Abstract
Introduction
Postoperative analgesia in elderly patients is still a thorny problem. Ultrasound-guided oblique subcostal transverse abdominis plane block (TAPB) has been demonstrated to provide postoperative analgesia after abdominal surgeries. However, recent studies have suggested that an alternative method, erector spinae plane block (ESPB), might also be effective. In this study, we compared the postoperative analgesic effects of ESPB and TAPB in elderly patients who had undergone laparoscopic colorectal surgery.
Methods
Sixty-two elderly patients (≥ 65 years old) scheduled for elective laparoscopic colorectal surgery with general anesthesia were randomly allocated to two equally sized groups: ESPB group and TAPB group. The ESPB group had a bilateral erector spinae plane block, and the TAPB group had a bilateral oblique subcostal transverse abdominis plane block. The primary outcome was visual analogue scale (VAS) pain score during the first 24 postoperative hours at resting and active states. The secondary outcomes were postoperative consumption of sufentanil, satisfaction score, the number of patients who required antiemetics, incidence of block-related complications, and other side events.
Results
There were no demographic differences between two groups. Compared to the TAPB group, the ESPB group had lower VAS pain scores and sufentanil consumption during the first 24 postoperative hours. Additionally, ESPB reduced the occurrence of postoperative nausea and vomiting. Furthermore, the satisfaction score was higher in the ESPB group. No other complications were reported between the two groups.
Conclusions
Compared with oblique subcostal TAPB, ESPB more effectively reduced postoperative pain and opioid consumption. Thus, ESPB is suitable for postoperative analgesia in elderly patients who have undergone laparoscopic colorectal surgery.
Trial Registration
Chinese Clinical Trial Registry: ChiCTR2000033236.
Similar content being viewed by others
Why carry out this study? |
Postoperative analgesia in elderly patients is still challenging due to high rates of degenerative liver and kidney functioning. |
Erector spinae plane block (ESPB) is a novel regional block technique have reported could be relieve postoperative pain, but the application in elderly patients after laparoscopic colorectal surgery has not been presented. |
We conducted this prospective randomized study to investigate the safety and effectiveness of ESPB in analgesia after laparoscopic colorectal surgery in elderly patients. |
What was learned from the study? |
This study showed that ESPB more effectively reduced postoperative pain and opioid consumption compared with oblique subcostal transverse abdominis plane block (TAPB). |
ESPB reduced the occurrence of postoperative nausea and vomiting. |
Patients treated with ESPB had higher satisfaction scores. |
Introduction
Among elderly patients that underwent curative resection of colorectal cancer, laparoscopic surgery was applied as a surgical method for more than 60% [1]. Pain after major abdominal surgeries not only causes a strong stress reaction and adverse emotional experience but also affects postoperative rehabilitation [2, 3]. However, the application of postoperative analgesia is still challenging due to high rates of degenerative liver and kidney functioning in elderly patients [4, 5]. Although it is a traditional regional anesthesia technique, epidural anesthesia carries risks of hypotension, urinary retention, and epidural hematoma [6, 7]. Opioid-based patient-controlled intravenous analgesia (PCIA) is also widely employed for relieving postoperative pain after colorectal surgeries [8, 9]. However, opioids can cause a range of side effects, from relatively mild symptoms such as nausea, vomiting, and itching, to serious symptoms including respiratory depression [10]. Therefore, it is necessary to find a safe and effective method to relieve pain after laparoscopic colorectal surgery in elderly patients.
Oblique subcostal transverse abdominal plane block (TAPB) is a regional block technique in which local anesthetics are injected between the transverse abdominal muscle plane and the internal oblique abdominal muscle plane [11]. TAPB relieves pain after abdominal surgery by blocking the sensory nerve of the anterolateral abdominal wall (T6-L1) [12]. A large number of studies have confirmed that TAPB can provide safe and effective postoperative analgesia for patients undergoing a variety of abdominal surgeries, including laparoscopic cholecystectomies [13], hysterectomies [14], and gastrointestinal surgeries [15].
Erector spinae plane block (ESPB) is a novel interfascial plane block technique that was firstly described by Forero and colleagues in 2016. It involves injecting local anesthetic into the plane between the deep fascia of the erector spinae muscle and the vertebral transverse process under ultrasound guidance to relieve acute and chronic neuropathic pain in the thoracoabdominal region [16]. Although ESPB was first used for chronic pain, it has now been widely employed as a postoperative analgesia in a variety of surgeries involving the shoulder and hip regions [17, 18]. Recent studies have demonstrated that ESPB plays an important role in analgesia after abdominal surgeries [19, 20]. However, there are still few studies focusing on the use of ESPB for postoperative analgesia in elderly patients after abdominal surgeries.
Thus, we performed a randomized controlled study to compare the effects of ultrasound-guided ESPB and oblique subcostal TAPB in decreasing postoperative pain in elderly patients who had undergone laparoscopic colorectal surgery.
Methods
We conducted this prospective, randomized, single-center clinical trial from June 2020 to July 2021, following the principles of the Declaration of Helsinki. The study was examined and approved by the Ethics Committee of Jiaxing First Hospital and was registered on the Chinese Clinical Trial Register (ChiCTR2000033236). All participants were informed of the risks of the study and signed an informed consent form. We also performed this study in accordance with Consolidated Standards of Reporting Trials (CONSORT) guidelines.
We enrolled elderly patients aged above 65 years with an American Society of Anesthesiology (ASA) physical status of I–III who were undergoing elective laparoscopic colorectal surgery. Exclusion criteria included: having blood clot dysfunction or being on anticoagulant therapy; experiencing serious complications associated with other systems (such as severe cardiac insufficiency, renal failure, and hepatic encephalopathy); allergy to local or general anesthetics; having a skin infection at or near the puncture site; having a history of opioid abuse; or inability to cooperate with the assessment of visual analogue scale (VAS) pain scores.
On the day of the operation, all participants were randomly divided into two equally sized groups (an ESPB group, which received ultrasound-guided bilateral erector spinae plane block at the T9 level; and TAPB group, which received an ultrasound-guided bilateral oblique subcostal transversus abdominis plane block). Randomization was achieved by using computer-generated random numbers, which were then placed in separate opaque envelopes and kept by a data administrator. The anesthesiologist who performed general anesthesia and the nurse who recorded the postoperative evaluations were blinded to group status. All ESPBs and TAPBs were performed in the anesthesia preparation room before the surgery by the same anesthesiologist, who was not involved in the rest of the study. The concentration and dose of local anesthetics refer to a previous study [21]. Midazolam 1 mg was given to all patients through intravenous access. Blood pressure, electrocardiogram, and pulse oxygen saturation monitoring took place throughout the block process.
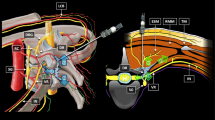
ESPB Application
After the patients were placed in the lateral recumbent position, the skin near the puncture site was disinfected. A convex ultrasound probe (GE Medical Systems Ultrasound and Primary Care Diagnostics LLC, USA) was placed vertically at the lateral 2–3 cm of the T9 vertebrae to identify the transverse process and erector spinal muscle. Then, 1% lidocaine was injected into the puncture site for local infiltration. Using an in-plane technique, a No. 22 needle (PAJUNK Gmbh, Medizintechnologie, Germany) was inserted through the muscle to touch the T9 transverse process. Next, 2 ml of saline was injected to separate the erect spinal muscle from the transverse process and further determine the position of the needle. After confirmation that the position of the needle was normal, and after excluding incidence of endovascular puncture, 0.25% ropivacaine mixed with normal saline for 20 ml was injected. The ultrasound showed that the local anesthetic separated the erector spinal muscle and the transverse process, confirming the success of the injection (Supplementary Material). Finally, the same steps were repeated on the other side.
Oblique Subcostal TAPB Application
After placing the patients in the supine position, the skin was disinfected. A linear probe (GE Medical Systems Ultrasound and Primary Care Diagnostics LLC, USA) was placed on the abdominal wall below the costal edge to identify three layers of muscles (abdominal external oblique muscles, abdominal internal oblique muscles, and abdominal transverse muscles) lateral to the linea semilunaris. A No. 22-G needle (PAJUNK Gmbh, Medizintechnologie, Germany) was placed in the space between the internal oblique muscle and the transverse muscle of the abdomen using the in-plane technique; 2 ml of saline was injected to separate the internal oblique muscle and the transverse muscle and to confirm the position of the needle. After negative aspiration, 0.25% ropivacaine mixed with normal saline for 20 ml was injected. The ultrasound showed that the local anesthetic separated the internal oblique muscle and the transversus abdominis muscle, confirming the success of the injection (Supplementary Material). Finally, the same procedure was repeated on the other side.
General Anesthesia
All patients were sent to the operating room for general anesthesia after receiving different interventions. Anesthesia was induced with sufentanil (0.5 ug/kg), propofol (2 mg/kg), and cisatracurium (0.2 mg/kg). After placing an endotracheal tube, general anesthesia was maintained using sevoflurane (1.5–2%) with 50% oxygen concentration, as well as remifentanil (0.1–0.2 μg/kg/min) to keep the bispectral index range between 40 and 60. The anesthetic dose was adjusted to maintain blood pressure within 20% of the baseline value. Additional doses of cisatracurium were administered when necessary. Ventilation parameters were set to a tidal volume of 6–8 ml/kg and a respiration rate of 12–14 beats/min to maintain ETCO2 between 30 and 40 mmHg. At the end of surgery, every patient was intravenously administrated 6 mg of ondansetron to relieve postoperative nausea and vomiting. All patients were sent to the postanesthesia care unit (PACU) after their operations. In the PACU, all patients were equipped with a PCIA containing 1 μg/ml of sufentanil with background infusion 2 ml, and a dose of 2 μg sufentanil that was locked for 20 min. For patients with a VAS score above 5 at active state or above 3 at rest state, the analgesic pump was pressed once, and the pain score was assessed again after 0.5 h. When the patient’s VAS score was still high, the analgesic pump was pressed again. The rescue antiemetic, metoclopramide, was given as a 5-mg dose intravenously in cases of severe nausea or two or more emetic episodes, or in response to the patient's request.
Outcomes
The primary outcome was VAS pain scores during the first 24 postoperative hours at resting and active states (with coughing). Secondary outcomes included postoperative consumption of sufentanil, satisfaction score, the number of patients who required antiemetics, incidence of block-related complications (bleeding, infection, pneumothorax, and bowel perforation) and other side events (nausea, vomiting, constipation, and respiratory depression (respiratory rate < 8 breaths/min)). A trained nurse who was blinded to group classification evaluated VAS pain scores at 0.5, 2, 4, 8, 12, 16, 20, and 24 postoperative hours. The time for extubation of the endotracheal tube was time 0. At 24 h after surgeries, satisfaction score was assessed with a numerical rating scale ranging from 1 (most unsatisfied) to 10 (most satisfied). Nausea and vomiting were assessed by a four-point verbal scale (none = no nausea, mild = nausea without vomiting, moderate = vomiting one attack, severe = vomiting > one attack).
Sample Size and Statistical Analyses
Required sample sizes were calculated using PASS 11.0 (NCSS, LLC, Kaysville, UT, USA), based on our pilot study, which showed mean of VAS pain scores values over 24 h of 2.61 ± 1.64 in the ESPB group, 3.96 ± 1.78 in the TAPB group. We performed analysis with α = 0.05 and power of 80%, which revealed that the number of patients required in each group was 28. Considering the 10% drop-out rate in clinical studies, we included 31 patients per group. All results were analyzed using SPSS 25.0 (IBM Corp. Armonk, NY, USA). Categorical variables were expressed by frequency (percentage) and analyzed using Fisher’s exact or the Chi-square tests. Kolmogorov–Smirnov tests were conducted to determine whether the continuous data conformed to a normal distribution. Normally distributed continuous variables were expressed as mean ± standard deviation, and independent samples T test was used to examine group differences. Non-normally distributed continuous variables were presented as median (interquartile range, IQR), and Mann–Whitney U tests were used to examine group differences. A two-sided p value of < 0.05 was considered statistically significant.
Results
Of the 74 elderly patients initially enrolled, 12 were excluded and 62 were included in the final analysis (four patients had their operations cancelled for various reasons; seven patients withdrew from the study before surgery; and one patient had a skin infection). Figure 1 shows the CONSORT diagram. There was no difference in demographic data (including age, height, weight, gender, ASA physical status, types of surgeries, duration of anesthesia ad surgery) between the two groups (Table 1).
Compared to the TAPB group, patients in the ESPB group had lower VAS pain scores throughout the first 24 postoperative hours at both resting (Fig. 2) and active states (Fig. 3).
Also, ESPB significantly decreased sufentanil consumption during the first 24 postoperative hours. Significantly lower occurrence of postoperative nausea and vomiting (PONV) was reported in the ESPB group compared to the TAPB group. Similarly, the number of patients who required rescue antiemetics was significantly reduced in the ESPB group. Furthermore, the satisfaction score was higher in the ESPB group (Table 2). No block-related complications were recorded in any of the patients (bleeding, infection, pneumothorax, and bowel perforation).
Discussion
Our findings indicated that, compared with oblique subcostal TAPB, ESPB could significantly reduce VAS scores during the first 24 postoperative hours. Additionally, patients in the ESPB group had significantly lower sufentanil consumption but higher satisfaction scores.
In recent years, the number of elderly patients undergoing laparoscopic colorectal surgery has significantly increased, and a considerable number of elderly patients had experienced severe pain after their operations. Severe postoperative pain affects the rehabilitation process of patients after their operations and is related to a series of postoperative complications, including increased length of hospital stays and increased costs of hospitalization [22]. As an important part of enhanced recovery after surgery (ERAS), effectively, relief of postoperative pain is a problem that needs to be solved. Pain after abdominal surgery mainly involves visceral and somatic components. For a long time, postoperative epidural analgesia was considered to be effective, but high requirements for blood coagulation and puncture techniques make it impossible for some patients to get these benefits [23]. It has been shown that incision-based local infiltration anesthesia can be used for postoperative analgesia, but its effects and action time are not fully satisfactory [24].
PICA with opioids is also a common method to relieve pain following surgeries. However, opioid-related complications are unbearable for some patients. Compared with drug-based analgesia, regional block techniques combined with general anesthesia appear to better control pain and reduce adverse drug reactions. Further, they do not interfere with respiratory functioning, which meets the requirements of ERAS [25].
Oblique subcostal TAPB has been shown to relieve pain after abdominal surgery, mainly by the injection of local anesthetics into the plane between the internal oblique muscles and the transverse muscles of the abdomen [21]. However, TAPB can only act on the anterolateral abdominal wall of the anterior innervation of the spinal nerve to relieve somatic pain. A previous meta-analysis concluded that oblique subcostal TAPB could provide effective analgesia in the first 12 h after abdominal surgery [26].
We found that patients treated with ESPB had lower VAS scores during the first 24 postoperative hours. Also, patients in the ESPB group required lower opioid consumption, which indicated that ESPB was providing more effective postoperative analgesia than oblique subcostal TAPB. This might be related to the mechanism of ESPB, which works by injecting local anesthetics into the plane between the erector spinal muscle and the transverse process, which then spreads to the paraspinal space and block the dorsal and ventral branches of the spinal nerve [16, 27]. Further studies might focus on different methods for prolonging the duration of blocks, such as continuous block technique or the addition of auxiliaries to local anesthetics. Furthermore, oblique subcostal TAPB could be performed after general anesthesia in the supine position, while ESPB requires to be in lateral or prone positions. The impact of these procedures on operation room turnover and patients' comfort was not measured in our study.
ESPB is a relatively easy regional block to operate, and previous larger sample size studies demonstrated that ESPB is safe [28, 29]. There are only a few case reports of operation-related complications. Ueshima [30] described a 73-year-old woman that suffered pneumothorax following ESPB, and OSelvi et al. [31] reported motor weakness related to the ESPB in a young woman after Cesarean section. No block-related adverse events were recorded in our study. As a new regional block technique, however, further clinical evidence is essential to verify safety.
In this study, the occurrence of PONV was lower in the ESPB group than the TAPB group. This may be a benefit from the decreased use of opioids during the postoperative period. A recent large sample and high-quality randomized clinical trial reports showed that the incidence of PONV in patients without intervention with opioid-based patient-controlled intravenous analgesia after abdominal surgery was 44.3% [32]. A reduction in the occurrence of PONV contributes to postoperative recovery and is consistent with ERAS. However, it is important to note that the use of inhaled anesthetics, different types of surgery, and routine use of postoperative antiemetic agents may limit the value of the result.
Our study has some limitations. First, we did not perform sensory evaluations of both blocks but did not impact outcomes. Second, although sample size calculation was performed in our study, the number of included patients was small, which needs to be confirmed by further large sample size studies. Third, the current study lacks optimal concentrations and dosages for local anesthetic; future studies might focus on this.
Conclusions
This study suggests that ESPB is a more effective regional block technique for postoperative pain relief in elderly patients undergoing laparoscopic colorectal surgery than oblique subcostal TAPB.
References
Son IT, Kim JY, Kim MJ, et al. Clinical and oncologic outcomes of laparoscopic versus open surgery in elderly patients with colorectal cancer: a retrospective multicenter study. Int J Clin Oncol. 2021. https://doi.org/10.1007/s10147-021-02009-4.
Larsen MB, Bachmann HH, Søborg B, et al. Prevalence of self-reported abdominal symptoms among 50–74-years-old men and women eligible for colorectal cancer screening—a cross-sectional study. BMC Cancer. 2021;21(1):910.
Teo ZHT, Tey BLJ, Foo CW, Wong WY, Low JK. Intraoperative celiac plexus block with preperitoneal infusion reduces opioid usage in major hepato-pancreato-biliary surgery: a pilot study. Ann Surg. 2021;274(1):e97–9.
Wennberg P, Möller M, Herlitz J, Kenne Sarenmalm E. Fascia iliaca compartment block as a preoperative analgesic in elderly patients with hip fractures—effects on cognition. BMC Geriatr. 2019;19(1):252.
Wenk M, Frey S. Elderly hip fracture patients: surgical timing and factors to consider. Curr Opin Anaesthesiol. 2021;34(1):33–9.
Boselli E, Hopkins P, Lamperti M, et al. European Society of Anaesthesiology and Intensive Care Guidelines on peri-operative use of ultrasound for regional anaesthesia (PERSEUS regional anesthesia): peripheral nerves blocks and neuraxial anaesthesia. Eur J Anaesthesiol. 2021;38(3):219–50.
Gottschalk A, Freitag M, Tank S, et al. Quality of postoperative pain using an intraoperatively placed epidural catheter after major lumbar spinal surgery. Anesthesiology. 2004;101(1):175–80.
Pan ZY, Hu ZH, Zhang F, et al. The effect of transversus abdominis plane block on the chronic pain after colorectal surgery: a retrospective cohort study. BMC Anesthesiol. 2020;20(1):116.
Kikuchi S, Kuroda S, Nishizaki M, et al. Comparison of the effects of epidural analgesia and patient-controlled intravenous analgesia on postoperative pain relief and recovery after laparoscopic gastrectomy for gastric cancer. Surg Laparosc Endosc Percutaneous Tech. 2019;29(5):405–8.
Szmit M, Agrawal S, Goździk W, et al. Transcutaneous electrical acupoint stimulation reduces postoperative analgesic requirement in patients undergoing inguinal hernia repair: a randomized. Placebo-Controlled Study. J Clin Med. 2021;10:1.
Fidkowski CW, Choksi N, Alsaden MR. A randomized-controlled trial comparing liposomal bupivacaine, plain bupivacaine, and the mixture of liposomal bupivacaine and plain bupivacaine in transversus abdominus plane block for postoperative analgesia for open abdominal hysterectomies. Can J Anaesthesia. 2021;68(6):773–81.
Baeriswyl M, Kirkham KR, Kern C, Albrecht E. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg. 2015;121(6):1640–54.
Vindal A, Sarda H, Lal P. Laparoscopically guided transversus abdominis plane block offers better pain relief after laparoscopic cholecystectomy: results of a triple blind randomized controlled trial. Surg Endosc. 2021;35(4):1713–21.
Imani F, Rahimzadeh P, Faiz HR, Abdullahzadeh-Baghaei A. An evaluation of the adding magnesium sulfate to ropivacaine on ultrasound-guided transverse abdominis plane block after abdominal hysterectomy. Anesthesiol Pain Med. 2018;8(4):e74124.
Abdelhamid BM, Khaled D, Mansour MA, Hassan MM. Comparison between the ultrasound-guided erector spinae block and the subcostal approach to the transversus abdominis plane block in obese patients undergoing sleeve gastrectomy: a randomized controlled trial. Minerva Anestesiol. 2020;86(8):816–26.
Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–7.
Ciftci B, Ekinci M, Gölboyu BE, et al. High thoracic erector spinae plane block for arthroscopic shoulder surgery: a randomized prospective double-blind study. Pain Med (Malden, Mass). 2021;22(4):776–83.
Lennon MJ, Isaac S, Currigan D, et al. Erector spinae plane block combined with local infiltration analgesia for total hip arthroplasty: a randomized, placebo controlled, clinical trial. J Clin Anesthesia. 2021;69:110153.
Canıtez A, Kozanhan B, Aksoy N, Yildiz M, Tutar MS. Effect of erector spinae plane block on the postoperative quality of recovery after laparoscopic cholecystectomy a prospective double-blind study. Br J Anaesthesia. 2021;127(4):629–635. https://doi.org/10.1016/j.bja.2021.06.030.
Yildiz M, Kozanhan B, Iyisoy MS, et al. The effect of erector spinae plane block on postoperative analgesia and respiratory function in patients undergoing laparoscopic cholecystectomy: a double-blind randomized controlled trial. J Clin Anesthesia. 2021;74:110403.
Boules ML, Goda AS, Abdelhady MA, Abu-El-Nour-Abd-El-Azeem SA, Hamed MA. Comparison of analgesic effect between erector spinae plane block and transversus abdominis plane block after elective cesarean section: a prospective randomized single-blind controlled study. J Pain Res. 2020;13:1073–80.
Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. 2020;125(4):492–504.
Ross SB, Mangar D, Karlnoski R, et al. Laparo-endoscopic single-site (LESS) cholecystectomy with epidural vs. general anesthesia. Surg Endosc. 2013;27(5):1810–9.
Barazanchi AWH, MacFater WS, Rahiri JL, et al. Evidence-based management of pain after laparoscopic cholecystectomy: a PROSPECT review update. Br J Anaesth. 2018;121(4):787–803.
Sultan P, Sultan E, Carvalho B. Regional anaesthesia for labour, operative vaginal delivery and caesarean delivery: a narrative review. Anaesthesia. 2021;76(Suppl 1):136–47.
Mishriky BM, George RB, Habib AS. Transversus abdominis plane block for analgesia after Cesarean delivery: a systematic review and meta-analysis. Can J Anaesthesia. 2012;59(8):766–78.
Ueshima H, Otake H. Similarities between the retrolaminar and erector spinae plane blocks. Reg Anesth Pain Med. 2017;42(1):123–4.
Weng WT, Wang CJ, Li CY, Wen HW, Liu YC. Erector spinae plane block similar to paravertebral block for perioperative pain control in breast surgery: a meta-analysis study. Pain Phys. 2021;24(3):203–13.
Liu MJ, Zhou XY, Yao YB, et al. Postoperative analgesic efficacy of erector spinae plane block in patients undergoing lumbar spinal surgery: a systematic review and meta-analysis. Pain Ther. 2021;10(1):333–47.
Ueshima H. Pneumothorax after the erector spinae plane block. J Clin Anesth. 2018;48:12.
Selvi O, Tulgar S. Ultrasound-guided erector spinae plane block as a cause of unintended motor block. Rev Esp Anestesiol Reanim. 2018;65(10):589–92.
Turan A, Essber H, Saasouh W, et al. Effect of intravenous acetaminophen on postoperative hypoxemia after abdominal surgery: the FACTOR randomized clinical trial. JAMA. 2020;324(4):350–8.
Acknowledgements
We thank the participants of the study.
Funding
This study was supported by grants from Jiaxing Key Discipline of Medicine -Anesthesiology (2019-zc-06). The journal’s Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
Shen Qi-hong: conceptualization and methodology. Zhou Xu-yan and Shen Xu: data curation and formal analysis. Wang Rong: project administration and supervision. Chen Yan-jun and Liu Ke: software, writing – original draft, and writing– review and editing. All authors contributed to the article and approved the submitted version.
Disclosures
Shen Qi-hong, Zhou Xu-yan, Shen Xu, Chen Yan-jun, Liu Ke, and Wang Rong have nothing to disclose.
Compliance with Ethics Guidelines
This study was approved by the ethics committee of The First Hospita of Jiaxing (No. 1882, Zhonghuan South Road, Jiaxing, Zhejiang, 315800, China). The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. The trial was registered at www. chictr.org.cn (registration number:ChiCTR2000033236). All participants consented to participate in this study and signed informed consent forms.
Data Availability
The data sets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Qi-hong, S., Xu-yan, Z., Xu, S. et al. Comparison of Ultrasound-Guided Erector Spinae Plane Block and Oblique Subcostal Transverse Abdominis Plane Block for Postoperative Analgesia in Elderly Patients After Laparoscopic Colorectal Surgery: A Prospective Randomized Study. Pain Ther 10, 1709–1718 (2021). https://doi.org/10.1007/s40122-021-00329-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-021-00329-x