Abstract
Introduction
Characteristics of the haptics and optic–haptic junction (OHJ) of an intraocular lens (IOL) affect IOL position in the capsular bag, positional stability, and the development of posterior capsule opacification. Therefore, the haptics and OHJ have a role in determining initial and long-term visual outcomes after cataract surgery. Understanding differences in the haptics and OHJ of available IOLs and in the relationships between the haptics of each IOL and the capsular bag across a range of capsular bag sizes might inform selection of an IOL model for individuals.
Purpose
To evaluate the geometry of five currently marketed, commonly used one-piece hydrophobic acrylic monofocal IOLs and changes in haptic–capsular bag relationships according to capsular bag size using a range of compression well diameters.
Methods
AcrySof SN60WF, CT LUCIA 621PY, enVista MX60, TECNIS ZCB00, and Vivinex XY1 IOLs were scanned with computed tomography (CT) in a dry, uncompressed state for quantitative analyses of haptic and OHJ dimensions and qualitative assessment of geometry. CT scanning was done after IOL placement into a series of compression wells (11.5, 11.0, 10.0, and 9.0 mm) for analyses of haptic angle of contact (AoC) and capsular bag contact (CBC). IOL axial alignment and haptic–capsular bag relationships were assessed on side-view and 3-dimensional top-view images, respectively.
Results
The qualitative and quantitative evaluations highlighted differences in haptic and OHJ geometry and dimensions across the five IOLs. All haptic dimensions (length, thickness, surface area, volume) and all OHJ dimensions (surface area and volume) were greatest for the CT LUCIA 621PY IOL. Compared to the IOL that had the smallest measurement for each parameter, the value for the CT LUCIA 621PY IOL was 31–91% larger. The lens with the largest OHJ surface area and volume showed values that were 500% and 240% greater than the corresponding values for the lens with the smallest OHJ surface area and OHJ volume. The AoC and CBC values decreased with increasing well size for all IOLs. The CT LUCIA 621PY had the greatest AoC and CBC values for all well sizes and the smallest percentage change in AoC and CBC comparing the values from the 9.0 mm and 11.5 mm wells.
Conclusion
The in vitro evaluations in this study highlight differences in the haptic and OHJ geometric characteristics of the five IOLs studied. The collected evidence refutes opinions that all hydrophobic acrylic one-piece IOLs are the same and supports the idea that individual IOLs can have relative advantages and disadvantages that depend on the individual case. We believe the knowledge of geometry is necessary for the surgeon to have the opportunity to select the best “customized” option in the individual case as a result of anatomical conditions and secondary diagnoses. Our bench study shows how big the differences are in currently available monofocal hydrophobic acrylic lenses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Although five acrylic, hydrophobic, monofocal lenses appear similar on gross examination, sharing a C-loop haptic design and having identical overall length and optic diameter, the computed tomography (CT) analyses revealed clear differences between the studied intraocular lenses (IOLs). |
We found variability among the tested lenses in all of the dimensions measured for both the haptics (length, thickness, surface area, volume) and optic–haptic junction (surface area and volume). |
Knowledge of the geometry and behavior of the lens depending on compression (angle of contact and capsular bag contact) seems important, as visual outcomes after cataract surgery depend on IOL position in the capsular bag. |
Introduction
Cataract surgery ranks as one of the most commonly done surgical procedures in many countries around the world, and it is estimated that 34 million cataract procedures would be performed worldwide in 2021 [1, 2]. Patients undergoing cataract surgery expect excellent refractive and visual outcomes, and surgeons are largely able to deliver on these goals thanks to a host of advances in surgical techniques and technologies, including the use of modern intraocular lenses (IOLs). Delivering on patient expectations to maintain quality vision over the longer term depends in part on both biomechanical stability of the IOL and the development of posterior capsule opacification (PCO). The biomechanical stability of an IOL and risk of PCO are influenced by several factors, of which the IOL’s haptic design and design of the optic–haptic junction (OHJ) have important roles [3,4,5,6,7].
The OHJ represents the site where the optic merges with the haptic, and on the basis of his extensive research on PCO, David J Apple, MD, described the OHJ as a possible Achilles’ heel in an IOL’s ability to block in-growth of lens epithelial cells that leads to PCO [7]. On the basis of this knowledge, various manufacturers have paid special attention to OHJ design when developing new lenses. The positive effects of a stable OHJ without increased risk of PCO could also be proven in clinical practice with studies [8, 9].
Currently available IOLs can be categorized in a variety of ways, including based on optic design, overall design, and material. Recent data indicate that non-toric monofocal IOLs account for approximately 90% of implanted lenses, a single-piece C-loop configuration is the most common overall design, and hydrophobic acrylic is the leading material (Fig. 1) [10]. Although surgeons may believe that currently available one-piece hydrophobic acrylic monofocal IOLs are all similar and likely to provide similar clinical outcomes, closer inspection of their design and geometry may show differences that have potential importance for IOL optical performance and clinical outcomes.
Haptic geometry is one of the features that varies among one-piece hydrophobic acrylic monofocal IOLs. Designs represented within this group of lenses include planar haptics with a 0° angle or a step-vaulted configuration in which the haptics are offset from the optic plane.
Differences may also exist between IOLs in haptic thickness and area and in OHJ volume and area. Each of these features may play a role in determining the response to force exerted through capsular bag compression and therefore the ability of an IOL to maintain optic position stability [5, 11].
Differences in haptic geometry may also result in differences in haptic angle of contact with the capsular bag that is another important parameter affecting IOL intraocular stability and PCO development. It also has the potential to impact PCO rates through its effect on the area open to cellular migration and proliferation described in the past as a “barrier effect” with the OHJ described as the weak point [12]. Although measurements of haptic and OHJ dimensions are standard for a given IOL model, haptic angle of contact will vary depending on capsular bag size [13]. As specified by ISO 11979-3, premarketing testing of the mechanical properties of IOLs intended for capsular bag implantation that determine angle of contact in addition to other endpoints is done with placement of the IOL in a single-size (10 mm) compression well [14]. However, it is well known that the anatomy and capsular bag size vary among eyes, increasing with increasing axial length [15,16,17,18]. Furthermore, as a result of capsular bag fibrosis, capsular bag size decreases postoperatively and in an unpredictable manner [17]. An IOL with haptics that maintain a consistent relationship and contact with the capsular bag independent of native size or postoperative contraction would be expected to confer intraocular positional stability, limit PCO development, and provide predictably reliable functional outcomes for patients undergoing cataract surgery.
The purpose of this bench study was to evaluate the geometry of currently commonly used hydrophobic acrylic monofocal IOLs. Computed tomography (CT) scanning was used to characterize and compare the design of the haptics and OHJ of five one-piece, monofocal, hydrophobic acrylic IOLs and to explore changes in the haptic–capsular bag relationships for a given IOL and between IOLs according to capsular bag size. Compression wells of different diameters were used as a surrogate model for the capsular bag that would allow comparisons of the projected angle of contact (AoC, according to ISO) and simulated capsular bag contact angle (CBC, reflecting the true contact zone) in a standardized setting.
Methods
The five hydrophobic, acrylic one-piece IOLs (power 21 D) included in the study are shown in Fig. 2; Table 1 summarizes their characteristics. All tests and measurements were done in dry ambient conditions using a new sample for each IOL. This article is based on bench evaluations and does not contain any studies with human participants or animals performed by any of the authors.
OHJ Characteristics
Evaluations of the OHJ included CT measurements of the uncompressed IOLs. After cleaning with deionized water, each IOL was positioned in its natural state (non-compressed) on a low-density foam block for CT scanning with the Metrotom 1500 (isotropic voxel size of 10 µm). Each IOL was scanned in air and ambient temperature (21 °C).
OHJ volume and OHJ surface area were analyzed using VGStudio Max 3.4 (Volume Graphics). Environment and IOL were segmented (separated) by extended surface determination, and filtering particles and artifacts were removed using the open/close function. The optic body was removed from the IOL, and the volume and total area of the remaining haptics were measured. The results for the two haptics were averaged.
Visual comparison of geometrical differences between IOLs was done by using the CT LUCIA IOL as the reference model by superimposing the top view 3-dimensional image of each of the other IOLs over the CT LUCIA image. Additionally, detailed images of the OHJ were obtained at ×5 magnification for each IOL under the AXIO Imager.Z2 microscope and analyzed with ZEN core 3.3 software (Carl Zeiss Microscopy GmbH).
In addition to CT scanning of the uncompressed IOLs, CT scans were acquired of compressed IOLs placed into 9.0 mm, 10.0 mm, 11.0 mm, and 11.5 mm diameter wells. The compression wells were modeled with Autodesk Inventor Professional 2019 and 3D-printed (Anycubic Photon, Anycubic ECO UV Resin Translucent Green 3D) (Fig. 3). The same set of wells was used for all five IOLs. To guide precise IOL alignment, a cross-hair was added to each well as an alignment guide and IOL placement was done under microscope visualization (SmartZoom 5, Carl Zeiss IMT GmbH).
Scanning of the compressed IOLs was done with each IOL placed first into the 11.5 mm well and then successively into each smaller diameter well with a relaxation period sufficiently long to eliminate remaining deformation.
Contact angle analyses, both angle of contact (AoC) and virtual capsular bag contact (CBC), on both well sides were done with VG Studio Max 3.4. All images were exported at the same zoom level for comparability. Environment and IOL were separated by extended surface determination and filtering particles, and artifacts were removed using the open/close function. A refined surface determination was performed, and the region of interest (ROI) was created. Alignment of the scanned volume (compression well and IOL) was done using the well bottom as the reference plane. A circle was created matching the compression well diameter and then a second circle was created that was concentric to the first and 0.5 mm smaller than the compression well diameter. AoC and CBC angles were measured from the center (Fig. 4). AoC was measured according to the ISO standard as the intercept of the IOL haptics with the second circle (Fig. 3). CBC, which simulates the estimated true contact between the IOL and capsular bag, was defined by the actual wall contact rather than the projected intercept of the ISO definition (Fig. 3).
Example of the CT measurements and analysis. a 3D representation of an IOL in a Ø10 mm compression well; b cross-section highlighting the proper alignment of the IOL during the scan; c analysis of the AoC via a concentric circle to the well; d analysis of the CBC using the same center, but evaluation of the true contact points
Results
Haptic Analyses
Geometry
Images of the haptics of the five IOLs show differences in their geometry (Fig. 5). The haptics were examined microscopically (SmartZoom 5) and evaluated for integrity and compared with data of the volume calculation.
Haptic Thickness
Results from measurement of haptic thickness at the distal and proximal ends are shown in Fig. 6. The distal and proximal haptic thicknesses are identical for the CT LUCIA 621PY (0.47 and 0.47 mm, respectively) and greater than all other IOLs. Compared to the enVista MX60 that has the thinnest distal and proximal haptics (0.36 and 0.35 mm, respectively), the CT LUCIA 621PY haptics are 31% thicker at the distal end and 34% thicker proximally. The distal and proximal haptic thicknesses are also identical for the AcrySof SN60WF (0.45 and 0.45 mm, respectively), differ by 0.01 mm for both the TECNIS ZCB00 (0.45 and 0.46 mm, respectively), and differ by 0.03 mm for the Vivinex XY1 IOL (0.37 and 0.40 mm, respectively).
Haptic Surface Area
Figure 7 shows results from haptic surface area measurements. Surface area is greatest for the CT LUCIA 621PY (18.82 mm2) and approximately 63% greater than the haptic surface area of the Vivinex XY1 that has the smallest haptic surface area (11.56 mm2). Haptic surface area is relatively similar for the AcrySof SN60WF (14.33 mm2), TECNIS ZCB00 (14.52 mm2), and enVista MX60 (14.81 mm2) IOLs.
Haptic Volume
Haptic volume data are displayed in Fig. 8. Haptic volume is greatest for the CT LUCIA 621PY IOL (2.22 mm3) and between 33% and 91% larger than the haptic volume of the other four IOLs (TECNIS ZCB00 1.67 mm3; AcrySof SN60WF 1.55 mm3, enVista MX60 1.29 mm3, Vivinex XY1 1.16 mm3).
OHJ Geometry
Images of the OHJ of the five IOLs show differences in their geometry (Fig. 9). Width of the OHJ is broadest for the CT LUCIA 621PY and enVista MX60. This difference is also seen in Fig. 10 that shows images from superimposing the top view 3-dimensional images of IOLs over the CT LUCIA 621PY image. The superimposed images also highlight differences in haptic length, although all tested lenses have the same overall diameter of 13.0 mm, except for the enVista MX60 with diameter of 12.5 mm.
OHJ Surface Area and Volume
The CT LUCIA 621PY has both the largest OHJ surface area and volume (1.0 mm2 and 0.51 mm3 respectively), and these values are 500% and 240% greater, respectively, than the corresponding values for the Vivinex XY1 that has the smallest OHJ surface area (0.2 mm2) and OHJ volume (0.21 mm3) (Figs. 11 and 12). Although OHJ surface area is relatively similar for the AcrySof SN60WF, TECNIS ZCB00, and enVista MX60 (0.6, 0.7, and 0.7 mm2, respectively), OHJ volume for the enVista MX60 is approximately 60% greater compared to the AcrySof SN60 WF and TECNIS ZCB00 (0.49 mm3 vs 0.31 and 0.31 mm3, respectively).
Haptic Contact Measurements
Angle of Contact (AoC) ISO Measurements
The images used to calculate the AoC (ISO) measurements for the five IOLs in the various compression wells and the corresponding data are shown in Figs. 13 and 14, respectively. AoC decreases with increasing well size for all IOLs, but the percentage change between the 9.0 mm and 11.5 mm wells is approximately 50% for the CT LUCIA 621PY versus approximately 63% to 66% for all of the other IOLs. The CT LUCIA 621PY also has the largest AoC across all well sizes, and the AoC values are smallest for the Vivinex XY1. Across the four well sizes, the AoC values for the CT LUCIA 621PY are between 20% and 74% larger than those of the Vivinex XY1.
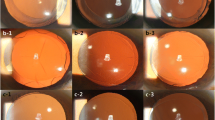
Capsular Bag Contact (CBC) Measurements
Figure 15 shows the images used to calculate the CBC values for the five IOLs in the various compression wells and the data are shown in Fig. 16. Across all well sizes, the CT LUCIA 621PY has the greatest CBC, but the IOL with the lowest CBC varies. For all IOLs except the TECNIS ZCB00, CBC is greater in the 9 mm well compared to the 10 mm well, but the TECNIS ZCB00 is the only IOL for which there is little difference in CBC between the 9 mm and 10 mm wells.
Axial Alignment and Position
The IOLs’ axial position and tilt in different well sizes are evaluated with side-view CT images (Fig. 17). In general, IOLs with greater CBC for a given well size or with longer/wider surface area seem to have more shift upward than IOLs with lower CBC values (indicating less capsular bag contact) and shorter/thinner haptics. All lenses showed good centration after positioning in the wells. No major abnormalities or differences between the five IOLs were observed.
3-Dimensional Images
The 3-dimensional CT images of the IOLs in the wells allow better visualization of haptic behavior with compression in different well diameters, especially eliminating their transparence by the CT technique (Fig. 18). This representation was chosen to give a good overall impression of the whole lens including movement/shift reaction depending on compression.
Discussion
Visual outcomes after cataract surgery depend on IOL position in the capsular bag. The effective lens position post-implantation and the potential for postoperative shift, including axial displacement, decentration, tilt, and axial rotation, are affected by multiple anatomic and IOL-related features, among which capsular bag size and haptic/OHJ design have prominent roles. A study evaluating 46 eye bank eyes found capsular bag size after lens removal averaged 10.38 ± 0.35 mm with a range from 9.75 to 11.00 mm [18]. Consistent with these data, a study measuring capsular bag diameter in the first days after cataract surgery in a series of 70 eyes reported the mean was 10.37 ± 0.25 mm [15]. The same researchers determined that capsular bag diameter correlated negatively with corneal power and positively with axial length. A study investigating postoperative change in capsular bag diameter reported an average decrease of 0.7 mm at 1 month after standard cataract surgery [17].
Previous research showed that IOLs with a flexible design as defined by hinge geometry have better biomechanical stability than those with a more rigid design [4]. Axial displacement is mainly affected by the width and thickness of the haptic, in an experimental parameter variation on an IOL base design, but also by the size of the haptic–optic junction. Haptic thickness also affects tilt as does the interaction between the haptic curvature and the OHJ. Rotation is affected by the start of the haptic curvature, the OHJ, haptic width, and angle of contact between the haptic and capsular bag, with a wider angle of contact improving rotational stability of toric IOLs, but also by biometric characteristics, with more rotation in eyes with longer axial length and a larger white-to-white measurement [19, 20].
In this study we evaluated the haptic design and OHJ features of five commonly used hydrophobic acrylic aspheric monofocal IOLs. In addition, because IOL positional stability is related to the degree of haptic contact with the capsular bag, we measured AoC and CBC for each of the IOLs across four well diameters that were chosen to represent the range of adult human capsular bag sizes pre- and post-IOL implantation [17, 18, 21]. To the best of our knowledge, this is the first in vitro investigation that used CT technology to provide accurate insights about haptic/OHJ characteristics and haptic contact of modern acrylic IOLs.
It is even surprising that currently companies provide only very few parameters of their highly technical and well-developed products—such as clear optic diameter and overall diameter. Surgeons are actually provided with very little data although they are fully responsible not only for the success during surgery but also for the best choice of the implant.
Although the five monofocal lenses appear similar on gross examination, sharing a C-loop haptic design and having identical (or nearly identical) overall length and optic diameter, the CT analyses revealed clear differences between the studied IOLs. We found variability among the lenses in all of the dimensions measured for both the haptics (length, thickness, surface area, volume) and OHJ (surface area and volume), but the values for all measures were consistently greatest for the CT LUCIA 621PY IOL.
Our finding that the AoC and CBC values decreased with increasing well size for all IOLs is consistent with previous research examining this relationship using both test wells and a rabbit model [22]. We also found variability in AoC and CBC between IOLs at all well sizes, but both values were consistently greatest for the CT LUCIA 621PY, which had the lowest AoC and CBC percentage change between the smallest and largest diameter wells.
It is interesting to note that although the enVista MX60 had a smaller overall diameter than the other four IOLs (12.5 vs 13.0 mm), it did not consistently have the lowest CBC and AoC values with increasing well size. This finding reinforces the idea that besides raw material and water content, the OHJ geometry and haptics design play a decisive role in the IOL–capsular bag relationship.
The CT side-view images of the IOLs provided an opportunity to explore possible correlations between haptics/OHJ features and IOL position. Overall, these qualitative assessments suggest that although IOLs with a wider OHJ and pronounced haptics achieve a greater angle of contact with the surrounding well, they seem to be more susceptible to axial movement/shift when compressed within a very small diameter. This should be investigated in further studies including measurements of positional changes that would determine the clinical relevance of any shifts.
Limitations
We want to emphasize that the parameters evaluated in our study are only some of the factors affecting the intraocular performance of a lens. Other issues, including material properties, optic design, and surgical factors, also play an important role. In addition, the results of this bench study cannot be used to draw conclusions about the clinical relevance of the qualitative and measured differences in haptic and OHJ characteristics or to rank any IOL as a superior option. All of the tested lenses have been demonstrated to be safe and effective through premarketing and postmarketing clinical studies [8, 9, 23,24,25]. However, the findings may be considered in relation to available clinical experience. There are correlations in size and overall diameter of capsular bag and behavior of the IOL during surgery (implantation, unfolding, positioning, stability during irrigation/aspiration, posterior capsule polishing, removing viscoelastic remnants) and in the postoperative period. The exact relationship and effect as well as clinical implications should be targeted in large clinical trials with diverse IOL models.
Conclusion
The bench evaluations in this study highlight differences in the haptic and OHJ geometric characteristics of the five IOLs studied. The collected evidence refutes opinions that all hydrophobic acrylic one-piece IOLs are the same and supports the idea that individual IOLs can have relative advantages and disadvantages that depend on the individual case.
We believe that the knowledge of geometry is necessary for the surgeon to have the opportunity to select the best option in the individual case. In this evaluation we showed how big the differences are in currently available monofocal hydrophobic acrylic lenses.
The findings provide objective evidence corroborating a phenomenon that is probably well known to many surgeons from their intraoperative observations of differences in IOL behavior when positioning in small versus larger capsular bags. They also might provide an impetus for conducting a large, multicenter study to establish clinical translation of the relationships described in this bench study. In the meantime, and because of the potential implications for improving predictability of effective lens position and refractive outcomes, surgeons might consider taking the findings of our study into account when choosing an IOL in cases of hyperopic eyes that are likely to have a relatively small capsular bag and high myopic eyes that are likely to have a large capsular bag. The opinion that all monofocal lenses with the same overall diameters are geometrically the same is outdated.
References
Market Scope. 2020 IOL market report: mid-year update. Market Scope, St. Louis, MO. https://www.market-scope.com. Accessed 28 Aug 2020.
Wang W, Yan W, Fotis K, et al. Cataract surgical rate and socioeconomics: a global study. Invest Ophthalmol Vis Sci. 2016;57:5872–81.
Remón L, Siedlecki D, Cabeza-Gil I, Calvo B. Influence of material and haptic design on the mechanical stability of intraocular lenses by means of finite-element modeling. J Biomed Opt. 2018;23(3):1–10.
Cabeza-Gil I, Pérez-Gracia J, Remón L, Calvo B. Effect of haptic geometry in C-loop intraocular lenses on optical quality. J Mech Behav Biomed Mater. 2021;114: 104165.
Mochiji M, Kaidzu S, Ishiba Y, Matsuda Y, Tanito M. Measurement of force required for anterior displacement of intraocular lenses and its defining parameters. Materials (Basel). 2020;13(20):4593.
Lane S, Collins S, Das KK, et al. Evaluation of intraocular lens mechanical stability. J Cataract Refract Surg. 2019;45(4):501–6.
Apple DJ, Escobar-Gomez M, Zaugg B, Kleinmann G, Borkenstein AF. Modern cataract surgery: unfinished business and unanswered questions. Surv Ophthalmol. 2011;56(6 Suppl):S3-53.
Borkenstein AF, Borkenstein EM. Surgical experience with a redesigned, fully preloaded, hydrophobic acrylic intraocular lens in challenging cases of pseudoexfoliation syndrome, phacodonesis, and small pupils. Clin Ophthalmol. 2019;13:199–206.
Ling R, Borkenstein EM, Borkenstein AF. Evaluation of Nd:YAG laser capsulotomy rates in a real-life population. Clin Ophthalmol. 2020;14:3249–57.
Market Scope. 2020 iol report: a global market analysis for 2019 to 2025. Market Scope, St. Louis, MO. https://www.market-scope.com. Accessed May 2020.
Cabeza-Gil I, Ariza-Gracia MÁ, Remón L, Calvo B. Systematic study on the biomechanical stability of C-loop intraocular lenses: approach to an optimal design of the haptics. Ann Biomed Eng. 2020;48(4):1127–36.
Ness PJ, Werner L, Maddula S, et al. Pathology of 219 human cadaver eyes with 1-piece or 3-piece hydrophobic acrylic intraocular lenses: capsular bag opacification and sites of square-edged barrier breach. J Cataract Refract Surg. 2011;37(5):923–30.
Wormstone IM, Damm NB, Kelp M, Eldred JA. Assessment of intraocular lens/capsular bag biomechanical interactions following cataract surgery in a human in vitro graded culture capsular bag model. Exp Eye Res. 2021;205: 108487.
International Organization for Standardization. Ophthalmic implants—intraocular lenses—part 3: mechanical properties and test methods (ISO 11979-3:2012). Geneva: ISO; 2012.
Vass C, Menapace R, Schmetterer K, et al. Prediction of pseudophakic capsular bag diameter based on biometric variables. J Cataract Refract Surg. 1999;25(10):1376–81.
Zhu X, Du Y, Li D, et al. Aberrant TGF-β1 signaling activation by MAF underlies pathological lens growth in high myopia. Nat Commun. 2021;12(1):2102.
Dick HB, Conrad-Hengerer I, Schultz T. Intraindividual capsular bag shrinkage comparing standard and laser-assisted cataract surgery. J Refract Surg. 2014;30(4):228–33.
Vasavada A, Singh R. Relationship between lens and capsular bag size. J Cataract Refract Surg. 1998;24(4):547–51.
Yao Y, Meng J, He W, et al. Associations between anterior segment parameters and rotational stability of a plate-haptic toric intraocular lens. J Cataract Refract Surg. 2021;47(11):1436–40.
Bozukova D, Werner L, Mamalis N, et al. Double-C loop platform in combination with hydrophobic and hydrophilic acrylic intraocular lens materials. J Cataract Refract Surg. 2015;41(7):1490–502.
Modesti M, Pasqualitto G, Appolloni R, Pecorella I, Sourdille P. Preoperative and postoperative size and movements of the lens capsular bag: ultrasound biomicroscopy analysis. J Cataract Refract Surg. 2011;37(10):1775–84.
Bozukova D, Pagnoulle C, Jérôme C. Biomechanical and optical properties of 2 new hydrophobic platforms for intraocular lenses. J Cataract Refract Surg. 2013;39(9):1404–14.
Lee KM, Park SH, Joo CK. Comparison of clinical outcomes with three different aspheric intraocular lenses. Acta Ophthalmol. 2011;89(1):40–6.
Packer M, Fry L, Lavery KT, et al. Safety and effectiveness of a glistening-free single-piece hydrophobic acrylic intraocular lens (enVista). Clin Ophthalmol. 2013;7:1905–12.
Chandra KK, Malhotra C, Jain AK, Sachdeva K, Singh S. Effect of decentration on the quality of vision: a comparison between aspheric balance curve design and posterior aspheric design intraocular lenses. J Cataract Refract Surg. 2021. https://doi.org/10.1097/j.jcrs.0000000000000810.
Acknowledgements
Funding
No funding was received for this study or publication of this article. The journal’s Rapid Service Fee was funded privately without external subsidies by the main author (Andreas F. Borkenstein).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Andreas F. Borkenstein designed the concept of the study and wrote the draft of the manuscript. Both authors critically reviewed the manuscript and contributed significantly to the final manuscript.
Disclosures
Andreas F. Borkenstein and Eva-Maria Borkenstein have no proprietary or commercial interest in the medical devices that are involved in this manuscript and confirm that they have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on bench evaluations and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Borkenstein, A.F., Borkenstein, EM. Geometry of Acrylic, Hydrophobic IOLs and Changes in Haptic–Capsular Bag Relationship According to Compression and Different Well Diameters: A Bench Study Using Computed Tomography. Ophthalmol Ther 11, 711–727 (2022). https://doi.org/10.1007/s40123-022-00469-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00469-z