Abstract
Introduction
The purpose of this study was to evaluate the efficacy and safety of iontophoretic collagen cross-linking (I-CXL) compared to epithelium-off standard collagen cross-linking (CXL) in treating the early stages of progressive keratoconus.
Methods
This retrospective cohort study at Oftaprof Clinic, Iasi, Romania included 40 eyes of 40 patients with progressive keratoconus stage I according to the Amsler classification who underwent I-CXL and the results were compared with a matched group of 40 eyes from 40 patients who received standard CXL. The follow-up period was 24 months. Uncorrected (UCVA) and corrected (CDVA) distance visual acuities, corneal topography, and pachymetry were evaluated in all patients.
Results
The mean patient age was 26.52 ± 3.77 years for the standard CXL group and 28.32 ± 4.91 for the I-CXL group. The mean UCVA and CDVA improved significantly in both groups. At 12 months, the improvement of UCVA was greater in the I-CXL group (P < 0.05). There was a statistically significant different trend in CDVA between groups with a more favorable outcome for the standard CXL group (P < 0.01). The manifest cylinder decreased by a mean of 0.962 ± 0.114 D in the epithelium-off CXL group and by 0.831 ± 0.082 D in the I-CXL group (P < 0.001). At 24 months, the K max values improved by 1.2 ± 0.199 D in the standard group and by 0.908 ± 0.177 D in the I-CXL group (P < 0.001).
Conclusion
All parameters either improved or remained unchanged after the iontophoretic collagen cross-linking intervention. I-CXL was found to be as effective as the standard technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Keratoconus (KC) is a degenerative eye disorder that progressively damages the internal structure of the cornea, which becomes cone-shaped and gets thinner, gradually causing visual impairment. The clinical findings in KC, such as astigmatism and various degrees of myopia, correspond to the stages of the disease [1]. The disorder is frequently diagnosed in adolescence and early adulthood and mostly affects men [2]. KC is a severe condition that requires early detection and treatment to stop it from progressing and thus prevent eyesight loss.
Riboflavin A and UVA-induced corneal collagen cross-linking (CXL) is currently one of the most efficient treatments for halting KC progression in both the short and long term [3–5]. Riboflavin has a small molecular weight (476 Da), a negative charge at physiological pH, and a high solubility in H2O. The CXL method increases the density and the stability of the cornea by inducing new cross-links between the collagen fibers of the cornea [6, 7]. The CXL method improves visual acuity by delaying or stopping the progression of keratoconus and in the long term may reduce the need for keratoplasty [8–10].
Keratoconus is associated with significantly impaired quality of life even in its early stages, and the problems it causes grow more severe with time [11]. The expected lifetime cost of treatment of keratoconus represents a significant economic impact and an important public health concern [12].
The standard protocol of CXL introduced by Wollensak et al. [13, 14] consists in removing the corneal epithelium, followed by an infusion of the cornea stroma with riboflavin solution and exposure to UVA radiation. However, despite its proven efficacy, the standard method of CXL has some important clinical drawbacks, including transient visual loss, a higher risk of infectious keratitis, or pain and haze caused by the invasive nature of the procedure [1, 15–17].
Modern medical approaches to keratoconus treatment use a transepithelial protocol to limit the side effects of standard CXL. Transepithelial CXL uses a special riboflavin solution allowing higher penetration through the intact epithelium owing to the addition of two enhancers: EDTA and trometamol. However, transepithelial CXL showed a limited efficacy in terms of keratoconus stabilization after 24 months of follow-up, caused by inadequate riboflavin penetration [18].
Recently, iontophoresis has been introduced into the transepithelial CXL protocol to preserve the benefits of the standard version while diminishing its side effects. Iontophoresis is an old medical technique that facilitates drug penetration into tissue using a small electric current [19, 20]. Iontophoresis has also been used in other medical fields such as neurology or dermatology for decades. Preclinical studies suggest that iontophoretic collagen cross-linking (I-CXL) is a promising technique for riboflavin delivery in cross-linking treatments, preserving the epithelium. Experimental studies on human cadaver corneas show that riboflavin penetration into the corneal stroma was greater and deeper with the iontophoresis imbibition method, compared to conventional epi-on, but did not reach the concentrations obtained with standard CXL [21]. Iontophoresis imbibition followed by UVA irradiation for 9 min at 10 mW led to less tissue damage and better stromal healing. By enhancing riboflavin penetration, iontophoresis decreases the time of intervention and improves the efficacy and safety of the CXL technique [19, 22]. However, there is limited clinical experience associated with this method; although it seems to be safe, the extent of its clinical benefit still needs to be further investigated. The reported results up to 2 years postoperatively indicate that I-CXL is effective in stabilizing progressive keratoconus and seems to be more comfortable for the patients [22–24].
The aim of the present study is to compare the results of I-CXL and standard CXL in terms of uncorrected visual acuity (UCVA), corrected distance visual acuity (CDVA), sphere, cylinder, and keratometry values after 24 months’ follow-up.
Methods
Study Design
This retrospective, single-center study included patients with progressive keratoconus who attended the Oftaprof Clinic of Iasi, Romania, between 1 January 2012 and 31 July 2015. The patients were identified using the computerized clinic record system; we included only those who attended every follow-up visit. The study was conducted on 40 eyes of 40 patients who received I-CXL treatment and were compared with a matched analysis on 40 eyes from 40 different patients who underwent standard CXL. All the patients signed an informed written consent at the time of the procedure. The study was approved by the local ethics committee according to the declaration of Helsinki of 1964, as revised in 2013.
Patients
Patients enrolled in the study met the following inclusion criteria: stage I keratoconus according to the Amsler–Krumeich grading system, documented progressive nature of the disease, age above 18 years, central corneal thickness (CCT) greater than 400 µm at the thinnest point, and endothelial cell density (ECD) greater than 2000 cell/mm2. Progression indicating necessity for treatment was documented by an increase of the maximum keratometry by at least 1 diopter (D) or by an increase in central corneal astigmatism of 1 D in 1 year, documented by at least two differential Scheimpflug corneal topographies. Keratoconus diagnosis and the necessity of treatment were assessed by two corneal specialists (AC, DC).
The study excluded patients that had other ocular corneal and immune system disorders, diabetes patients, or female patients who were pregnant or breastfeeding.
Visits
Patients were examined at baseline and at 1, 3, 6, 12, 18, and 24 months after intervention. The following measurements were performed at baseline and at each follow-up visit: uncorrected visual acuity (UCVA), corrected distance visual acuity (CDVA), manifest refractometry (Topcon autorefractometer), sphere and cylinder, slitlamp biomicroscopy, keratometry (K min and K max), optical tomography and pachymetry (Pentacam, Oculus Optikgeräte GmbH, Wetzlar, Germany), ultrasonic pachymetry for central corneal thickness (CCT) and for corneal thickness at the thinnest point (CTTP), endothelial cell count (ECC) (Konan Specular Microscope; Konan Medical, Inc., Hyogo, Japan), and intraocular pressure (IOP) by Goldmann applanation tonometry.
Procedures
Collagen cross-linking by iontophoresis without epithelial removal was indicated and performed for 40 eyes (40 patients) included in the study. Pilocarpine 1% drops were instilled 30 min prior to the procedure, to reduce the risk for ultraviolet light exposure of the lens and retina. The procedure was performed under topical anesthesia with three applications of 4% lidocaine drops under sterile conditions during 15 min. A special ring applicator (9 mm in diameter) containing the negative electrode was applied to the cornea, and a patch containing the positive pole was applied to the forehead. A continuous current generator (I-ON XL, SOOFT) set at 1 mA, powered by batteries, was connected to the relevant cables. The applicator was filled with 0.5 ml hypotonic solution of rRiboflavin (Ricrolin+; SOOFT, Montegiorgio, Italy) and the corneas underwent imbibition for 5 min (Fig. 1). The corneas were irradiated with an ultraviolet lamp (CBM VEGA 10 mW UVA Illumination System) with a wavelength of 370 nm for 9 min at 10 mW at a distance of 45 mm. After surgery, a bandage contact lens was applied and it was removed after 48 h. Post-intervention, patients received tobramycin–dexamethasone drops (Tobradex, Alcon) and artificial tears (Blu Yal, SOOFT), four times daily, for 4 weeks.
Standard CXL was performed for 40 eyes of 40 patients with stage I keratoconus, according to the protocol described elsewhere [13, 24]. Epithelial removal was performed using a blunt knife. Isoosmolar riboflavin 0.1% solution with 20% dextran (Ricrolin; SOOFT, Montegiorgio, Italy) was applied every 3 min for 15 min. Irradiation was performed with a UVA lamp (CBM VEGA 10 mW UVA Illumination System) with a wavelength of 370 nm for 9 min at 10 mW at a distance of 45 mm. A bandage lens was placed after surgery and it was removed after 1 week if the epithelial healing was complete. The post-CXL medication consisted of tobramycin eye drops (Tobrex, Alcon) and artificial tears (Blu Yal, SOOFT), five times daily until epithelial healing was documented, followed by tobramycin–dexamethasone drops (Tobradex, Alcon) and artificial tears (Blu Yal, SOOFT), four times daily, for 3 weeks more.
Statistical Analysis
After the study was completed, data collected from all the patients was statistically analyzed using SPSS Statistics software version 20. Baseline measurements between the treatment groups were compared using an independent-sample t test. The difference from baseline for each parameter was calculated at each time point (1, 3, 6, 12, 18, and 24 months) for each eye. The differences within each group were compared using a one-sample t test. The data in our cohorts do not have a normal distribution (according to Kolmogorov–Smirnov and Shapiro–Wilk tests); despite this, we employed parametric (and not non-parametric) tests because the samples of the cohorts are balanced (40 subjects in each cohort).
These changes were compared between the standard cross-linking and iontophoresis groups using an independent-sample t test. To report the trend over time, a variance analysis, the general linear model repeated measures was used by applying the polynomial option wherein seven time points (baseline, 1, 3, 6, 12, 18, and 24 months) were used as categorical variables. The level of significance was P < 0.05 in all cases.
Results
The present study compared the 24 months’ evolution of two groups consisting of 40 eyes of 40 patients, each diagnosed with early stages of keratoconus, one group being treated using iontophoresis CXL and the other using standard CXL. The two groups were matched for demographic and other clinical parameters. The mean age was 26.52 ± 3.77 (range 18–34) for the standard CLX group and 28.32 ± 4.91 (range 18–35) for the I-CLX group. At baseline, before the intervention, the demographic data and the clinical parameters were statistically analyzed and no significant difference was found between the two groups (P > 0.05) (Table 1).
Visual Acuity
There was no statistically significant difference in the mean preoperative logMAR UCVA and CDVA between the standard CXL and the I-CXL group (Table 1).
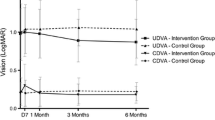
The UCVA improved in the I-CXL group compared with baseline at 3, 6, 12, 18, and 24 months postoperatively. In the standard CXL group, the UCVA remained stable at 3 months, but started to improve at the 6 months’ follow-up visit. The change of the UCVA was significantly greater in the I-CXL group compared to the standard CXL group at 3 (P < 0.01), 6 (P < 0.01), and 12 (P < 0.05) months, respectively (Table 2). At 24 months the mean improvement in UCVA was 0.9 Snellen lines in the epithelium-off CXL group and 1.7 lines in the I-CXL group. The improvement of UCVA was significantly greater in the I-CXL group at 24 months (P < 0.05) (Table 2; Fig. 2).
In the standard CXL group, the CDVA slightly decreased at the first follow-up visit. Improvement of the CDVA was first noticed at the 6 months’ visit and continued throughout the follow-up period. The mean CDVA remained stable in the I-CXL group for the first 3 months. The eyes treated with I-CXL significantly improved in CDVA at 6, 12, 18, and 24 months compared with baseline. At 24 months, the mean improvement in CDVA was 1.6 Snellen lines in the epithelium-off CXL group and 1.3 lines in the I-CXL group (Fig. 3).
There was a statistically significant different trend, reported by the general linear model repeated measures, towards improvement in CDVA between both groups, with a more favorable outcome for the standard CXL group (P < 0.01) (Table 2).
Refractive Outcomes
The manifest spherical error did not change significantly in both groups at 3, 6, and 12 months postoperatively. A statistically significant decrease in the sphere value was observed at the 18 months’ follow-up visit in both groups (P < 0.05). The decrease of the spherical error continued for the remainder of the follow-up in both groups (Fig. 4). There was no statistically significant difference between the improvement of the sphere in both groups (Table 2).
The improvement in the manifest cylindrical error was statistically significant after 3 months in both groups and continued for the remainder of the follow-up (Fig. 5). At 24 months, the manifest cylinder decreased by a mean of −0.831 ± 0.082 D in the standard CXL group and 0.962 ± 0.114 D in the I-CXL group. The changes reached high statistical significance in both groups (P < 0.001); there was no significant difference between the trends over time between the groups (Table 2).
Keratometry
Figure 6 shows the postoperative differences between the two treatment groups. A significant flattening of the K max values was noticed in both groups at 12 months postoperatively (P < 0.05). In the standard CXL group K max continued to flatten at 18 and 24 months with average values of 0.720 ± 0.201 D (P < 0.01) and 1.202 ± 0.199 D (P < 0.001), respectively. In the I-CXL group the flattening of the K max was noticed at 12 months with a reduction of 0.713 ± 0.092 D (P < 0.01) and continued throughout the follow-up. At 24 months K max demonstrated flattening of 0.908 ± 0.177 D (P < 0.001). The standard CXL group had greater reduction in K max values than the I-CXL group at 18 and 24 months, but the difference was not statistically significant. The trends of the two groups over time were not significantly different (Table 2).
The minimum keratometry (K min) values were stable in both group at every time frame.
Corneal Thickness Measurements (Pachymetry)
The preoperative thickness values at the center of the cornea and at the thinnest point were measured with a manual ultrasound pachymeter. The mean values were comparable at baseline and were greater than 500 μm, consistent with the early stage of the disease (Table 1).
At the first month’s follow-up visit, CCT and CTTP values showed a slight decrease that reached statistical significance at 3 months in both groups (P < 0.05). The pachymetry values returned to baseline values after 12 months; no statistical difference was registered between the two groups. There was no difference in the trends over time between the two groups (P < 0.05) (Table 2).
Endothelial Cell Count
No endothelial damage was observed at any time during the follow-up period. Postoperative cell density did not register significant changes in any group. No significant difference was found between the two techniques at any time point (P > 0.05) (Table 2). Intraocular pressure measured with the Goldmann applanation tonometer did not change significantly from baseline in either group throughout the follow-up period (Table 2). Lens and fundus did not change throughout the entire follow-up period. No adverse events were found in the I-CXL group. Adverse events occurred in 8 eyes (20%) in the standard CXL group: five cases of corneal haze, two cases of delayed re-epithelization, and one case of sterile infiltrate.
Discussion
Recent studies indicate that the use of iontophoresis in CXL technique seems to have some advantages, as compared to other methods, showing not only good riboflavin diffusion but also improvement in clinical and paraclinical indices [21, 25]. In the present study, we investigated the extent of the clinical benefits of iontophoretic CXL by analyzing important ophthalmologic parameters in a group of patients diagnosed with early keratoconus (stage I according to the Amsler–Krumeich classification) before and after I-CXL intervention, compared to a group of subjects with keratoconus who received standard CXL. To our knowledge, this is the first study to compare the efficacy and safety of I-CXL with that of standard CXL in two groups of patients with early stage keratoconus (stage I), monitored during a period of 24 months.
Numerous studies have proven the efficacy of standard CXL in treating progressive keratoconus in patients who were monitored over medium or long follow-up periods. Conventional standard CXL techniques are safe, but might lead to transient ocular discomfort, a longer recovery time of visual acuity, and in rare cases adverse reactions that might seriously affect the vision, e.g., stromal opacity, infectious keratitis, corneal melting, etc. A number of different technical solutions were introduced to preserve the corneal epithelium: transepithelial CXL, stromal pockets created with a femtosecond laser to inject riboflavin, iontophoresis.
Transepithelial CXL might be a solution for avoiding such complications and might also offer faster recovery times. The fact that it can stop the progression of keratoconus has been the subject of controversy and debate: some studies indicate a certain degree of efficiency, but lower than the efficiency of the standard CXL procedure [26, 27], whereas other studies show a stabilization or improvement in various topographic parameters [18, 28–30]. On the other hand, there are also studies that have shown a lack of efficiency for this technique [31–33].
Iontophoresis is a non-invasive technique that allows the penetration of a substance within a solid tissue with the aid of a low intensity electric current. Iontophoretic collagen cross-linking employs this principle for a better penetration of riboflavin into the corneal stroma. Preclinical studies have shown increases in the concentration of riboflavin in corneal stroma, comparable to the increase obtained after TE-CXL procedures [19, 21, 34].
Few clinical studies have evaluated I-CXL without comparing it to other procedures. Furthermore, these studies were conducted on a small number of patients over short periods of time [22, 23]. Bikbova et al. [22] evaluated this procedure in 22 patients with progressive keratoconus stages I–II according to the Amsler classification, and noticed a decrease in the keratometry values, as well as in corneal astigmatism values, together with improvements in the uncorrected distance visual acuity, without any loss in endothelial cells. Vinciguerra et al. [23] supervised I-CXL in 20 patients with progressive keratoconus over a 12-month period. They noticed that no patient exhibited any signs of keratoconus progression, and also a stabilization in all the topographic parameters and in the cornea’s thickness, without any significant loss of endothelial cells. The study concluded that the “relative efficacy of this technique compared to standard epithelium-off techniques remains to be determined” [23].
The only study that compared the efficiency and safety of I-CXL and CXL was conducted on 149 eyes with keratoconus stages I–II according to the Amsler classification. One group (73 eyes) was subjected to standard CXL and the other group (76 eyes) was subjected to I-CXL [24]. Keratoconus was halted and regression was obtained for both groups, but the standard CXL technique was more efficient. I-CXL halted the disease’s progression in patients followed-up for 24 months.
Our study compares the safety and efficacy of I-CXL with those of CXL for two groups of patients with progressive keratoconus stage I according to the Amsler–Krumeich grading system, monitored over a 24-month period. The two groups are similar in terms of demographics and the quantitative parameters taken into consideration. All the patients were examined using the same protocols after 1, 3, 6, 12, and 24 months.
The refractive parameters improved over time for both patient groups. The spherical error did not changed in either group at 3, 6, and 12 months. The decrease in the spherical error is of statistical relevance after 18 months for both groups. The reduction in cylindrical error occurs at 3 months post-surgery, and the tendency for improvement is maintained throughout the follow-up period, without significant differences from a statistical viewpoint. Similar observations were reported by Vinciguerra et al. [23] and Bikbova et al. [22] for I-CXL, and numerous other studies have noticed similar results for standard CXL [35–39]. Uncorrected visual acuity improved in both groups without any significant statistical difference at the end of the follow-up period. In the I-CXL group, UCVA improvement was faster and more important than in the standard CXL group. The same profile was found for CDVA, which began to improve in the I-CXL group starting with the third post-surgery month and going on throughout the follow-up period. CDVA changes are more precocious and more important during the first 12-months of follow-up for the I-CXL group.
In the recent literature, improvement of UCVA was reported both after standard CXL [35–38] and I-CXL [22, 23]. In our study, the I-CXL technique was superior in terms of a faster and more rapidly occurring visual acuity improvement, which can be a significant advantage for a faster professional recovery. Postoperative keratometric data indicates favorable effects for both procedures. In both groups, K max decrease was of greater importance when measured at 12 months post-surgery. For the last check-up, K max decrease was more important for the standard CXL group, but this factor did not reach statistical significance, and the tendency to decrease was maintained. For the I-CXL group, K max values remained stable throughout the second year of the follow-up, while K min values remained stable for both groups during the first year of follow-up. The I-CXL technique led to the improvement and stabilization of parameters on the short term. However, it has been shown that for progressive keratoconus patients, the standard CXL procedure yields better results and increases the chances of stopping the disease’s progression in the long term.
The results obtained in our study on standard CXL are comparable to those found in other studies, but we have to mention that no study has been conducted exclusively on patients with progressive keratoconus stage I according to the Amsler classification. The improvements in the topographic parameters after I-CXL seen in our study confirm other results found in the literature [22–24]; however, note that only one study was conducted exclusively on patients with early keratoconus [23, 24], and the difference is that in our study, the follow-up period was greater.
Our study can be compared with a recent one by Bikbova and Bikbov [24]. The common parameters that were analyzed (CDVA, keratometry, CCT, cylindrical error) offered similar conclusions. The measurements on absolute value cannot be compared because patients with various stages of the disease were included (stage I in our study and stages I and II in Bikbova and Bikbov’s study), whereas the instruments for determining refractive and topographic parameters, as well as the technical protocols, were different.
Pachymetry data showed high preoperative values due to the disease being in its early stages. Both patient groups have shown a small decrease in the thickness of the central cornea, detected after 3 months postoperative. Pachymetric values went back to normal and remained stable throughout the follow-up period, and no differences were recorded in the CCT evolution in the two groups.
For both groups, no decrease in the density of endothelial cells was recorded throughout the follow-up period, as compared to the preoperative value. Also, no adverse reactions were encountered in the I-CXL group; for the standard CXL group, adverse reactions were recorded in 20% of the eyes operated on, but no reaction resulted in negative consequences in terms of visual acuity or the evolution of corneal topographic parameters. In both patient groups, no progression of keratoconus was recorded during the entire 24-month follow-up period.
Our study proves that the I-CXL method is a viable alternative for stopping the progression of keratoconus in early stages. The comparative analysis with the standard CXL method did not show major differences between the two procedures at the end of the follow-up periods. The advantages evident for the I-CXL technique are linked to the early postoperative period and relate to faster recovery times for visual acuity, the absence of adverse reactions, and immediate social and professional reintegration. The advantages of the standard CXL technique can be seen in the medium and long-term follow-up and relate to the stabilization of the disease and the improvements of corneal topographic parameters. The results of the study cannot be used for suggesting the elective therapeutic method for early keratoconus, but only underline the similarities between the two techniques in terms of efficiency and safety. More important is the goal of detecting keratoconus as early as possible, as well as ensuring standardized monitoring procedures and immediate treatment methods after confirming the progression of the disease.
The study included homogenous groups of comparable patients with early progressive keratoconus, each group having gone through a specific therapy for halting the progression of the disease. This is the first comparative study focused exclusively on progressive keratoconus stage I according to the Amsler classification. The follow-up on the 80 patients was conducted using the same protocol for a period of 24 months by a small number of investigators (two) with significant experience in managing keratoconus.
The limitations of the study concern its retrospective nature: the use of one technique was linked to the fact that I-CXL was introduced into practice later on. Therefore, the standard CXL patient group consisted of consecutive patients who were first treated prior to the introduction of the I-CXL technique. After its introduction, the I-CXL procedure was used exclusively for consecutive patient cases with early progressive keratoconus.
The study includes a relatively small cohort of patients, monitored for a short period, and does not provide insights into the efficiency and safety of these methods when it comes to the more advanced stages of keratoconus. Furthermore, the analysis does not include data regarding the aberrometric parameters, and does not include all the morphologic parameters obtained using corneal tomography. In addition, the study did not analyze the demarcation line after cross-linking. However, we do not consider that these limitations might have changed the relevance of our results.
Conclusion
Our study reveals that I-CXL is non-inferior to standard technique for stopping the progression of keratoconus in its early stages with a higher degree of safety for the patients and a faster recovery of visual acuity. For further insights into the efficiency and uses of these methods, prospective studies are required, using higher numbers of patients with various stages of keratoconus, monitored over longer follow-up periods.
References
Asri D, Touboul D, Fournié P, et al. Corneal collagen crosslinking in progressive keratoconus: multicenter results from the French National Reference Center for Keratoconus. J Cataract Refract Surg. 2011;37:2137–43.
Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319.
Raiskup-Wolf F, Hoyer A, Spoerl E, Pillunat LE. Collagen crosslinking with riboflavin and ultraviolet-A light in keratoconus: long-term results. J Cataract Refract Surg. 2008;34:796–801.
Raiskup F, Theuring A, Pillunat LE, Spoerl E. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results. J Cataract Refract Surg. 2015;41:41–6.
Spoerl E, Mrochen M, Sliney D, Trokel S, Seiler T. Safety of UVA-riboflavin cross-linking of the cornea. Cornea. 2007;26:385–9.
Hafezi F, Tabibian D, Richoz O. Additive effect of repeated corneal collagen cross-linking in keratoconus. J Refract Surg. 2014;30:716–8.
Spoerl E, Huhle M, Seiler T. Induction of cross-links in corneal tissue. Exp Eye Res. 1998;66:97–1038.
Kohlhaas M, Spoerl E, Schilde T, et al. Biomechanical evidence of the distribution of cross-links in corneas treated with riboflavin and ultraviolet A light. J Cataract Refract Surg. 2006;32:279–83.
Agrawal V. Long-term results of cornea collagen cross-linking with riboflavin for keratoconus. Indian J Ophthalmol. 2013;61:433–4.
Caporossi A, Mazzotta C, Baiocchi S, Caporossi T. Long-term results of riboflavin ultraviolet a corneal collagen cross-linking for keratoconus in Italy: the Siena eye cross study. Am J Ophthalmol. 2010;149:585–93.
Ortiz-Toquero S, Rodriguez G, de Juan V, Mayo-Iscar A, Martin R. The influence of the refractive correction on the vision-related quality of life in keratoconus patients. Qual Life Res. 2016;25:1043–51.
Rebenitsch R, Kymes S, Walline J, Gordon M. The lifetime economic burden of keratoconus: a decision analysis using a Markov model. Am J Ophthalmol. 2011;151:768–73.
Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–7.
Wollensak G. Crosslinking treatment of progressive keratoconus: new hope. Curr Opin Ophthalmol. 2006;17:356–60.
Angunawela R, Arnalich-Montiel F, Allan B. Peripheral sterile corneal infiltrates and melting after collagen crosslinking for keratoconus. J Cataract Refract Surg. 2009;35:606–7.
Dhawan S, Rao K, Natrajan S. Complications of corneal collagen cross-linking. J Ophthalmol. 2011;2011:869015.
Raiskup F, Hoyer A, Spoerl E. Permanent corneal haze after riboflavin-UVA-induced cross-linking in keratoconus. J Refract Surg. 2009;25:S824–8.
Caporossi A, Mazzotta C, Paradiso AL, et al. Transepithelial corneal collagen crosslinking for progressive keratoconus: 24-month clinical results. J Cataract Refract Surg. 2013;39:1157–63.
Cassagne M, Laurent C, Rodrigues M, et al. Iontophoresis transcorneal delivery technique for transepithelial corneal collagen crosslinking with riboflavin in a rabbit model. Invest Ophthalmol Vis Sci. 2016;57:594–603.
Bouheraoua N, Jouve L, Borderie V, Laroche L. Three different protocols of corneal collagen crosslinking in keratoconus: conventional accelerated and iontophoresis. J Vis Exp. 2015;12:105.
Mastropasqua L, Nubile M, Calienno R, et al. Corneal cross-linking: intrastromal riboflavin concentration in iontophoresis-assisted imbibition versus traditional and transepithelial techniques. Am J Ophthalmol. 2014;157:623–30.
Bikbova G, Bikbov M. Transepithelial corneal collagen cross-linking by iontophoresis of riboflavin. Acta Ophthalmol. 2014;92:e30–4.
Vinciguerra P, Randleman JB, Romano V, et al. Transepithelial iontophoresis corneal collagen cross-linking for progressive keratoconus: initial clinical outcomes. J Refract Surg. 2014;30:746–53.
Bikbova G, Bikbov M. Standard corneal collagen crosslinking versus transepithelial iontophoresis-assisted corneal crosslinking, 24 months follow-up: randomized control trial. Acta Ophthalmol. 2016. doi:10.1111/aos.13032.
Magli A, Chiariello Vecchio E, et al. Pediatric keratoconus and iontophoretic corneal crosslinking: refractive and topographic evidence in patients underwent general and topical anesthesia, 18 months of follow-up. Int Ophthalmol. 2015. doi:10.1007/s10792-015-0166-3.
Buzzonetti L, Petrocelli G, Valente P, et al. Iontophoretic transepithelial corneal cross-linking to halt keratoconus in pediatric cases: 15-month follow-up. Cornea. 2015;34:512–5.
Çerman E, Toker E, Ozarslan Ozcan D. Transepithelial versus epithelium-off crosslinking in adults with progresive keratoconus. J Cataract Refract Surg. 2015;41:1416–25.
Khairy HA, Marey HM, Ellakwa AF. Epithelium on corneal crosslinking treatment of progressive keratoconus: a prospective, consecutive study. Clin Ophtalmol. 2014;8:819–23.
Rossi S, Orrico A, Romano V, et al. Standard versus trans-epithlial collagen cross-linking in keratoconus patients suitable for standard collagen cross-linking. Clin Ophthalmol. 2015;9:503–9.
Kocak I, Aydin A, Kaya F, Koc H. Comparison of transepithelial corneal collagen crosslinking with epithelium-off crosslinking in progressive keratoconus. J Fr Ophtalmol. 2014;37:371–6.
Koppen C, Wouters K, Mathysen D, Rozema J, Tassignon MJ. Refractive and topographic results of benzalkonium chloride-assisted transepithelial crosslinking. J Cataract Refract Surg. 2012;38:1000–5.
Ma Uematsu, Ta Kumagami, Kusano M, et al. Acute corneal epithelial change after instillation of benzalkonium chloride evaluated using a newly developed in vivo corneal transepithelial electric resistance measurement method. Ophthalmic Res. 2007;39:308–14.
Filippello M, Stagni E, O’Brart D. Transepithelial corneal collagen crosslinking: bilateral study. J Cataract Refract Surg. 2012;38:283–91.
Soeters N, Wisse RP, Godefrooij DA, Imhof SM, Tahzib NG. Transepithelial versus epithelium-off corneal cross-linking for the treatment of progressive keratoconus: a randomized controlled trial. Am J Ophthalmol. 2015;159:821–8.
Vinciguerra P, Mencucci R, Romano V, et al. Imaging mass spectrometry by matrix-assisted laser desorption/ionization and stress-strain measurements in iontophoresis transepithelial corneal collagen cross-linking. Biomed Res Int. 2014;2014:404587.
Wittig-Silva C, Whiting M, Lamoureux E, et al. A randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: preliminary results. J Refract Surg. 2008;24:S720–5.
O’Brart DP, Chan E, Samaras K, Patel P, Shah SP. A randomised, prospective study to investigate the efficacy of riboflavin/ultraviolet A (370 nm) corneal collagen cross-linkage to halt the progression of keratoconus. Br J Ophthalmol. 2011;95:1519–24.
Kymionis GD, Grentzelos MA, Liakopoulos DA, et al. Long-term follow-up of corneal collagen cross-linking for keratoconus–the Cretan study. Cornea. 2014;33:1071–9.
Wittig-Silva C, Chan E, Islam FM, et al. A randomized, controlled trial of corneal collagen cross-linking in progressive keratoconus: three-year results. Ophtalmology. 2014;121:812–21.
Acknowledgements
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. All authors want to thank any study participants for their involvement in the study. The authors disclose any patient involvement in the study trial design or dissemination of results.
Disclosures
Alina Cantemir, Anisia I. Alexa, Nicoleta Anton, Roxana E. Ciuntu, Ciprian Danielescu, Dorin Chiselita, and Danut Costin have nothing to disclose.
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for being included in the study. Additional informed consent was obtained from all patients for which identifying information is included in this article.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/4D77F0605700577F.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Cantemir, A., Alexa, A.I., Anton, N. et al. Evaluation of Iontophoretic Collagen Cross-linking for Early Stage of Progressive Keratoconus Compared to Standard Cross-linking: A Non-Inferiority Study. Ophthalmol Ther 6, 147–160 (2017). https://doi.org/10.1007/s40123-017-0076-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-017-0076-8