Abstract
Introduction
Acinetobacter baumannii is an important opportunistic pathogen responsible for causing nosocomial infections. Carbapenems are considered to be the drug of choice to treat infections caused by multidrug-resistant A. baumannii. The prevalent mechanism of carbapenem resistance in A. baumannii is enzymatic degradation by β-lactamases. Therefore, the aim of the study is to determine the prevalence and distribution of molecular determinants among the clinical isolates of carbapenem-resistant A. baumannii.
Methods
A total of 103 consecutive, non-duplicate carbapenem-resistant A. baumannii isolated from blood and endotracheal aspirates (ETAs) were included in the study. The CarbAcineto NP test was performed for the screening of carbapenemase production. Polymerase chain reaction (PCR) was performed to detect extended spectrum β-lactamases (ESBLs), metallo-β-lactamases (MBLs) and oxacillinases (OXAs). PCR was done for the detection of ISAba1 elements, and mapping PCR was performed to identify the position of ISAba1 with respect to the OXA-23-like gene.
Results
Among the 103 A. baumannii isolates, 94 were phenotypically identified as carbapenemase producers. blaPER was the most common among the ESBLs. Among MBLs, blaNDM was predominant followed by the blaVIM gene. blaOXA-51 and blaOXA-23 were the most common and present in all 103 isolates. Almost 80% of the isolates had ISAba1 upstream blaOXA-23 gene.
Conclusion
The blaOXA-23 and blaNDM genes are the most common type of oxacillinases and metallo β-lactamases, respectively, and contribute to carbapenem resistance in clinical isolates of A. baumannii. The presence of ISAba1 upstream of the blaOXA-23 gene suggests that the insertion element acts as a promoter for its increased expression.
Funding
Indian Council of Medical Research, New Delhi, India (ref. no. AMR/TF/54/13ECDHII dated 23 October 2013).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acinetobacter baumannii is a leading cause of nosocomial infections with increased morbidity and mortality [1]. A. baumannii is intrinsically resistant to most antibiotics and has the ability to acquire resistance genetic determinants from the environment as well [2]. Antimicrobial resistance to β-lactams in A. baumannii includes: (1) enzymatic mechanisms or production of β-lactamases and (2) non-enzymatic mechanisms such as modification of membrane permeability by either loss of or decrease in expression of outer membrane porins or an increased expression of efflux pumps [2, 3].
Carbapenems are the drug of choice to treat infections caused by multidrug-resistant A. baumannii. However, resistance to carbapenems is increasing and has been reported worldwide. Carbapenem resistance in A. baumannii can be either carbapenemase mediated or non-carbapenemase mediated. Carbapenemase-mediated resistance is mainly due to the production of class A (serine proteases), class B (metallo-beta-lactamases) and class D (oxacillinases) carbapenemases, whereas non-carbapenemase-mediated resistance involves upregulation of the efflux pumps and/or loss of outer membrane porins [4].
Resistance to carbapenem in A. baumannii is most frequently due to oxacillinases, which can be intrinsic or acquired. The intrinsic blaOXA-51 gene is considered to be specific for A. baumannii, since the said gene is carried in its chromosome. Acquired OXA enzymes, which are encoded by the blaOXA-23, blaOXA-40 and blaOXA-58 genes, are more predominant in A. baumannii, whereas MBLs encoded by the blaIMP, blaVIM, blaNDM and blaSIM genes are more predominant in non-baumannii Acinetobacter isolates [5].
The insertion sequence has a major role in the overproduction and dissemination of OXA genes in A. baumannii. Overexpression of OXA genes is driven by insertion sequences, which provide promoter sequences, thereby contributing to high levels of carbapenem resistance. The insertion sequence ISAba1 belongs to the IS4 family and has been associated with several resistance genes in A. baumannii, such as blaOXA-23, blaOXA-51 and blaOXA-58 [6].
Limited data are available on the resistance pattern and molecular determinants responsible for carbapenem resistance in A. baumannii from India. The objectives of this study were (1) to determine the trend in the antibiotic resistance profile for invasive Acinetobacter species and (2) to detect the prevalence of the resistance genes responsible for beta lactamases such as extended spectrum and carbapenamases in Acinetobacter species.
Methods
Bacterial Isolates
The study was conducted at a tertiary care hospital, South India, from January 2014 to July 2015. A total of 103 non-duplicate, consecutive, carbapenem-resistant isolates recovered from invasive infections of Acinetobacter species were included in this study. The isolates were obtained from invasive clinical specimens including blood and endotracheal aspirates (ETAs). The isolates were identified up to the species level as Acinetobacter baumannii calcoaceticus complex (ABCC) by standard biochemical tests and confirmed as Acinetobacter baumannii using blaOXA-51 PCR, which is intrinsic to this species [7].
Antimicrobial Susceptibility Testing
Susceptibility to different classes of antibiotics was determined by the Kirby Bauer disc diffusion method and interpreted according to the Clinical Laboratory Standard Institute guidelines [8, 9]. Antibiotics tested were ceftazidime (30 µg), cefepime (30 µg), piperacillin/tazobactam (100/10 µg), cefoperazone/Sulbactam (75/30 µg), amikacin (30 µg), netilmycin (30 µg), tobramycin (10 µg), aztreonam (30 µg), levofloxacin (5 µg), tetracycline (30 µg), co-trimoxazole (1.25/23.75 µg), imipenem (10 µg), meropenem (10 µg) and polymyxin B (10 µg).
Phenotypic Characterization
Phenotypic detection of carbapenemase was done by the CarbAcineto NP test. In brief, all the study isolates to be tested were grown on a Mueller-Hinton agar plate for 24 h, and the isolated colonies were re-suspended in two 1.5-ml centrifuge tubes (A and B) containing 100 µl NaCl (5 M). In tube A, 100 µl of solution A (phenol red solution with zinc sulfate) was added, and in tube B, 100 µl of solution A with imipenem (6 mg/ml) was added. The tubes were incubated at 37 °C for a maximum of 2 h. The carbapenemase activity was detected by color change in tube B resulting from hydrolysis of imipenem leading to a decrease in pH value [10]. Concurrently, BAA-1705 and BAA-1706 were included as positive and negative controls, respectively.
Molecular Characterization
PCR for the Detection of Carbapenemase Genes
Uniplex PCR was performed to detect the presence of the intrinsic blaOXA-51 gene. Multiplex PCR was performed to detect ESBL genes such as blaTEM, blaSHV, blaPER, blaVEB and blaGES. A second multiplex PCR was performed for MBL genes such as blaKPC, blaIMP, blaVIM, blaSIM, blaNDM and blaSPM. A third multiplex PCR was performed to detect the presence of acquired OXA genes, namely blaOXA-23, blaOXA-24 and blaOXA-58. Uniplex PCR was performed to detect the presence of the insertion sequence (IS) element, ISAba1 and PCR mapping was performed to map the position of the IS element relative to the blaOXA-23 gene.
Primers used in this study were described earlier [11–16]. Briefly, for PCR amplification, 2 µl of template DNA was added to 18 µl reaction containing 10 µl of Qiagen master mix, 2 µl of primer mix (1 µl each of the respective forward and reverse primers) and 6 µl of molecular-grade water. The cyclic conditions for the intrinsic OXA-51 gene were: initial denaturation at 94 °C for 3 min, 35 cycles of 94 °C for 45 s, 57 °C for 45 s and 72 °C for 1 min, followed by extension of 72 °C for 5 min. For ESBL and MBL genes, initial denaturation at 95 °C for 15 min, 30 cycles of 94 °C for 30 s, 59 °C for 1 min 30 s and 72 °C for 1 min 30 s were followed by extension of 72 °C for 10 min.
For acquired OXA genes, the initial denaturation was at 95 °C for 15 min, 30 cycles of 94 °C for 30 s, 52 °C for 1 min 30 s and 72 °C for 1 min 30 s, followed by extension of 72 °C for 1 min 30 s.
For the IS element PCR, briefly, 5 µl of template DNA was added to 20 µl reaction containing 12.5 µl of Hot Start Master Mix, 1 µl each of forward and reverse primer and 5.5 µl of molecular-grade water. For mapping PCR, 5 µl of template DNA was added to a 20-µl reaction containing 12.5 µl of Hot Start Master Mix, 1 µl each of IS forward and OXA-23 reverse primer, and 5.5 µl of molecular-grade water. The cyclic conditions for IS element PCR and mapping PCR were as follows: initial denaturation at 95 °C for 15 min, 35 cycles of 95 °C for 45 s, 56 °C for 45 s and 72 °C for 2 min, followed by extension of 72 °C for 10 min.
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Results
A total of 103 invasive clinical isolates of Acinetobacter species were included in this study. Thirty isolates were from blood specimens, and 73 isolates were from ETA.
All 103 isolates (100%) were confirmed as Acinetobacter baumannii by the presence of the blaOXA-51 gene.
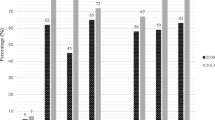
Antimicrobial Susceptibility
Antimicrobial susceptibility testing revealed that all the isolates were resistant to ceftazidime, cefepime, piperacillin/tazobactam, cefoperazone/sulbactam, aztreonam, imipenem, meropenem, amikacin, netilmycin, tetracycline, tobramycin, levofloxacin and co-trimoxazole. Almost 102 (98%) of the study isolates were susceptible to polymyxin B.
Phenotypic Detection
Among the 103 clinical isolates, the CarbAcineto NP test was positive in 94 (91.2%) isolates and negative in 9 (8.7%) (Table 1).
PCR for ESBL, MBL and OXA Genes
Among the 103 isolates tested for ESBLs, the PER gene was present in 42 isolates (41.5%) followed by the TEM gene in 8 (7.9%), SHV gene in 1 (0.9%) and VEB gene in 1 (0.9%) isolate. PER and TEM genes coexisted in seven (6.9%) isolates followed by PER and SHV coexisting in one isolate (2%). None of the isolates had the GES gene (Table 1).
Twenty isolates were positive for the NDM gene (19.2%), and six isolates were positive for the VIM gene (5.7%). One isolate (0.9%) had both VIM and NDM genes. None of the isolates had KPC, IMP, SPM and SIM genes (Table 1).
The acquired OXA carbapenemase, blaOXA-23 gene was present in 101 isolates (98%). Two isolates (2%) had both blaOXA-23 and blaOXA-24 genes. None of the isolates had the blaOXA-58 gene (Table 1).
ISAba1 and Mapping PCR
ISAba1 and mapping PCR was performed for all the clinical isolates (n = 103). The ISAba1 element was found upstream of the corresponding blaOXA-23 gene in 82 isolates (79.6%). Seven isolates (6.7%) were positive for the ISAba1 element but not found upstream of the blaOXA-23 gene. Fourteen isolates (14%) were negative for the ISAba1 element (Table 1).
Discussion
Multidrug-resistant A. baumannii is increasingly reported in healthcare-associated infections worldwide. This scenario has left carbapenems as the drug of choice to treat severe infections caused by MDR A. baumannii. However, increased resistance to carbapenems due to diverse intrinsic and acquired resistance mechanisms is emerging. Production of class D OXA carbapenemases and class B metallo-β-lactamases plays a predominant role in contributing to carbapenem resistance to A. baumannii worldwide [17].
The SENTRY study reports that the susceptibility rate of imipenem to A. baumannii has declined from 73.7% in 2001–2004 to 37.4 in 2009 in the Asia-Pacific region [18]. The Tigecycline Evaluation and Surveillance Trial (TEST) study between 2005 and 2009 reported the overall susceptibility rate for imipenem and meropenem was 54.1% and 51.8%, respectively [1]. A recent study from South India has reported 34–93.6% carbapenem susceptibility in A. baumannii isolates [19].
Due to the intrinsic low permeability of carbapenems, phenotypic detection of carbapenemase is difficult in Acinetobacter sp. A number of phenotypic tests such as the modified Hodge test and inhibition-based tests have been proposed for the rapid detection of carbapenemases in Acinetobacter sp. These tests were efficient in detecting IMP and VIM producers, leaving the most predominant carbapenemases such as OXA and NDM producers undetected [10]. Although CLSI 2015 recommends the use of the carba NP test, it has not been well validated for the detection of carbapenemase-producing Acinetobacter sp. The rate of imipenem hydrolysis achieved with OXA enzymes is too low to be detected with the carba NP test [10]. Therefore, a modified version of the Carba NP known as the CarbAcineto NP was proposed for the phenotypic detection of carbapenemase production in Acinetobacter sp. The sensitivity and specificity of the CarbAcineto NP test are reported to be 100% and 94.7%, respectively, in comparison to the carba NP test where the sensitivity is 11.9% only [10]. However, the CLSI is non-committal about this modification.
In this study, 94 out of 103 clinical isolates were positive for the CarbAcineto NP test, and all were positive for the blaOXA-23 gene. Nine isolates were negative for the CarbAcineto NP.
Among the study isolates, OXA carbapenemases were detected in 101 (98%) isolates of carbapenem-resistant A. baumannii. The blaOXA-23-like oxacillinases were the most common type. A study from East India also showed the OXA-23 genes as the prevalent type of oxacillinase contributing to carbapenem resistance [17]. Another study from South India showed the prevalence of the OXA-23 gene to be 56.8% [19]. Among the metallo β-lactamases (MBLs), 20 isolates were positive for the NDM gene while 6 were positive for the VIM gene. This study showed NDM as the predominant MBL gene. However, studies by Saranathan et al. and Amudhan et al. showed IMP-like and VIM-like as the prevalent MBL genes [19, 20]. Of the 103 isolates tested, 52 (50%) were positive for 1 of the ESBL genes such as PER, TEM and SHV. In addition, we found coexistence of PER, TEM and OXA-23 in six isolates, PER, TEM, VIM and OXA-23 in one isolate, and PER, SHV and OXA-23 in one isolate.
Class D OXA enzymes possess weak carbapenemase activity. However, the presence of an insertion sequence upstream of the OXA gene promotes their expression and can modulate the mobility of OXA genes. Evans et al. reported that a promoter for the blaOXA-23-like gene is provided by ISAba1 when it is inserted 25-bp upstream of the gene [21]. Also studies have shown that transposons such as Tn2006 can be formed by two ISAba1 elements bracketing the blaOXA-23 gene, which in turn involves in the dissemination of resistance determinants [22]. In this study, we found that 79.6% of the isolates had ISAba1 upstream of the OXA-23-like gene, which could provide a promoter for OXA-23 gene overproduction.
Even though the blaOXA-51-like gene is chromosomally encoded and has weak carbapenemase activity, studies have reported that the presence of ISAba1 upstream to this gene can provide a promoter that allows the hyper-production of carbapenemase, resulting in carbapenem resistance [6]. In this study, 6% of the carbapenem-resistant A. baumannii isolates had an ISAba1 element, which was not found upstream but seen elsewhere than the blaOXA-23 gene. Carbapenem resistance in these isolates might be due to overexpression of the blaOXA-51 gene. Future studies are required to confirm the role of insertion sequence-induced overexpression of the blaOXA-51 gene. Studies have reported that carbapenem resistance in A. baumannii is mainly due to carbapenemase mediated [4]. However, non-carbapenemase-mediated resistance mechanisms such as reduced membrane permeability due to porin changes and overexpression of efflux pumps make a trivial contribution toward carbapenem resistance in A. baumannii [23]. Heritier et al. reported that the synergism between acquired oxacillinases and the RND efflux pump, AdeABC, was implicated in the increased levels of resistance toward carbapenems [24]. Therefore, future studies on the role of non-carbapenemase-mediated mechanisms in A. baumannii are required.
Conclusion
In conclusion, this study reports the emergence of blaOXA-23-like and blaNDM-like genes as the predominant cause of carbapenem resistance in Acinetobacter baumannii. Additionally, in this study we found the ISAba1 insertion sequence, which plays an important role in the overexpression of blaOXA-23.
References
Abbott Iain, Cerqueira GM, Bhuiyan S, Peleg AY. Carbapenem resistance in Acinetobacter. Laboratory challenges, mechanistic insights and therapeutic strategies. Expert Rev Anti Infect Ther. 2013;11(4):395–409.
Dijkshoorn L, Nemec A, Seifert H. An increasing threat in hospitals: multidrug-resistant Acinetobacter baumannii. Nat Rev Microbiol. 2007;5:939–51.
Roca I, Espinal P, Vila-Farrés X, Vila J. The Acinetobacter baumannii oxymoron: commensal hospital dweller turned pan-drug-resistant menace. Front Microbiol. 2012;3:Article 148.
Poirel L, Nordmann P. Carbapenem resistance in Acinetobacter baumannii: mechanisms and epidemiology. Clin Microbiol Infect. 2006;12:826–36.
Kim UJ, Kim HK, An JH, Cho SK, Park K-H, Jang H-C. Update on the epidemiology, treatment, and outcomes of carbapenem-resistant Acinetobacter infections. Chonnam Med J. 2014;50(2):37.
Turton JF, Ward E, Woodford N, Kaufmann ME, Pike R, Livermore DM, Pitt TL. The role of ISAba1 in expression of OXA carbapenemase genes in Acinetobacter baumannii. FEMS Microbiol Lett. 2006;258:72–7.
Turton JF, Woodford N, Glover J, Yarde S, Kaufmann ME, Pitt TL. Identification of Acinetobacter baumannii by detection of the blaOXA-51-like carbapenemase gene intrinsic to this species. J Clin Microbiol. 2006;44(8):2974–6.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: twenty second informational supplement M100–S22. Wayne: CLSI; 2014.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: twenty second informational supplement M100–S22. Wayne: CLSI; 2015.
Dortet L, Poirel L, Errera C, Nordmann P. Carbacineto NP test for rapid detection of carbapenemase-producers in Acinetobacter spp. J Clin Microbiol. 2014. doi:10.1128/JCM.00594-14.
Dallenne C, Da Costa A, Decré D, Favier C, Arlet G. Development of a set of multiplex PCR assays for the detection of genes encoding important b-lactamases in Enterobacteriaceae. J Antimicrob Chemother. 2010;65:490–5.
Lascols C, Hackel M, Marshall SH, et al. Increasing prevalence and dissemination of NDM-1 metallo-β-lactamase in India: data from the SMART study (2009). J Antimicrob Chemother. 2011;9:1992–7.
Yigit H, Queenan AM, Anderson GJ, et al. Novel carbapenem-hydrolyzing betalactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother. 2001;45:1151–61.
Poirel L, Walsh TR, Cuvillier V, Nordmann P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis. 2011;70:119–23.
Woodford Neil, Ellington Matthew J, Coelho Juliana M, Turton Jane F, Elaina Ward M, Brown Susan, et al. Multiplex PCR for genes encoding prevalent OXA carbapenemases in Acinetobacter spp. Int J Antimicrob Agents. 2006;27:351–3.
Segal H, Garny S, Elisha BG. Is ISABA-1 customized for Acinetobacter? FEMS Microbiol Lett. 2005;243:425–9.
Peleg AY, Seifert H, Paterson DL. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev. 2008;21(3):538–82.
Kamolvit W, Sidjabat HE, Paterson DL. Molecular epidemiology and mechanisms of carbapenem resistance of Acinetobacter spp. in Asia and Oceania. Microb Drug Resist. 2015;21(4):424–34.
Saranathan R, Vasanth V, Vasanth T, Shabareesh PRV, Shashikala P, Devi CS, et al. Emergence of carbapenem non-susceptible multidrug resistant Acinetobacter baumannii strains of CC 103B and CC 92B clonal complexes harboring OXA-type carbapenemases and metallo-β-lactamases in Southern India. Microbiol Immunol. 2015;59(5):277–84.
Amudhan SM, Sekar U, Arunagiri K, Sekar B. OXA beta-lactamase-mediated carbapenem resistance in Acinetobacter baumannii. Indian J Med Microbiol. 2011;29(3):269–74.
Evans BA, Amyes SGB. OXA β-lactamases. Clin Microbiol Rev. 2014;27(2):241.
Mugnier PD, Poirel L, Naas T, Nordmann P. Worldwide dissemination of the blaOXA-23 Carbapenemase Gene of Acinetobacter baumannii. Emerg Infect Dis. 2010;16(1):35–40.
Evans BA, Hamouda A, Amyes SGB. The rise of carbapenem-resistant Acinetobacter baumannii. Curr Pharm Des. 2013;19:223–38.
Héritier C, Poirel L, Lambert T, Nordmann P. Contribution of acquired carbapenem-hydrolyzing oxacillinases to carbapenem resistance in Acinetobacter baumannii. Antimicrob Agents Chemother. 2005;49(8):3198–202.
Acknowledgments
The authors gratefully acknowledge Dr. Kamini Walia, Scientist E, Division of Epidemiology and Communicable Diseases, Indian Council of Medical Research (ICMR), New Delhi, and the ICMR Council itself for providing the grant for this research and the Institutional Review Board of the Christian Medical College, Vellore (83-i/11/13). All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole and have given final approval for the version to be published. The study has been funded by Indian Council of Medical Research, New Delhi, India (ref. no. AMR/TF/54/13ECDHII dated 23/10/2013).
Compliance with Ethical Standards
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Disclosures
The authors Saranya Vijayakumar, Radha Gopi, Priya Gunasekaran, Manjurekar Bharathy, Kamini Walia, Shalini Anandan and Balaji Veeraraghavan declare no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/5AE4F060371B2550.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Vijayakumar, S., Gopi, R., Gunasekaran, P. et al. Molecular Characterization of Invasive Carbapenem-Resistant Acinetobacter baumannii from a Tertiary Care Hospital in South India. Infect Dis Ther 5, 379–387 (2016). https://doi.org/10.1007/s40121-016-0125-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-016-0125-y