre-dose, and the percentage of patients with macular edema tended to be lower at final observation than at pre-dose (Table 5). Both anterior chamber cell grade and vitreous haze grade tended to shift to lower grades (i.e., improved) at final observation compared with pre-dose (Fig. 2). The proportion of patients with anterior chamber cell grade or vitreous haze grade of 0 increased from pre-dose to final observation.
At week 0, 121 patients were receiving concomitant oral corticosteroids; at week 52, 93 of these patients were still receiving adalimumab, and 69 were receiving both adalimumab and corticosteroids. The mean dose of oral corticosteroids (prednisolone equivalent) decreased from 14.6 mg/day at week 0 to 7.2 mg/day at week 52 (Fig. 3). Patients who were also receiving immunosuppressants had a mean corticosteroid dose of 12.6 mg/day at week 0 and 7.5 mg/day at week 52. Patients without immunosuppressants had a mean corticosteroid dose of 15.3 mg/day at week 0 and 7.1 mg/day at week 52. By week 52, 25.8% (24/93) of patients were corticosteroid-free; the percentage was 30.0% (6/20) in patients who were receiving immunosuppressants and 24.7% (18/73) in those who were not.
Mean changes in the daily oral corticosteroid dose (prednisolone equivalent) from week 0 to week 52. Week 0 was the start of adalimumab administration. The number of patients at each time point, expressed as the number receiving concomitant corticosteroids over the total number of patients receiving adalimumab (n/N), is shown under the graph. In patients who stopped using oral corticosteroids between time points, a corticosteroid dose of 0 mg/day was used for the subsequent time point
The mean change in total VFQ-25 score was 5.71, indicating improvement, and mean changes of 4 points or more in the VFQ-25 were observed in most subscales (Fig. 4). Changes greater than 6 points were seen in mental health (10.01), near vision (8.89), dependency (6.93), and general vision (6.73). Moderate changes of approximately 4–6 points were observed in ocular pain, distance vision, social functioning, role difficulties, color vision, and peripheral vision. In contrast, changes of < 2 points were seen in general health and driving.
Discussion
This is the first nationwide, prospective post-marketing evaluation of the long-term safety and effectiveness of adalimumab for the treatment of noninfectious uveitis in Japanese clinical practice. The safety profile of adalimumab was generally similar to that reported in previous clinical trials in noninfectious uveitis [9, 10, 13, 29] and other diseases [30], in observational studies in both Japan [17, 18] and other countries [14,15,16, 19,20,21], and in Japanese post-marketing surveillance studies in other inflammatory diseases [31,32,33,34]. Importantly, the incidence rates of serious infections, including tuberculosis, and malignancy were low. Moreover, sustained improvements were seen in visual acuity, macular edema, anterior chamber cell grade, vitreous haze, and HR-QoL, and the daily dose of oral corticosteroids decreased. These results support the long-term use of adalimumab in Japanese patients with noninfectious uveitis.
The long-term safety profile of adalimumab in Japanese clinical practice was consistent with the known effects of TNF-α inhibitors, and no new ADRs were identified. As expected based on extensive experience with adalimumab in other indications [12, 30,31,32,33,34], infections were the most common of the ADRs of interest and other important potential risks, and increased susceptibility to infections is typical of TNF-α inhibitors [6]. Similar results have been reported in Japanese post-marketing surveillance studies of the TNF-α inhibitor infliximab in refractory uveoretinitis associated with Behçet’s disease [7] and in rheumatoid arthritis [35]. Not surprisingly, the incidence of ADRs was higher in older patients and in patients with concurrent diseases or a past medical history; as with most treatments, these patients require additional care and safety monitoring during adalimumab treatment. ADRs were also more frequent in patients with sarcoidosis than in patients with VKH disease or Behçet’s disease, although the reason for this is unknown and may be related to the smaller sample size of patients with sarcoidosis. Serious cases of tuberculosis and malignancy were observed in four and two patients, respectively. These AEs also occurred at low rates in the VISUAL I–III trials [9, 10, 13, 29], as well as in post-marketing surveillance studies in other indications [30, 31, 33, 34]. Despite the higher prevalence of tuberculosis in Japan compared with European and North American countries [22], the overall incidence of tuberculosis in this post-marketing surveillance study (1.6%; 4/251 patients) was consistent with the incidence seen in the global VISUAL I (1/111 patients) and VISUAL II (3/115 patients) trials [9, 10]. The Japanese Ocular Inflammation Society recommends screening for tuberculosis and hepatitis B virus, as well as other serious infectious diseases, before initiating treatment with a TNF inhibitor [23]. Unfortunately, this screening was not conducted in a small proportion of patients in this study of clinical practice. The guidelines also note that false negative results may occur if the patient is currently treated with corticosteroids or immunosuppressants; therefore, monitoring should be repeated periodically after starting adalimumab treatment. Although the rate of malignancy was low, comparison with reference populations is needed to evaluate whether adalimumab increases the risk. The potential effect of TNF inhibitors on newly developed or recurrent cancer is currently unclear [8]. Psoriasis or psoriasis aggravation was observed in one patient (0.4%), a rate similar to that reported in VISUAL III (0.44 per 100 patient-years) [13]. Although sarcoidosis deterioration occurred at a rate of 0.35 per 100 patient-years in VISUAL III [13], it was not observed in this study.
Treatment with adalimumab was associated with improvements in the ocular symptoms of uveitis, visual acuity, and a broad range of HR-QoL categories. These results are consistent with those of the long-term VISUAL III extension study [13] and previous observational studies [14,15,16,17,18,19,20,21] and indicate that continued adalimumab treatment results in sustained control of uveitis. By week 52 of this study, > 90% of eyes had an anterior chamber cell grade of 0 or 0.5+, and > 80% had a vitreous haze grade of 0 or 0.5+. Foveal retinal thickness had also decreased, and the proportion of eyes with macular edema had approximately halved. In addition, the recurrence rate of uveitis was 24.8%, which is lower than the treatment failure rate seen in the VISUAL II trial (39% [45/115] of patients receiving adalimumab compared with 55% [61/111] of patients receiving placebo) [10], but similar to the 26 relapses per 100 patient-years seen over 12 months of treatment in a retrospective study conducted in Italy [16]. Interestingly, another Italian retrospective study reported an even lower rate of four relapses per 100 patient-years during the first 12 months of treatment with SB5, an adalimumab biosimilar [20]. These results suggest that adalimumab is at least as effective, and possibly more effective, at preventing uveitis recurrence in real-world clinical practice as in clinical trials.
Importantly, the observed improvements in ocular symptoms were accompanied by improvements in visual acuity and VFQ-25 scores, indicating better vision and less negative impact on quality of life. Noninfectious uveitis adversely affects all aspects of HR-QoL, as shown by worse scores on all VFQ-25 subscales compared with a population with normal vision [36]. In VISUAL I and II, adalimumab was associated with greater improvements in VFQ-25 total, general vision, and mental health scores, as well as in ocular pain and near vision scores in VISUAL I, compared with placebo [37]. In this post-marketing surveillance study, clinically meaningful improvements were observed in the total VFQ-25 score and in 10 of 12 subscales, indicating that the benefits of adalimumab extend beyond visual acuity alone. Further, adalimumab allowed the daily dose of oral corticosteroids to be reduced and a greater percentage of patients to be corticosteroid-free, even among patients who were receiving other immunosuppressants at baseline. This suggests that adalimumab has a corticosteroid-sparing effect in patients who have become refractory to corticosteroids and/or immunosuppressants. To minimize the potential for adverse effects with extended corticosteroid use, guidelines recommend doses < 10 mg/day for the treatment of noninfectious uveitis, as well as other inflammatory diseases [5, 38,39,40]. Despite these recommendations, reducing corticosteroid doses is sometimes difficult in patients with persistent inflammation, and adalimumab may be an option that allows corticosteroid doses to be further reduced.
This study provides real-world evidence of the use of adalimumab for noninfectious uveitis, including in patients who may have been excluded from clinical trials. In addition to evaluating safety, the study assessed a broad range of effectiveness measures, including patient-reported HR-QoL. However, changes in effectiveness parameters from week 0 to week 52 were not examined using inferential statistics and, given the observational nature of the study, there was no control group for comparison. Further, we did not collect or assess image data of fundus examination such as by fluorescein angiography and indocyanine angiography. In addition, the results may only be applicable to Japanese patients. Finally, longer-term follow-up and/or larger sample size may be needed to accurately assess rare events, such as malignancies.
Conclusions
In conclusion, this post-marketing surveillance study confirmed the long-term (52 weeks) safety and effectiveness of adalimumab for noninfectious uveitis in Japanese clinical practice. No new safety concerns were identified, sustained improvements in uveitis symptoms and HR-QoL were achieved, and a corticosteroid-sparing effect was observed.
References
Sonoda KH, Hasegawa E, Namba K, et al. Epidemiology of uveitis in Japan: a 2016 retrospective nationwide survey. Jpn J Ophthalmol. 2021;65(2):184–90.
Lee RW, Dick AD. Current concepts and future directions in the pathogenesis and treatment of non-infectious intraocular inflammation. Eye (Lond). 2012;26(1):17–28.
Rossi DC, Ribi C, Guex-Crosier Y. Treatment of chronic non-infectious uveitis and scleritis. Swiss Med Wkly. 2019;149:w20025.
Castiblanco C, Foster CS. Review of systemic immunosuppression for autoimmune uveitis. Ophthalmol Ther. 2014;3(1–2):17–36.
Jabs DA, Rosenbaum JT, Foster CS, et al. Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am J Ophthalmol. 2000;130(4):492–513.
Valenzuela RA, Flores I, Urrutia B, et al. New pharmacological strategies for the treatment of non-infectious uveitis. A minireview. Front Pharmacol. 2020;11:655.
Ohno S, Umebayashi I, Matsukawa M, Goto T, Yano T. Safety and efficacy of infliximab in the treatment of refractory uveoretinitis in Behçet’s disease: a large-scale, long-term postmarketing surveillance in Japan. Arthritis Res Ther. 2019;21(1):2.
Chen JL, Lobo-Chan A-M, Chan RVP, Bhat P. Tumor necrosis factor-alpha inhibitory therapy for non-infectious autoimmune uveitis. In: Rodriguez-Garcia A, Foster CS, editors. Advances in the diagnosis and management of uveitis. London: IntechOpen; 2019. p. 115–33. https://doi.org/10.5772/intechopen.82800.
Jaffe GJ, Dick AD, Brézin AP, et al. Adalimumab in patients with active noninfectious uveitis. N Engl J Med. 2016;375(10):932–43.
Nguyen QD, Merrill PT, Jaffe GJ, et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): a multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet. 2016;388(10050):1183–92.
Cantini F, Niccoli L, Goletti D. Adalimumab, etanercept, infliximab, and the risk of tuberculosis: data from clinical trials, national registries, and postmarketing surveillance. J Rheumatol Suppl. 2014;91:47–55.
Minozzi S, Bonovas S, Lytras T, et al. Risk of infections using anti-TNF agents in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis: a systematic review and meta-analysis. Expert Opin Drug Saf. 2016;15(sup1):11–34.
Suhler EB, Jaffe GJ, Fortin E, et al. Long-term safety and efficacy of adalimumab in patients with noninfectious intermediate uveitis, posterior uveitis, or panuveitis. Ophthalmology. 2021;128:899–909.
Bitossi A, Bettiol A, Silvestri E, et al. Adalimumab accounts for long-term control of noninfectious uveitis also in the absence of concomitant DMARD treatment: a multicenter retrospective study. Mediat Inflamm. 2019;2019:1623847.
Fabiani C, Sota J, Vitale A, et al. Cumulative retention rate of adalimumab in patients with Behçet’s disease-related uveitis: a 4-year follow-up study. Br J Ophthalmol. 2018;102(5):637–41.
Fabiani C, Vitale A, Rigante D, et al. Comparative efficacy between adalimumab and infliximab in the treatment of non-infectious intermediate uveitis, posterior uveitis, and panuveitis: a retrospective observational study of 107 patients. Clin Rheumatol. 2019;38(2):407–15.
Hiyama T, Harada Y, Kiuchi Y. Efficacy and safety of adalimumab therapy for the treatment of non-infectious uveitis: efficacy comparison among uveitis aetiologies. Ocul Immunol Inflamm. 2021. https://doi.org/10.1080/09273948.2020.1857791.
Kunimi K, Usui Y, Asakage M, et al. Anti-TNF-α therapy for refractory uveitis associated with Behçet’s syndrome and sarcoidosis: a single center study of 131 patients. Ocul Immunol Inflamm. 2020. https://doi.org/10.1080/09273948.2020.1791346.
Lee JT, Yates WB, Rogers S, Wakefield D, McCluskey P, Lim LL. Adalimumab for the treatment of refractory active and inactive non-infectious uveitis. Br J Ophthalmol. 2018;102(12):1672–8.
Sota J, Gentileschi S, Vitale A, et al. Effectiveness of SB5, an adalimumab biosimilar, in patients with noninfectious uveitis: a real-life monocentric experience. Asia Pac J Ophthalmol (Phila). 2021;10(4):360–5.
Tang-Lee-Say TL, Yang V, Fingret JM, et al. Adalimumab in patients with vision-threatening uveitis: real-world clinical experience. BMJ Open Ophthalmol. 2021;6(1):e000819.
World Health Organization. Global Tuberculosis Report. 2020. https://apps.who.int/iris/bitstream/handle/10665/336069/9789240013131-eng.pdf. Accessed 8 Jul 2021.
Japanese Ocular Inflammation Society. TNF Inhibitor Use Guidelines and Safety Measures Manual for Non-Infectious Uveitis (2nd Edition) [in Japanese]. 2019. http://jois.umin.jp/TNF.pdf. Accessed 8 Jul 2021.
Jabs DA, Nussenblatt RB, Rosenbaum JT, Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509–16.
Nussenblatt RB, Palestine AG, Chan CC, Roberge F. Standardization of vitreal inflammatory activity in intermediate and posterior uveitis. Ophthalmology. 1985;92(4):467–71.
Trusko B, Thorne J, Jabs D, et al. The Standardization of Uveitis Nomenclature (SUN) Project. Development of a clinical evidence base utilizing informatics tools and techniques. Methods Inf Med. 2013;52(3):259–65.
Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119(7):1050–8.
Suñer IJ, Kokame GT, Yu E, Ward J, Dolan C, Bressler NM. Responsiveness of NEI VFQ-25 to changes in visual acuity in neovascular AMD: validation studies from two phase 3 clinical trials. Invest Ophthalmol Vis Sci. 2009;50(8):3629–35.
Goto H, Zako M, Namba K, et al. Adalimumab in active and inactive, non-infectious uveitis: global results from the VISUAL I and VISUAL II trials. Ocul Immunol Inflamm. 2019;27(1):40–50.
Burmester GR, Panaccione R, Gordon KB, McIlraith MJ, Lacerda APM. Adalimumab: long-term safety in 23458 patients from global clinical trials in rheumatoid arthritis, juvenile idiopathic arthritis, ankylosing spondylitis, psoriatic arthritis, psoriasis and Crohn’s disease. Ann Rheum Dis. 2013;72(4):517–24.
Koike T, Harigai M, Ishiguro N, et al. Safety and effectiveness of adalimumab in Japanese rheumatoid arthritis patients: postmarketing surveillance report of 7740 patients. Mod Rheumatol. 2014;24(3):390–8.
Koike T, Harigai M, Ishiguro N, et al. Safety and effectiveness of adalimumab in Japanese rheumatoid arthritis patients: postmarketing surveillance report of the first 3000 patients. Mod Rheumatol. 2012;22(4):498–508.
Ogata H, Watanabe M, Matsui T, et al. Safety of adalimumab and predictors of adverse events in 1693 Japanese patients with Crohn’s disease. J Crohns Colitis. 2016;10(9):1033–41.
Suzuki Y, Hagiwara T, Kobayashi M, Morita K, Shimamoto T, Hibi T. Is adalimumab safe and effective in patients with intestinal Behcet’s disease in real-world practice? Intest Res. 2021;19(3):301–12.
Takeuchi T, Tatsuki Y, Nogami Y, et al. Postmarketing surveillance of the safety profile of infliximab in 5000 Japanese patients with rheumatoid arthritis. Ann Rheum Dis. 2008;67(2):189–94.
Naik RK, Rentz AM, Foster CS, et al. Normative comparison of patient-reported outcomes in patients with noninfectious uveitis. JAMA Ophthalmol. 2013;131(2):219–25.
Sheppard J, Joshi A, Betts KA, et al. Effect of adalimumab on visual functioning in patients with noninfectious intermediate uveitis, posterior uveitis, and panuveitis in the VISUAL-1 and VISUAL-2 trials. JAMA Ophthalmol. 2017;135(6):511–8.
Duru N, van der Goes MC, Jacobs JWG, et al. EULAR evidence-based and consensus-based recommendations on the management of medium to high-dose glucocorticoid therapy in rheumatic diseases. Ann Rheum Dis. 2013;72(12):1905–13.
Manson SC, Brown RE, Cerulli A, Vidaurre CF. The cumulative burden of oral corticosteroid side effects and the economic implications of steroid use. Respir Med. 2009;103(7):975–94.
Strehl C, Bijlsma JWJ, de Wit M, et al. Defining conditions where long-term glucocorticoid treatment has an acceptably low level of harm to facilitate implementation of existing recommendations: viewpoints from an EULAR task force. Ann Rheum Dis. 2016;75(6):952–7.
Acknowledgements
Funding
This study was sponsored by AbbVie GK, Tokyo, Japan, manufacturer/licensee of adalimumab in Japan, and Eisai Co., Ltd. The sponsors participated in the study design, data collection, analysis and interpretation of data, and writing, reviewing, and approving the publication. Medical writing assistance was provided by Rebecca Lew, PhD, CMPP, and Serina Stretton, PhD, CMPP, of ProScribe–Envision Pharma Group, under the direction of the authors, and was funded by AbbVie GK. AbbVie GK also funded the journal’s Rapid Service Fees. ProScribe’s services complied with international guidelines for Good Publication Practice (GPP3).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Kenichi Namba: conception and design; analysis and interpretation of data; drafting the manuscript; critical revision for intellectual content; administrative, technical, or material support; supervision. Toshikatsu Kaburaki: acquisition of data; critical revision for intellectual content; administrative, technical, or material support. Hidekazu Tsuruga: analysis and interpretation of data; drafting the manuscript; critical revision for intellectual content; supervision. Yohei Ogawa: analysis and interpretation of data; drafting the manuscript; critical revision for intellectual content; supervision. Eri Iwashita: analysis and interpretation of data; drafting the manuscript; critical revision for intellectual content; supervision. Hiroshi Goto: analysis and interpretation of data; critical revision for intellectual content; supervision.
Disclosures
Kenichi Namba reports receiving study funding and medical writing support for this manuscript from AbbVie GK, other grants or contracts from AbbVie GK, Mitsubishi Tanabe Pharma Corporation, Eisai Co., Ltd., and EP-CRSU Co., Ltd., and speaker fees from Alcon Pharmaceuticals Ltd., Pfizer Japan Inc., Novartis Pharma K.K., Kowa Pharmaceutical Co., Ltd., Senju Pharmaceutical Co., Ltd., Mitsubishi Tanabe Pharma Corporation, Eisai Co., Ltd., AbbVie GK, Santen Pharmaceutical Co., Ltd., and Celgene Co., Ltd.
Toshikatsu Kaburaki reports receiving study funding and medical writing support for this manuscript from AbbVie GK, research grants-in-aid from Santen Pharmaceutical Co., Ltd., Eisai Co., Ltd., Novartis Pharma K.K., AbbVie GK, Kowa Pharmaceutical Co., Ltd., Senju Pharmaceutical Co., Ltd., and Wakamoto Pharmaceutical Co., Ltd., funding for physician-initiated trials from Ono Pharmaceutical Co., Ltd, consulting fees from AbbVie GK, and speaker fees from AbbVie GK, Santen Pharmaceutical Co., Ltd., Novartis Pharma K.K., Eisai Co., Ltd., Mitsubishi Tanabe Pharma Corporation, Kowa Pharmaceutical Co., Ltd., Wakamoto Pharmaceutical Co., Ltd., Senju Pharmaceutical Co., Ltd., and Ono Pharmaceutical Co., Ltd.
Hidekazu Tsuruga, Yohei Ogawa, and Eri Iwashita are employees and stockholders of AbbVie GK and received study funding and medical writing support for this manuscript from AbbVie GK.
Hiroshi Goto reports receiving study funding and medical writing support for this manuscript from AbbVie GK, and honoraria from Santen Pharmaceutical Co., Ltd., Senju Pharmaceutical Co., Ltd., Alcon Japan Ltd., AbbVie GK, Eisai Co., Ltd., Kowa Pharmaceutical Co., Ltd., Mitsubishi Tanabe Pharma Corporation, and Hoya Corporation.
Prior Presentation
The data in this manuscript were presented at the 54th Annual Meeting of the Japanese Ocular Inflammation Society (Foursome 2021), July 23–25, 2021, Sendai International Center, Sendai, Japan.
Compliance with Ethics Guidelines
This post-marketing surveillance was conducted in accordance with Good Post-marketing Study Practices for Drugs, and Japanese regulatory and legal requirements. The protocol was approved by the Pharmaceuticals and Medical Devices Agency of Japan. Patients provided written informed consent before any surveillance-specific procedures.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Other Acknowledgments
The authors would like to thank all of the patients, investigators, and support staff who participated in this study.
The authors would also like to thank Eisai Co., Ltd. (Tokyo, Japan) for surveillance monitoring, EPS Corporation (Tokyo, Japan) for the central registration system, data management, and statistical analyses, and Fujitsu FIP Corporation (now Fujitsu Japan Limited, Tokyo, Japan) for the electronic data capture system, which was approved by the Post-Marketing Surveillance group at AbbVie GK.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Namba, K., Kaburaki, T., Tsuruga, H. et al. Long-Term Safety and Effectiveness of Adalimumab in Japanese Patients with Noninfectious Intermediate, Posterior, or Panuveitis: Post-Marketing Surveillance of 251 Patients. Ophthalmol Ther 11, 1147–1161 (2022). https://doi.org/10.1007/s40123-022-00493-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00493-z