Abstract
Introduction
Limited data exist regarding real-world utilization of nirmatrelvir/ritonavir. We identified predictors of nirmatrelvir/ritonavir use among Veterans Affairs (VA) outpatients nationally.
Methods
We conducted a retrospective cohort study among outpatients with coronavirus disease 2019 (COVID-19) who were eligible to receive nirmatrelvir/ritonavir between January and December of 2022, to identify factors associated with nirmatrelvir/ritonavir use (i.e., demographics, medical history, prior medication and healthcare exposures, frailty, and other clinical characteristics) using multivariable logistic regression.
Results
We included 309,755 outpatients with COVID-19 who were eligible for nirmatrelvir/ritonavir, of whom 12.2% received nirmatrelvir/ritonavir. Nirmatrelvir/ritonavir uptake increased from 1.1% to 23.2% over the study period. Factors associated with nirmatrelvir/ritonavir receipt included receiving a COVID-19 booster vs. none (adjusted odds ratio [aOR] 2.19 [95% confidence interval [CI] 2.12–2.26]), age ≥ 50 vs. 18–49 years (aORs > 1.5 for all age groups ≥ 50 years), having HIV (aOR 1.36 [1.22–1.51]), being non-frail vs. severely frail (aOR 1.22 [1.13–1.33]), and having rheumatoid arthritis (aOR 1.12 [1.04–1.21). Those with concomitant use of potentially interacting antiarrhythmics (aOR 0.35 [0.28–0.45]), anticoagulants/antiplatelets (aOR 0.42 [0.40–0.45]), and/or psychiatric/sedatives (aOR 0.84 [0.81–0.87]) were less likely to receive nirmatrelvir/ritonavir.
Conclusions
Despite increases over time, overall utilization of nirmatrelvir/ritonavir was low. Predictors of nirmatrelvir/ritonavir utilization were consistent with known risk factors for progression to severe COVID-19, including older age and underlying medical conditions. Unvaccinated and undervaccinated patients and those receiving potentially interacting medications for cardiovascular or mental health conditions (antiarrhythmic, alpha-1 antagonist, anticoagulant/antiplatelet, sedative/hypnotic/psychiatric) were less likely to receive nirmatrelvir/ritonavir. Further education of prescribers and patients about nirmatrelvir/ritonavir treatment guidelines is needed to improve overall uptake and utilization in certain high-risk subpopulations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
COVID-19 remains a significant clinical burden, and we sought to better understand which patients have been treated with nirmatrelvir/ritonavir in the real-world clinical setting. |
We identified predictors of nirmatrelvir/ritonavir treatment in the national Veterans Affairs Healthcare System among patients eligible to receive nirmatrelvir/ritonavir. |
What was learned from the study? |
Our work is among the first to describe real-world utilization of nirmatrelvir/ritonavir in a large national cohort of more than 300,000 outpatients with COVID-19 and to identify predictors of outpatient treatment with this new oral antiviral. |
Despite uptake increasing from 1.1% to 23.2% during the study period, fewer than 15% of eligible patients overall, and fewer than one-in-four eligible patients by the end of the study period (December 2022) were treated with nirmatrelvir/ritonavir. |
Predictors of nirmatrelvir/ritonavir treatment included known risk factors for progression to severe disease (e.g., older age and underlying medical conditions), vaccination status (less likely in unvaccinated and undervaccinated patients), as well as other factors that have not been previously identified, including frailty, rheumatoid arthritis, and taking known potentially interacting medications for cardiovascular or mental health conditions (antiarrhythmic, alpha-1 antagonist, anticoagulant/antiplatelet, sedative/hypnotic/psychiatric). |
Further education of prescribers and patients about nirmatrelvir/ritonavir treatment guidelines is needed to improve overall uptake and utilization in certain high-risk subpopulations. |
Introduction
Despite global and federal public health emergencies due to coronavirus disease 2019 (COVID-19) ending in May 2023, COVID-19 is still associated with a significant clinical burden after more than 3 years [1, 2]. Therefore, the need for effective COVID-19 treatment options to reduce the risk of progression to serious disease, hospitalization, and death remains.
Many drugs have been tested as potential COVID-19 treatments options; however, many of these therapies have failed to demonstrate improved outcomes, have been associated with significant toxicity, or both [3, 4]. Nirmatrelvir/ritonavir is an oral antiviral drug that was recently approved for the prevention of hospitalization among patients with mild-to-moderate COVID-19 at risk for progression to severe disease [5,6,7,8]. Nirmatrelvir/ritonavir consists of two drugs: (1) nirmatrelvir, a protease inhibitor that blocks the activity of SARS-CoV-2-3CL protease (an enzyme necessary for viral replication); and (2) ritonavir, an HIV-1 protease inhibitor, that is co-administered with nirmatrelvir to enhance the pharmacokinetics of nirmatrelvir through cytochrome P450 3A4 inhibition [7].
On December 22, 2021, the US Food and Drug Administration (FDA) issued an emergency use authorization (EUA) of nirmatrelvir/ritonavir for the treatment of COVID-19 based on a randomized controlled trial showing an 88% reduction in hospitalization or death in non-hospitalized adults with laboratory-confirmed SARS-CoV-2 infection and at least one risk factor for progression to severe disease, when treatment was taken within 5 days of symptom onset [9]. On May 25, 2023, nirmatrelvir/ritonavir became the first oral antiviral approved by the US FDA for mild-to-moderate COVID-19 in adults at high risk of disease progression [10]. Large, national studies of real-world predictors of nirmatrelvir/ritonavir utilization are needed. We described use of nirmatrelvir/ritonavir in the national Veterans Affairs (VA) Healthcare System and identified independent predictors of nirmatrelvir/ritonavir receipt.
Methods
Data Sources
We performed a retrospective cohort study of existing clinical data in the national VA Healthcare System. The Veterans Health Administration (VHA) Corporate Data Warehouse was used for this study. This data source contains health information from electronic health records and other administrative systems. We collected data from the following databases: demographics, inpatient admissions and outpatient visits, inpatient and outpatient pharmacy data (including barcode administration data, pharmacy dispensing data, and non-VA medications), inpatient and outpatient diagnoses (International Statistical Classification of Diseases, Tenth Revision, [ICD-10] Clinical Modification codes), laboratory and microbiology results, vital signs and vital status, and other health factors.
Study Population
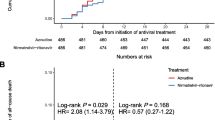
Our cohort included adults (≥ 18 years of age) who either tested positive for SARS-CoV-2 (including PCR or antigen tests) or had a COVID-19 diagnosis (ICD-10 code U07.1) in the outpatient setting (i.e., non-hospitalized) of the national VA Healthcare System between January 1 and December 31, 2022. We included only active VA users (i.e., at least one VA outpatient or inpatient visit in the previous 12 months). Further, patients had to be eligible for nirmatrelvir/ritonavir treatment on the basis of Centers for Disease Control and Prevention (CDC) criteria for high risk of progression to severe COVID-19 and NIH guidelines for drug interactions [9, 11,12,13]. Specifically, we excluded patients who were (1) less than 50 years of age without a CDC high-risk condition, (2) had severe renal impairment (eGFR < 30 mL/min in the 180 days prior), and (3) were currently taking medications contraindicated with nirmatrelvir/ritonavir for which alternative COVID-19 therapy is recommended (details presented in the footnote of Fig. 1) [11]. For patients meeting selection criteria multiple times over the study period, only the first episode was included. The index date was defined as the date of first positive SARS-CoV-2 test date or COVID-19 diagnosis (if no positive SARS-CoV-2 test was recorded).
Flowchart for study population. *High-risk patients include those that are at higher risk for progression to severe COVID-19, as defined by age 50 years or older or presence of at least one underlying medical condition or risk factor including asthma, cancer, cardiomyopathies, cerebrovascular disease, chronic heart failure, chronic kidney disease, chronic liver disease, chronic lung disease, coronary artery disease, current or former smoker, cystic fibrosis, delirium, dementia, and other cognitive disorders, diabetes mellitus type 1 or 2, human immunodeficiency virus, immunocompromised, mental health conditions, obesity, pregnancy, and tuberculosis. **Drugs contraindicated with nirmatrelvir/ritonavir included drugs that require the use of an alternative COVID-19 therapy, including albuvirtide, amiodarone, apalutamide, avapritinib, bepridil, bexarotene, bosentan, carbamazepine, cenobamate, cisapride, clopidogrel, clozapine, dabrafenib, dasatinib, dextropropoxyphene, dihydroergotamine, disopyramide, dofetilide, dronedarone, enasidenib, enzalutamide, eplerenone, ergometrine (ergonovine), ergotamine, flecainide, glecaprevir/pibrentasvir, halofantrine, ibrutinib, infigratinib, ivabradine, ivacaftor/lumacaftor, ivosidenib, lorlatinib, lurasidone, mefloquine, methylergometrine (methylergonovine), midazolam (oral), mitotane, nilotinib, pexidartinib, phenobarbital (phenobarbitone), phenytoin, pimozide, primidone, propafenone, quinidine, reboxetine, rifampicin, rifapentine, sonidegib, sotorasib, St John’s wort, tepotinib, tolvaptan, toremifene, tranylcypromine, umbralisib, vardenafil, venetoclax, and voclosporin. Contraindicated drug exposures include those with any days supply during the 90 days prior to the index date
Variables
We assessed patient demographics, socioeconomic status, medical history in the year prior, prior healthcare and medication exposures, overweight and obese status, immunocompromised status, frailty, and COVID-19 vaccination status as potential predictors. Socioeconomic status was assessed using the area deprivation index (ADI) grouped into quintiles from least to most deprived [14]. We assessed drugs with clinically significant potential for drug–drug interaction with nirmatrelvir/ritonavir (with recommendations to adjust concomitant medication and monitor, or to temporarily withhold concomitant medication, if clinically appropriate) [12, 13]. Overweight and obesity status were defined using CDC body mass index (BMI) categories for adults [15]. Immunocompromised status was based on a previously described algorithm [16]. Frailty was defined using the ICD-10 updated Veterans Affairs Frailty Index (VA-FI) [17]. COVID-19 vaccination status was based on recommendations for immunocompetent patients.
Statistical Analyses
We compared patients who were treated with nirmatrelvir/ritonavir to those who were not. Potential predictors were identified a priori and included previously described risk factors for progression to severe COVID-19, factors previously identified to be associated with COVID-19 treatment, and common, known potential drug–drug interactions with nirmatrelvir/ritonavir [11,12,13, 18, 19]. Adjusted odds ratios (aOR) and 95% confidence intervals (CI) were calculated to identify factors significantly associated with nirmatrelvir/ritonavir use (p value < 0.05). Collinearity in the final model was assessed using estimates of tolerance and variance inflation [20]. A sensitivity analysis was conducted that included only patients with a positive SARS-CoV-2 test. Analyses were conducted using SAS (Version 9.2, SAS Institute Inc., Cary, NC). We assessed time trends with Joinpoint regression to calculate average monthly percent changes (AAPC) and 95% CIs.
Ethical Approval
This study was determined to be exempt by the VA Providence Healthcare System (VAPHS). Institutional Review Board (IRB) and approved by the VAPHS Research and Development Committee. As this was a retrospective study of existing health records and exempt from IRB review, informed consent requirements are not applicable.
Results
After selection criteria were applied, 309,755 VA outpatients with a SARS-CoV-2 positive laboratory test or COVID-19 diagnosis were included between January 1 and December 31, 2022 (Fig. 1). Supplemental Table 1 describes demographic and clinical characteristics of patients treated with nirmatrelvir/ritonavir who were excluded from analyses. Overall, nirmatrelvir/ritonavir was used in 12.2% (n = 37,767) of eligible patients, and utilization increased 28.9% (95% CI 19.0–39.7%) per month over the study period (Supplemental Fig. 1) from 1.1% in January to 23.2% in December. Laboratory confirmation of SARS-CoV-2 infection occurred in 67.7% (n = 209,539) of all included patients with COVID-19 and in 60.9% (n = 22,983) of those treated with nirmatrelvir/ritonavir.
Table 1 describes demographics and clinical characteristics of outpatients by nirmatrelvir/ritonavir treatment status. Nirmatrelvir/ritonavir treated patients were older (mean age 63.7 vs. 59.7 years, p < 0.001) and more likely to be White (70.0% vs. 66.3%, p < 0.001) compared to those not treated with nirmatrelvir/ritonavir. Treated patients were more likely to have received a COVID-19 booster vaccination (58.9% vs. 39.2%, p < 0.001) compared to untreated. Nirmatrelvir/ritonavir treated patients were more likely to have a medical history of hypertension (56.7% vs. 49.6%, p < 0.001), diabetes (40.2% vs. 34.8%, p < 0.001), and cancer (37.5% vs. 30.4%, p < 0.001), and more likely to have concomitant use of potentially interacting HMG-CoA reductase inhibitors (44.4% vs. 36.5%, p < 0.001) compared to those not treated with nirmatrelvir/ritonavir.
Table 2 describes independent factors associated with the use of nirmatrelvir/ritonavir from multivariable models which included receiving a COVID-19 booster vs. none (aOR 2.19 [95% CI 2.12–2.26]), age ≥ 50 vs. 18–49 years (aOR 1.67 [95% CI 1.56–1.79] for ≥ 85 years; aOR 1.68 [95% CI 1.60–1.75] for 75–84 years; aOR 1.55 [95% CI 1.49–1.61] for 65–74 years; aOR 1.32 [95% CI 1.28–1.37] for 50–64 years), HIV (aOR 1.36 [95% CI 1.22–1.51]), VA Frailty Index (non-frail vs. frail, aOR 1.22 [95% CI 1.13–1.33]), rheumatoid arthritis (aOR 1.12 [95% CI 1.04–1.21]), and concomitant use of interacting medications from the following classes: antiarrhythmics (aOR 0.35 [95% CI 0.28–0.45]), anticoagulants/antiplatelets (aOR 0.42 [95% CI 0.40–0.45]), and sedative/psychiatric medications (aOR 0.84 [95% CI 0.81–0.87]). Results were similar when analyses were restricted to those with a positive SARS-CoV-2 test (Supplemental Table 2).
Discussion
Our study is among the first to describe real-world utilization of nirmatrelvir/ritonavir in a large national cohort of outpatients with COVID-19 and to identify predictors of outpatient treatment with this oral antiviral. Despite nirmatrelvir/ritonavir uptake increasing over the study period, it was concerning that fewer than 15% of eligible patients overall, and fewer than 25% of eligible patients by the end of the study period (December 2022) received nirmatrelvir/ritonavir. While several of the predictors of nirmatrelvir/ritonavir receipt that we identified are consistent with known risk factors for progression to severe disease (e.g., older age and underlying medical conditions), we also identified other factors associated with nirmatrelvir/ritonavir receipt that have not been previously identified, including frailty status, having rheumatoid arthritis, and currently taking known potentially interacting medications for cardiovascular or mental health conditions, including antiarrhythmic, alpha-1 antagonist, anticoagulant/antiplatelet, and sedative/hypnotic/psychiatric medications.
Though nirmatrelvir/ritonavir utilization was low in our study, similarly low rates have been observed in other health systems. Overall, only 12% of patients with COVID-19 were treated with nirmatrelvir/ritonavir between January and July 2022 in an analysis of electronic health records from 30 US sites participating in the National Patient-Centered Clinical Research Network (PCORnet) [21]. Another analysis of several large US health systems reported overall uptake of nirmatrelvir/ritonavir of 28% among treatment-eligible adults with an outpatient COVID-19 diagnosis between April and August 2022 [22], which was higher than the 18% identified in our population during the same time frame (April–August). Differences in nirmatrelvir/ritonavir uptake across studies are likely explained by differences in study populations. For example, Veterans have high rates of underlying comorbid illness and thus may have disproportionate use of potentially interacting medications, which could explain lower overall uptake compared to the general population [23, 24]. This topic, however, requires further study. Regardless, all three studies suggest that fewer than one in three patients with COVID-19 who are treatment-eligible actually receive nirmatrelvir/ritonavir [22].
Our results showing that older age and underlying comorbid illness predict nirmatrelvir/ritonavir prescribing suggest that many prescribers are aware of key risk factors for progression to severe COVID-19 and are prescribing nirmatrelvir/ritonavir to these patients [11]. Age is the strongest risk factor for progression to severe COVID-19 [11]. Further, other factors related to nirmatrelvir/ritonavir treatment that we identified, like HIV, asthma, active cancer, diabetes mellitus, and obesity, are all underlying medical conditions that are categorized by the CDC as conclusive higher-risk conditions associated with progression to severe COVID-19 [11]. However, overall nirmatrelvir/ritonavir uptake among eligible patients was still low, which may suggest that not all physicians are aware of nirmatrelvir/ritonavir availability or that risk-appropriate patients are not always identified.
Hypertension, which is categorized by the CDC as having mixed evidence regarding progression to severe COVID-19, was also identified as a predictor of nirmatrelvir/ritonavir utilization in our study [11]. While rheumatoid arthritis is not included on the CDC’s list of medical conditions associated with higher risk for severe COVID-19, interstitial lung disease is, which is the most common pulmonary manifestation of rheumatoid arthritis [11, 25]. Moreover, patients with rheumatoid arthritis may be receiving immunosuppressive drugs that would make them eligible for nirmatrelvir/ritonavir treatment. A previous retrospective, comparative, multicenter cohort study at two large US healthcare systems found that patients with rheumatoid arthritis or rheumatoid arthritis-associated interstitial lung disease had 1.8 and 2.5 times higher risk for severe COVID-19 compared to patients without these conditions, respectively [26].
Our work did identify several patient populations that were less likely to be treated with nirmatrelvir/ritonavir despite these populations being at high risk for progression to severe illness, including the unvaccinated and patients who were not up-to-date with current COVID-19 vaccine recommendations [27]. Public health efforts to encourage COVID-19 vaccination among these populations are warranted, and these high-risk patients should be encouraged to seek medical care if they test positive for SARS-CoV-2. Furthermore, it is possible that vaccine avoiders similarly dismiss nirmatrelvir/ritonavir treatment for COVID-19 when offered. Our analysis was restricted to individuals who tested positive for SARS-CoV-2, and therefore sought care for COVID-19 in the healthcare setting. However, we were not able to determine which patients were offered nirmatrelvir/ritonavir but refused treatment, and this remains an important area of future study.
Additionally, concomitant use of known potentially interacting antiarrhythmics, anticoagulants, and sedative/psychiatric medications were all associated with lower use of nirmatrelvir/ritonavir treatment despite these drugs often being used in patients that are at high risk of severe COVID-19. Thus, prescriber and patient education efforts should include current COVID-19 treatment guidelines to ensure effective treatments are being considered in all high-risk patients, that risk–benefit of nirmatrelvir/ritonavir treatment is discussed with patients, and that providers know how to effectively manage concomitant use of drugs with known potential interactions [13]. For example, in a survey of providers conducted from November to December 2022, nearly 30% reported they did not prescribe nirmatrelvir/ritonavir to a patient 65 and older because the patient was taking a medication that could potentially interact with nirmatrelvir/ritonavir and management for this potential interaction was unclear. Thus, provider education on management of potential drug–drug interactions likely remains an important area for future improvement to help ensure appropriate nirmatrelvir/ritonavir use among eligible patients [28]. Though the effectiveness of patient and provider education to improve medication use has been effective in other therapeutic areas, patient and provider education of COVID-19 treatment remains an important area for future study [29, 30].
Interestingly, HMG-CoA reductase inhibitor use was predictive of nirmatrelvir/ritonavir treatment despite known potential drug interactions of this drug class and corresponding recommendations to temporarily discontinue their use, before, during, or after nirmatrelvir/ritonavir treatment [31]. In patients with cardiovascular conditions requiring HMG-CoA reductase inhibitor use, such as hypercholesterolemia or prevention of acute coronary syndromes, prescribers appear to be more willing to utilize nirmatrelvir/ritonavir, perhaps because holding these treatments for short periods may have less clinical impact than holding other cardiac medications.
We also found that non-frail patients were more likely to receive nirmatrelvir/ritonavir compared to frail patients. Several recent studies have demonstrated that frailty is associated with adverse outcomes in patients with COVID-19 [32] and therefore prompt treatment in this population is important. It is possible that our findings may relate to higher acute care hospitalization rates among frail patients and thus less outpatient opportunity to prescribe nirmatrelvir/ritonavir. Alternatively, our results may also be related to non-frail patients being more likely to advocate for themselves and seek out nirmatrelvir/ritonavir treatment as compared to patients with higher frailty. Indeed, recent reports have shown that nirmatrelvir/ritonavir use in the nursing home setting (where frail patients are often concentrated) has been suboptimal [33]. Interventions to improve nirmatrelvir/ritonavir use among the frail are warranted; however, more research is needed.
We also saw racial and ethnic disparities in nirmatrelvir/ritonavir prescribing despite the equal access nature of the VA Healthcare System. Our results are consistent with prior research identifying racial and ethnic disparities in treatment with nirmatrelvir/ritonavir, molnupiravir, remdesivir, or monoclonal antibodies, which demonstrated that among 692,570 adult patients with COVID-19 (≥ 20 years of age), Black patients were 36% less likely and patients of other non-White races were 19–25% less likely to be given nirmatrelvir/ritonavir compared to White patients, when prescribing was highest (between April and July of 2022) [21]. Further, this study found that Hispanic patients received nirmatrelvir/ritonavir 30% less often than non-Hispanics [21]. In our study, patients from the least socioeconomically disadvantaged areas were more likely to receive nirmatrelvir/ritonavir as compared to patients from the most disadvantaged areas and the Southern region of the USA. These findings are concerning as patients from traditionally marginalized racial, ethnic, and socioeconomic groups have been disproportionally impacted by the COVID-19 pandemic with regards to COVID-19 illnesses, hospitalizations, and deaths [34,35,36,37]. Efforts are warranted to reduce racial, ethnic, and socioeconomic disparities in nirmatrelvir/ritonavir treatment, including measures to ensure healthcare access in socioeconomically disadvantaged areas (e.g., virtual care or pharmacy-based clinics).
Results of subgroup analyses in patients with laboratory confirmed COVID-19 were similar to overall results. Interestingly, from our subgroup analyses, we found that only 68% patients in our cohort had a COVID-19 positive laboratory test result in their VA record. As home testing for COVID-19 is becoming more common (including for obtaining treatment), it will become increasingly important for health systems to document COVID-19 diagnoses and for real-world studies to include the COVID-19 diagnosis code to identify these patients [38].
There are limitations to this work. We defined COVID-19 on the basis of a SARS-CoV-2 positive laboratory test or COVID-19 diagnosis in the VA Healthcare System. Thus, it is possible that some patients diagnosed with COVID-19 did not have laboratory-confirmed illness. However, we found similar results when we restricted analyses to those only with laboratory-confirmed COVID-19. Another limitation is that we only captured care that was recorded within the VA Healthcare System and may have missed patients who were tested for or diagnosed with COVID-19 outside the VA. We mitigated this by including only active VA users, who are more likely to use the VA for care. Another limitation is that symptom onset is not systematically captured in large electronic databases and, as such, we were unable to measure the amount of time from symptom onset to nirmatrelvir/ritonavir treatment. Further, we assumed that patients who were dispensed nirmatrelvir/ritonavir took their medication as prescribed, and we did not assess medication compliance or early discontinuation. Further, we did not determine vaccine history based on immunocompromised status, which could lead to misclassification in some instances. For example, immunocompromised patients were considered “boosted” if they received more than two doses, despite a recommendation for a three-dose primary series in this population. It should also be noted that there may be other unknown predictors that were not included in our study or known predictors that we could not capture from our data source. Additionally, we could not confirm the underlying reasons for why certain patient groups were more or less likely to receive nirmatrelvir/ritonavir, which would require future in depth qualitative interviews with providers and patients. Finally, the generalizability of this work may be limited, as the Veteran population consists primarily of older, White men.
Conclusions
Despite increases in use over time, real-world nirmatrelvir/ritonavir utilization was low (< 25% even at its highest point) among eligible patients with COVID-19 in the VA. We identified several predictors of nirmatrelvir/ritonavir receipt that are consistent with known risk factors for progression to severe disease, including older age and presence of certain underlying medical conditions. We also identified several high-risk patient groups that were less likely to receive nirmatrelvir/ritonavir treatment, even though nirmatrelvir/ritonavir would have been an effective COVID-19 treatment for these patients, including unvaccinated and undervaccinated patients, those with high frailty, and those from traditionally underserved racial, ethnic, and socioeconomic groups. Additionally, those receiving medications for cardiovascular or mental health conditions, including antiarrhythmic, alpha-1 antagonist, anticoagulant/antiplatelet, and sedative/hypnotic/psychiatric medications, that could potentially interact with ritonavir were less likely to receive treatment, possibly because of fear of a significant drug–drug interaction. Efforts should be made to increase patient and prescriber awareness about recommendations for use of effective and safe COVID-19 treatments in patients with risk factors for severe illness, and to determine whether such interventions are effective in increasing utilization of COVID-19 treatment.
Data Availability
The study data may be made available upon reasonable request and approval by the Department of Veterans Affairs.
References
Centers for Disease Control and Prevention (CDC). End of the federal COVID-19 public health emergency (PHE) declaration. https://www.cdc.gov/coronavirus/2019-ncov/your-health/end-of-phe.html. Published May 5, 2023. Accessed 16 May 2023.
World Health Organization (WHO). Coronavirus disease (COVID-19) pandemic. https://www.who.int/europe/emergencies/situations/covid-19. Published 2023. Accessed 16 May 2023.
Alagheband Bahrami A, Azargoonjahromi A, Sadraei S, Aarabi A, Payandeh Z, Rajabibazl M. An overview of current drugs and prophylactic vaccines for coronavirus disease 2019 (COVID-19). Cell Mol Biol Lett. 2022;27(1):38.
Bartoli A, Gabrielli F, Alicandro T, Nascimbeni F, Andreone P. COVID-19 treatment options: a difficult journey between failed attempts and experimental drugs. Intern Emerg Med. 2021;16(2):281–308.
Hammond J, Leister-Tebbe H, Gardner A, et al. Oral nirmatrelvir for high-risk, nonhospitalized adults with Covid-19. N Engl J Med. 2022;386(15):1397–408.
Pfizer. Pfizer announces additional phase 2/3 study results confirming robust efficacy of novel COVID-19 oral antiviral treatment candidate in reducing risk of hospitalization or death. https://www.pfizer.com/news/press-release/press-release-detail/pfizer-announces-additional-phase-23-study-results. Published December 14, 2021. Accessed 1 August 2022.
Najjar-Debbiny R, Gronich N, Weber G, et al. Effectiveness of Paxlovid in reducing severe COVID-19 and mortality in high risk patients. Clin Infect Dis. 2023;76(3):e342–e349.
Pitre T, Van Alstine R, Chick G, et al. Antiviral drug treatment for nonsevere COVID-19: a systematic review and network meta-analysis. CMAJ. 2022;194(28):E969–80.
Pfizer. Emergency use authorization (EUA) of Paxlovid for coronavirus disease 2019 (COVID-19). https://www.fda.gov/media/155051/download. Published June 28, 2022. Accessed 1 Aug 2022.
Food and Drug Administration. FDA approves first oral antiviral for treatment of COVID-19 in adults. https://www.fda.gov/news-events/press-announcements/fda-approves-first-oral-antiviral-treatment-covid-19-adults#:~:text=Today%2C%20the%20U.S.%20Food%20and,19%2C%20including%20hospitalization%20or%20death. Published May 25, 2023. Accessed 1 June 2023.
Centers for Disease Control and Prevention (CDC). Underlying medical conditions associated with higher risk for severe COVID-19: information for healthcare professionals. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html. Published June 15, 2022. Accessed 1 Aug 2022.
University of Liverpool. COVID-19 drug interactions checker. https://www.covid19-druginteractions.org/checker. Published 2023. Accessed 13 Apr 2023.
National Institutes of Health (NIH). COVID-19 treatment guidelines. Drug–drug interactions between ritonavir-boosted nirmatrelvir (Paxlovid) and concomitant medications. https://www.covid19treatmentguidelines.nih.gov/therapies/antivirals-including-antibody-products/ritonavir-boosted-nirmatrelvir--paxlovid-/paxlovid-drug-drug-interactions/. Published March 6, 2023. Accessed 13 Apr 2023.
Kitchen C, Hatef E, Chang HY, Weiner JP, Kharrazi H. Assessing the association between area deprivation index on COVID-19 prevalence: a contrast between rural and urban U.S. jurisdictions. AIMS Public Health. 2021;8(3):519–30.
Centers for Disease Control and Prevention (CDC). Defining adult overweight & obesity. https://www.cdc.gov/obesity/basics/adult-defining.html. Published June 3, 2022. Accessed 13 Apr 2023.
Tartof SY, Slezak JM, Puzniak L, et al. Effectiveness of a third dose of BNT162b2 mRNA COVID-19 vaccine in a large US health system: a retrospective cohort study. Lancet Reg Health Am. 2022;9: 100198.
Cheng D, DuMontier C, Yildirim C, et al. Updating and validating the U.S. veterans affairs frailty index: transitioning from ICD-9 to ICD-10. J Gerontol A Biol Sci Med Sci. 2021;76(7):1318–25.
Fernandes AL, Pereira RMR. Frailty in the context of COVID-19 pandemic: a life-threatening condition. Front Med (Lausanne). 2022;9: 965562.
Magesh S, John D, Li WT, et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis. JAMA Netw Open. 2021;4(11):e2134147.
Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. New York: Wiley; 2000.
Boehmer TK, Koumans EH, Skillen EL, et al. Racial and ethnic disparities in outpatient treatment of COVID-19—United States, January-July 2022. MMWR Morb Mortal Wkly Rep. 2022;71(43):1359–65.
Shah MM, Joyce B, Plumb ID, et al. Paxlovid associated with decreased hospitalization rate among adults with COVID-19—United States, April-September 2022. MMWR Morb Mortal Wkly Rep. 2022;71(48):1531–7.
Washington DL, editor. National Veteran Health Equity Report 2021. Focus on Veterans Health Administration patient experience and health care quality. Washington, DC: VHA Office of Health Equity; September 2022.
Betancourt JA, Granados PS, Pacheco GJ, et al. Exploring health outcomes for U.S. veterans compared to non-veterans from 2003 to 2019. Healthcare (Basel). 2021;9(5):604.
Kim EJ, Collard HR, King TE. Rheumatoid arthritis-associated interstitial lung disease: the relevance of histopathologic and radiographic pattern. Chest. 2009;136(5):1397–405.
Figueroa-Parra G, Gilbert EL, Valenzuela-Almada MO, et al. Risk of severe COVID-19 outcomes associated with rheumatoid arthritis and phenotypic subgroups: a retrospective, comparative, multicentre cohort study. Lancet Rheumatol. 2022;4(11):e765–74.
Centers for Disease Control and Prevention (CDC). Interim clinical considerations for COVID-19 treatment in outpatients. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/outpatient-treatment-overview.html#:~:text=Risk%20Factors%20for%20Severe%20COVID%2D19,-Clinicians%20can%20use&text=Age%20is%20the%20most%20important,date%20on%20COVID%2D19%20vaccinations. Published February 10, 2023. Accessed 1 May 2023.
Medscape. Medscape survey finds reasons Paxlovid is underprescribed for those 65nd older, despite its effectiveness again COVID complications. https://www.prnewswire.com/news-releases/medscape-survey-finds-reasons-paxlovid-is-underprescribed-for-those-65-and-older-despite-its-effectiveness-against-covid-complications-301720681.html. Published January 13, 2023. Accessed 19 Nov 2023.
Roumie CL, Elasy TA, Greevy R, et al. Improving blood pressure control through provider education, provider alerts, and patient education: a cluster randomized trial. Ann Intern Med. 2006;145(3):165–75.
Conn VS, Ruppar TM, Enriquez M, Cooper PS, Chan KC. Healthcare provider targeted interventions to improve medication adherence: systematic review and meta-analysis. Int J Clin Pract. 2015;69(8):889–99.
Food and Drug Administration. Paxlovid patient eligibility screening checklist tool for prescribers. https://www.fda.gov/media/158165/download. Accessed 1 May 2023.
Lee C, Frishman WH. Implications of frailty in COVID-19. Cardiol Rev. 2021;29(6):285–8.
McGarry BE, Sommers BD, Wilcock AD, Grabowski DC, Barnett ML. Monoclonal antibody and oral antiviral treatment of SARS-CoV-2 infection in US nursing homes. JAMA. 2023;330(6):561–3.
Ko JY, Danielson ML, Town M, et al. Risk factors for coronavirus disease 2019 (COVID-19)-associated hospitalization: COVID-19-associated hospitalization surveillance network and behavioral risk factor surveillance system. Clin Infect Dis. 2021;72(11):e695–703.
Wortham JM, Lee JT, Althomsons S, et al. Characteristics of persons who died with COVID-19—United States, February 12-May 18, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(28):923–9.
Yang X, Zhang J, Chen S, et al. Demographic disparities in clinical outcomes of COVID-19: data from a statewide cohort in South Carolina. Open Forum Infect Dis. 2021;8(9):ofab428.
McLaughlin JM, Khan F, Pugh S, et al. County-level predictors of coronavirus disease 2019 (COVID-19) cases and deaths in the United States: what happened, and where do we go from here? Clin Infect Dis. 2021;73(7):e1814–21.
Park S, Marcus GM, Olgin JE, et al. Unreported SARS-CoV-2 home testing and test positivity. JAMA Netw Open. 2023;6(1):e2252684.
Acknowledgements
Views expressed are those of the authors and do not necessarily reflect the position or policy of the United States Department of Veterans Affairs. This material is based upon work supported, in part, by the Office of Research and Development, Department of Veterans Affairs. The research study would not have been possible without the health information from patients under the care of the Veterans Health Administration. We express our gratitude to the VA patients for their invaluable contributions to medical and scientific progress.
Funding
This study was conducted as a collaboration between the VA Providence Healthcare System and Pfizer. The VA Providence Healthcare System is the study sponsor. Pfizer provided funding to the VA Providence Healthcare System for data analysis and manuscript development. HJA, ARC, VVL and KLL are employees of the VA Providence Healthcare System. Pfizer also provided funding for the journal’s Rapid Service and Open Access Fees.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: Haley J. Appaneal, Kerry L. LaPlante, Catherine Martin, Laura Puzniak, Timothy L. Wiemken, Evan J. Zasowski, John M. McLaughlin, Aisling R. Caffrey. Data generation: Haley J. Appaneal, Vrishali V. Lopes. Analysis and/or interpretation of the data: Haley J. Appaneal, Kerry L. LaPlante, Vrishali V. Lopes, Laura Puzniak, Timothy L. Wiemken, Evan J. Zasowski, John M. McLaughlin, Aisling R. Caffrey. Preparation or critical revision of the manuscript: Haley J. Appaneal, Kerry L. LaPlante, Vrishali V. Lopes, Catherine Martin, Laura Puzniak, Timothy L. Wiemken, Evan J. Zasowski, John M. McLaughlin, Aisling R. Caffrey.
Corresponding author
Ethics declarations
Conflict of Interest
Haley J. Appaneal has received research funding from Pfizer. Aisling R. Caffrey has received research funding from AbbVie, Gilead, Merck, Pfizer, and Shionogi, and has been a speaker/advisor for Merck. No other conflicts to report. Kerry L. LaPlante has received research funding from Merck, AbbVie, and Pfizer and has been an advisor for Ferring Pharmaceuticals, AbbVie, and Seres Therapeutics. Catherine Martin, Laura Puzniak, Timothy L. Wiemken, Evan J. Zasowski, and John M. McLaughlin are employees and shareholders of Pfizer Inc.
Ethical Approval
This study was determined to be exempt by the VA Providence Healthcare System (VAPHS) Institutional Review Board (IRB) and approved by the VAPHS Research and Development Committee. As this was a retrospective study of existing health records and exempt from IRB review, informed consent requirements are not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Appaneal, H.J., LaPlante, K.L., Lopes, V.V. et al. Nirmatrelvir/Ritonavir Utilization for the Treatment of Non-hospitalized Adults with COVID-19 in the National Veterans Affairs (VA) Healthcare System. Infect Dis Ther 13, 155–172 (2024). https://doi.org/10.1007/s40121-023-00910-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00910-1