Abstract
Primary immune thrombocytopenia (ITP) is an acquired autoimmune disease with highly variable presentation, characteristics, and clinical course. Thrombocytopenia is a common complication of many viral infections, including SARS-CoV-2. In addition, both de novo ITP and exacerbation of ITP after vaccination against SARS-CoV-2 have been reported. Patients infected with SARS-CoV-2 develop a prothrombotic coagulopathy called COVID-19-associated coagulopathy (CAC). In addition, autoimmune hematological disorders secondary to SARS-CoV-2 infection, mainly ITP and autoimmune hemolytic anemia (AIHA), have been described. Furthermore, SARS-CoV-2 infection has been associated with exacerbation of autoimmune processes, including ITP. In fact, there is evidence of a high relapse rate in patients with preexisting ITP and COVID-19. As for vaccination against SARS-CoV-2, hematological adverse events (HAE) are practically anecdotal. The most common HAE is thrombocytopenia-associated thrombosis syndrome (TTS) linked to vectored virus vaccines. Other HAEs are very rare, but should be considered in patients with previous complement activation disease or autoimmunity. In patients with ITP who are vaccinated against SARS-CoV-2, the main complication is exacerbation of ITP and the bleeding that may result. In fact, this complication occurs in 12% of patients, with splenectomized and refractory patients with more than five lines of previous treatment and platelet counts below 50 × 109/L being the most vulnerable. We conclude that, in general, there is no greater risk of severe SARS-CoV-2 infection in ITP patients than in the general population. Furthermore, no changes are advised in patients with stable ITP, the use of immunosuppressants is discouraged unless there is no other therapeutic option, and patients with ITP are not contraindicated for vaccination against COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In general, there is no greater risk of severe SARS-CoV-2 infection in immune thrombocytopenia (ITP) patients than in the general population. |
No changes are suggested in the management of patients with stable ITP compared to what was advised before the SARS-CoV-2 pandemic. |
We suggest a platelet threshold of 30 × 109/L in adults with newly diagnosed ITP who are asymptomatic or have minor mucocutaneous bleeding to begin treatment with steroids. |
The use of immunosuppressants is discouraged unless there is no other therapeutic option. |
Patients with ITP are not contraindicated for vaccination against COVID-19. |
Introduction
Lymphopenia and thrombocytopenia [1, 2] are the two most frequent hematological alterations observed in coronavirus disease 2019 (COVID-19) patients. Thrombocytopenia occurs in up to 60% of patients with COVID-19 and responds to various pathophysiological mechanisms.
Thrombocytopenia, understood as a platelet count below 100 × 109/L, constitutes an adverse prognostic factor in this pathology [3]. Despite the development of thrombocytopenia, the decrease in platelet numbers does not seem to entail a higher bleeding risk in patients affected with COVID-19, except for counts of < 30 × 109/L that may compromise hemostasis [4].
Immune thrombocytopenia (ITP) is one of the mechanisms described as being responsible for the decrease in platelet counts in patients with COVID-19. Several causes for this phenomenon have been reported to date, with viral induction of autoimmunity being the most important mechanism described. Thus, molecular mimicry, expression of cryptic antigens, or the propagation of epitopes can explain this immune dysregulation. Most ITP cases develop within 2–3 weeks after COVID-19 infection [5]. This condition has also been described after vaccination against COVID-19, i.e., an elevated frequency of newly diagnosed ITP or exacerbation of previously diagnosed ITP cases was observed [6].
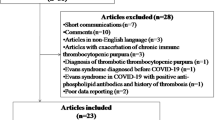
Regarding this topic, few publications have been published to date [7, 8], including two recent meta-analyses [5, 9] being the most important papers to report the current status of this treatment challenge. The first of them [5] analyzed 42 patients from 13 publications and provides epidemiology data about COVID-19 infection associated with immune thrombocytopenia. The latter [9] analyzed post-COVID-19 hematologic complications. Nevertheless, given the lack of major publications/clinical trials, we consider that expert consensus guidelines are needed to guide ITP management. Therefore, our guidelines will address the management of newly diagnosed ITP (ND-ITP) in adult COVID-19 patients and the hematological complications observed with COVID-19 vaccines. Furthermore, given that the management of ITP during the COVID-19 pandemic could vary from the usual approach, the therapy for patients with a previous diagnosis of ITP and subsequently infected with SARS-CoV2 will also be considered. The target population of these guidelines are adult ITP patients only, and the target audience is medical professionals. These consensus recommendations comply with ethical guidelines and are based on previously conducted studies and do not contain any new studies with human participants or animals performed by any of the authors.
Pathogenesis of Thrombocytopenia by COVID-19
The pathogenesis of immune thrombocytopenia secondary to COVID-19 is diverse and affects multiple levels of platelet physiology:
Involvement of Hematopoietic Progenitor Cells
SARS-CoV-2 invades hematopoietic tissues by binding to angiotensin-converting enzyme 2 (ACE2) present in these cells. In addition, through the CD13 and CD66 receptors that are expressed on the surface of megakaryocytes (MK), the virus is able to access the cell, replicating itself and causing apoptosis of these precursors. The immune system responds by generating antibodies against the infected cells, decreasing the platelet production [10].
Alterations in Thrombopoietin and Cytokines
Thrombopoietin (TPO) is synthesized in hepatocytes, which in turn have ACE2 receptors on their surface that allow their invasion and destruction by SARS-CoV-2. This translates into a lower synthesis of TPO than is necessary for the production of platelets. In this sense, the presence of proinflammatory cytokines [interleukin-1ß (IL-1ß) and tumor necrosis factor-alpha (TNFα)] caused by the infection, damage the medullary progenitor cells, negatively interfering with the differentiation and maturation of MK. Increased levels of transforming growth factor-β (TGF-ß) and interferon alpha (IFN-α) that inhibit MK maturation have also been described [11].
Lung Damage and Platelet Consumption
Megakaryocytes, together with other hematopoietic cells, are present in the lung tissue, so when the alveolus is invaded by SARS-CoV-2, it generates a decrease in the vascular bed, decreasing the production of platelets at this level. Concomitantly, vascular endothelial injury at the pulmonary level increases platelet activation and aggregation, leading to platelet consumption [12].
Other Causes
Thrombocytopenia caused by drugs, dilutions, heparin, or secondary to invasive procedures (hemodialysis, plasmapheresis, cardiorespiratory support, etc.) must be taken into account (Fig. 1).
Diagnosis of Thrombocytopenia Due to COVID-19
Any decrease in platelets below 100 × 109/L should be considered thrombocytopenia. Nonimmune thrombocytopenia associated with COVID-19 is usually mild or moderate, with platelet counts ≥ 50 × 109/L and with scarce hemorrhagic symptoms. When platelet numbers are below 20 × 109/L or, on the contrary, they decrease > 50% in 24–48 h, that should leads us to suspect an immune etiology, such as ITP, hereditary thrombotic thrombocytopenic purpura (TTP), or hemolytic uremic syndrome (HUS) (especially if microangiopathic hemolytic anemia is associated). Drug-induced thrombocytopenia appears between 5 and 15 days after exposure to drugs and it usually never reaches a nadir lower than 20–30 × 109/L platelets [13].
Mandatory tests for an accurate etiological study of thrombocytopenia in this context are:
-
1.
Complete blood count (immature platelet fraction or similar is recommended) with peripheral blood smear.
-
2.
Liver, kidney, thyroid function, proteinogram, and immunoglobulins.
-
3.
Ripening factors (vitamin B12, folic acid, and iron profile)
-
4.
Antinuclear (ANAs) and antiphospholipid antibodies. Lupus anticoagulant testing.
-
5.
Hepatitis C virus (HCV), Human immunodeficiency virus (HIV), Helicobacter pylori (according to geographic area). Chronic hepatitis B [to be considered as part of the initial workup for thrombocytopenia in certain parts of the world e.g., World Health Organization (WHO) western pacific and WHO African region where Hepatitis B is endemic].
In this sense, we consider it important to note that some tests, e.g., antithyroid autoimmunity, may play a role as a predictive biomarker of chronic immune thrombocytopenia [14], which supports their use to establish an accurate diagnosis.
The bone marrow study, as in classic ITP, must include aspiration or biopsy, immunophenotype, and cytogenetic study, being indicated in the following circumstances [15]:
-
Patients with suspicion of dysplasia in peripheral blood and aged over 60 years.
-
Patients who do not respond to first-line treatment or relapse after a complete remission.
-
Before a splenectomy is performed.
-
When any morphological alteration in peripheral blood indicative of possible underlying blood disease is observed.
However, it should be kept in mind that ITP remains a diagnosis of exclusion, with no confirmatory test for this entity. In this setting, the diagnosis of ITP secondary to SARS-CoV-2 infection will be given by the presence of thrombocytopenia in a patient with no prior history of low platelet counts who, in the context of a recent SARS-CoV-2 infection, develops a platelet count drop not attributable to any other cause.
Clinical Presentation
Several studies have reported the pejorative prognosis of the presence of thrombocytopenia in patients with moderate–severe disease due to SARS-CoV-2 [3], with, on the other hand, no correlation with an increased bleeding risk, especially if platelet counts are ≥ 30 × 109/L.
Thrombocytopenia has been described in both mild and moderate–severe COVID-19 patients at any time during the course of the disease. The symptoms of the immune thrombocytopenia secondary to COVID-19 do not differ from those reported in primary ITP, with mucocutaneous bleeding (epistaxis, ecchymosis) or bleeding from venipuncture sites in patients with counts < 20 × 109/L as most frequent episodes observed.
Cases without hemorrhagic symptoms have also been described, even with counts below 15–20 × 109/L. Severe bleeding or bleeding affecting a critical organ is not frequent and, if it does occur, it is usually favored by the concomitance of other predisposing factors present in the patient.
Treatment
The treatment of ITP secondary to COVID-19 disease is similar to that applied in patients with ITP outside this setting [16].
Corticosteroids (GCs)
There is currently no consensus to recommend a specific dose or duration of this therapy for COVID-19 patients.
The most recommended treatment schedule is to use steroids at currently approved doses for the treatment of classic ITP [17], unless the patient has to receive GCs for their underlying COVID disease.
In our patients with platelet counts below 30 × 109/L and/or active bleeding and COVID19 infection, we shall start prednisone at a dose of 0.5–1 mg/kg/day and keep it for a maximum of 2 weeks, withdrawing it shortly afterwards for a maximum of 8 weeks. We recommend dexamethasone use at standard ITP doses as an alternate steroid to be used in this scenario. We should also evaluate potential hospital admission in newly diagnosed patients.
If we are facing severe COVID-19 disease patients who were already receiving corticosteroids and presented platelet counts below 20 × 109/L and/or active bleeding, we must consider concomitant treatment with intravenous immunoglobulins (IVIG) at a dose of 2 g/kg (total dose). In the rest of the cases that have responded to corticosteroid therapy for the treatment of COVID-19, we subsequently begin a gradual decrease in corticosteroids until they are discontinued.
Intravenous Immunoglobulins (IVIG)
The use of IVIG will be conditioned by the severity of the thrombocytopenia, when a rapid increase in the number of platelets is required due to bleeding or the need to perform an invasive procedure. Its use is also postulated as a second-line treatment if there has been no response to corticosteroids [18].
The doses are the same as those used in patients with primary ITP, that is, a total dose of 2 g/kg that can be divided between two and five doses.
Thrombopoietic Agents (TPO-RAs)
The use of TPO-RAs in this COVID19 scenario has been controversial since the initiation of the pandemic due to the potential thrombotic risk of these drugs, to which is added the thromboembolic risk associated with SARS-CoV-2 infection itself. In addition to the above, in this type of patient there may be abnormalities in liver function tests that can make it difficult to monitor these agonists.
However, in different series of patients published in Spain, the UK, and Italy [19], no differences have been found in the evolution of patients treated with the two TPO-RAs, romiplostim (Nplate) and eltrombopag (Revolade) in patients with ITP and COVID.
Therefore, their use is recommended in the event of no response to GCs and IVIG, in patients with platelets less than 20 × 109/L and/or active bleeding. They shall be used at the lowest therapeutic dose with which a response is obtained. Close monitoring of the patient for platelet count and thrombotic risk is also required.
Rituximab, Splenectomy, and Other Immunosuppressants
The use of rituximab is not recommended, since it can decrease the formation of antibodies against SARS-CoV-2 virus. In this sense, the use of immunosuppressants is discouraged unless there is no adequate therapeutic option, although it should be assessed individually [20].
Splenectomy continues to be a therapeutic option in patients refractory to several lines of treatment especially once the SARS-CoV-2 infection has been overcome [21].
Platelet Transfusions
The need for platelet transfusion is unusual in patients with SARS-CoV-2, since they do not usually present severe thrombocytopenia at diagnosis and when they do, they usually have a predominance of the immune component. In addition, it cannot be forgotten that COVID19 disease generates a prothrombotic state that platelet transfusion could increase. For all of the above, platelet transfusion is only recommended in the presence of thrombocytopenia with active bleeding that translates into a life-threatening hemorrhage [22].
Thromboprophylaxis and Antithrombotic Therapy in Patients with Thrombocytopenia Due to SARS-CoV-2:
Thromboprophylaxis with low-molecular-weight heparin (LMWH) should be administered to patients with ITP and severe COVID-19 infection if the platelet count is higher than 30 × 109/L. In the case of needing anticoagulation or antiaggregation, they can receive full doses if platelet count is ≥ 50 × 109/L, always individualizing case by case.
Special Situations
ITP Due to COVID-19 in Pregnancy
In the event that a newly diagnosed ITP or an exacerbation of a preexisting ITP develops in a COVID-19-positive pregnant woman, and according to the clinical status and gestational age of the patient, we shall administer low doses of steroids (20–30 mg/day) and assess concomitant treatment with IVIG. If thromboprophylaxis is required, we recommend following the recommendations of the Spanish published guidelines in this regard (https://www.covid-19.seth.es/recomendaciones-sobre-profilaxis-de-enfermedad-tromboembolica-etv-en-el-embarazo-y-puerperio-dur-la-pandemia-covid-19/).
A constant multidisciplinary approach is recommended for pregnant women with ITP and infected with SARS-CoV-2, including the involvement of different specialists (hematologist, gynaecologist, infectious disease specialist, and, if necessary, intensive care unit colleagues) [23].
Complications in Patients with Previously Diagnosed Primary Immune Thrombocytopenia who Become Infected with SARS-CoV-2
Currently, there is limited data on the impact of SARS-CoV-2 infection in patients diagnosed with chronic primary immune thrombocytopenia. The COVID-19 pandemic has posed a challenge in the management of these patients because viral infections are a relevant factor in relapses of patients with ITP.
In patients with known ITP who become infected by SARS-CoV-2, they should maintain their background treatment, be it corticosteroids, immunosuppressants, or thrombopoietin analogs, with closer monitoring of platelet counts. In the case of thrombopoietin analogs, the lowest effective dose should be maintained for a hemostatic count, and the establishment of thromboprophylaxis measures should be assessed. In the case of splenectomized patients, no increased risk of viral infections has been demonstrated. On the contrary, the risk of bacterial infections increase and the vaccination schedule must be kept up to date and patients must be instructed to start antibiotic therapy early in the event of signs or symptoms of infection [23].
In patients with known prior ITP who experience a relapse in the context of SARS-CoV-2 infection, in light of the available data and recommendations from scientific societies, we recommend treatment with IVIG in case of severe thrombocytopenia and platelet transfusion only if mild/severe bleeding occurs. Patients previously treated with TPO-RAs can increase their previous dose or add a second analog or fostamatinib. If corticosteroids are used, low doses reduced over time are recommended [18].
The need for thromboprophylaxis measures should always be kept in mind with any of these patients. Thus, we advise to use low-molecular-weight heparins if platelet counts are higher than 25–30 × 109/L without hemorrhagic symptoms and especially if they require hospitalization. These recommendations are outlined in Fig. 2.
Thrombocytopenia Secondary to Vaccination for SARS-COV-2
Coronavirus disease 2019 caused by successive variants of the sarbecovirus SARS-CoV-2, was described in December 2019 in Wuhan, China.
Since the beginning of the pandemic, multiple strategies have been developed both to prevent infection and the development of disease and, in the event that it appears, to limit its severity. One of the most effective and efficient measures for the control of COVID-19 has been the use of vaccines. Although the vaccines used in the rest of the world (both currently and in development) are very diverse, only four have been used in Spain to date: two vaccines based on nonvectorized RNA and two that use adenovirus as a spike protein vector (S) [24, 25]. In December 2021, the use of a new vaccine (Novaxsovid), which contains spike protein and the Matrix M2 adjuvant, has been authorized (Table 1).
It has long been known that vaccines in general can cause secondary thrombocytopenia. It is estimated that approximately 1:40,000 children develop secondary immune thrombocytopenia after receiving different types of vaccine [26, 27].
Regarding the vaccines against SARS-CoV-2, in the publications of the clinical trials of the different vaccines thrombocytopenia was not described within the adverse effects [28,29,30,31]. Even in an Israeli observational study, according to data from ClalitHealthServices (CHS) in May 2021, vaccinated patients (n = 884,828) had fewer episodes of thrombocytopenia than the placebo arm (n = 884,828) [31].
Subsequently, in real life, cases of vaccine-induced immune thrombotic thrombocytopenia (VITT) were described associated with adenovirus vaccines and hemorrhages secondary to immune thrombocytopenia, more frequent with mRNA vaccines [32].
Post-vaccination thrombocytopenia is rare, but it can occur and is due to autoimmune phenomena, since the same mechanisms involved in the anti-infective immune response are involved in autoreactivity (Fig. 1) [33]. Both viruses and vaccines can trigger an autoimmune response, although the relative risk is ten times higher after natural infection than with the corresponding vaccine.
Being rare side effects, we can find three causes of post-vaccine thrombocytopenia:
-
1.
Primary immune thrombocytopenia (ITP)
-
2.
Vaccine-induced thrombotic thrombocytopenia (VITT)
-
3.
Acquired thrombotic thrombocytopenic purpura (ATP)
Primary Immune Thrombopenia:
From an epidemiological point of view, if we consult the registries of adverse effects of SARS-CoV-2 vaccines, from different public services (USA, France, UK, etc.), immune thrombocytopenia after vaccination had a lower incidence than expected for primary immune thrombocytopenia (ITP) for the same population range [26].
Immune thrombocytopenia secondary to vaccination is believed to be caused by the activation of antibodies and T cells responsible for the elimination of virus antigens, which can cross-react with antigens present on the platelet membrane. Antibody-coated platelets are cleared by tissue macrophages, resulting in a shorter platelet half life. In addition, these antibodies also inhibit platelet production [34].
The symptomatology is similar to ITP. The diagnosis is made as we would do it in ITP. In terms of treatment, it is similar, except that the use of anti-CD20 should be restricted because they can nullify the effect of the vaccine [25, 26, 35].
Vaccine-Induced Thrombotic Thrombocytopenia (VITT)
Faced with any post-vaccination thrombocytopenia, it will be necessary to be vigilant in case the condition is the beginning of a VITT. The incidence of VITT is 3.8 cases per million vaccinated with SARs-COV-2 adenovirus vaccines [34, 36]. VITT is an autoimmune disease, characterized by antibodies that directly activate platelets, triggering thrombosis in the arterial and venous circulation. The mechanism of VITT resembles that of heparin-induced thrombocytopenia (HIT), as both reflect the pathogenic role for platelet-activating antiplatelet factor 4 (PF4) antibodies. The causative anti-PF4/polyanion immunoglobulin G (IgG) antibody induces platelet activation and aggregation by cross-linking the Fcγ IIA receptor on platelets and leading to thrombosis.
Regarding VITT, thrombocytopenia and venous and/or arterial thrombosis occur, which may be in atypical locations, 5–30 days after the first vaccination against SARS-CoV-2 with AstraZeneca-Oxford or Johnson & Johnson. Elevated D-dimer is detected in blood and associated with positive anti-PF4 antibodies (Ab) detected by enzyme-linked immunosorbent assay (ELISA) [37, 38].
The therapeutic management of VITT is based on three components: modulation of the autoimmune phenomenon, anticoagulation and supportive care, and management of complications [37].
-
1.
Modulation of the autoimmune phenomenon: intravenous immunoglobulins (IVIGs) inhibit platelet activation mediated by VITT. The recommended dose of IVIG is 1 g/kg for 2 days. In case of severity or refractoriness to treatment, plasma exchange can be used. During plasma exchange, IgG antibodies that trigger VITT are removed. Associated corticosteroids have also been used.
-
2.
Anticoagulation: It is recommended not to use heparins. Fondaparinux, direct thrombin inhibitors (argotraban and bivalirudin), or direct-acting oral anticoagulants can be used.
-
3.
Supportive therapy and complications: If thrombocytopenia appears, anticoagulation should be adjusted or platelet transfusion is advised. We must assess fibrinogen levels. Monitor the patient to prevent respiratory and cardiac failure is also recommended.
-
4.
The second vaccine dose can be done with a mRNA vaccine [39].
Acquired Thrombotic Thrombocytopenic Purpura (aTTP)
As with other vaccines (H1N1, pneumococcus), both the “de novo” appearance and the relapse of cases of aTTP, although rare, have been described after the administration of vaccines against COVID-19, with the appearance of auto-antibodies against ADAMTS13 [40,41,42,43].
The mechanism could be the exacerbation of autoimmunity after vaccination with the creation of antibodies against ADAMTS13. Tso et al. hypothesized that vaccine-induced molecular mimicry and cross-reactivity in genetically susceptible hosts may be responsible for aTTP [44]. They demonstrated that in three patients with aTTP, they had significant levels of neutralizing IgG antibodies against the SARS-CoV-2 spike S1 protein after COVID-19 vaccinations. However, no cross-reactivity was demonstrated between their autoantibodies to ADAMTS-13 and the SARS-CoV-2 S1 spike protein binding from two different commercial suppliers. aTTP cases described have been specifically associated with the Pfizer-BioNtech vaccine. aTTP has been described as a complication in patients with COVID-19, where in addition to this mechanism there could be an excessive release of von Willebrand factor (vWF) from the vascular endothelium, which exceeds the cleavage capacity of ADAMTS13. The clinic and treatment (plasma exchange, corticosteroids, rituximab, caplacizumab) do not differ from other forms of aTTP. Rituximab can interfere with the immunization from the vaccine.
Summary of Recommendations/Conclusions/“Take Home Messages”
-
SARS-CoV-2 (COVID-19) infection can cause ITP debut-like other viral infections.
-
The diagnosis of ITP secondary to SARS-CoV-2 infection continues to be a diagnosis of exclusion in patients with active infection by this pathogen.
-
In general, first-line treatment initiation is not indicated in patients with stable platelet counts of around 20–30 × 109/L without active bleeding. We should individualize each case anyway.
-
In patients with platelet counts below 30 × 109/L and/or active bleeding, start prednisone at a dose of 0.5–1 mg/kg/day and keep it for a maximum of 2 weeks, withdrawing it shortly afterwards for a maximum of 8 weeks.
-
In patients with severe COVID disease who were already receiving corticosteroids and had platelet counts below 20 × 109/L and/or active bleeding, then consider associating treatment with intravenous immunoglobulins (IVIG) at a dose of 2 g/kg (total dose).
-
The use of thrombopoietic agents (AR-TPO) is recommended in the event of corticosteroid and immunoglobulin failure, in patients with platelets below 20 × 109/L and/or active bleeding, at the lowest possible therapeutic dose with which a response is obtained, and with close monitoring of the patient. In case of lack of response, toxicity, or high thrombotic risk, consider the use of fostamatinib.
-
The use of rituximab is not recommended for the treatment of ITP secondary to COVID, since it can decrease the formation of antibodies against SARS-CoV-2.
-
The use of other immunosuppressants is not recommended unless there is no adequate therapeutic option, although it should be assessed individually.
-
In patients with chronic ITP who receive treatment with corticosteroids, immunosuppressants or TPO-RAs with correct control of the platelet count and have COVID-19 infection, it is recommended to continue with the same treatment without making major changes in their dosage. Close clinical and platelet count monitoring is necessary.
-
In patients with chronic ITP who present a relapse secondary to infection by SARS-CoV-2, IVIG treatment is recommended in case of severe thrombocytopenia. Platelet transfusion should be used only if there is major bleeding. Patients previously treated with TPO-RAs can increase its dose or add a second analog or fostamatinib. In case of corticosteroid use, doses of 0.5–1 mg/kg/day and reduced over time are recommended.
-
In pregnant women with ITP secondary to COVID-19, the standard therapy is low-dose prednisone. This must be associated with immunoglobulins in cases of severity or high bleeding risk, and its use also depends on gestational age.
-
The risk of ITP secondary to vaccination against SARS-CoV-2 is low, similar to that of other vaccines against viral agents available on the market.
-
There is no contraindication for the COVID-19 vaccine in pregnant women or in patients with previous ITP.
-
Thromboprophylaxis with low-molecular-weight heparin should be administered even to patients with ITP and severe COVID-19 infection, if the platelet count is greater than 30 × 109/L. In the case of requiring anticoagulation or antiaggregation, they can be administered at full doses from 50 × 109 (Table 2).
References
Rahman A, Niloofa R, Jayarajah U, De Mel S, Abeysuriya V, Seneviratne SL. Hematological abnormalities in COVID-19: a narrative review. Am J Trop Med Hyg. 2021;104(4):1188–201.
Fan BE, Chong VCL, Chan SSW, Lim GH, Lim KGE, Tan GB, et al. Hematologic parameters in patients with COVID-19 infection. Am J Hematol. 2020;95(6):E131–4.
Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–8.
Zhang Y, Zeng X, Jiao Y, Li Z, Liu Q, Ye J, et al. Mechanisms involved in the development of thrombocytopenia in patients with COVID-19. Thromb Res. 2020;193:110–5.
Alharbi MG, Alanazi N, Yousef A, Alanazi N, Alotaibi B, Aljurf M, et al. COVID-19 associated with immune thrombocytopenia: a systematic review and meta-analysis. Expert Rev Hematol. 2022;15(2):157–66.
Chou SC, Chang YC, Liao CK, Chen TC, Sun KJ, Huang WH, et al. New presentations and exacerbations of immune thrombocytopenia after coronavirus disease 2019 vaccinations: the Taiwan experience. Platelets. 2022;33(4):531–5.
Al-Saadi EAKD, Abdulnabi MA. Hematological changes associated with COVID-19 infection. J Clin Lab Anal. 2022;36(1):e24064.
Mocan M, Chiorescu RM, Tirnovan A, Buksa BS, Farca AD. Severe thrombocytopenia as a manifestation of COVID-19 infection. J Clin Med. 2022;11(4):1088.
Alahyari S, Moradi M, Rajaeinejad M, Jalaeikhoo H. Post-COVID-19 hematologic complications: a systematic review. Expert Rev Hematol. 2022;15(6):539–46.
Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol. 2020;38(1):1–9.
Fu Y, Cheng Y, Wu Y. Understanding SARS-CoV-2-mediated inflammatory responses: from mechanisms to potential therapeutic tools. Virol Sin. 2020;35(3):266–71.
Xu P, Zhou Q, Xu J. Mechanism of thrombocytopenia in COVID-19 patients. Ann Hematol. 2020;99(6):1205–8.
Rahi MS, Jindal V, Reyes SP, Gunasekaran K, Gupta R, Jaiyesimi I. Hematologic disorders associated with COVID-19: a review. Ann Hematol. 2021;100(2):309–20.
Giordano P, Urbano F, Lassandro G, Bianchi FP, Tolva A, Saracco P, et al. Role of antithyroid autoimmunity as a predictive biomarker of chronic immune thrombocytopenia. Pediatr Blood Cancer. 2019;66(1): e27452.
Provan D, Arnold DM, Bussel JB, Chong BH, Cooper N, Gernsheimer T, et al. Updated international consensus report on the investigation and management of primary immune thrombocytopenia. Blood Adv. 2019;3(22):3780–817.
Neunert C, Terrell DR, Arnold DM, Buchanan G, Cines DB, Cooper N, et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv. 2019;3(23):3829–66.
Choi PY, Merriman E, Bennett A, Enjeti AK, Tan CW, Goncalves I, et al. Consensus guidelines for the management of adult immune thrombocytopenia in Australia and New Zealand. Med J Aust. 2022;216(1):43–52.
Mingot-Castellano ME, Alcalde-Mellado P, Pascual-Izquierdo C, Perez Rus G, Calo Pérez A, Martinez MP, et al. Incidence, characteristics and clinical profile of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection in patients with pre-existing primary immune thrombocytopenia (ITP) in Spain. Br J Haematol. 2021;194(3):537–41.
Lapietra G, Ferretti A, Baldacci E, Chistolini A, Santoro C. Immune thrombocytopenia management during COVID-19 pandemic: an Italian monocentric experience. EJHaem. 2022;3(2):453–6.
Bahadoram M, Saeedi-Boroujeni A, Mahmoudian-Sani MR, Hussaini H, Hassanzadeh S. COVID-19-induced immune thrombocytopenic purpura Immunopathogenesis and clinical implications. Infez Med. 2022;30(1):41–50.
Nazi I, Kelton JG, Larché M, Snider DP, Heddle NM, Crowther MA, et al. The effect of rituximab on vaccine responses in patients with immune thrombocytopenia. Blood. 2013;122(11):1946–53.
Pavord S, Thachil J, Hunt BJ, Murphy M, Lowe G, Laffan M, et al. Practical guidance for the management of adults with immune thrombocytopenia during the COVID-19 pandemic. Br J Haematol. 2020;189(6):1038–43.
Rampotas A, Watson E, Burton K, Hill QA, Pavord S. A real-world study of immune thrombocytopenia management during the COVID-19 pandemic in the UK. Br J Haematol. 2022;196(2):351–5.
Cooper N, Bussel J. The pathogenesis of immune thrombocytopaenic purpura. Br J Haematol. 2006;133(4):364–74.
Jeyanathan M, Afkhami S, Smaill F, Miller MS, Lichty BD, Xing Z. Immunological considerations for COVID-19 vaccine strategies. Nat Rev Immunol. 2020;20(10):615–32.
Lee EJ, Cines DB, Gernsheimer T, Kessler C, Michel M, Tarantino MD, et al. Thrombocytopenia following Pfizer and Moderna SARS-CoV-2 vaccination. Am J Hematol. 2021;96(5):534–7.
Welsh KJ, Baumblatt J, Chege W, Goud R, Nair N. Thrombocytopenia including immune thrombocytopenia after receipt of mRNA COVID-19 vaccines reported to the Vaccine Adverse Event Reporting System (VAERS). Vaccine. 2021;39(25):3329–32.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N Engl J Med. 2020;383(27):2603–15.
Frenck RW Jr, Klein NP, Kitchin N, Gurtman A, Absalon J, Lockhart S, et al. Safety, immunogenicity, and efficacy of the BNT162b2 COVID-19 vaccine in adolescents. N Engl J Med. 2021;385(3):239–50.
Thomas SJ, Moreira ED Jr, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine through 6 months. N Engl J Med. 2021;385(19):1761–73.
Moreira ED Jr, Kitchin N, Xu X, Dychter SS, Lockhart S, Gurtman A, et al. Safety and efficacy of a third dose of BNT162b2 COVID-19 vaccine. N Engl J Med. 2022;386(20):1910–21.
Barda N, Dagan N, Ben-Shlomo Y, Kepten E, Waxman J, Ohana R, et al. Safety of the BNT162b2 mRNA COVID-19 vaccine in a nationwide setting. N Engl J Med. 2021;385(12):1078–90.
Arellano JLP (2020) Capítulo 14: mecanismos inmunológicos de la enfermedad (III): Tolerancia a los antígenos propios, Autoinmunidad. En: Sisinio de Castro. Manual de Patología general. 8ª edition,©2020 Elsevier España, S.L.U. ISBN: 978-84-9113-123-6. eISBN: 978-84-9113-162-5.
Klok FA, Pai M, Huisman MV, Makris M. Vaccine-induced immune thrombotic thrombocytopenia. Lancet Haematol. 2022;9(1):e73–80.
Saudagar V, Patil S, Goh S, Pothiawala S. Vigilance regarding immune thrombocytopenic purpura after COVID-19 vaccine. Ir J Med Sci. 2022;191(2):919–20.
Liu Y, Shao Z, Wang H. SARS-CoV-2 vaccine-induced immune thrombotic thrombocytopenia. Thromb Res. 2022;209:75–9.
Iba T, Levy JH. Thrombosis and thrombocytopenia in COVID-19 and after COVID-19 vaccination. Trends Cardiovasc Med. 2022;32(5):249–56.
Sarkar M, Madabhavi IV, Quy PN, Govindagoudar MB. COVID-19 vaccine-induced immune thrombotic thrombocytopenia: a review. Ann Thorac Med. 2022;17(1):1–13.
Schönborn L, Thiele T, Kaderali L, Günther A, Hoffmann T, Seck SE, et al. Most anti-PF4 antibodies in vaccine-induced immune thrombotic thrombocytopenia are transient. Blood. 2022;139(12):1903–7.
Ruhe J, Schnetzke U, Kentouche K, Prims F, Baier M, Herfurth K, et al. Acquired thrombotic thrombocytopenic purpura after first vaccination dose of BNT162b2 mRNA COVID-19 vaccine. Ann Hematol. 2022;101(3):717–9.
Yoshida K, Sakaki A, Matsuyama Y, Mushino T, Matsumoto M, Sonoki T, et al. Acquired thrombotic thrombocytopenic purpura following BNT162b2 mRNA coronavirus disease vaccination in a Japanese patient. Intern Med. 2022;61(3):407–12.
Deucher W, Sukumar S, Cataland SR. Clinical relapse of immune-mediated thrombotic thrombocytopenic purpura following COVID-19 vaccination. Res Pract Thromb Haemost. 2022;6(1): e12658.
Sissa C, Al-Khaffaf A, Frattini F, Gaiardoni R, Mimiola E, Montorsi P, et al. Relapse of thrombotic thrombocytopenic purpura after COVID-19 vaccine. Transfus Apher Sci. 2021;60(4): 103145.
Tso ACY, Ong KH, Sum CLL, Fan BE, Chan GYL, Christopher D, et al. Acquired thrombotic Thrombocytopenic purpura: a rare coincidence after COVID-19 mRNA vaccine? Semin Thromb Hemost. 2022.
Acknowledgements
We are grateful to SEHH (Sociedad Española de Hematología y Hemoterapia; Spanish Hematology and Hemotherapy Society) for providing scientific endorsement to this project.
Funding
No funding or sponsorship was received for the publication of this article. The study was funded by Novartis, Sobi, Amgen and Grifols laboratories but none of them had influence on the content of the manuscript.
Author Contributions
All authors have collaborated in the literature review and writing, provided input on each draft of the manuscript and approved the final version for submission. Conceptualization, methodology and style has been developed by Tomás José González-López and Isidro Jarque Ramos.
Disclosures
All named authors confirm that they have no conflicts of interest to declare.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
González-López, T.J., Bárez, A., Bernardo-Gutiérrez, A. et al. Recommendations on the Management of Patients with Immune Thrombocytopenia (ITP) in the Context of SARS-CoV-2 Infection and Vaccination: Consensus Guidelines from a Spanish ITP Expert Group. Infect Dis Ther 12, 303–315 (2023). https://doi.org/10.1007/s40121-022-00745-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00745-2