Abstract
Introduction
Propofol is the main drug used to induce sedation for endoscopic procedures, and few drugs had shaken its dominant clinical use for a decade until the development of remimazolam. Remimazolam has been demonstrated to perform well in post-marketing studies on sedation for colonoscopy or other procedures requiring short periods of sedation. This study aimed to establish whether remimazolam was effective and safe for inducing sedation for hysteroscopy.
Methods
One hundred patients who were scheduled to undergo hysteroscopy were randomly assigned to receive induction with remimazolam or propofol. A dose of 0.25 mg/kg remimazolam was administered. Propofol was started at 2–2.5 mg/kg. Before remimazolam or propofol induction, 1 μg/kg fentanyl was infused. Hemodynamic parameters, vital signs, and bispectral index (BIS) values were measured and adverse events recorded to evaluate safety. We comprehensively evaluated the efficacy and safety of the two drugs by the success rate of induction, fluctuation of vital signs, depth of anesthesia, adverse reactions, recovery time, and other indicators.
Results
Information on 83 patients was successfully recorded and carefully documented. The success rate of sedation in the remimazolam group (group R) was 93%, which was lower than for the propofol group (group P) (100%), but there was no statistically significant difference between the two groups. The incidence of adverse reactions in group R (7.5%) was significantly lower than that in group P (67.4%), and the results were statistically significant (P < 0.01). The fluctuation of vital signs in group P was more severe after induction, especially in patients with cardiovascular diseases.
Conclusions
Remimazolam avoids the injection pain produced by propofol sedation, has a better pre-sedation experience, had the advantage of stable hemodynamics after injection compared to propofol, and a lower respiratory depression rate in the study patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Remimazolam is a relatively new sedative drug, and many studies have reported that it has high safety, but there are few studies on sedation for hysteroscopy. |
Hysteroscopy under sedation improves the patient's comfort and coordination, shortens the examination time, and improves efficiency. |
To determine whether remimazolam can successfully produce satisfactory hysteroscopic sedation and to explore and additional effects on patients during sedation. |
What was learned from the study? |
The success rate of sedation in the remimazolam group was 93%, with no statistical significance difference compared to the propofol group (P > 0.05). The incidence of adverse reactions in the remimazolam group was 7.5% and was significantly lower than that in the propofol group (67.4%) (P < 0.01). |
Remimazolam is effective and safe in inducing sedation required for hysteroscopy, mainly because it elicited almost no injection pain, and the fluctuations in respiration, heart rate, and blood pressure were less than for the commonly used propofol. |
The experiment design of this study is rigorous, the operation flow is consistent, the bias caused by different operators and different devices is excluded, and the experimental results have high credibility. The data are calculated by professional statistical software, and the statistical process is calculated under appropriate conditions. |
Introduction
Hysteroscopy, considered the gold standard technique for the evaluation and management of intrauterine pathology, is performed using endoscopy to access the uterine cavity [1]. It allows for minimally invasive diagnosis and surgical management of endocervical and intrauterine pathology [1]. Indications for hysteroscopy are numerous, including abnormal uterine bleeding, infertility, removal of intrauterine foreign bodies, and congenital Mullerian anomalies [1].
Remimazolam, one of the newest ultra-short-acting benzodiazepines, was developed by GSK [2] and was approved for use in China in July 2020 as a programmed sedative drug in adults. Similar to midazolam, remimazolam enhances γ-aminobutyric acid A (GABAA) receptor activity to induce cell membrane hyperpolarization, thereby inhibiting neural activity via an increase in chloride influx [3]. With similar structural modifications to remifentanil, remimazolam is rapidly hydrolyzed to a pharmacologically inactive metabolite (CNS-7054) through the actions of non-specific tissue esterase activity [4]. Remimazolam is termed a “soft drug”, i.e., it is pharmacologically active and is biotransformed or degraded in vivo to what are termed predictable nontoxic and inactive metabolites [5]. Both painless gastroscopy and hysteroscopy require the use of sedatives that take effect quickly, are rapidly metabolized, have no accumulation, a good safety profile, and from which patients wake up quickly. The safety and efficacy of remimazolam for endoscopic sedation have been internationally recognized. However, there are relatively few observational studies on remimazolam for hysteroscopy, and therefore this trial was conducted to learn more about remimazolam’s actions during hysteroscopy.
Methods
Grouping
This was a single-center randomized controlled trial that assessed the efficacy and safety of remimazolam tosylate versus propofol in patients undergoing hysteroscopy. The patients were randomly allocated by computer-generated randomization to a remimazolam group (N = 40) or a propofol group (N = 43) to receive remimazolam tosylate or propofol for sedation during hysteroscopy.
Patients were eligible if they met all of the following inclusion criteria: (1) scheduled to undergo hysteroscopy; (2) aged 20–60 years; (3) American Society of Anesthesiologists (ASA) physical status classification system risk class I–II; (4) patients voluntarily participated in the trial, signed informed consent, and complied with the protocol requirements; (5) patient was scheduled to undergo only basic hysteroscopy and segmental dilation and curettage; (6) the patient’s disease type included only abnormal uterine bleeding. Exclusion criteria were (1) the endoscopy procedure was expected to take more than 30 min; (2) heart disease; (3) respiratory disease (acute respiratory infection, acute onset of chronic obstructive pulmonary disease, uncontrolled asthma); (4) psychiatric disorders; (5) obviously abnormal liver and kidney functions; (6) history of drug abuse; (7) allergy or a contraindication to benzodiazepines, opioids, propofol, and their components [6]; (8) patients with unstable vital signs.
Process
The trial protocols were approved by the hospital ethics committee before implementation. One day before hysteroscopy, we received a patient list, and the trial personnel considered whether the patient met the inclusion criteria on the basis of the patient’s basic and general information. If the patient agreed to participate in the trial, the relevant informed consent form was signed. All procedures performed in studies were in accordance with the ethics committee of the Ninth People’s Hospital of Chongqing number 2021(伦审017) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. After the patient entered the examination room, the last feeding time was documented, they were placed in the examination position, and ECG monitoring, oxygen saturation, non-invasive blood pressure measurements, and bispectral index (BIS) sensors were connected. About 3–5 min before starting the examination, fentanyl (Yichang Humanwell Pharmaceutical Co., Ltd.) 1 μg/kg was administered intravenously by injection. Remimazolam besylate (Yichang Humanwell Pharmaceutical Co., Ltd.) 0.25 mg/kg was intravenously injected in the remimazolam group (group R), and in the propofol (AstraZeneca Pharmaceuticals Co. Ltd., China) group (group P), 2.5 mg/kg propofol was injected intravenously. The same gynecologist used the same manufacturer’s instruments with the same specifications to perform the operation, and the operation procedures were consistent. The types of procedures were also limited, with patients included undergoing only basic hysteroscopy and fractional curettage procedures; hysteroscopic procedures and examinations longer than 30 min were excluded. The sedative effect of 0.2 mg/kg remimazolam is no less than that of propofol (at dosage of 2.0–2.5 mg/kg) [7]. However, during the process of sedation, although the patient fell asleep after an intravenous injection of 7 mg remimazolam, obvious body movements were observed when hysteroscopy commenced. When the researchers increased the injection concentration to 0.25 mg/kg, the body movements decreased significantly. It has been pointed out that the maximum tolerated single intravenous dose of remimazolam is 0.4 mg/kg [8]. In the present trial, patients received a theoretically safe dose of remimazolam that was within the maximum they could tolerate. The depth of anesthesia was maintained by additional doses according to the BIS value. The BIS value was not higher than 60 during the maintenance of sedation. The supplementary doses of remimazolam were 2.5 mg each time, but no more than five supplements, and the dose of propofol was 0.5–1 mg/kg. After the initial dose, if five doses was not sufficient, the rescue medication was administered. Severe hypoxemia, hypotension, and a low heart rate were managed during the procedure. In the course of the experiment, rescue drugs and tools were fully prepared to protect the safety of patients.
Outcomes
(1) The basic information on each patient was recorded, including their age, height, weight, and BMI index. (2) Heart rate (HR), diastolic blood pressure (DBP), and systolic blood pressure (SBP), oxygen saturation (SpO2), and the BIS score was recorded at three time points. T0 refers to the time point before the start of hysteroscopy; T1 the time point at the beginning of the procedure; T2 the time point at which the procedure was completed. (3) BIS score were recorded at T0, T1, and T2. Sheng et al. reported that BIS monitoring is appropriate for assessing awareness signs during remimazolam sedation [8]. Therefore, in this study, we used the BIS scores to assess the depth of sedation. (4) The number of cases of sedation failure was used to calculate the failure rate between the two drug groups. Sedation failure was defined as when the induction dose plus five additional intravenous doses was not sufficient to complete the hysteroscopy procedure (hysteroscopic procedures lasting more than 30 min were excluded). (5) Recovery time was defined as the time from the beginning of the last drug injection until the BIS score was greater than 75. (6) The number, type, and severity of adverse events were recorded, including respiratory depression, hypotension, hypertension, bradycardia, tachycardia, injection pain, hiccups, dizziness, nausea, vomiting, and so on. Hypertension or hypotension was defined as a fluctuation greater than 20% from the basal blood pressure values.
Sample Size and Statistical Analysis
SPSS Statistics 27.0.1.0 (IBM Corp. in Armonk, NY) was used for all statistical analyses. A one-sided type I error rate of 0.025 and a power of 90% were adopted. According to a previous study in 2021 [9], the sampling size calculation was based on the assumption of an adverse events rate of 36.6% [9] for group P and 3.7% [9] for group R, requiring sample sizes of 34 patients per treatment group. The sample size in each group was expanded to about 40 to allow for a 20% dropout rate.
All data are presented as mean ± standard deviation or numbers and percentages when appropriate. Quantitative variables were tested for normality using the Shapiro–Wilk test. Comparison of normally distributed quantitative variables between groups was performed using Student’s t test. Asymmetrically distributed quantitative data were analyzed using the Mann–Whitney U test. Qualitative variables between groups were compared using the χ2 test and hemodynamic parameters compared using repeated measures analysis of variance (ANOVA). All analysis was assessed with a two-tailed test and P < 0.05 was deemed to indicate statistical significance.
Results
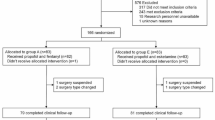
From March 2022 to September 2022, 125 patients were initially willing to participate in this study, of whom 31 were excluded. A total of 94 were randomly divided into the remimazolam group or the propofol group and 11 patients could not complete the trial. The detailed protocol is shown in Fig. 1. Ultimately, 83 patients participated in the trial. Their basic information is shown in Table 1, namely the beginning of surgery, age, height, weight, BMI, HR, SBP, DBP, and BIS scores, which were all similar between the two groups of patients.
Primary Outcome
The primary outcomes of the study were the success and adverse event rates. The comparison of rates is shown in Table 2. The procedure success rate was 100% in the propofol group and 92% in the remimazolam group, the difference in the success rate being 0.075 (95% CI 0.990–1.181), with no obvious difference between the two groups (P > 0.05). Adverse events observed during the study included hiccup, respiratory depression, nausea and vomiting, bradycardia, injection pain, and noteworthy fluctuations in blood pressure. The adverse event rate was 67.4% in the propofol group and 7.5% in the remimazolam group and the difference in the adverse event rate was 0.599 (95% CI 0.227–0.546), with a significant difference found between the two groups (P < 0.001).
Safety Assessment
Compared with the propofol group, the remimazolam group exhibited a lower incidence of adverse events, less injection pain, respiratory depression, fluctuations in blood pressure, variations in heart rate, and less decreases in oxygen saturation. Comparison of the heart rate, blood pressure, and oxygen saturation at three time points during hysteroscopy showed that the remimazolam group had a smaller amplitude of fluctuations. Figures 2, 3, 4, and 5 depict the trends of heart rate, blood pressure, and oxygen saturation at three time points. The heart rate, systolic blood pressure, and respiratory rate observed at the T1 time point, which was the beginning of the produce, were significantly different between the two groups (P < 0.05), presented in Table 3.
BIS
Scores
BIS values did not conform to the normal distribution and were therefore reported as the median and interquartile range. The Mann–Whitney U test was used for non-normally distributed continuous variables. The BIS values recorded at the beginning of the procedure showed that the remimazolam group had a more appropriate depth of anesthesia compared to the propofol group, which had a deeper degree of sedation. The comparison values between the two groups are shown in Table 4, and the trend plot is shown in Fig. 6.
Recovery Time
Recovery time (RT) was defined from the beginning of the last drug injection until the BIS score being greater than 75. Compared with the remimazolam group (10.208 ± 0.342 min), the recovery time of the propofol group (7.912 ± 0.476 min) was significantly shorter than that of the remimazolam group, with the difference being statistically significant. A box plot of the results is shown in Fig. 7.
Discussion
The main objective of this study was to compare the safety and efficacy of remimazolam and propofol during hysteroscopy sedation. According to the related indicators recorded, we found the following: (1) Remimazolam administration allowed the hysteroscopy to be performed. (2) Compared to propofol, remimazolam elicited fewer adverse events. The probability of injection pain elicited by propofol was higher, which seriously affected the experience of patients, goes against the original intention of painless medical treatment, and cannot better achieve the purpose of comfortable medical treatment. (3) In terms of safety, remimazolam led to fewer hemodynamic fluctuations than propofol; remimazolam consistently produced a more appropriate depth of sedation. In summary, remimazolam and propofol had similar success rates for sedation, but remimazolam had a more favorable safety profile.
According to the drug package insert of remimazolam besylate approved for marketing in China, the typical adult dose of remimazolam for procedural sedation is 7 mg administered by an intravenous injection over 1 min and then 2.5 mg via intravenous injection over 15 s as a rescue dose. Several previous studies [6, 10] have demonstrated that an initial loading dose of 7 mg can also achieve satisfactory endoscopic sedation. Previous clinical trials found that remimazolam could induce either a low sedation level or a deep sedation level by using different doses [11, 12]. However, according to the standard of 7 mg initial dose, although it can meet the requirements of sedation, it is not satisfactory to complete a hysteroscopy procedure. Even if the measurements of analgesia were increased, the patient may also have an obvious body movement reaction due to the lack of sedation depth. The initial dose was administered according to the weight standard. While researchers [13] have explained why remimazolam can be given without considering the weight of the patient (weight range studied 65–90 kg), this will likely not mean that the dose should never be adjusted. This is because we also have to consider the effect of lower body weight and different degrees of physical fitness that may influence the drug’s actions. Therefore, we believe that it is more reasonable to set the drug dose according to body weight. It is suggested that remimazolam has a wide therapeutic window for endoscopic sedation [14], indicating the potential of remimazolam for conducting various procedures that require different depths of patient sedation.
One important concern regarding sedation for endoscopy is sedation-related complications [15], which can lead to significant morbidity and occasional mortality in patients [16]. In particular, propofol is often responsible for producing serious cardiovascular and respiratory depression, often requiring endotracheal intubation [17], but few studies have reported similar effects of remimazolam. The cardiorespiratory suppression f propofol is caused by its effect on central chemoreceptor sensitivity [6]. Propofol induces unconsciousness through GABAA-mediated inhibition of histamine release in the hypothalamus, blockade of N-methyl-d-aspartate receptors, and modulation of calcium influx to inhibit postsynaptic neuronal activity [18]. Thus, preventing or reducing the occurrence of sedation-related complications is the best form of clinical management of the patient [14]. Despite remimazolam and propofol both causing transient cardiovascular and respiratory depression, the effects of remimazolam are likely to be less severe. Theoretically, cardiovascular and respiratory depression is often associated with moderate and deep sedation levels [19]. Here, we have demonstrated that propofol produced a deeper depth of sedation, more severe cardiovascular events and respiratory depression, and the injection pain elicited by propofol reached 48.8%. We observed that 21 patients experienced different degrees of injection pain, but some reported severe pain and even shed tears during the injection. There was no similar phenomenon during remimazolam administration. Pain has a strong negative effect on emotions. If the patient feels anxious and agitated because of pain before entering the sedation state, this emotion will continue after resuscitation, which will affect the painless experience, thus contrary to the original intention of painless endoscopy. Further analysis revealed the reduction of postoperative recovery in the remimazolam group, which focused on the aspects of physical comfort and emotional state of the patient [20]. This trial is very important, as it has provided us with a way to evaluate general sedation with remimazolam from the point of view of postoperative recovery [20].
In clinical studies, it was found that the conclusions were different in terms of recovery time, the reason being that the induction dose of remimazolam was different. In our research, the recovery time of the remimazolam group was significantly longer than that of the propofol group. Some literature conclusions include that remimazolam showed faster recovery from sedation compared with propofol [14]; the ultra-short action of remimazolam leads to its rapid breakdown into an inactive metabolite by tissue esterases [21]; the time to adequate sedation may be associated with the initial loading dose of remimazolam, which would affect the time and speed required to achieve adequate sedation under the drug titration pattern [14]. As a result, if the dose is followed according to the manufacturer’s instructions, sedation can be completed in patients with the first loading dose but would be bound to extend the time to sedation; this action can be attributed to the lower depth of sedation induced by remimazolam, as the endoscopy is a short procedure that does not require deep sedation. In a previous phase 1 study in volunteers, remimazolam was shown to produce deep sedation with a fast onset of action and recovery due to its relatively high clearance, a small steady-state volume of distribution, and a short elimination half-life [22]. Thus, investigations into its optimized initial loading dose should be carried out.
Remimazolam was first synthesized and reported in 2007. It is a water-soluble, ultra-short-acting intravenously administered benzodiazepine that binds with high affinity to the GABAA receptor. The enhancement of GABA activity is similar to that caused by midazolam but with marginally greater potency and maximum effect. The principal metabolite of remimazolam, CNS-7054, binds with a 410 times lower affinity than the parent drug and is considered to be inactive [23]. The incorporation of an ester linkage in remimazolam permits hydrolysis by tissue esterases to an inactive metabolite [24]. Tissue esterases are distributed throughout the body, so the drug is rapidly metabolized when administration ceases. Elimination of remimazolam is organ-independent; like remifentanil, it acts on the same receptor as midazolam—GABA [25]. The sedative effect of remimazolam is caused by modulation of the GABA receptor, like most sedative-hypnotic agents. Remimazolam is metabolized rapidly, mainly by liver tissue esterases, and is predominantly excreted in the urine. After 24 h of remimazolam injection (0.2 or 0.3 mg/kg IV), more than 80% of the dose was detected in the urine as a metabolite and less than 1% of the original dose was detected as unchanged drug [26]. The binding of remimazolam to plasma proteins was approximately 92%, predominantly serum albumin [27]. The pharmacokinetics and pharmacodynamics of remimazolam are characterized by relatively high clearance, a small steady-state volume of distribution, short elimination half-life, short context-sensitive half-life, and fast onset and recovery, indicating rapid elimination, minimal tissue accumulation, and good control in a clinical setting [28].
In 1985, Dundee [29] wrote: “Ideally one would like a water-soluble, non-irritant, rapidly acting, smooth induction agent with no analgesic action. Cardiovascular and respiratory depression should be minimal with normal dosage... A slight delay in onset would not be a major obstacle, provided this is predictable.” Through literature review and this study, we know that remimazolam has the advantages of a rapid onset and offset of sedation, a predictable duration, less impact on the respiratory and circulatory system, fewer injection-site reactions during administration, and the availability of flumazenil to reverse the sedative effects. To date, we believe that remimazolam is the closest to an ideal sedative drug. Remimazolam is unlikely to cause RYR1-mediated hyperthermia mutation (MH), so it has been speculated to be potentially safe for use in MH-sensitive patients [30]. This makes the advantage of remimazolam even more obvious.
Conclusions
Remimazolam can be safely and effectively used for sedation during hysteroscopy procedures lasting less than 30 min. Its advantages include less impact on the cardiovascular and respiratory systems, appropriate depth of sedation, it produces a lower incidence of adverse events and no injection pain. It is the closest to a perfect sedative and the most promising new drug for use in sedation during endoscopy. However, more research is needed to improve its safety and efficacy, such as differences relating to gender, age, and weight groups, as well as its use among critically ill patients.
References
Moore JF, Carugno J. Hysteroscopy. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022.
Goudra BG, Singh PM. Propofol alternatives in gastrointestinal endoscopy anesthesia. Saudi J Anaesth. 2014;8:540–5. https://doi.org/10.4103/1658-354X.140893.
Hu K, Xiang Q, Wang Z, et al. Effects of vitamin D receptor, cytochrome P450 3A, and cytochrome P450 oxidoreductase genetic polymorphisms on the pharmacokinetics of remimazolam in healthy Chinese volunteers. Clin Pharmacol Drug Dev. 2021;10:22–9. https://doi.org/10.1002/cpdd.797.
Egan TD. Is anesthesiology going soft?: trends in fragile pharmacology. Anesthesiology. 2009;111:229–30.
Greenblatt DJ. A soft benzodiazepine. Clin Pharmacol Drug Dev. 2015;4:81–2. https://doi.org/10.1002/cpdd.186.
Chen S, Wang J, Xu X, et al. The efficacy and safety of remimazolam tosylate versus propofol in patients undergoing colonoscopy: a multicentered, randomized, positive-controlled, phase III clinical trial. Am J Transl Res. 2020;12:4594–603.
Doi M, Hirata N, Suzuki T, et al. Safety and efficacy of remimazolam in induction and maintenance of general anesthesia in high-risk surgical patients (ASA class III): results of a multicenter, randomized, double-blind, parallel-group comparative trial. J Anesth. 2020;34:491–501. https://doi.org/10.1007/s00540-020-02776-w.
Sheng XY, Liang Y, Yang XY, et al. Safety, pharmacokinetic and pharmacodynamic properties of single ascending dose and continuous infusion of remimazolam besylate in healthy Chinese volunteers. Eur J Clin Pharmacol. 2020;76:383–91. https://doi.org/10.1007/s00228-019-02800-3.
Zhang X, Li S, Liu J. Efficacy and safety of remimazolam besylate versus propofol during hysteroscopy: single-centre randomized controlled trial. BMC Anesthesiol. 2021;21:156. https://doi.org/10.1186/s12871-021-01373-y.
Pastis NJ, Yarmus LB, Schippers F, et al. Safety and efficacy of remimazolam compared with placebo and midazolam for moderate sedation during bronchoscopy. Chest. 2019;155:137–46. https://doi.org/10.1016/j.chest.2018.09.015.
Pambianco DJ, Borkett KM, Riff DS, et al. A phase IIb study comparing the safety and efficacy of remimazolam and midazolam in patients undergoing colonoscopy. Gastrointest Endosc. 2016;83:984–92. https://doi.org/10.1016/j.gie.2015.08.062.
Worthington MT, Antonik LJ, Goldwater DR, et al. A phase Ib, dose-finding study of multiple doses of remimazolam (CNS 7056) in volunteers undergoing colonoscopy. Anesth Analg. 2013;117:1093–100. https://doi.org/10.1213/ANE.0b013e3182a705ae.
Masui K. Remimazolam besilate, a benzodiazepine, has been approved for general anesthesia!! J Anesth. 2020;34:479–82. https://doi.org/10.1007/s00540-020-02755-1.
Chen SH, Yuan TM, Zhang J, et al. Remimazolam tosilate in upper gastrointestinal endoscopy: a multicenter, randomized, non-inferiority, phase III trial. J Gastroenterol Hepatol. 2021;36:474–81. https://doi.org/10.1111/jgh.15188.
Wernli KJ, Brenner AT, Rutter CM, Inadomi JM. Risks associated with anesthesia services during colonoscopy. Gastroenterology. 2016;150:888–94. https://doi.org/10.1053/j.gastro.2015.12.018. (quiz e18).
Razpotnik M, Bota S, Essler G, Weber-Eibel J, Peck-Radosavljevic M. Impact of endoscopist experience, patient age and comorbidities on dose of sedation and sedation-related complications by endoscopic ultrasound. Eur J Gastroenterol Hepatol. 2022;34:177–83. https://doi.org/10.1097/MEG.0000000000002084.
Choi GJ, Kang H, Baek CW, Jung YH, Ko JS. Etomidate versus propofol sedation for electrical external cardioversion: a meta-analysis. Curr Med Res Opin. 2018;34:2023–9. https://doi.org/10.1080/03007995.2018.1519501.
Roback MG, Carlson DW, Babl FE, Kennedy RM. Update on pharmacological management of procedural sedation for children. Curr Opin Anaesthesiol. 2016;29(Suppl 1):S21-35. https://doi.org/10.1097/ACO.0000000000000316.
Amornyotin S. Sedation-related complications in gastrointestinal endoscopy. World J Gastrointest Endosc. 2013;5:527–33. https://doi.org/10.4253/wjge.v5.i11.527.
Mao Y, Guo J, Yuan J, Zhao E, Yang J. Quality of recovery after general anesthesia with remimazolam in patients’ undergoing urologic surgery: a randomized controlled trial comparing remimazolam with propofol. Drug Des Devel Ther. 2022;16:1199–209. https://doi.org/10.2147/DDDT.S359496.
Rex DK, Bhandari R, Desta T, et al. A phase III study evaluating the efficacy and safety of remimazolam (CNS 7056) compared with placebo and midazolam in patients undergoing colonoscopy. Gastrointest Endosc. 2018;88:427-37 e6. https://doi.org/10.1016/j.gie.2018.04.2351.
Schuttler J, Eisenried A, Lerch M, et al. Pharmacokinetics and pharmacodynamics of remimazolam (CNS 7056) after continuous infusion in healthy male volunteers: Part I. pharmacokinetics and clinical pharmacodynamics. Anesthesiology. 2020;132:636–51. https://doi.org/10.1097/ALN.0000000000003103.
Sneyd JR, Gambus PL, Rigby-Jones AE. Current status of perioperative hypnotics, role of benzodiazepines, and the case for remimazolam: a narrative review. Br J Anaesth. 2021;127:41–55. https://doi.org/10.1016/j.bja.2021.03.028.
Sneyd JR. Remimazolam: new beginnings or just a me-too? Anesth Analg. 2012;115:217–9. https://doi.org/10.1213/ANE.0b013e31823acb95.
Oka S, Satomi H, Sekino R, et al. Sedation outcomes for remimazolam, a new benzodiazepine. J Oral Sci. 2021;63:209–11. https://doi.org/10.2334/josnusd.21-0051.
Zhou Y, Hu P, Jiang J. Metabolite characterization of a novel sedative drug, remimazolam in human plasma and urine using ultra high-performance liquid chromatography coupled with synapt high-definition mass spectrometry. J Pharm Biomed Anal. 2017;137:78–83. https://doi.org/10.1016/j.jpba.2017.01.016.
Kilpatrick GJ. Remimazolam: non-clinical and clinical profile of a new sedative/anesthetic agent. Front Pharmacol. 2021;12:690875. https://doi.org/10.3389/fphar.2021.690875.
Kim KM. Remimazolam: pharmacological characteristics and clinical applications in anesthesiology. Anesth Pain Med (Seoul). 2022;17:1–11. https://doi.org/10.17085/apm.21115.
Dundee JW. Intravenous anaesthesia and the need for new agents. Postgrad Med J. 1985;61(Suppl 3):3–6.
Watanabe T, Miyoshi H, Noda Y, et al. Effects of remimazolam and propofol on Ca(2+) regulation by ryanodine receptor 1 with malignant hyperthermia mutation. Biomed Res Int. 2021;2021:8845129. https://doi.org/10.1155/2021/8845129.
Acknowledgements
We thank the patients and gynecologists in our hospital or participating in the study.
Funding
Not applicable. We have not received any funding from the company that provided the products necessary for the execution of the clinical trial.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Dr. Shunyi Fan, Dr. Qian Li were involved in conduct of the study. Dr. Changzhong Sui was involved in designing the study. Dr. Yun Zhu, Dr. Wenxin Jiang, and Dr. Li Zhang were involved in data interpretation and manuscript writing and finalizing. All authors have read and approved the final manuscript.
Disclosures
The design and conduct of the clinical trial were entirely carried out by the authors of this manuscript without any indication from the company that provided the products necessary for the experimentation. The authors, Shunyi Fan, Yun Zhu, Changzhong Sui, Qian Li, Wenxin Jiang, and Li Zhang, have no conflicts of interest to declare.
Compliance with Ethics Guidelines
This study does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethics committee of Ninth People’s Hospital of Chongqing number 2021 (伦审017) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was provided by all individual patients included in the study.
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fan, S., Zhu, Y., Sui, C. et al. Remimazolam Compared to Propofol During Hysteroscopy: A Safety and Efficacy Analysis. Pain Ther 12, 695–706 (2023). https://doi.org/10.1007/s40122-023-00483-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00483-4