Abstract
Introduction
We estimated the safety and efficacy of ultrasound-guided multipoint fascial plane block, including serratus anterior plane block (SAPB) and bilateral transversus abdominis plane block (TAPB) in elderly patients who underwent combined thoracoscopic–laparoscopic esophagectomy (TLE).
Methods
The authors enrolled 80 patients in this prospective study after patient selection using the inclusion and exclusion criteria who were scheduled for elective TLE from May 2020 to May 2021. Patients were randomly assigned to the treated group (group N) or the control group (group C) (n = 40 per group) using the sealed-envelope method. Multipoint fascial plane blocks, including serratus anterior plane block (SAPB) and bilateral TAPB, were performed on patients undergoing TLE using a solution of 60 mL 0.375% ropivacaine plus 2.5 mg dexamethasone by 3 injections of 20 mL each (group N) or no interventions (group C).
Results
Systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) at T incision and 30 min after T incision were significantly higher in group C than in group N, and also significantly higher than at baseline (P < 0.01). Blood glucose at 60 min, 2 h after T incision, was significantly higher in group C than in group N and significantly higher than at baseline (P < 0.01). Compared to group N, the dosages of propofol and remifentanil used during surgery in group C were more than those in group N (P < 0.01). The time to first rescue analgesic in group C was earlier than in group N. The total postoperative use of sufentanil, and the number of patients requiring rescue analgesics in group C, were more than in group N (P < 0.01).
Conclusions
This study showed that applying the multipoint fascia pane block technique in TLE for elderly patients could significantly reduce postoperative pain, decrease the dosages of drugs used in general anesthesia, improve the quality of the awakening, and have no obvious adverse reactions.
Trial Registration: Chinese Clinical Trial Registry (ChiCTR-2000033617).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The incidence and mortality rate of esophageal cancer rank fifth and fourth in all malignant tumors in China. Thoracoscopic–laparoscopic esophagectomy (TLE) is widely used in patients with esophageal cancer. |
However, TLE generates seven endoscopic surgery holes in the chest and abdomen, which result in severe trauma, long surgery time, and seriously affect postoperative recovery, particularly for older patients. |
We used the combination of SAPB and TAPB, which provides an analgesic effect and simplifies the procedure, in the anesthesia of TLE to investigate the effectiveness in pain management, stress response, and TLE recovery in older patients with esophageal cancer. |
The multipoint fascia plane block technique in TLE for older patients significantly reduced postoperative pain, narcotics usage, the incidence of postoperative nausea, vomiting, and hypertension, and improved the quality of the awakening. |
Introduction
Esophageal cancer is the fifth most common cancer and the fourth cause of cancer-related mortality [1]. Esophagectomy is still the main treatment option for resectable esophageal cancer. Open laparoscopic and thoracoscopic–laparoscopic esophagectomy (TLE) are two common techniques used to perform esophagectomy. However, compared with other laparoscopic techniques, TLE involves a small incision and thus reduces postoperative pain and complications. In addition, it also facilitates lymphadenectomy [2,3,4].
The TLE procedure involves three surgical incisions in the upper right chest, abdomen, and left neck under the guidance of thoracoscopy and laparoscopy. Seven endoscopic operation holes are also required in the chest and abdomen [5, 6]. The main abdominal incisions were: 2 cm outside the junction between the midclavicular line and the costal arch, 1 cm above the umbilicus, 1 cm below xiphoid process, and 1 cm below the umbilicus. The three incisions in the lateral chest were: 1 cm at the fourth intercostal space of anterior axillary line, 1 cm at the seventh intercostal space of midaxillary line, and 1 cm at the eighth intercostal space of posterior axillary line. The operation time of TLE ranges from 4 h to 5 h. The anesthesia technique typically involves endobronchial general anesthesia, with or without regional anesthesia. Epidural and peripheral nerve blocks are two types of regional anesthesia commonly used for pain management during TLE. While both techniques involve injecting local anesthetic medication to block pain signals, they target different nerves. The epidural nerve block technique involves the injection of local anesthetic medication into the space around the spinal cord, which blocks pain signals from a large body area, including the chest and abdomen. This technique provides excellent pain control and can reduce the need for opioid pain medications. However, the epidural approach is associated with risks and potential complications, such as bleeding, infection, nerve damage, respiratory depression, and hypotension [7]. The peripheral nerve block involves the injection of local anesthetic medication directly into the nerves that supply the surgical site. This technique blocks pain signals from a smaller body area. Compared with the epidural approach, the peripheral pain block technique can still provide effective pain control, but it carries a lower risk of complications post-surgery [8].
In the case of esophagectomy, the peripheral nerve block typically involves blocking the bilateral transversus abdominis plane (TAPB) or the serratus anterior plane (SAPB). The SAPB procedure was first described by Blanco et al. in 2013 [9]. Several studies have shown that the SAPB was an effective adjuvant treatment option to control pain following thoracic and breast surgery [10, 11]. On the other hand, similar studies have found that TAPB could achieve effective pain control following abdominal surgery [12, 13].
However, there is currently limited research on using multipoint fascial plane blocks with SAPB and TAPB to manage postoperative pain, reduce stress response, and improve recovery in patients undergoing TLE. Therefore, this prospective study aimed to investigate the effectiveness of SAPB combined with TAPB in managing postoperative pain, stress response, and postoperative recovery after TLE in elderly patients with esophageal cancer.
Methods
Study Design
A single-center randomized controlled prospective clinical study was conducted for TLE. This study was approved by the ethics committee of the First Affiliated Hospital of the University of Science and Technology of China and registered on the Chinese Clinical Trial Registry (ChiCTR, http://www.chictr.org.cn) by Zhang Min (registration number, ChiCTR-2000033617). The study inclusion criteria were patients undergoing TLE. Each participant provided written informed consent before initiating any study-related procedures. Patients of either sex, with physical status of II–III on the American Society of Anesthesiologists classification, age ≥ 60 years, and with no history of mental illness, hearing and language disorders, volunteered to participate in the study and signed informed consent.
Patients
The authors enrolled 80 patients in this prospective study, after patient selection using the inclusion and exclusion criteria, who were scheduled for elective TLE from May 2020 to May 2021. Patients were randomized to the nerve block group (group N) or the control group (group C) (n = 40 per group) using the sealed-envelope method. Exclusion criteria included the following: allergic history of local anesthetics, infection at the puncture site, coagulation dysfunction, patients with paresthesia dysfunction, refusal of nerve block by patients or family members, intraoperative blood loss greater than 600 mL, reoperation, or patients admitted to intensive care unit (ICU) after surgery.
Anesthesia Procedure
Patients were sent to the surgical room and received standard monitoring, which consisted of five-lead electrocardiography (ECG), oxygen saturation (SpO2), non-invasive blood pressure measurements, and bispectral index monitoring (BIS). Then we monitored the radial artery pressure by radial artery puncture under local anesthesia. Midazolam 0.02–0.04 mg/kg, etomidate 0.2–0.4 mg/kg, sufentanil 0.4–0.5 μg/kg, and rocuronium 0.6–1 mg/kg were given for anesthesia induction. Manual face mask ventilation was continued for no less than 3 min until the jaw relaxed and the value of BIS was less than 50, to allow endotracheal intubation. The appropriate type of endotracheal tube was inserted, an occluder was inserted, and the bronchoscopy was used to assess its correct placement. Then, the patients were connected to a mechanical ventilator and the SpO2 and end-tidal carbon dioxide pressure (PetCO2) were maintained in the normal range. Propofol, remifentanil, sufentanil, and cisatracurium were used to maintain the BIS value between 40 and 60 and to ensure that the mean arterial pressure (MAP) and heart rate (HR) variation did not exceed 20% from the baseline values in the two groups. The same surgical team, comprising three thoracic surgeons, performed all the surgeries.
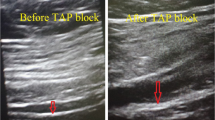
After induction of anesthesia, group N received an ultrasound-guided right SAP block. The ultrasound probe was placed at the level of the fourth and fifth rib of the right axillary midline [9]. SABP was given 20 mL of local anesthetics in the serratus anterior deep fascia space, including 0.375% ropivacaine plus 2.5 mg dexamethasone (Fig. 1A). Then, after the chest operation, the patient was transferred to the supine position to perform a bilateral TAP block before the abdominal operation. In this study, bilateral TAP blocks were performed by a subcostal approach, which targets the transversus abdominis plane compartment in the anterior abdominal wall [14]. Both sides received 20 mL of local anesthetics, including 0.375% ropivacaine plus 2.5 mg dexamethasone in the transverse abdominal fascia space (Fig. 1B). Group C did not accept the above two nerve block methods. The patients were transferred to the anesthesia recovery room (PACU) after the surgery and sent back to the ward when they were fully awake.
After extubation, A PCA pump (ZZB-IB, Nantong AIPU Medical Inc., China) was connected to the intravenous line and administered the analgesic drugs (1-μg demand dose, 10-min lockout period without background infusion). A 150 mL solution was prepared in the PCA reservoir bag containing 1 μg/mL of sufentanil alone. When sufficiently awake, patients were instructed to assess their pain level on visual analog scale (VAS). If VAS scores > 4 in any patient, parecoxib 40 mg was immediately administered as rescue analgesia.
Observation Index
The perioperative data and postoperative assessments were performed by the anesthesiologist who was blind to each patient’s group. All patients who were drowsy, on mechanical ventilation, and did not respond appropriately to oral commands were excluded from the study. The systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) were recorded at baseline, 30 min, 60 min, and 2 h after the thoracoscopic incision. Blood glucose was recorded at baseline, 30 min, 60 min, and 2 h after the thoracoscopic incision. Intraoperative consumption of propofol, remifentanil, and cisatracurium, number of local anesthetic toxicity, the time of respiratory recovery, the first opening of eyes, extubation after the end of anesthesia, and time in PACU were recorded. The time to first rescue analgesic, the number of patients who required rescue analgesic, and the total postoperative use of sufentanil were also recorded within 48 h after returning to the ward. Postoperative VAS scores (0–10 points) at rest and cough at 2, 6, 12, 24, and 48 h were recorded after returning to the hospital. Adverse reactions that occurred 48 h after the surgery: postoperative nausea and vomiting (PONV), drowsiness, and chronic pain at 3 and 6 months were recorded.
Sample Size
The purpose of the study was to test the hypothesis that the multipoint fascial plane block and total intravenous anesthesia would result in better postoperative control of pain compared with simple total intravenous anesthesia alone in elderly patients undergoing TLE. After a pilot study (5 patients per group), the authors detected a difference of 25% reduction in postoperative VAS scores. The authors estimated that the required sample size would be 40 patients per group with a significance level of 0.05 and a power of 90% [15]. Finally, 80 patients were then enrolled to allow for dropout.
Statistical Analysis
Statistical analyses were conducted using SPSS Statistics 22.0 software (SPSS, Inc., Chicago, IL, USA). Continuous (numerical) data were expressed as mean ± standard deviation (SD) with normally distributed data, or as the median and quartiles for skewed data distributions. Repeated measurements were used to analyze differences in the interaction effects between groups and timepoints. The Pearson chi-squared (χ2) test and Fisher’s exact test were used to analyze categorical variables. Confidence intervals (95% CI) are reported for the specific aims (VAS); P value < 0.05 was considered to indicate statistical significance.
Results
Demographic and Clinical Case Data
A total of 80 patients with esophageal cancer were enrolled in the study and randomized into groups N and C. Four of these patients dropped out of this study, and 76 patients completed the study, 38 in group N and 38 in group C (Fig. 2). Two patients had postoperative bleeding and needed reoperation to stop bleeding, three had sustained hypoxia and needed breathing support and intensive care, one patient died of esophageal–tracheal fistula during hospitalization, and four patients died of tumor recurrence within 6 months after the operation. There was no statistically significant difference in the sex, age, body mass index (BMI), the American Society of Anesthesiologists Physical Status (ASA) grade, and surgery time between the two groups, as shown in Table 1.
The Intraoperative Hemodynamics and Blood Glucose Between the Two Groups of Patients
The SBP, DBP, and HR values at the T incision and 30 min after the T incision were significantly higher in group C than in group N and significantly higher than the baseline values (P < 0.01). The blood glucose levels at 60 min and 2 h after the T incision were significantly higher in group C than those in group N and significantly higher than the baseline values (P < 0.01) (Fig. 3).
SBP, DBP, HR, and blood glucose measured intraoperatively. Values are presented as mean ± standard deviation. (A–C) SBP, DBP, and H.R. at T incision and 30 min after T incision were significantly higher in group C than in group N, and also significantly higher at baseline (*#P < 0.01). (D) Blood glucose at 60 min, 2 h after T incision, was significantly higher in group C than in group N, and also significantly higher at baseline (*#P < 0.01). SBP systolic blood pressure, DBP diastolic blood pressure, HR heart rate, Glu blood glucose, T incision thoracoscopic incision
The Intraoperative and Postoperative Events Between the Two Groups
The dosages of propofol and remifentanil used during the surgery, and the postoperative recovery parameters, including the spontaneous breathing recovery time, eyes-opening time, endotracheal tube removal time, and stay time in PACU, were significantly higher in group C than those in group N. The time to first rescue analgesic in group C was shorter than in group N. In addition, the total postoperative use of sufentanil and the number of patients requiring rescue analgesics in group C were significantly higher than those in group N (P < 0.01), as illustrated in Table 2.
Postoperative VAS
VAS showed higher scores at rest and on coughing in group C than in the group N in the first 12 h after the operation (Fig. 4).
(A) VAS at rest during the first 48 postoperative hours. (B) VAS on coughing during the first 48 postoperative hours. Values are presented as mean ± standard deviation. VAS showed higher scores at rest and when coughing in group C than in group N in the first 12 h postoperatively (*P < 0.01). VAS visual analog scale, CI confidence interval
The Postoperative Complications
Overall the incidence of adverse reactions in the two groups was low except for the relatively high incidence of chronic pain. The incidence of nausea and vomiting was lower in group N (3/38) than that in group C (12/38) (P < 0.01). A total of seven patients experienced drowsiness in group C, as opposed to only three patients in group N. Although not statistically significant, the incidence of chronic pain in group C was higher than that in group N at both 3 months (31.6% versus 23.7%) and 6 months (26.3% versus 21.1%) post-surgery (Table 3).
Discusion
TLE is one of the main treatment options for esophageal cancer. This procedure involves a major operation with a total of seven incisions on the chest and abdomen. As a result, after the surgical procedure, patients often experience severe pain in these areas, leading to prolonged post-surgery recovery and dependence on analgesic pain management. In addition, elderly patients undergoing TLE are more likely to have respiratory and cardiovascular complications from anesthesia and have a lower tolerance to the high anesthesia dosages required as a result of the long TLE procedure. Therefore, new methods are needed to improve pain management and reduce the dosages of anesthesia required to sedate the patient during the TLE procedure.
Nerve blocking involves the injection of local anesthetic near specific nerves affected by the surgery to decrease pain during and after the surgical procedure. In recent years, SAPB has been widely utilized to relieve the pain in the chest following thoracic surgery. The main advantages of this technique are its excellent analgesic effect and the simplicity of the procedure. On the other hand, the TAP block is a common technique used to control pain in uterine and colorectal surgeries and involves the injection of local anesthetics into the plane between the obliquus internus and transversus abdominis muscles to block the T6–L1 thoracolumbar nerves and, subsequently, the conduction of nerve pain to the anterior abdominal wall [16, 17]. Sondekoppam et al. [18] found that the spread of ultrasound-guided subcostal and lateral TAP injections in embalmed cadavers ranged from the T7/8–L1 dermatomes in most of the hemiabdomens. However, the blocking of the lateral cutaneous branches using an anterolateral or median approach can be challenging to perform. Nevertheless, this approach could be used to block the lateral cutaneous branches of the spinal nerve supplying the skin of the anterolateral abdomen [18].
The problem with applying effective nerve block in TLE is that the pain involves both the chest and abdomen. The combination of the SAPB and TAP nerve-blocking techniques may improve pain control following TLE. However, the efficacy of combining the two methods in achieving pain relief has not yet been explored. Therefore, in this prospective randomized study, we compared the analgesic effect and post-surgery recovery in patients anesthetized with SAPB and TAP (group N) with patients who received no nerve block intervention during the TLE procedure (group C).
Our novel surgical techniques involved performing SAPB before the chest surgery, after applying general anesthesia. The SAPB procedure involved two injections of 180 mg of ropivacaine. A 2–3 h interval was allowed between the two injections to reduce the risk of local anesthetic poisoning that could have been caused by injecting a large dose of local anesthetics at once. After the chest operation, the patient was transferred to the supine position, and a bilateral TAP block was performed before the abdominal operation, which involved the administration of 180 mg of ropivacaine. The SAPB and TAP procedures were not performed simultaneously to reduce the risk of developing severe toxicity caused by the overlapping reactions of the two anesthetics.
Several parameters were observed during the surgical procedure to evaluate the efficacy of the combined SAPB and TAP procedures in relation to the control group, including the hemodynamics, the anesthesia dosage and the glucose level. The hemodynamics in group N was more stable than that in group C, especially in the initial stage of the skin incision. Consistent with previous studies [19,20,21], the patients in group N required lower dosages of propofol and remifentanil. Two hours after the thoracic incision, the blood glucose was significantly higher than the baseline values. However, the glucose levels were significantly higher in group C than in group N. This finding suggests that the nerve block can inhibit the stress response caused by the skin incision, eventually leading to a slower increase in the blood glucose levels.
Following the surgery, the patients in group N also had a shorter and better awakening than the patients in group C. The time to respiratory recovery, opening eyes, and extubation of patients in group N were 42.7 ± 5.3, 52.3 ± 4.7, and 54.7 ± 3.7, respectively. The time was significantly shortened, which may be related to the reduction of the use of analgesic drugs during operation. A clinical experiment showed that the BIS value of thoracic surgery under anterior serratus block increased more rapidly after 15 min and 30 min, following the end of anesthesia, than that of surgery with thoracic paravertebral block. General anesthesia combined with nerve block is used in elderly patients to reduce the use of anesthetics and accelerate patient recovery.
After the operation, we followed up the patients to identify any adverse reactions and to assess the pain severity. The pain score within 12 h post-surgery, dosage of drugs, and the number of analgesic treatments required within 48 h after the surgery in group N were less than those of group C. These findings are consistent with previous studies that utilized the TAPB to control pain following abdominal surgery [16, 17]. No local anesthetic toxicity was reported in groups C and N. Various factors can cause nausea and vomiting following TLE, including the discomfort caused by the gastric tube, duodenal feeding tube, and the use of narcotic drugs, especially opioids, to manage pain. However, the incidence of nausea and vomiting was lower in group N than in group C, possibly because the patients in group N required fewer opioids to control their pain. The occurrence of chronic pain after thoracic surgery can have a big impact on the quality of life postoperatively. In this study, the incidence of chronic pain was lower in group N than in group C. However, the difference was not statistically significant, which may be due to the small sample size. In previous studies, the incidence of chronic pain after thoracic endoscopic surgery was around 30% [4, 5]. Overall the research findings indicate that SAPB combined with TAP can provide an effective analgesic effect within the whole trunk and can improve the postoperative recovery.
The epidural and paravertebral block technique is an alternative to the combined SAPB and TAP nerve-blocking technique used in our study. However, the epidural nerve block is a complex procedure, as the block plane is high and the procedure carries a higher postoperative risk of infection [22]. Incisional infiltration to block the anterior serratus is also commonly used to reduce postoperative pain. The advantage of this technique is that it can provide prolonged pain relief, has a low probability of local anesthetic poisoning and complications, and is relatively simple to perform [23,24,25].
This study has several limitations that have to be acknowledged. Our study utilized a single-center prospective design with a small sample size, thus limiting the generalizability of the research findings. In addition, only blood glucose levels were used to measure the intraoperative stress response, and other serum inflammatory mediators were not investigated. Patients were followed up for only 6 months after surgery, and four cases were lost in the follow-up. As a result, it was not possible to evaluate the effectiveness of the SAPB and TAP nerve block technique in managing chronic pain. Therefore, further multicenter longitudinal prospective studies with a larger cohort are still needed to evaluate the safety and effectiveness of the multipoint fascia plane block and its long-term impact on pain management in patients treated with TLE.
Conclusions
This study showed that the multipoint fascia plane block technique in TLE for elderly patients could significantly reduce postoperative pain, decrease the dosages of drugs used to anesthetize the patient, reduce the incidence of postoperative nausea, vomiting, and hypertension, and improve the quality of the awakening. Overall the procedure was safe, as no obvious adverse events were reported. Moreover, it reduced the time required to get out of bed and restore gastrointestinal function. Based on these findings, we concluded that the multipoint fascia pane block technique could provide a safe and effective technique to reduce the pain experienced by elderly patients undergoing TLE for esophageal cancer.
References
Hongo M, Nagasaki Y, Shoji T. Epidemiology of esophageal cancer: orient to occident. Effects of chronology, geography and ethnicity. Gastroenterol Hepatol. 2009;24:729–35.
Vijayvargiya P, Chedid V, Erwin P, et al. Efficacy of promotility agents in improving gastric emptying and upper gastrointestinal symptoms: a systematic review and meta-analysis. Am J Gastroenterol. 2018;113:677–8.
Wei K, Min S, Hao Y, et al. Postoperative analgesia after combined thoracoscopic–laparoscopic esophagectomy: a randomized comparison of continuous infusion and intermittent bolus thoracic epidural regimens. J Pain Res. 2018;12:29–37.
Ju WM, Shu GG, Xue Q, et al. Comparison of short-term outcomes and three years urvival between total minimally invasive McKeown and dual-incision esophagectomy. Thorac Cancer. 2017;8:80–7.
Straatman J, van der Wielen N, Cuesta MA, et al. Minimally invasive versus open esophageal resection: three-year follow-up of the previously reported randomized controlled trial: the TIME trial. Ann Surg. 2017;266:232–6.
Yang H, Liu H, Chen Y, et al. Neoadjuvant chemoradiotherapy followed by surgery versus surgery alone for locally advanced squamous cell carcinoma of the esophagus (NEOCRTEC5010): a phase III multicenter, randomized, open-label clinical trial. J Clin Oncol. 2018;36:2796–803.
Tzimas P, Prout J, Papadopoulos G, et al. Epidural anaesthesia and analgesia for liver resection. Anaesthesia. 2013;68:628–35.
Chen Y, Shi K, Xia Y, et al. Sensory assessment and regression rate of bilateral oblique subcostal transversus abdominis plane block in volunteers. Reg Anesth Pain Med. 2018;43:174–9.
Blanco R, Parras T, McDonnell JG, et al. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68:1107–13.
Semyonov M, Fedorina E, Grinshpun J, et al. Ultrasound-guided serratus anterior plane block for analgesia after thoracic surgery. J Pain Res. 2019;12:953–60.
Yoon HS, Yu BW, Kim YM, et al. Serratus anterior plane block combined with monitored anesthesia care for breast surgery on the lateral side. Korean J Anesthesiol. 2019;72:500–3.
Yoshida T, Furutani K, Watanabe Y, et al. Analgesic efficacy of bilateral continuous transversus abdominis plane blocks using an oblique subcostal approach in patients undergoing laparotomy for gynaecological cancer: a prospective, randomized, triple-blind, placebo-controlled study. Br J Anaesth. 2016;117:812–20.
Hernandez MC, Panchamia J, Finnesgard EJ, et al. Transversus abdominis plane blocks with liposomal bupivacaine after open major hepatectomy is associated with reduced early patient-reported pain scores and opioid administration. Surgery. 2018;164:1251–8.
Tran DQ, Bravo D, Leurcharusmee P, et al. Transversus abdominis plane block: a narrative review. Anesthesiology. 2019;131:1166–90.
Novak-Jankovic V, Milan Z, Potocnik I, et al. A prospective, randomized, double-blinded comparison between multimodal thoracic paravertebral bupivacaine and levobupivacaine analgesia in patients undergoing lung surgery. J Cardiothorac Vasc Anesth. 2012;26:863–7.
Kamel AAF, Amin OAI, Ibrahem MAM. Bilateral ultrasound-guided erector spinae plane block versus transversus abdominis plane block on postoperative analgesia after total abdominal hysterectomy. Pain Physician. 2020;23:375–82.
Desai N, El-Boghdadly K, Albrecht E. Epidural vs transversus abdominis plane block for abdominal surgery—a systematic review, meta-analysis and trial sequential analysis. Anaesthesia. 2021;76:101–17.
Zhang W, Fang C, Li J, et al. Single-dose, bilateral paravertebral block plus intravenous sufentanil analgesia in patients with esophageal cancer undergoing combined thoracoscopic–laparoscopic esophagectomy: a safe and effective alternative. J Cardiothorac Vasc Anesth. 2014;28:966–72.
Lee J, Kim S. The effects of ultrasound-guided serratus plane block, in combination with general anesthesia, on intraoperative opioid consumption, emergence time, and hemodynamic stability during video-assisted thoracoscopic lobectomy: A randomized prospective study. Medicine (Baltimore). 2019;98:e15385.
Patel SJ, Augoustides JGT. Serratus anterior plane block—a promising technique for regional anesthesia in minimally invasive cardiac surgery. J Cardiothorac Vasc Anesth. 2020;34:2983–5.
Baldinelli F, Capozzoli G, Pedrazzoli R, et al. Are thoracic wall blocks efficient after video-assisted thoracoscopy surgery-lobectomy pain? A comparison between serratus anterior plane block and intercostal nerve block. J Cardiothorac Vasc Anesth. 2021;35:2297–302.
Yeung JH, Gates S, Naidu BV, Wilson MJ, GaoSmith F. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016;2(2):CD009121.
Ardon AE, Lee J, Franco CD, et al. Paravertebral block: anatomy and relevant safety issues. Korean J Anesthesiol. 2020;73(5):394–400.
NeMoyer RE, Pantin E, Aisner J, et al. Paravertebral nerve block with liposomal bupivacaine for pain control following video-assisted thoracoscopic surgery and thoracotomy. J Surg Res. 2020;246:19–25.
Hegazy MA, Awad G, Abdellatif A, et al. Ultrasound versus thoracoscopic-guided paravertebral block during thoracotomy. Asian Cardiovasc Thorac Ann. 2021;29:98–104.
Acknowledgements
We would like to thank all the patients who participated in this study.
Funding
No funding or sponsorship was received for this study or publication of this article. The rapid service fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Chenchen Zhu and Jun Fang designed the study and wrote the first draft of the manuscript. Min Zhang, Jia Yang, and Qingtian Geng performed data collection and analysis. Qijian Li and Huaming Zhang contributed to the material preparation and technical operation, and Yanhu Xie designed the study and revised the manuscript. All authors read and approved the final manuscript.
Disclosures
Chenchen Zhu, Jun Fang, Min Zhang, Jia Yang, Qingtian Geng, Qijian Li, Huaming Zhang, and Yanhu Xie declare that they have no conflict of interest.
Compliance with Ethics Guidelines
The trial protocol was approved by the ethics committee of the First Affiliated Hospital of USTC (approval no. KY2019-108) and registered in the Chinese clinical trial registry (ChiCTR-2000033617). Each participant provided written informed consent before initiating any study-related procedures. This study was conducted in accordance with the Declaration of Helsinki.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhu, C., Fang, J., Yang, J. et al. The Role of Ultrasound-Guided Multipoint Fascial Plane Block in ElderlyPatients Undergoing Combined Thoracoscopic–Laparoscopic Esophagectomy: A Prospective Randomized Study. Pain Ther 12, 841–852 (2023). https://doi.org/10.1007/s40122-023-00514-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00514-0