Abstract
Endophthalmitis is a sight-threatening condition, and its timely and appropriate management is essential in preventing permanent vision loss. Recent changes in clinical practice in endophthalmitis and advances in modern vitreoretinal surgery may limit the applicability of established randomised clinical trial evidence to current management. This review discusses the epidemiology, pathophysiology, changing patient presentation, diagnosis and advances in the management of endophthalmitis, presenting the existing literature on this topic and results from Sydney Eye Hospital.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Micro-incision vitrectomy surgery (MIVS) has changed the way the Early Vitrectomy Study (EVS) should be interpreted in current practice. |
Increased use of intravitreal injections and improved practices in cataract surgery have changed the common pathogens encountered in endophthalmitis. |
Modifications in vitrectomy techniques in the context of poor visualisation can improve the safety of the procedure. |
Digital Features
This article is published with digital features, including a video, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.16699714.
Introduction
Endophthalmitis—defined as inflammation of the intraocular tissues and fluids—is a sight-threatening condition, and potentially results in loss of the eye. Permanent sight loss in endophthalmitis may occur by a number of mechanisms, including exposure to bacterial toxins, vascular occlusion, retinal necrosis and detachment. However, prompt treatment in the absence of significant structural and morphological damage can result in good clinical outcomes, even in the long term [1].
The role of surgical washout (in the form of vitrectomy) of the intraocular compartment in endophthalmitis remains controversial. The Early Vitrectomy Study (EVS), published in 1995, is the only large-scale prospective randomised controlled trial (RCT) comparing pars plana vitrectomy (PPV) to intravitreal injection of antibiotics in the management of acute (i.e. within 6 weeks of the inciting procedure) post-operative endophthalmitis [2]. Although it has strongly guided management, significant evolution in clinical practice has occurred since its publications. This includes changes in the spectrum of causative organisms of acute endophthalmitis and the ophthalmic procedures which are now commonly performed; improvements in surgical techniques, including the development of small-gauge micro-incision vitrectomy surgery (MIVS); and the widespread availability of fourth-generation fluoroquinolones. These developments may account for deviations in current practice patterns from the recommendations of the EVS. In this review, we consider newer evidence in the diagnosis and management of endophthalmitis. All data presented in this article were gathered following approval from the local research ethics committee.
Classification
Endophthalmitis may be classified by the mode of inoculation into (i) exogenous endophthalmitis, in which the pathogen is introduced directly into the eye (e.g. post-trauma or surgery), or (ii) endogenous endophthalmitis, in which the pathogen gains access internally (e.g. via the haematogenous spread of mycotic emboli). Post-operative endophthalmitis can be further classified as acute, defined by onset within 6 weeks post-operatively, or chronic, where onset occurs 6 or more weeks after surgery.
Diagnosis
Endophthalmitis is a clinical diagnosis, which may be supported by ancillary investigations. Symptoms include redness, pain, reduced vision, watering or mucopurulent discharge, ocular and periocular swelling and hypopyon. Diagnosis is supported by microscopy, culture and sensitivity (MC&S), and more recently by pan-bacterial polymerase chain reaction (PCR) techniques (e.g. through amplification of conserved regions encoding the microbial 16S ribosomal subunit). Collection of anterior chamber and vitreous samples, either with a vitrector in a PPV, or with a needle in a ‘tap and inject’ setting, should ideally precede the administration of intravitreal antibiotics, and the samples delivered to a forewarned microbiologist for gram stain, culture and microbial sensitivity testing [3]. However, in settings where a ‘dry’ vitreous tap is obtained, antibiotic injection should not be deferred to obtain a sample. Considering the rapid doubling times of bacteria within the intraocular compartment, delays in administering antimicrobial therapy may have devastating consequences. Furthermore, newer detection methods such as PCR do not require viable organisms to return a ‘positive’ sample. Therefore, they will frequently remain positive despite the administration of antibiotics (70% vs 9% for culture) [4].
Incidence and Risk Factors
The incidence of endophthalmitis depends on the mode of inoculation. The most recent reports suggest an incidence of between 1/2000 to 1/3333 [5] following cataract surgery. The European Society of Cataract and Refractive Surgeons (ESCRS) study found that clear corneal incision, silicone intraocular lens implants (IOLs) and surgical complications (e.g. rupture of the lens capsule) significantly increased the risk of endophthalmitis. In contrast, the use of intracameral cefuroxime significantly reduced its risk [6].
Post-intravitreal injection (IVI) endophthalmitis has an incidence of about 1/3000 [7]. Risk factors include advanced age, diabetes mellitus, blepharitis and poor patient cooperation during injection [7].
The reported rates of bleb-related endophthalmitis vary from 1.3%/patient/year for superior blebs to 7.8%/patient/year for inferior blebs [8,9,10]. Risk factors include the use of anti-fibrotic agents, chronic bleb leak, a thin avascular bleb, bleb manipulation, bacterial conjunctivitis, blepharitis, accidental trauma, epithelial drying, young age and male sex [11,12,13,14,15].
The incidence of endophthalmitis post-PPV is low, though there is a large spread in the reported incidence (1/1000 to 1/5000) [5]. The removal of vitreous as a growth medium for bacteria contributes to the low rates of PPV-related endophthalmitis.
Measures taken to reduce the risk of post-operative endophthalmitis include management of ocular surface disease before surgery, including blepharitis, which is associated with increased ocular surface microbial load, the application of povidone-iodine 5–10% to the cornea, conjunctival sac and periocular surface for 3 min before surgery, the use of face masks and meticulous sterilisation of instruments.
Causative Organisms
The causative organisms in endophthalmitis are a function of the mode of inoculation, geographical location and local practices. The most commonly cultured organisms from vitreous samples from eyes with acute endophthalmitis post-cataract surgery are gram-positive bacteria. [24,25,26] Staphylococcus epidermidis is the commonest causative organism in the Western Hemisphere.
Virulence factors of the causative pathogen, such as motility, enzyme production (e.g. pneumolysin) and biofilm production, influence the clinical course. The EVS found significant differences between bacterial species with regard to virulence and final visual acuity (VA) outcomes [2]. Studies have demonstrated that negative cultures, Staphylococcus spp. and post-cataract surgery endophthalmitis are associated with more favourable visual outcomes [16, 17]. Endophthalmitis following other intraocular procedures generally has poorer visual outcomes. This may be related to the effects of the disease requiring treatment (e.g. neovascular age-related macular degeneration [AMD]) and/or differences in the spectrum of causative organisms, which is skewed towards more virulent pathogens following surgical procedures other than cataract [16, 18]. Visual prognosis is guarded when Streptococcus spp. or gram-negative microbes are involved [3, 19]. Outcomes for endophthalmitis secondary to Streptococcus spp. are notoriously poor, with a final VA less than 20/400 in 50–80% of cases and a significant proportion resulting in evisceration or enucleation [20,21,22]. Negative cultures may indicate a lower bacterial load, earlier diagnosis or non-infectious aetiology, all of which may contribute to better clinical outcomes.
In the past, cataract extraction was the most commonly performed intraocular procedure when the EVS was conducted: it was, therefore, the most frequent cause of acute post-operative endophthalmitis. However, with the subsequent development of anti-vascular endothelial growth factor (anti-VEGF) therapy for the management of age-related macular degeneration (AMD), diabetic retinopathy and vascular occlusive disease, intravitreal injections have now become the most common penetrating ocular procedure [23].
Streptococcus spp. are an important cause of post-IVI endophthalmitis and bleb-associated endophthalmitis. In culture-positive cases of post-intravitreal injection acute endophthalmitis, Streptococcus-associated endophthalmitis is up to three times more common following IVI when compared to other forms of intraocular surgery [18]. At Sydney Eye Hospital during 2007–2010 inclusive, post-IVI endophthalmitis was presented earlier, resulted in poorer outcomes and was associated with increased odds of Streptococcus spp. infection when compared to post-cataract extraction (CE)/IOL infection [17]. Given that Streptococcus spp. constitute approximately 40% of the salivary flora [27], it was postulated that the higher incidence of Streptococcus spp. infection following intravitreal injection reflects aerosolisation of saliva from the proceduralist or patient, which may contaminate the operative field [18] (see Table 1). Consequently, the routine wearing of face masks by ophthalmologists and asking patients to refrain from talking when performing injections was incorporated in the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) guidelines [28]. Such guideline-driven changes in practice may explain why, more recently, there has been a statistically significant reduction in the proportion of Streptococcus spp. infection post-IVI at the same tertiary referral service (July 2012–June 2017) without increased odds of Streptococcus spp. endophthalmitis following intravitreal injections [23]. Table 1 presents a summary of causative organisms in acute post-intravitreal injection endophthalmitis cases in patients presenting to Sydney Eye Hospital during 2007–2010 versus 2012–2017. Decreased rates of Streptococcus spp. infections coincided with the introduction of national guidelines directed at minimising the contamination of surgical fields with oral flora.
Multiple studies have associated post-injection endophthalmitis with earlier presentation and worse visual outcomes than post-cataract surgery endophthalmitis [17]. However, the earlier presentation could not be attributed to an increased incidence of Streptococcus spp. infection reported in some studies and may reflect the increased ability of inoculated organisms to multiply in the vitreous compared to the anterior chamber [29].
Bleb-associated endophthalmitis is usually associated with more virulent microorganisms, such as Streptococcus spp., Haemophilus, and gram-negative organisms [30, 31]. Onset can occur months to years after filtration surgery [30]. Although the onset of endophthalmitis is delayed, inoculation is presumed to be acute and due to intraocular migration of causative organisms such as Streptococcus spp. through iatrogenic fistulas or across intact conjunctival epithelium (Streptococcus spp. can penetrate an intact conjunctival epithelium) [20, 32]. Bacteria may subsequently act as a nidus within a bleb with direct communication to the intraocular compartment. A retrospective study of 61 cases over a 10-year period by Almeida et al. found that the best outcomes of post-surgical endophthalmitis were encountered in post-cataract cases. In contrast, the worst outcomes occurred in cases of bleb-related endophthalmitis [33]. Therefore, it has been proposed that PPV is likely to be required in these latter cases, given the aggressive organisms involved and the poor anticipated visual outcomes [31].
Endogenous endophthalmitis results from the haematogenous spread of organisms from a source of infection and accounts for less than 10% of all endophthalmitis. Depending on the source, there is a wide range of causative organisms, including fungi such as Candida spp., often seen in association with so-called central line and intravenous drug use [34]; gram-positive bacteria such as Streptococcus spp. secondary to endocarditis, Staphylococcus aureus from cutaneous infections, Bacillus spp. as a result of intravenous drug use; and gram-negative bacteria such as enteric organisms, e.g. Escherichia Coli and Klebsiella in diabetics, urinary tract infection and liver abscess [35, 36]. Fungal and gram-negative endophthalmitis are generally associated with poorer visual outcomes than endophthalmitis secondary to gram-positive organisms.
Vitreous growth rates of bacteria are exponential over the first 24 h, with typically a tenfold increase in the first 3 h. Therefore, the timely delivery of antibiotics is essential in limiting bacterial loads.
Management
‘Tap and Inject’
It is generally agreed that empirical broad-spectrum antibiotics are required in the initial management of post-procedural endophthalmitis. A combination of two intravitreal antibiotics to ensure sufficient coverage of both gram-positive and gram-negative bacteria is recommended, with vancomycin 1.0 mg/0.1 ml to cover gram-positive organisms and ceftazidime 2.25 mg/0.1 ml to cover gram-negative organisms as first-line therapy [37, 38]. The two drugs form a white precipitate when mixed. For this reason, many surgeons opt to deliver these drugs in separate syringes using separate needles (though both the precipitate and the supernatant are reported to be efficacious) (40). In patients allergic to cephalosporins, an aminoglycoside such as amikacin 0.4 mg/0.1 ml can be used instead of ceftazidime. Benzylpenicillin 0.18 mg/0.1 ml can be used instead of ceftazidime in cases of confirmed or presumed Streptococcus spp. infection. Experimental studies have documented the safety and efficacy of intravitreal fluoroquinolones, including levofloxacin and moxifloxacin, against causative intraocular organisms [39,40,41].
A recent prospective study conducted by Sharma et al. found a significantly higher level of drug-resistant organisms in post-traumatic endophthalmitis (PTE), which accounted for 60% of patients with antibiotic resistance [42]. Consequently, the authors recommended using newer-generation intravitreal antibiotics like piperacillin and tazobactam for PTE [42]. Fungal endophthalmitis was the most common form of endogenous endophthalmitis, accounting for up to 50% of patients. This underlines the importance of empirical broad-spectrum antifungal cover for endogenous endophthalmitis of unknown aetiology. In such cases, amphotericin B 5 μg or voriconazole 100 μg (the intravitreal treatments of choice for suspected fungal endophthalmitis) are given in conjunction with intravitreal vancomycin and ceftazidime.
Repeat intravitreal injection of antimicrobials is sometimes performed, usually after at least 48 h, and tailored to sensitivity results. However, the decision to re-inject antibiotics should be considered carefully, as repeat injection may increase the risk of retinal toxicity. For example, 100% retinal toxicity rates with three intravitreal doses of 1 mg vancomycin combined with 400 µg amikacin or 200 µg gentamicin have been observed in rabbit eyes [43]. Furthermore, antibiotic concentrations appear to remain at bactericidal levels at 3–4 days post-injection [43], and repeat injection may result in retinotoxic levels, at least in some patients [44].
Clinical reports are conflicted on the utility of intravitreal dexamethasone 0.4 mg/0.1 ml in treating immune pathology in bacterial endophthalmitis [45,46,47,48]. Although some earlier studies postulated that intravitreal steroids might reduce antimicrobial efficacy, more recent studies have demonstrated no adverse effects of intravitreal dexamethasone [48], with faster resolution implied by ‘less need for repeat intravitreal antibiotics’ [48]. Although there is a lack of definitive evidence for or against, intravitreal dexamethasone at 0.4 mg in 0.1mL is commonly used in conjunction with antibiotics to treat bacterial endophthalmitis. It should furthermore be noted that the EVS protocol included systemic steroids. In cases where there is a suspicion of fungal endophthalmitis, intravitreal steroids are routinely avoided due to concerns regarding fulminant infection [49].
Systemic Antibiotics
The EVS findings did not support the addition of intravenous antibiotics (amikacin plus ceftazidime or amikacin plus ciprofloxacin in patients allergic to cephalosporins) [2]. However, intravenous amikacin and ceftazidime have been shown to have poor intraocular penetration [50, 51] (although ocular bioavailability may be improved with blood–retina barrier [BRB] breakdown). Ciprofloxacin has excellent ocular penetration and bioavailability when delivered orally, with some studies suggesting vitreous levels to be bactericidal [53]. However, in the EVS, fluoroquinolones were only given to patients with suspected cephalosporin allergies. The EVS took place before the availability of oral fourth-generation fluoroquinolones (e.g. moxifloxacin), which have broad coverage of gram-positive and gram-negative bacteria, excellent ocular and vitreous penetration [52, 54, 55], and excellent bioavailability when administered orally. In our unit, a 10-day course of 750 mg oral ciprofloxacin twice daily or 400 mg oral moxifloxacin daily is incorporated into treatment as part of therapy. Hooper et al. [55] compared the use of ciprofloxacin with moxifloxacin in 72 eyes with culture-positive acute bacterial endophthalmitis. They suggested clinical superiority of oral moxifloxacin 400 mg once daily for 10 days over ciprofloxacin. Patients treated with moxifloxacin had a quicker resolution of hypopyon, reduced need for repeat intravitreal injection and a better chance of a good clinical outcome, even when adjusting for resistance to ciprofloxacin [56]. However, fluoroquinolones are excreted in sweat, and have been found to increase colonisation with methicillin-resistant Staphylococcus aureus (MRSA), so in some units the use of these drugs is discouraged [57].
Surgery
The EVS is the only RCT to compare medical and surgical management (PPV vs vitreous tap and injection of antibiotics) in acute post-operative endophthalmitis. The primary outcome was best-corrected visual acuity (BCVA) and clinical/photographic assessment of media clarity at 9 months.
In this trial, PPV was defined as vitreous clearance of 50% or more [2]. The aims of PPV included reducing bacterial load, toxins and inflammatory mediators and the removal of vitreous as a growth medium for bacteria. It concluded that immediate (< 6 h of presentation) PPV improved visual outcome in patients who presented with perception of light (LP) vision, with three times the likelihood of final vision of 6/12 or better. However, no such benefit could be demonstrated in patients presenting with vision of hand movements (HM) or better [2]. An exception to this was observed in diabetic patients, where post hoc analysis found vitrectomy beneficial even if vision was better than LP at presentation.
Perceived shortcomings of the EVS study include the following: a limited/core PPV was performed; treatment could occur up to 6 h following presentation (animal models suggest that early PPV at ≤ 4 h following inoculation is of benefit [57]); systemic antibiotics with limited ocular penetrance were used; the incidence and causative organisms have changed since the study; and significant developments in PPV equipment and techniques have occurred since the study was performed.
Developments in Surgical Equipment and Techniques
In the EVS, PPV was defined as 50% removal of vitreous and was conducted with 20-gauge instrumentation [2]. Since its publication, the subsequent development of micro-incision vitrectomy surgery (MIVS) has meant that most modern-day PPV is conducted with 23-gauge and 25-gauge instruments. Small-gauge surgery obviates the need for peritomy and is often sutureless; this results in reduced surgical times. When compared to 20-gauge surgery, it is argued that MIVS results in reduced intra-operative trauma and fewer complications such as so-called port tears and subsequent retinal detachments, reduced post-operative inflammation and faster post-operative visual recovery [58,59,60].
Advances in surgical techniques have meant that PPV in the context of endophthalmitis frequently involves induction of posterior vitreous detachment (PVD) and a greater than 50% clearance of vitreous. It is argued that there is therefore greater reduction of bacterial load and greater clearance of toxins and inflammatory debris than that achieved in EVS. Recent studies have suggested that early PPV in the context of endophthalmitis may even reduce the incidence of retinal detachment [60].
Pars Plana Vitrectomy
Recent surveys of vitreoretinal surgeons have found that the majority perform PPV if there is clinical worsening within 48 h following tap and injection of antibiotics [61]. Additionally, it has been argued that PPV should be considered sooner in higher-risk eyes. In particular, Kuhn and Gini report excellent outcomes for early ‘complete’ PPV in endophthalmitis. However, this study (and all subsequent studies) is limited by the absence of a control group [62].
A recent retrospective study by Ho et al. of 64 consecutive patients who underwent PPV within 72 h of presentation with acute-onset infectious endophthalmitis secondary to a mixture of cataract surgery, intravitreal injections, glaucoma filtration surgery, endogenous endophthalmitis and trauma, found significant visual gains in patients who presented with HM vision or worse [16]. A recent retrospective study by Sridhar et al. of 70 patients undergoing early PPV for acute post-operative endophthalmitis found evidence for a reduced likelihood of evisceration or enucleation in Streptococcus spp. endophthalmitis when compared to previous reports [63]. The authors argued that there might be an anatomically protective benefit of PPV that prevents either phthisis or panophthalmitis from developing [63].
Birnbaum and Gupta retrospectively explored the role of PPV in the treatment of fungal endogenous endophthalmitis (FEE) in six eyes that underwent PPV within 24 h of presentation in addition to intravitreal vancomycin (1 mg/ml), ceftazidime (2.25 mg/ml) and amphotericin B (5 μg/ml). They report that four out of six eyes achieved final vision of 6/12 or better. They suggest that this compares favourably to other reported outcomes, with visual acuity of counting fingers or better reported in only 22–41% of cases [64, 65]. This was attributed to the fact that all their patients received PPV followed by intravitreal antifungals within 24 h of suspected endophthalmitis, compared to other studies where PPV was delayed and only conducted after eyes did not respond to medical therapy or where PPV was reserved for severe cases only. Based on their findings, Birnbaum and Gupta recommended a PPV within 24 h in high-risk individuals with suspected FEE for prompt diagnosis and improved outcomes [64]. However, Birnbaum and Gupta’s study was limited by its small sample size, and it is difficult to draw a firm conclusion from their data [64]. Another retrospective study of 44 eyes with Candida FEE found that early PPV significantly reduced the risk of retinal detachment: two of 26 eyes undergoing PPV within a week progressed to retinal detachment, compared to seven of 17 eyes that did not undergo PPV [65]. Technical advances in PPV, including MIVS and improved visualisation through wide-angle viewing systems, may be responsible for better reported visual outcomes in recent retrospective reports.
In endogenous endophthalmitis, the mainstay of management includes the diagnosis and treatment of the infective nidus. PPV in the context of endogenous endophthalmitis may be both diagnostic and therapeutic, as the condition may have an indolent course with non-specific inflammatory symptoms. Thus it can be misdiagnosed in 16–50% of cases [66]. With sensitivity ranging from 40 to 70%, vitreous biopsy has a higher diagnostic yield than aqueous or vitreous needle aspiration [67,68,69].
Recent data from our own centre (185 consecutive admissions for acute post-procedural endophthalmitis over 5 years) suggests that patients undergoing early PPV (≤ 24 h) have greater improvements in vision compared to patients receiving initial medical management. The mean change in 3-month versus presentation logMAR acuity for patients undergoing early PPV was −1.47 ± 0.76 logMAR (mean ± SD), whilst the mean change for patients undergoing late PPV/T&I was −1.14 ± 0.90 logMAR (P = 0.007) (see Table 2). Furthermore, patients in the early PPV group were more likely to achieve final acuity of 20/40 or better (24.3% vs 12.6%, OR 2.27, P = 0.047). Patients undergoing early vitrectomy also had worse presenting acuity (2.34 ± 0.37 and 1.81 ± 0.76 logMAR, respectively, P = 0.0001). For this reason, there is no statistically significant difference between early vitrectomy and initial medical management for change in BCVA on analysis of covariance (ANCOVA) with presenting acuity as the covariate (P = 1.00). Those undergoing early PPV were more likely to have positive cultures (73% vs 36%, OR 0.202, P = 9.4 × 10–7).
Oil Tamponade
The effect of oil tamponade as an adjuvant to PPV was not explicitly examined in the EVS. Silicone oil has antimicrobial properties [70], and studies have demonstrated a more rapid control of infection and improvement in vision in eyes undergoing vitrectomy with silicone oil tamponade compared to vitrectomy alone [71]. However, silicone oil may be ineffective against some organisms, such as Propionibacterium acnes, the most common causative organism in chronic post-operative endophthalmitis [72]. Disadvantages to oil tamponade include further surgery for oil removal, oil emulsification, elevated intraocular pressure, silicone-oil induced inflammation and band keratopathy in long-term retention. In practice, oil tamponade is considered when endophthalmitis is associated with retinal detachment, inability to perform a satisfactory ‘search’ for retinal breaks before completing surgery or when severely damaged or necrotic retina are present [70, 71].
Current Approach
The prognosis following acute infective endophthalmitis is dependent on the virulence and inoculum size of the causative organism, the time to presentation, the time to initiation of appropriate therapy and the patient’s immune status [3, 73, 74]. Risk factors for poor outcomes include rapid onset, poorer presenting vision, a causative organism other than coagulase-negative Staphylococcus, corneal oedema, a hypopyon larger than 1.5 mm, extensive media haze and absence of fundus visibility, and the presence of retinal detachments or intraocular foreign bodies [75,76,77]. Presenting vision is the strongest predictor of visual prognosis [76].
Since the EVS, the primary management of acute endophthalmitis has been the immediate intravitreal injection of empirical broad-spectrum antibiotics. However, the success rate of PPV in the management of acute endophthalmitis (defined as final VA of 6/120 or better) has improved over the last three decades, ranging from 42 to 73% [38]. The 2013 ESCRS guidelines suggest that immediate and complete PPV in conjunction with intravitreal antibiotics is now the gold standard for endophthalmitis management [38]. Immediate ‘tap and inject’ is described in the same guidelines as the ‘silver standard’ [38]. However, the justification for this approach appears to rest largely on a Latin aphorism (Ubi pus, ibi evacua [where there is pus, evacuate it]). As alluded to above, time is of the essence in the management of endophthalmitis. According to the ESCRS 2013 guidelines, PPV should not delay the administration of intravitreal antibiotics, which should be given immediately following vitreous tap if a PPV would be delayed or unavailable [38].
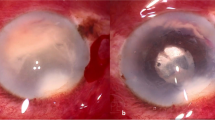
Our approach to vitrectomy in endophthalmitis is to simultaneously obtain a view and ‘clearance’ of the intraocular compartment from anterior to posterior.
Surgery commences with a repeat inspection of the eye. If there is a poor view, an anterior chamber infusion is placed initially. A posterior chamber infusion may be placed in the presence of a sufficient view: a 6 mm cannula can be used, or the light pipe introduced to confirm correct placement of the ports through visualisation of its tip. Clearance of the anterior chamber may include washout, though often fibrinous pupillary membranes must be removed with the aid of forceps and an ophthalmic viscoelastic device (see video). Once a satisfactory clearance of the anterior chamber is obtained, the anterior vitreous is cleared first, progressing posteriorly as the view improves. A pre-operative B-scan is necessary in all cases where the ocular fundus cannot be visualised. In the presence of thick purulent material within the vitreous compartment, the surgeon must be vigilant for any signs of unrecognised retinal detachment, such as bleeding from the cut edge of an apparent purulent posterior vitreous face.
Vitrectomy for endophthalmitis: video summary of the surgical approach. See text for details. (MP4 118688 KB)
Discussion
It has been suggested that PPV hastens and improves recovery [2] by the removal of vitreous, a potential growth medium for bacteria [78]. Furthermore, it is proposed to reduce the bacterial load, toxins and pus [6] by removing vitreous membranes and slime that could otherwise lead to significant increases in bacterial minimum inhibitory concentration (MIC) or mature to cause retinal detachment, and by improving intravitreal circulation and thus the penetration of injected antibiotics [78, 79]. Additionally, PPV is associated with better vitreous sampling for culturing [6], which can lead to improved identification of the causative organism and its antibiotic sensitivity, which may allow targeted antimicrobial management.
Since the publication of the key findings of the EVS, PPV has evolved significantly. This has arguably led vitreoretinal surgeons worldwide to lower their threshold for PPV in endophthalmitis [60]. Although there have been concerns that operating on inflamed eyes may result in iatrogenic complications, some recent studies (though limited by the absence of a control group) have demonstrated favourable functional and anatomical outcomes, even when PPV was carried out in eyes with better than LP vision [34, 35]. Prompt management and advances in surgical equipment and techniques are thought to contribute to these results [6, 60].
Indications for early vitrectomy include clinical deterioration despite intravitreal antibiotics, concomitant retained lens material or retinal detachment, poor presenting vision of HM or worse [2], absence of red reflex, patient groups known to do more poorly such as diabetic patients [2], and endophthalmitis more likely associated with more virulent pathogens, for example, post-trauma, bleb-related or secondary to intravitreal injections.
Disadvantages of PPV include an unsatisfactory or limited surgical view in phakic patients, intra-operative complications such as iatrogenic tears, retinal detachments and sympathetic ophthalmia, and theatre space and staff availability, which can hinder the provision of immediate PPV for patients with endophthalmitis in practice. Surgical considerations include the use of a longer infusion cannula (e.g. 6.0 mm) if visualisation is difficult, placing an anterior chamber infusion line first if dense vitritis renders intravitreal visualisation of the infusion cannula difficult, and avoiding aggressive peripheral vitrectomy if the view is inadequate. Modern wide-angle viewing systems improve visualisation during PPV. This, in addition to modern vitrectors with improved duty cycles, reduces the risk of intra-operative complications.
Since the EVS, both surgical and medical management have evolved. Although immediate PPV is now considered the gold standard in the ESCRS 2013 guidelines [38], this may not be practical in many centres due to limitations of theatre space and staff. Furthermore, data comparing outcomes following MIVS versus medical management remain limited. In the management of acute endophthalmitis, we recommend immediate intravitreal injection of antibiotics in all cases. PPV should be performed as soon as possible in patients presenting with LP vision, in those at high risk of more virulent causative pathogens, such as post-trauma or post-glaucoma filtration surgery, and in those not improving 48 h post tap and inject. Topical therapy including antibiotics (e.g. ofloxacin), steroids (e.g. dexamethasone) and cycloplegic eye drops (e.g. atropine) and a 10-day course of oral antibiotics (in our unit fluoroquinolones) according to local microbiological guidelines are recommended. Intravitreal dexamethasone, or a short course of oral steroids, can be given at the clinician’s discretion. Because of ongoing uncertainty regarding the benefit of PPV in endophthalmitis, a repeat RCT re-investigating this issue is long overdue.
References
Maneschg OA, Volek E, Németh J, Somfai GM, Géhl Z, Szalai I, Resch MD. Spectral domain optical coherence tomography in patients after successful management of postoperative endophthalmitis following cataract surgery by pars plana vitrectomy. BMC Ophthalmol. 2014;2(14):76.
Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study: a randomised trial of immediate vitrectomy and of intravenous antibiotics for the treatment of post- operative bacterial endophthalmitis. Arch Ophthalmol. 1995;113(12):1479–96.
Pathengay A, Flynn HW Jr, Isom RF, Miller D. Endophthalmitis outbreaks following cataract surgery: causative organisms, etiologies and visual acuity outcomes. J Cataract Refract Surg. 2012;38(7):1278–82.
Chiquet, et al. Eubacterial PCR for bacterial detection and indentification in 100 acute post cataract surgery endophthalmitis. Invest Ophthalmol Vis Sci. 2008;49:1971.
Clarke B, Williamson TH, Gini G, Gupta B. Management of bacterial postoperative endophthalmitis and the role of vitrectomy. Surv Ophthalmol. 2018;63(5):677–93. https://doi.org/10.1016/j.survophthal.2018.02.003.
Barry P, Cordoves L, Gardner S. ESCRS guidelines for prevention and treatment of endophthalmitis following cataract surgery. 2013.
Hsu J, Gerstenblith AT, Garg SJ, Vander JF. Conjunctival flora antibiotic resistance patterns after serial intravitreal injections without post-injection topical antibiotics. Am J Ophthalmol. 2014;157(3):514-518.e1.
Wolner B, Liebmann JM, Sassani JW, Ritch R, Speaker M, Marmor M. Late bleb-related endophthalmitis after trabeculectomy with adjunctive 5-fluorouracil. Ophthalmology. 1991;98(7):1053–60.
DeBry PW, Perkins TW, Heatley G, Kaufman P, Brumback LC. Incidence of late-onset bleb-related complications following trabeculectomy with mitomycin. Arch Ophthalmol. 2002;120(3):297–300.
Vaziri K, Kishor K, Schwartz SG, Maharaj AS, Moshfeghi DM, Moshfeghi AA, et al. Incidence of bleb-associated endophthalmitis in the United States. Clin Ophthalmol (Auckl, NZ). 2015;9:317.
Jampel HD, Quigley HA, Kerrigan-Baumrind LA, Melia BM, Friedman D, Barron Y. Risk factors for late-onset infection following glaucoma filtration surgery. Arch Ophthalmol. 2001;119(7):1001–8.
Soltau JB, Rothman RF, Budenz DL, Greenfield DS, Feuer W, Liebmann JM, et al. Risk factors for glaucoma filtering bleb infections. Arch Ophthalmol. 2000;118(3):338–42.
Mochizuki K, Jikihara S, Ando Y, Hori N, Yamamoto T, Kitazawa Y. Incidence of delayed onset infection after trabeculectomy with adjunctive mitomycin C or 5-fluorouracil treatment. Br J Ophthalmol. 1997;81(10):877–83.
Leng T, Miller D, Flynn HW Jr, Jacobs DJ, Gedde SJ. Delayed-onset bleb-associated endophthalmitis (1996–2008): causative organisms and visual acuity outcomes. Retina. 2011;31(2):344–52.
Wallin O, Al-ahramy AM, Lundström M, Montan P. Endophthalmitis and severe blebitis following trabeculectomy. Epidemiology and risk factors; a single-centre retrospective study. Acta Ophthalmol. 2014;92(5):426–31.
Ho IV, Fernandez-Sanz G, Levasseur S, Ting E, Liew G, Playfair J, Downie J, Gorbatov M, Hunyor AP, Chang AA. Early pars plana vitrectomy for treatment of acute infective endophthalmitis. Asia Pac J Ophthalmol (Phila). 2019;8(1):3–7.
Simunovic MP, Rush RB, Hunyor AP, et al. Endophthalmitis following intravitreal injection versus endophthalmitis following cataract surgery: clinical features, causative organisms and post-treatment outcomes. Br J Ophthalmol. 2012. https://doi.org/10.1136/bjophthalmol-2011-301439.
McCannel CA. Meta-analysis of endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents: causative organisms and possible prevention strategies. Retina. 2011;31:654e61.
Han DP, Wisniewski SR, Wilson LA, Barza M, Vine AK, Doft BH, et al. Spectrum and susceptibilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am J Ophthalmol. 1996;122(1):1–17.
Kuriyan AE, Weiss KD, Flynn HW Jr, et al. Endophthalmitis caused by streptococcal species: clinical settings, microbiology, management, and outcomes. Am J Ophthalmol. 2014;157:774–80.
Moshfeghi AA, Rosenfeld PJ, Flynn HW Jr, et al. Endophthalmitis after intravitreal anti-vascular endothelial growth factor antagonists: a six year experience at a university referral center. Retina. 2011;31:662–8.
Miller JM, Scott IU, Flynn HW Jr, Smiddy WE, Corey RP, Miller D. Endophthalmitis caused by Streptococcus pneumoniae. Am J Ophthalmol. 2004;138:231–6.
Ong AP, Angbue Te N, Zagora SL, Symes RJ, Yates W, Chang AA, McCluskey PJ, Simunovic MP. Post-surgical versus post-intravitreal injection endophthalmitis: changing patterns in causative flora. Clin Exp Ophthalmol. 2019;47(1):57–62.
Aaberg TM Jr, Flynn HW Jr, Schiffman J, et al. Nosocomial acute-onset postoperative endophthalmitis survey. A 10-year review of incidence and outcomes. Ophthalmology. 1998;105:1004e10.
Eifrig CW, Flynn HW Jr, Scott IU, et al. Acute-onset postoperative endophthalmitis: review of incidence and visual outcomes. Ophthalmic Surg Lasers. 2002;33:373e8.
Wykoff CC, Parrott MB, Flynn HW Jr, et al. Nosocomial acute-onset postoperative endophthalmitis at a university teaching hospital. Am J Ophthalmol. 2010;150:392e8.e2.
Gordon DF, Jong BB. Indigenous flora from human saliva. Appl Microbiol. 1968;16:428e9.
RANZCO. Guidelines for Performing Intravitreal Therapy 2012. Accessed 10 January 2018. Version 3. Available from: https://ranzco.edu/ArticleDocuments/176/IVI%20Guidelines%20for%20Performing%20Intravitreal%20Therapy%202017.pdf.aspx?Embed=Y.
Levison AL, Mendes TS, Bhisitkul R. Post procedural endophthalmitis: a review. Expert Rev Ophthalmol. 2013;8(1):45–62.
Almeida DR, Miller D, Alfonso EC. Anterior chamber and vitreous concordance in endophthalmitis: implications for prophylaxis. Arch Ophthalmol. 2010;128(9):1136–9.
Al-Turki TA, Al-Shahwan S, Al-Mezaine HS, Kangave D, Abu El-Asrar AM. Microbiology and visual outcome of bleb-associated endophthalmitis. Ocul Immunol Inflamm. 2010;18(2):121–6.
Katz LJ, Cantor LB, Spaeth GL. Complications of surgery in glaucoma. Early and late bacterial endophthalmitis following glaucoma filtering surgery. Ophthalmology. 1985;92:959–63.
Almeida DR, Chin EK, Shah SS, Bakall B, Gehrs KM, Boldt HC, Russell SR, Folk JC, Mahajan VB. Comparison of microbiology and visual outcomes of patients undergoing small-gauge and 20-gauge vitrectomy for endophthalmitis. Clin Ophthalmol. 2016;10:167–72.
Brod RD, Flynn HW Jr. Endophthalmitis: current approaches to diagnosis and therapy. Curr Opin Infect Dis. 1993;6:628–37.
Margo CE, Mames RN, Guy JR. Endogenous Klebsiella endophthalmitis. Report of two cases and review of the literature. Ophthalmology. 1994;101:1298–301.
Tseng CY, Liu PY, Shi ZY, Lau YJ, Hu BS, Shyr JM, et al. Endogenous endophthalmitis due to Escherichia coli: case report and review. Clin Infect Dis. 1996;22:1107–8.
ESCRS Guidelines on prevention, investigation and management of postoperative endophthalmitis. In: Peter Barry, Wolfgang Behrens-Baumann, Uwe Pleyer & David Seal, editors. The European Society for Cataract & Refractive Surgeons, Version 2 August 2007.
Group EES. Prophylaxis of postoperative endophthalmitis following cataract surgery: 740 Adv Ther (2016) 33:727–746 results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007;33(6):978–88.
Kazi AA, Jermak CM, Peyman GA, Aydin E, Riazi-Esfahani M. Intravitreal toxicity of levofloxacin and gatifloxacin. Ophthalmic Surg Lasers Imaging Retina. 2006;37:224–9.
Aydin E, Kazi AA, Peyman GA, Esfahani MR. Intravitreal toxicity of moxifloxacin. Retina. 2006;26:187–90.
Gao H, Pennesi ME, Qiao X, et al. Intravitreal moxifloxacin: retinal safety study with electroretinography and histopathology in animal models. Invest Ophthalmol Vis Sci. 2006;47:1606–11.
Sharma YR, Gaur N, Chandra P, Takkar B. Predictors of visual outcomes and microbial profile in endophthalmitis. Ophthalmic Surg Lasers Imaging Retina. 2016;47(11):991–8.
Oum BS, D’Amico DJ, Wong KW. Intravitreal antibiotic therapy with vancomycin and aminoglycoside. An experimental study of combination and repetitive injections. Arch Ophthalmol. 1989;107(7):1055–60.
Gan, et al. Intravitreal vancomycin and gentamicin concentrations in patients with postoperative endophthalmitis. BJO. 2001;85:1289.
Gan IM, Ugahary LC, van Dissel JT, et al. Intravitreal dexamethasone as adjuvant in the treatment of postoperative endophthalmitis: a prospective randomised trial. Graefes Arch Clin Exp Ophthalmol. 2005;243:1200–5.
Das T, Jalali S, Gothwal VK, Sharma S, Naduvilath TJ. Intravitreal dexamethasone in exogenous bacterial endophthalmitis: results of a prospective randomised study. Br J Ophthalmol. 1999;83:1050–5.
Hall EF, Scott GR, Musch DC, Zacks DN. Adjunctive intravitreal dexamethasone in the treatment of acute endophthalmitis following cataract surgery. Clin Ophthalmol. 2008;2:139–45.
Shah GK, Stein JD, Sharma S, et al. Visual outcomes following the use of intravitreal steroids in the treatment of postoperative endophthalmitis. Ophthalmology. 2000;107:486–9.
Moisseiev E, Abbassi S, Park SS. Intravitreal dexamethasone in the management of acute endophthalmitis: a comparative retrospective study. Eur J Ophthalmol. 2017;27(1):67–73.
El-Massry A, Meredith TA, Aguilar HE, et al. Aminoglycoside levels in the rabbit vitreous cavity after intravenous administration. Am J Ophthalmol. 1996;122:684–9.
Aguilar HE, Meredith TA, Shaarawy A, et al. Vitreous cavity penetration of ceftazidime after intravenous administration. Retina. 1995;15:154–9.
Hariprasad SM, Shah GK, Mieler WF, et al. Vitreous and aqueous penetration of orally administered moxifloxacin in humans. Arch Ophthalmol. 2006;124(2):178–82.
Fuller JJ, Lott MN, Henson NM, et al. Vitreal penetration of oral and topical moxifloxacin in humans. Am J Ophthalmol. 2007;143(2):338–40.
Lott MN, Fuller JJ, Hancock HA, et al. Vitreal penetration of oral moxifloxacin in humans. Retina. 2008;28(3):473–6.
Hooper CY, Lightman SL, Pacheco P, Tam PM, Khan A, Taylor SR. Adjunctive antibiotics in the treatment of acute bacterial endophthalmitis following cataract surgery. Acta Ophthalmol. 2012;90(7):e572–3.
Callegan MC, et al. Pathogenesis of gram-positive bacterial endophthalmitis. Infect Immun. 1999;67:3348.
Misra, et al. 23 Gauge sutureless vitrectomy and 20-gauge vitrectomy: a case series comparison. Eye (Lond). 2009;23(5):1187–91.
Tarantola RM, Graff JM, Somani R, et al. Temporal approach for small gauge pars plana vitrectomy combined with anterior segment surgery. Retina. 2012;32(8):1614–23.
Mahajan VB, Tarantola RM, Graff JM, et al. Sutureless triplanar sclerotomy for 23-gauge vitrectomy. Arch Opthalmol. 2011;129(5):585–90.
Sallam A, Tayler SRJ, Khan A, et al. Factors determining visual outcome in endogenous Candida endophthalmitis. Retina. 2012;32:1129–34.
Fliney GD, et al. Trends in treatment strategies for suspected bacterial endophthalmitis. Graefes Arch Clin Exp Ophthalmol. 2018;256:833–8.
Kuhn F, Gini G. Ten years after … are findings of the Endophthalmitis vitrectomy study still relevant today? Graefe’s Arch Clin Exp Ophthalmol. 2005;243(12):1197–9.
Birnbaum FA, Gupta G. The role of early vitrectomy in the treatment of fungal endogenous endophthalmitis. Retin Cases Brief Rep. 2016;10(3):232–5.
Sridhar, et al. Microbiologic spectrum and visual outcomes of acute-onset endophthalmitis undergoing therapeutic pars plana vitrectomy. Retina. 2017;37(7):1246–51.
Riddell J 4th, Comer GM, Kauffman CA. Treatment of endogenous fungal endophthalmitis: focus on new antifungal agents. Clin Infect Dis. 2011;52(5):648–53.
Binder MI, Chua J, Kaiser PK, et al. Endogenous endophthalmitis: an 18-year review of culture-positive cases at a tertiary care center. Medicine. 2003;82:97–105.
Zhang YQ, Wang WJ. Treatment outcomes after pars plana vitrectomy for endogenous endophthalmitis. Retina. 2005;25:746–50.
Shen X, Xu G. Vitrectomy for endogenous fungal endophthalmitis. Ocul Immunol Inflamm. 2009;17(148–152):11.
Lingappan A, Wykoff C, Albini T, et al. Endogenous fungal endophthalmitis: causative organisms, management Strategies, and visual acuity outcomes. Am J Ophthalmol. 2012;153:162–6.
Ozdamar A, Aras C, Ozturk R, Karacorlu M, Ercikan C. In-vitro antimicrobial activity of silicone oil against endophthalmitis causing agents. Retina. 1999;2:122–6.
Bali E, Huyghe P, Caspers L, Libert J. Vitrectomy and silicone oil in the treatment of acute endophthalmitis. Preliminary results. Bull Soc Belge Ophtalmol. 2003;288:9–18.
Arici C, Aras C, Tokman H, Torun M. An in vitro experimental study on the antimicrobial activity of silicone oil against anaerobic bacteria. Ocul Immunol Inflamm. 2016;24(2):173–7.
Chen X, Adelman RA. Microbial spectrum and resistance patterns in endophthalmitis: a 21-year (1988–2008) review in Northeast United States. J Ocul Pharmacol Ther. 2012;28(4):329–34.
Lemley CA, Han DP. Endophthalmitis: a review of current evaluation and management. Retina. 2007;27(6):662–80.
Lalwani GA, Flynn HW Jr, Scott IU, et al. Acute-onset endophthalmitis after clear corneal cataract surgery (1996–2005). Clinical features, causative organisms, and visual acuity outcomes. Ophthalmology. 2008;115(3):473–6.
Gupta A, Gupta V, Gupta A, et al. spectrum and clinical profile of post cataract surgery endophthalmitis in north India. Indian J Ophthalmol. 2003;51(2):139–45.
Fan JC, Niederer RL, von Lany H, Polkinghorne PJ. Infectious endophthalmitis: clinical features, management and visual outcomes. Clin Exp Ophthalmol. 2008;36(7):631–6.
Almeida DRP, Chin EK. Postoperative Infectious Endophthalmitis: Evolving Trends and Techniques. Practices have changed since publication of the EVS in the 1990s. Retina Today. September 2016.
Ness T, Pelz K, Hansen LL. Endogenous endophthalmitis: microorganisms, disposition and prognosis. Acta Ophthalmol Scand. 2007;85:852–6.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
Drs Shao, Yates, Ho, Chang and Simunovic meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author contributions
Manuscript writing (Emily H Shao, Matthew P Simunovic). Data generation & analysis (Matthew P Simunovic, Andrew A Chang, William B Yates, I-Van Ho). Critical review (Emily H Shao, William Yates, I-Van Ho, Andrew Chang, Matthew P Simunovic).
Disclosures
Drs Emily H Shao, William B Yates, I-Van Ho, Andrew A Chang and Matthew P Simunovic declare that they have no pertinent conflicts of interest.
Compliance with Ethics Guidelines
The data contained within the article were gathered following approval from the Local Research Ethics Committee.
Data Availability
Data generated or analysed during this study are included as supplementary information.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Shao, E.H., Yates, W.B., Ho, IV. et al. Endophthalmitis: Changes in Presentation, Management and the Role of Early Vitrectomy. Ophthalmol Ther 10, 877–890 (2021). https://doi.org/10.1007/s40123-021-00406-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-021-00406-6