Abstract
Introduction
Despite the increasing age of the multiple sclerosis (MS) patient population, data are lacking on MS patients in later life. This retrospective study investigated treatment patterns, healthcare resource utilization (HCRU), and healthcare costs (HCCs) for patients enrolled in Medicare, in relation to disease-modifying therapy (DMT) and corticosteroid treatment as a marker for relapse.
Methods
Medical and pharmacy claims between January 1, 2010 and July 31, 2015 identified MS patients. The anchor date was defined as the most recent MS claim. Analyses were performed on claims in the 12-month baseline period before the anchor date. Outcomes were stratified by DMT use and number (0, 1, or ≥ 2) of corticosteroid treatments.
Results
Among Medicare MS patients (n = 7072; mean age 57 years), 66% received DMT during the baseline period; 31% had 1 claim and 16% had ≥ 2 claims for corticosteroids. Compared with patients not receiving DMT, patients on DMT were less likely to receive corticosteroids (39% vs 62%) and had fewer all-cause hospitalization episodes and ER visits. DMT use was associated with lower HCRU but higher HCCs in patients both with and without corticosteroid treatment. DMT switching rates were low, both among patients with no corticosteroid (5.6%) and patients with 1 (9.3%) or ≥ 2 (11.1%) corticosteroid treatments. DMT switches were most frequently from an injectable to an oral therapy.
Conclusion
In Medicare patients with MS, DMT use was associated with higher HCCs but lower HCRU, indicative of better health outcomes; however, low DMT switching rates may be an indicator of possible clinical inertia.
Funding
Sanofi.
Plain Language Summary
Plain language summary available for this article.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Plain Language Summary
What did this study look at?
-
Disease-modifying therapy (known as DMT) is used to treat MS and help prevent relapses. There are several types of DMT.
-
People taking DMT may still relapse. If so, some may receive steroid treatment and can switch to another type of DMT, which may be more effective at preventing relapses.
-
The researchers used health insurance records of MS patients covered by Medicare or by commercial insurance to see if DMT helped people with MS to:
-
Avoid having relapses.
-
Avoid costly care, including hospital visits.
-
Who took part in this study?
-
The study included more than 8400 people with MS living in the US.
What were the results of the study?
-
MS patients in Medicare were not much older than those with commercial insurance, suggesting that they were in Medicare because of disability instead of age.
-
Two-thirds of people with MS received DMT during the year-long study.
-
Of these, almost half had one or more relapses treated with steroids.
-
People taking DMT had fewer relapses and hospital visits compared with people not taking DMT.
-
Fewer than one in ten people in Medicare who relapsed while taking DMT switched to another DMT that could work better.
How could this study benefit MS patients?
-
Shows that DMT can improve health of MS patients, resulting in fewer relapses and hospital visits.
-
Raises awareness that doctors treating Medicare patients who relapse on DMT may not be switching their patients’ DMT as much as they could after patients relapse.
Introduction
Multiple sclerosis (MS) is a chronic and potentially debilitating neurological disorder categorized into several relapsing or progressive subtypes [1]. It affects an estimated 2.3 million people worldwide [2], and onset commonly occurs between 20 and 50 years of age [3]. MS is characterized by neurological damage that could result in physical, social, and mental dysfunction that negatively affects quality of life and leads to disability and unemployment [4,5,6]. The burden of MS is further exacerbated by the onset of comorbidities, including hypertension, hyperlipidemia, chronic pain, gastrointestinal conditions, epilepsy, depression, anxiety, and diabetes [4, 7,8,9]. An increase in the number or degree of comorbidities has been associated with a lower likelihood of initiating treatment with a disease-modifying therapy (DMT) for MS [8, 10].
A primary goal of a DMT for relapsing–remitting MS is to reduce the relapse rate and mitigate long-term disease progression and cumulative disabilities [11, 12]. At the time of this study, available DMTs for patients with MS included injectable (interferon beta-1a and -1b, glatiramer acetate, and peginterferon beta-1a); infusible (natalizumab, alemtuzumab, and mitoxantrone); and oral (fingolimod, dimethyl fumarate, and teriflunomide) treatments [13]. Conventionally, injectable therapies have been used as first-line treatments for MS [14, 15]. However, recent advances in DMTs have enabled a shift in treatment patterns to newer oral or high-efficacy infusible therapies [16,17,18]. Published studies of DMT treatment patterns show that adherence and discontinuation rates may vary [10, 14], and indicate that treatment switching is fairly common through the course of the disease [14, 15].
Although treatment guidelines recommend use of an appropriate DMT for MS, patients may receive treatments in addition to, or in place of, DMT to address relapses, as well as physical and mental symptoms [13]. Where appropriate, concomitant short-term therapy with steroids is recommended for patients experiencing relapses [19]. Accordingly, in healthcare claims databases, corticosteroid use in MS patients is a likely indicator of relapse activity [20]. Failure to initiate or switch DMT after relapse could indicate clinical inertia, in which patients are not provided with individually optimized treatment. Consistent with this possibility, we previously observed that only a small percentage of MS patients who received corticosteroid treatment subsequently switched DMT [21].
Although the lifespan of MS patients has been extended in the past few decades [22, 23], the proportion dropping out of the workforce has not decreased [24, 25], and fewer than half of patients maintain full- or part-time employment [26], suggesting a gap in awareness of the burdens on patients with MS as they age into their 40s and 50s. Furthermore, patients entering middle age are met with unique challenges compared with those of younger patients, including increased prevalence of physical comorbidities [9]. As a result, MS treatment choices may differ between middle-aged or older patients, and younger patients.
A descriptive study was conducted to better understand treatment patterns in MS patients enrolled in Medicare, a federally subsidized insurance program, as well as in a private (commercial) insurance patient population. The mean age of 57 reported for MS patients in Medicare is younger than the typical Medicare entry age of 65 years [21], suggesting that enrollment is primarily due to disability rather than age. The Medicare population therefore provides a picture of MS patients who are middle aged or older, and allows further analysis of this understudied population. The objectives of this study were to complement the existing body of evidence by describing demographic and clinical characteristics, DMT adherence and switching patterns, and healthcare resource utilization (HCRU) and healthcare costs (HCCs) for MS patients in Medicare, and to determine whether the number of relapses correlated with the choice of medication or switching patterns.
Methods
Study Design
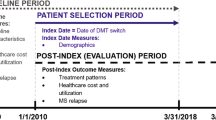
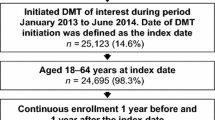
Medical and pharmacy claims recorded in the Humana Medicare Advantage Plus (Part D) and commercial insurance databases between January 1, 2010 and July 31, 2015 were used to identify patients diagnosed with MS according to the International Classification of Disease, 9th Revision, Clinical Modifications (ICD-9-CM; code: 340). Medical claims data included diagnosis codes based on the ICD-9-CM associated with medical encounters and financial information. Pharmacy claims included dates for prescriptions, national drug codes, and drug cost data. The date of the most recent claim with a diagnosis of MS during the identification period served as the anchor date, in order to capture the most recent prescribing behavior and treatment patterns. Eligible patients were aged 18–80 years at the anchor date, were continuously enrolled in either program for 12 months before the anchor date (baseline period), and had no claims for rheumatoid arthritis, systemic lupus erythematosus, end stage renal disease, cancer, pregnancy, or organ transplant. Patients were categorized according to whether they received a DMT and by the number of corticosteroid treatments (0, 1, or ≥ 2) received at any time during the baseline period. A corticosteroid treatment was defined as the presence of an initial corticosteroid delivery; a refill or re-injection within 45 days of the initial corticosteroid delivery was not considered a new corticosteroid treatment. Corticosteroid treatment could be before or after DMT administration, and the delay between the events could range from 0 days (DMT and corticosteroid treatment on the same day) to 365 days (maximum period observed). Treatments were identified using Current Procedural Terminology and Generic Product Identifier codes. The current study was submitted and approved by an institutional review board, Schulman Associates IRB, Inc, before study initiation. All procedures performed in this study were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Outcome Measures
Demographic characteristics included age (as of the anchor date), gender, and race/ethnicity. Clinical characteristics included the Deyo-Charlson Comorbidity Index (DCCI) score, and comorbidities of interest that were present before the anchor date.
Outcomes included DMT adherence and switching, and all-cause and MS-related HCRU and HCCs. Adherence was determined using the proportion of days covered (PDC) for the DMT most recent to the anchor date during the 12-month baseline period, and used a variable denominator corresponding to the number of days from the date of the first fill of the most recent therapy identified to the anchor date. Adherence was defined as PDC ≥ 80%. DMT switching was defined by the presence of at least two distinct DMTs during the baseline period, and assessed as the number of patients who switched from one DMT to another. Analyses of DMT switching did not allow for overlap of supply of treatments, and no additional switches after the first switch were considered. Assessment of HCRU included the number of patients with a magnetic resonance imaging (MRI) scan, and whether the patient had an office visit with their general practitioner or a specialist, received blood work, undertook physical therapy, or had a hospitalization or emergency room (ER) visit. All DMT switching and healthcare utilizations were analyzed for the initial corticosteroid treatment in the case of patients with ≥ 2 corticosteroid treatments.
HCRU and HCCs were calculated for both all-cause and MS-related claims. HCRU was assessed in terms of inpatient visits and length of stay, ER visits, outpatient visits, physician encounters, imaging and MRI services, and pharmacy services. Inpatient stays excluded facility transfers contiguous to a stay. Outpatient visits were calculated using distinct service dates and distinct providers with place of treatment listed as “outpatient including office visits”. Physician encounters were based on a subset of outpatient visits where the place of service was listed as “office”. MRI services constituted a subset of imaging services.
Pharmacy services were determined by the counts of distinct service dates (fill date) and national drug code. Services associated with injectable DMTs were identified through pharmacy claims using the national drug code identifier, and services associated with infusible DMTs were identified through medical claims using Current Procedural Terminology codes. All pharmacy services for injectable and infusible DMTs were normalized to a 30-day supply period. All drug services, whether associated with a medical or pharmacy claim, were assigned to pharmacy costs.
HCCs were determined using the allowable amount remitted to providers on claims. HCCs were categorized as pharmacy costs, medical costs (including office visits, outpatient and inpatient costs, ER service and imaging service costs) and total costs (sum of medical and pharmacy costs). All-cause HCRU and HCCs were calculated using all medical, pharmacy, and laboratory claims during the baseline period. MS-related HCRU and HCCs were calculated using claims that had an MS diagnosis code in any of the nine diagnoses positions.
Statistical Analysis
Descriptive statistics were generated to describe the demographic and clinical characteristics, and proportions of patients receiving DMTs and/or corticosteroid treatment during the baseline period. General linear regression models were used for analysis of HCRU outcomes. A generalized linear regression model with a log-link and gamma distribution was used for the analysis of HCCs. Both models used demographic (age, gender, geographical region, plan type, and race/ethnicity) and clinical (DCCI score, additional comorbid conditions, DMT and corticosteroid treatment) characteristics as covariates. HCRU and HCCs were aggregated over the 12-month baseline period. HCCs were adjusted to the 2015 Consumer Price Index generated by the US Bureau of Labor Statistics. All statistical analyses were performed using SAS Institute Inc. Enterprise Guide 7.11 (base v9.4).
Results
Patients
A total of 15,978 Medicare beneficiaries with a diagnosis of MS were initially identified, of whom 7072 met the criteria for study inclusion. Of these, 2168 (30.7%) had 1 claim and 1136 (16.1%) had ≥ 2 claims for corticosteroids during the baseline period, and 4689 (66.3%) received DMT during the baseline period. Medicare patients receiving DMT were less likely to receive any corticosteroids than patients not receiving DMT (38.8% vs 62.3%), and less likely to receive ≥ 2 corticosteroids (13.1% vs 21.9%).
Of the 1484 MS patients covered by commercial insurance and meeting the inclusion criteria, 451 (30.4%) had 1 claim and 217 (14.6%) had ≥ 2 claims for corticosteroids during the baseline period, and 1157 (78.0%) received DMT during the baseline period. Commercial insurance patients receiving DMT were also less likely to receive corticosteroids than patients not receiving DMT (38.9% vs 66.7%).
Demographic and Clinical Characteristics
Demographic and clinical characteristics for patients with MS in the Medicare population are described in Table 1, stratified by DMT use and by number (0, 1, or ≥ 2) of corticosteroid treatments (corresponding data for the commercial insurance patient population are reported in Table S1 in the electronic Supplementary materials). The Medicare MS population (mean age: 57 years) was younger than the typical Medicare entry age of 65 years. Only 38% of the Medicare MS population was over age 60. Average age for the commercial insurance MS population was 47 years. Patients not receiving DMT were 3 to 5 years older than those who received DMT among the Medicare population, and 5 to 7 years older among the commercial insurance population. Medicare patients were predominantly residing in the Southern USA, and of white race/ethnicity; a similar pattern was observed for commercial insurance patients, except that a lower proportion were of white race/ethnicity. DCCI scores were low overall, with slightly higher scores among Medicare patients who did not receive a DMT and those who received corticosteroid treatments. Approximately 92–97% of Medicare patients had an additional comorbidity (71–86% for commercial insurance MS patients), with no differences in cormorbidity incidence between DMT groups. Incidence of certain comorbidities was higher for Medicare patients with corticosteroid treatments (versus those without corticosteroid), most notably with regard to anxiety, pain, and fatigue.
Patterns of DMT Use
The majority of Medicare patients treated with a DMT received an injectable treatment (53.8%), whereas 35.7% received an oral treatment and 10.5% received an infusible treatment. The most commonly used injectable treatments among Medicare patients were glatiramer acetate (24.3%) and interferon beta-1a (22.9%). Dimethyl fumarate was the most common oral treatment (21.4%) and natalizumab was the most common infusible treatment (10.3%).
Among Medicare patients, mean PDC for DMTs was high for oral (94%), injectable (90%), and infusible (98%) treatments, and each individual DMT also had PDC of at least 89%. Too few patients were treated with mitoxantrone (< 10) to accurately calculate mean PDC. Adherence (defined as PDC ≥ 80%) was achieved by 87% of patients (oral, 90%; injectable, 83%; infusible, 97%).
Of the 4689 Medicare patients receiving a DMT, 341 (7.3%) had switched treatments. Rates of DMT switching were low, both among patients who did not receive corticosteroid and patients with 1 or ≥ 2 episodes of corticosteroid use (Table 2). Among Medicare patients who switched DMT, interferon beta-1a was the most common pre-switch DMT, followed by glatiramer acetate (Table 2). Patients most often switched to an oral DMT, including dimethyl fumarate, teriflunomide, or fingolimod. There was no trend for switching to an infusible DMT with increasing number of corticosteroid treatments.
Healthcare Resource Utilization
Among Medicare MS patients, a greater proportion of those who received corticosteroid treatment had MRI services, inpatient visits, and ER visits compared with patients who had no corticosteroid, and the proportion of patients using these services increased with increasing corticosteroid treatments (Table 3). DMT use was not only associated with fewer corticosteroid treatments, but also with fewer inpatient and ER visits across all corticosteroid use categories. The impact of DMT use and corticosteroid use on HCRU was similar in the commercially insured patient population, except that corticosteroid use in commercially insured patients was also associated with a higher frequency of physical therapy services (Table S2).
MS-related utilization of pharmacy services, outpatient visits, and physician encounters were higher for Medicare patients on DMT than those not taking a DMT (Table 4), and a similar pattern was observed for the commercial insurance patient population (Table S3). However, the Medicare MS patient population who received DMT had fewer all-cause ER visits, fewer inpatient stays, and a shorter mean length of inpatient stays, compared with patients not taking a DMT. Among DMT-treated Medicare patients, corticosteroid use was associated with more MS-related and all-cause pharmacy services, outpatient visits, physician encounters, and ER visits. This pattern of increased utilization of services among corticosteroid-treated patients was also observed for the commercial insurance population.
Healthcare Costs
Costs and cost trends were similar in the Medicare (Table 5) and commercial insurance (Table S4) populations. Total MS-related and total all-cause HCCs were higher for patients receiving DMT than for those without DMT, driven by higher pharmacy costs. MS-related medical costs were slightly higher with DMT use among Medicare patients. In contrast, all-cause medical costs were lower with DMT use. MS-related medical costs were similar across all corticosteroid use categories, but all-cause medical costs and total costs increased with increasing corticosteroid treatments.
Discussion
This retrospective claims-based study sought to examine the cost and resource burden of MS in patients in Medicare, as well as care and treatment patterns in this understudied population. The average age of the Medicare MS population included in this study was younger than the typical Medicare entry age of 65 years, and about 10 years older than the commercially insured MS population. This likely reflects that the Medicare population included younger patients, whose disability—rather than age—was driving them into the Medicare program. This observation highlights that for MS patients, participation in Medicare is not necessarily synonymous with older age and progressive disease.
Approximately two-thirds of Medicare MS patients received treatment with a DMT; this proportion is higher than reported DMT use in other studies [27]. A majority of the Medicare MS patients were adherent to their DMT, and the mean PDC for each DMT was 89% or higher. The adherence rate among DMT-treated Medicare patients in the present study is somewhat higher than that reported in previous studies, although methods to assess DMT adherence varied [18, 28, 29]. DMT use among Medicare MS patients lowered corticosteroid use (a proxy for relapse), hospitalizations, and ER visits, consistent with a previous study showing an inverse association of DMT use and the risk of relapse, hospitalizations, ER visits, and disease progression [28].
The use of a corticosteroid by patients on a DMT may be indicative of a relapse and that the DMT may be suboptimal for those patients. Patient response to a DMT may not be immediate, so a mild relapse may occur while using a DMT. However, failure to switch DMT following multiple steroid treatments may indicate clinical inertia, in which treatment is not changed despite apparent therapy failure [15]. The low proportion of patients changing their DMT after receiving corticosteroids in the present study possibly suggests clinical inertia among the Medicare patient population, particularly among those who received ≥ 2 corticosteroid treatments. However, most patients treated with a corticosteroid during the baseline period only received the corticosteroid once, which may suggest that the study duration was not long enough to detect multiple steroid treatments, or alternatively, that the DMTs patients are currently using are adequately controlling their MS, depending on the patient’s and physician’s limit of tolerance for disease activity. DMT switching may also be driven by factors other than disease activity, for example, poor tolerability, which may confound the analysis of switching as it relates to corticosteroid treatment. Another factor that may affect treatment switching is immunosenescence that may occur as patients age, and which represents a challenge when considering immunosuppressive therapies [30]. We observed patients switching away from natalizumab treatment in the Medicare population, particularly those with ≥ 2 episodes of corticosteroid use. This suggests natalizumab inefficacy in this population, but does not rule out a potential safety concern. Of the Medicare patients who did switch DMT, most switches were from an injectable to an oral medication, consistent with a trend toward oral therapies for MS patients [16, 31].
HCRU and HCCs showed a different pattern among Medicare MS patients receiving DMT compared with those not receiving DMT. Pharmacy service use, pharmacy costs, and total costs were higher for those receiving a DMT regardless of whether they received corticosteroid treatment. However, DMT use was associated with fewer corticosteroid treatments (potentially indicating fewer relapses), fewer all-cause hospitalization episodes and ER visits, and lower all-cause medical costs, indicative of better health outcomes. The lower overall HCRU and HCCs associated with DMT use were observed both in patients who did and did not receive corticosteroid treatments, raising the possibility that DMT use lessens relapse severity.
Beyond its retrospective nature, this study has several limitations that should be considered when interpreting the current findings. These findings are only applicable to the patients identified in the study population and may not be applicable to a larger population. Administrative claims data are limited in scope; information on the severity and type of MS disease is not readily available. Use of steroids may not always reflect relapse, particularly in patients with increased disability. However, the data show decreased use of corticosteroids in DMT-treated patients, regardless of the reason for corticosteroid use. Furthermore, cormorbidity incidence was similar in patients with and without DMT, arguing against the possibility that increased comorbidities in patients without DMT drove their increased corticosteroid use. Finally, a longer baseline period than the 12-month period utilized in the present study may provide additional information on DMT utilization patterns, frequency of corticosteroid treatment, and treatment switching behavior.
Conclusions
Given the chronic, progressive nature of MS, resource utilization and costs are expected to escalate as the patients age. This descriptive claims-based study examining patients with MS in Medicare shows a population with significant HCRU and costs. The majority of the cost burden was directly related to the treatments for MS; however, DMT treatment lowered all-cause medical costs. Although many Medicare patients received corticosteroid treatment for relapse, few switched their DMT during the 12-month timeframe, suggesting an opportunity to further optimize therapy for this population (as well as the commercially insured population). Further studies are needed to understand the factors driving these treatment patterns.
References
Lublin FD, Reingold SC, Cohen JA, et al. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology. 2014;83:278–86.
National Multiple Sclerosis Society. Estimating the prevalence of MS. Available from: http://www.nationalmssociety.org/About-the-Society/MS-Prevalence. Accessed 24 Oct 2018.
National Multiple Sclerosis Society. Who gets MS? Available from: http://www.nationalmssociety.org/What-is-MS/Who-Gets-MS. Accessed 24 Oct 2018.
Simpson RJ, McLean G, Guthrie B, Mair F, Mercer SW. Physical and mental health comorbidity is common in people with multiple sclerosis: nationally representative cross-sectional population database analysis. BMC Neurol. 2014;14:128.
Ford HL, Gerry E, Johnson MH, Tennant A. Health status and quality of life of people with multiple sclerosis. Disabil Rehabil. 2001;23:516–21.
Forbes A, While A, Mathes L, Griffiths P. Health problems and health-related quality of life in people with multiple sclerosis. Clin Rehabil. 2006;20:67–78.
Marrie RA, Patten SB, Tremlett H, et al. Sex differences in comorbidity at diagnosis of multiple sclerosis: a population-based study. Neurology. 2016;86:1279–86.
Zhang T, Tremlett H, Leung S, et al. Examining the effects of comorbidities on disease-modifying therapy use in multiple sclerosis. Neurology. 2016;86:1287–95.
Marrie R, Horwitz R, Cutter G, Tyry T, Campagnolo D, Vollmer T. Comorbidity, socioeconomic status and multiple sclerosis. Mult Scler. 2008;14:1091–8.
Margolis JM, Fowler R, Johnson BH, Kassed CA, Kahler K. Disease-modifying drug initiation patterns in commercially insured multiple sclerosis patients: a retrospective cohort study. BMC Neurol. 2011;11:122.
Lublin FD, Baier M, Cutter G. Effect of relapses on development of residual deficit in multiple sclerosis. Neurology. 2003;61:1528–32.
Gold R, Wolinsky JS, Amato MP, Comi G. Evolving expectations around early management of multiple sclerosis. Ther Adv Neurol Disord. 2010;3:351–67.
National Multiple Sclerosis Society. Medications. Available from: http://www.nationalmssociety.org/Treating-MS/Medications#section-3. Accessed 24 Oct 2018.
Bonafede MM, Johnson BH, Wenten M, Watson C. Treatment patterns in disease-modifying therapy for patients with multiple sclerosis in the United States. Clin Ther. 2013;35:1501–12.
Morris K, Yiannikas C. Treatment update in multiple sclerosis. Curr Allergy Asthma Rep. 2012;12:246–54.
Cross AH, Naismith RT. Established and novel disease-modifying treatments in multiple sclerosis. J Intern Med. 2014;275:350–63.
Munsell M, Frean M, Menzin J, Phillips AL. An evaluation of adherence in patients with multiple sclerosis newly initiating treatment with a self-injectable or an oral disease-modifying drug. Patient Prefer Adherence. 2017;11:55–62.
Bergvall N, Petrilla AA, Karkare SU, et al. Persistence with and adherence to fingolimod compared with other disease-modifying therapies for the treatment of multiple sclerosis: a retrospective US claims database analysis. J Med Econ. 2014;17:696–707.
National Multiple Sclerosis Society. Recommendations regarding corticosteroids in the management of multiple sclerosis. Available from: https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical_Bulletin_Corticosteroids-in-Management-of-MS.pdf. Accessed 24 Oct 2018.
McQueen RB, Livingston T, Vollmer T, et al. Increased relapse activity for multiple sclerosis natalizumab users who become nonpersistent: a retrospective study. J Manag Care Spec Pharm. 2015;21:210–8b.
Sanchirico M, Ma I, Caldwell-Tarr A, Hashemi L, Mudumby P, Dufour R. Real-world healthcare resource utilization and treatment switching patterns in multiple sclerosis patients in a large US health plan. Mult Scler. 2016;22:EP1546.
Sanai SA, Saini V, Benedict RH, et al. Aging and multiple sclerosis. Mult Scler. 2016;22:717–25.
DiLorenzo T. National Multiple Sclerosis Society. Aging with multiple sclerosis. Available from: http://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical-Bulletin-Aging.pdf. Accessed 24 Oct 2018.
Zwibel HL, Smrtka J. Improving quality of life in multiple sclerosis: an unmet need. Am J Manag Care. 2011;17(Suppl 5):S139–45.
Ponzio M, Brichetto G, Zaratin P, Battaglia MA. Workers with disability: the case of multiple sclerosis. Neurol Sci. 2015;36:1835–41.
Bass A, Van Wijmeersch B, Mayer L, et al. Impact of multiple sclerosis on patients’ daily activities, emotional well-being and relationships: results of the global vsMS™ survey. Neurology. 2017;88(16 Suppl):P3.334.
Pozniak A, Hadden L, Rhodes W, Minden S. Change in perceived health insurance coverage among people with multiple sclerosis. Int J MS Care. 2014;16:132–9.
Remington G, Rodriguez Y, Logan D, Williamson C, Treadaway K. Facilitating medication adherence in patients with multiple sclerosis. Int J MS Care. 2013;15:36–45.
Halpern R, Agarwal S, Dembek C, Borton L, Lopez-Bresnahan M. Comparison of adherence and persistence among multiple sclerosis patients treated with disease-modifying therapies: a retrospective administrative claims analysis. Patient Prefer Adherence. 2011;5:73–84.
Grebenciucova E, Berger JR. Immunosenescence: the role of aging in the predisposition to neuro-infectious complications arising from the treatment of multiple sclerosis. Curr Neurol Neurosci Rep. 2017;17:61.
Weinstock-Guttman B. An update on new and emerging therapies for relapsing-remitting multiple sclerosis. Am J Manag Care. 2013;19:s343–54.
Acknowledgements
Funding
This study and the article processing charges were funded by Sanofi (Cambridge, MA, USA). All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Medical Writing and/or Editorial Assistance
Editorial assistance in the preparation of this article was provided by David R. Thomas, PhD, and Valerie P. Zediak, PhD, of Envision Scientific Solutions, and funded by Sanofi.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
The study was conceived and designed by authors Sanchirico, Caldwell-Tarr, Mudumby, and Dufour. Analyses were performed by Pallavi Mudumby. The manuscript was reviewed for content and revised by all authors.
Prior Presentation
Aspects of this work have been presented previously at the 7th Joint European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS)–Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) Meeting, October 25–28, 2017, Paris, France, the 20th Annual European Conference of the International Society for Pharmacoeconomics Outcomes Research (ISPOR), November 4–8, 2017, Glasgow, UK, and the 30th Annual Meeting of the Academy of Managed Care and Specialty Pharmacy (AMCP) April 23–26, 2018, Boston, MA, USA.
Disclosures
Comprehensive Health Insights, a Humana Company, received funding from Sanofi to conduct this study. Marie Sanchirico is an employee of Sanofi. Lobat Hashemi is an employee of Sanofi. Amanda Caldwell-Tarr was an employee of Comprehensive Health Insights, a Humana Company, at the time the analysis was performed; currently an employee of HealthCore. Pallavi Mudumby is an employee of Comprehensive Health Insights, a Humana Company, Robert Dufour was an employee of Comprehensive Health Insights, a Humana Company, at the time the analysis was performed; currently an employee of Vector Oncology.
Compliance with Ethics Guidelines
The current study was reviewed and approved by an institutional review board, Schulman Associates IRB, Inc, before study initiation. All procedures performed in this study were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article is based on healthcare claims data and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Qualified researchers may request access to patient-level data and related study documents including the clinical study report, study protocol with any amendments, blank case report form, statistical analysis plan, and dataset specifications. Patient-level data will be anonymized and study documents will be redacted to protect the privacy of trial participants. Further details on Sanofi’s data sharing criteria, eligible studies, and process for requesting access can be found at: https://www.clinicalstudydatarequest.com.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7387358.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Sanchirico, M., Caldwell-Tarr, A., Mudumby, P. et al. Treatment Patterns, Healthcare Resource Utilization, and Costs Among Medicare Patients with Multiple Sclerosis in Relation to Disease-Modifying Therapy and Corticosteroid Treatment. Neurol Ther 8, 121–133 (2019). https://doi.org/10.1007/s40120-018-0123-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-018-0123-y