Abstract
We present four cases with Gram-positive bacteremia (pathogens: MRSA n = 1, Enterococcus spp. n = 3) due to an intravascular source (left ventricular assist device: n = 2, transfemoral aortic valve implantation n = 1, prosthetic aortic valve: n = 1) where no curative treatment was available. These patients received indefinite, chronic suppressive (palliative) therapy with dalbavancin (500 mg weekly or 1000 mg biweekly regimens). Outcomes and clinical characteristics are described; treatment was effective in suppression of bacteremia in all patients over several months (range: 1 to more than 12 months), we observed no relevant side effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Long-term suppressive therapy is a last option in patients with chronic bacterial infections, consisting of substances that are well tolerated, have good oral bioavailability and antimicrobial activity. Unfortunately, in some cases not all of these options are available. This might either be due to resistance of the pathogens involved or side effects in patients.
Dalbavancin is a lipoglycopeptide with an exceptional long terminal half-life that was licensed for the treatment of skin and soft tissue infections. It is not licensed for bacteremia, although it is broadly used for this specific indication [1, 2]. It has broad activity against Gram-positive bacteria including methicillin-resistant Staphylococcus aureus (MRSA), coagulase-negative staphylococci (CoNS, such as S. epidermidis, S. haemolyticus) and enterococci (E. faecalis and E. faecium). Its long half-life of more than 14 days allows weekly or biweekly infusions [3] making it an attractive choice for outpatient antibiotic treatment.
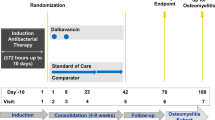
We present a series of four patients with Gram-positive bacteremia due to an intravascular source, where dalbavancin was used as suppressive, indefinite therapy after prior intravenous therapy with different substances.
Methods
All patients were seen by an infectious diseases specialist before initiating dalbavancin treatment and in all cases oral suppressive therapy was deemed not feasible.
In all four patients a broad interdisciplinary consensus for chronic suppressive therapy was established. Conventional therapy was mainly limited by comorbidities, side effects including allergies and a lack of other (non-antibiotic) options (e.g., surgery and appropriate focus control).
All patients provided informed consent for dalbavancin off-label use. The health insurances involved were informed about the off-label use of dalbavancin and funding was requested and approved.
Dalbavancin was started after clearance of bacteremia. In all cases dalbavancin was infused by the patients` general practitioner on an out-patient basis.
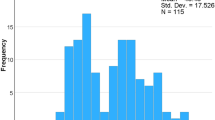
The isolated organisms (including resistance patterns) are listed in Table 1 together with a short synopsis of the clinical course. Dalbavancin susceptibility testing was not available, but all pathogens involved were susceptible to glycopeptides (vancomycin).
Patient 1
An 81-year-old male patient was transferred to our hospital in June 2018 with methicillin-resistant S. aureus (MRSA) bacteremia and a previous history of prosthetic aortic valve replacement in 2001. Transesophageal echocardiography (TEE) showed endocardial vegetations (8 × 5 mm, aortic valve) leading to the diagnosis of prosthetic valve endocarditis (two major DUKE criteria positive).
After initial treatment with vancomycin antibiotic therapy was switched to daptomycin (8 mg/kg) plus rifampicin (2 × 450 mg) and i.v. treatment was continued for 6 weeks. Blood cultures (BC) cleared within several days, no complications arose during the hospital stay.
Twelve days after discharge the patient was readmitted to a different hospital and BC grew MRSA again. The resistance profile showed that linezolid would be the only oral treatment option available. The patient was transferred to our hospital where cardiothoracic surgeons judged major cardiac surgery not feasible because of comorbidities and the patient’s general condition.
The patient was treated with linezolid initially for several days before dalbavancin was administered once weekly (loading dose 1000 mg, followed by 350 mg weekly—dose adjusted for renal insufficiency—GFR CKD-EPI 23 ml/min/1.73qm).
The patient received dalbavancin only twice, before he was readmitted in the beginning of October 2018 with acute decompensated heart failure and transferred to another hospital. He died in November 2018 due to heart failure and kidney failure. There was no clinical suspicion of relapse of MRSA bacteremia, but no BCs were obtained.
Patient 2
A 59-year-old male patient was admitted to an intensive care unit in our hospital with acute bowel obstruction in September 2018. The patient had a previous history of neuroendocrine neoplasm (NEN). Due to end-stage heart failure (dilated cardiomyopathy (DCM)), a left ventricular assist device (LVAD) had been implanted in June 2018. After laparotomy and adhesiolysis, the patient recovered but then developed an episode of Clostridioides difficile infection (CDI) after broad spectrum antibiotic therapy. During treatment with oral vancomycin, the patient developed fever and Enterococcus faecium (E. faecium) as well as two different species of coagulase-negative staphylococci (S. epidermidis and S. haemolyticus) were isolated from his blood, all of them in several different BC sets.
The patient was treated with intravenous vancomycin (target trough serum concentration: 15–20 mcg/ml) and later switched to daptomycin (10 mg/kg once daily). Subsequent BCs remained sterile under intravenous therapy. A PET/CT was performed where an infection of the LVAD was suspected. Owing to his general clinical condition and his history of NEN the patient was neither considered a candidate for heart transplantation nor for LVAD exchange. Dalbavancin was offered as salvage therapy. The once weekly infusion was performed by the general practitioner of the patient (loading dose 1000 mg, followed by 500 mg weekly).
He was readmitted several times during the following year (for different reasons: recurrent CDI, acute renal failure; both under dalbavancin therapy, both resolved despite continued dalbavancin infusions). There was no recurrence of bacteremia. A PET/CT performed nearly 1 year after initiating dalbavancin showed evidence of still active LVAD infection and dalbavancin therapy was continued.
At the latest follow-up (more than 1 year of dalbavancin treatment) the patient was in stable condition.
Patient 3
A 67-year-old male patient was admitted with fever and chills to our hospital in May 2019. He had a history of hairy cell leukemia and toxic cardiomyopathy (gladribine-induced) with LVAD implanted January 2019.
After admission treatment with vancomycin and piperacillin/tazobactam was started. Two days later, two BCs taken at admission grew Enterococcus faecalis (E. faecalis). I.v. therapy with piperacillin/tazobactam had to be stopped due to an allergic reaction (rash). Vancomycin was continued and lead to clearance of bacteremia.
Again, like in the previously described patient neither heart transplantation nor LVAD exchange (with high surgical risk) was a suitable option for this patient according to an interdisciplinary consensus.
With E. faecalis bacteremia in this penicillin-allergic patient dalbavancin chronic suppressive palliative therapy was offered to the patient and started in the end of May 2019 (loading 1000 mg, followed by 500 mg weekly). Since no other focus could be established the LVAD was considered to be the most likely source of bacteremia.
The patients did fine on an outpatient revisit two months later. He was, however, readmitted in October 2019 with sepsis and E. faecalis breakthrough bacteremia despite continued dalbavancin therapy (500 mg weekly). He was again treated with vancomycin and cleared bacteremia. Since there were no other options available, dalbavancin was re-administered (loading 1000 mg, followed by 500 mg weekly) and the patient was discharged from our hospital.
He was again re-admitted in the end of November 2019 with (most likely LVAD associated ischemic) stroke. BCs, however, were negative at admission and during his hospital stay. He died in December 2019 due to complications of stroke.
Patient 4
An 80-year-old male patient was admitted with fever in September 2019. He had a previous history of transcatheter aortic valve implantation (TAVI) due to aortic valve stenosis in May 2016 and several other chronic conditions (chronic renal failure, diabetes, chronic osteomyelitis of the calcaneus, total knee endoprosthesis, early stages of dementia). He was in reduced general condition due to age and comorbidities. BCs grew E. faecalis.
During the hospital stay, a thorough work-up was repeated. TEE showed no vegetations on the aortic valve. CT scan, however, revealed septic emboli in kidneys, spleen and brain, leading to the diagnosis of TAVI endocarditis (based on one major and three minor DUKE criteria).
The calcaneus was evaluated by orthopedic surgeons and surgery with amputation was recommended. The patient, however, refused both heart surgery and amputation. Simultaneously, he was deemed not operable owing to his age and comorbidities.
Unfortunately, he had an amoxicillin allergy (rash); amoxicillin re-exposure was tried during the hospital stay, but again, he developed a severe generalized rash.
An oral treatment with moxifloxacin 1 × 400 mg and rifampicin 1 × 600 mg was attempted after several weeks of intravenous therapy (and negative BCs). Although doing well initially under oral therapy, the patient was seen on an outpatient appointment (in October 2019) and relapse of E. faecalis bacteremia could be documented. A short treatment course with linezolid over only several days failed due to poor tolerability (nausea).
The patient was readmitted and treated with vancomycin intravenously (and piperacillin, which he tolerated despite his amoxicillin allergy) leading to clearance of bacteremia. After 4 weeks of treatment, the patient was discharged from the hospital (at the beginning of December 2019) with dalbavancin therapy (1500 mg loading, followed by 1000 mg biweekly).
Until March 2020 there was still no clinical sign of bacteremia. A minor rash after the administration of dalbavancin did not lead to discontinuation of the drug. However, his general condition worsened, and the treatment protocol was changed to best supportive care. The patient died in April 2020.
Discussion
We present four patients with bacteremia caused by Gram-positive cocci due to an intravascular source. All patients had cardiovascular foreign bodies implanted and finally received (or continue to receive) indefinite suppressive therapy with dalbavancin after prior intravenous therapy with other substances.
Patient 1 was treated with dalbavancin only twice, but he could be discharged home and was stable for roughly 4 weeks (2 weeks linezolid and 2 weeks dalbavancin combined), before he was readmitted.
Although dalbavancin therapy was not effective in preventing relapse of infection in patient 3, he did fine for several months after the initial diagnosis of bacteremia and was able to stay at home most of the time after discharge (more than 5 months) which can be considered as a success of suppressive therapy.
The possibility exists, that patient 2 does not have true LVAD infection, but several BC sets were repeatedly positive for different pathogens and PET/CT was suggestive for LVAD infection. On the other hand, antibiotic therapy was never stopped to document recurrence of bacteremia since this was judged be too high of a risk in a patient with severe heart failure. He was also the only patient of our small series, where dalbavancin was started right after the cessation of the previous intravenous therapy (with no oral treatment in between).
Patient 4 also received dalbavancin and the treatment was effective for several months. The only other option for this patient would have been continued vancomycin treatment (due to his renal insufficiency once daily), but implementation would have been much more complicated in an outpatient setting.
These four patients share some unique features:
-
1. All had bacterial infection of a prosthetic device and a curative approach (surgical removal) was not possible.
-
2. There was always broad interdisciplinary consensus that a relapse of bacteremia would inevitably happen if antibiotics were stopped.
-
3. Oral substances for chronic suppressive therapy were not available, not feasible or not effective and an intravenous therapy offered the advantage of higher drug levels in the blood. The long half-life of dalbavancin offers the further advantage of a nearly comfortable dosing interval, even in an outpatient setting.
All isolated pathogens were also susceptible to linezolid. However, problems with myelotoxicity in long-term use are well described in the literature [4] and reflect our own clinical experience. Furthermore, linezolid lacks bactericidal activity of dalbavancin. Outpatient parenteral antimicrobial therapy (OPAT) is not well established in our region and problems arise frequently especially during weekends and on holidays. A once weekly or biweekly infusion is preferable, and implementation is easier.
Patients have been treated with dalbavancin for endocarditis before [1, 5] and a case report describes the (successful) suppressive therapy of MRSA prosthetic valve endocarditis [6]. Dalbavancin was also effective as suppressive therapy in a patient with MRSA LVAD infection (however this patient was not bacteremic) [7]. In a letter to the editor Cicullo et al. describe the case of a patient with MRSA bacteremia and an abdominal aortic prothesis, where dalbavancin was used and resulted in cure of infection [8]. Dalbavancin may also be effective in biofilm-forming infections, as previous in-vitro studies suggest [9]. On the other side dalbavancin treatment in chronic osteomyelitis resulted in poor outcomes (cure rate of less than 40%) [10]. Overall, off label use of dalbavancin is common and the substance seems to be an acceptable safe alternative to other intravenous options even in patients with bacteremia.
The ideal dosing regimen for dalbavancin in this setting is still unclear. Several different regimens are published in the literature:
-
1. 1000 mg loading dose, followed by 500 mg weekly [1].
-
2. 1500 mg loading dose, followed by 1000my biweekly [4].
-
3. 1500 mg weekly [7].
Wunsch et al. describe 25 patients with endocarditis and a third of these patients were treated with the same regime as the patients from our series (36% received dalbavancin only once) [1]. Most (63%), but not all patients with endocarditis in the retrospective study of Tobudic et al. were treated with the biweekly regimen [5]. Patients with endocarditis in the Spanish DALBACEN cohort were treated with both dosing regimens also [11].
A completely different approach was applied by Spaziante et al., where serum dalbavancin concentrations were monitored and dosing was managed via drug monitoring [6]. The authors note, however, that the appropriate target concentration for guiding dalbavancin dosing intervals is not yet established.
Although we used the weekly regimen in three of our patients, we do see the benefit in the biweekly approach (meaning less frequent infusions). Drug monitoring would be the optimal approach for monitoring of dalbavancin in our opinion.
Within our limited experience we could not see any relevant side effects of long-term dalbavancin treatment. Two of our patients (No. 2 and 3) received dalbavancin for several months without any documented problems. Patient No. 4 developed a mild rash, which did not lead to discontinuation of the substance. Other studies also documented a low rate of side effects: in one study 5% of patients receiving dalbavancin did experience nausea or rash [10].
Long-term, even indefinite suppressive therapy is a decision on a case-by-case basis and needs to be discussed with the patient and all people involved in patient management (relatives, general practitioner, nursing service, etc.). Long-term side effects of dalbavancin therapy cannot be ruled out with the data of our small case series and patients must be followed closely. Overall tolerance, however, was good in our patients.
Conclusions
Dalbavancin is an attractive option for outpatient antibiotic therapy including patients in need for a long-term suppressive therapy. Therapy with dalbavancin might be considered in patients with Gram-positive bacteremia due to an intravascular source as a salvage option when other options (such as oral antibiotics) are not available or not feasible. Long-term therapy seems to be well tolerated in these patients with few side effects. Although only once weekly or biweekly application is necessary long-term suppressive therapy still requires a huge effort on several sides (general practitioner, patient, health insurance, nursing service, etc.). Of note, the optimal dosing strategy is still a matter of debate and might depend on several factors. Drug monitoring might possibly be helpful to monitor drug levels and prevent long-term drug accumulation.
References
Wunsch S, Krause R, Valentin T, Prattes J, Janata O, Lenger A, et al. Multicenter clinical experience of real life Dalbavancin use in gram-positive infections. Int J Infect Dis. 2019;81:210–4.
Hakim A, Braun H, Thornton D, Strymish J. Successful treatment of methicillin-sensitive Staphylococcus aureus tricuspid-valve endocarditis with dalbavancin as an outpatient in a person who injects drugs: a case report. Int J Infect Dis. 2020;91:202–5.
Scott LJ. Dalbavancin: a review in acute bacterial skin and skin structure infections. Drugs. 2015;75:1281–91.
Kishor K, Dhasmana N, Kamble S, Sahu R. Linezolid induced adverse drug reactions—an update. Curr Drug Metab. 2015;16:553–9.
Tobudic S, Forstner C, Burgmann H, Lagler H, Ramharter M, Steininger C, et al. Dalbavancin as primary and sequential treatment for gram-positive infective endocarditis: 2-year experience at the General Hospital of Vienna. Clin Infect Dis. 2018;67:795–8.
Spaziante M, Franchi C, Taliani G, D’Avolio A, Pietropaolo V, Biliotti E, et al. Serum bactericidal activity levels monitor to guide intravenous dalbavancin chronic suppressive therapy of inoperable staphylococcal prosthetic valve endocarditis: a case report. Open Forum Infect Dis. 2019;6:ofz427.
Howard-Anderson J, Pouch SM, Sexton ME, Mehta AK, Smith AL, Lyon GM, et al. Left ventricular assist device infections and the potential role for dalbavancin: a case report. Open Forum Infect Dis. 2019;6:ofz235.
Ciccullo A, Giuliano G, Segala FV, Taddei E, Farinacci D, Pallavicini F. Dalbavancin as a second-line treatment in methicillin-resistant Staphylococcus aureus prosthetic vascular graft infection. Infection. 2020;48:309–10.
Knafl D, Tobudic S, Cheng SC, Bellamy DR, Thalhammer F. Dalbavancin reduces biofilms of methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-resistant Staphylococcus epidermidis (MRSE). Eur J Clin Microbiol Infect Dis. 2017;36:677–80.
Tobudic S, Forstner C, Burgmann H, Lagler H, Steininger C, Traby L, et al. Real-world experience with dalbavancin therapy in gram-positive skin and soft tissue infection, bone and joint infection. Infection. 2019;47:1013–20.
Hidalgo-Tenorio C, Vinuesa D, Plata A, Martin Dávila P, Iftimie S, Sequera S, et al. DALBACEN cohort: dalbavancin as consolidation therapy in patients with endocarditis and/or bloodstream infection produced by gram-positive cocci. Ann Clin Microbiol Antimicrob. 2019;18:30.
Iversen K, Ihlemann N, Gill SU, Madsen T, Elming H, Jensen KT, et al. Partial oral versus intravenous antibiotic treatment of endocarditis. N Engl J Med. 2019;380:415–24.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All authors contributed to the design of the case series. Data collection and analysis were performed by FHi, AM and FH. The first draft of the manuscript was written by FHi and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Hitzenbichler: travel grants from Gilead Sciences, lecture fees from MSD. Mohr: travel grants from Gilead Sciences. Camboni: no conflicts of interest. Simon: lecture fees from Becton Dickinson, grants from Pfizer. Salzberger: advisory and lecture fees from Falk Foundation, GSK, Roche, Sanofi; research grants from Bosch-Stiftung, GSK, Biochryst. Hanses: advisory and lecture fees from Correvio.
Ethical approval
The study was reviewed and approved by the local ethics committee of the University of Regensburg (number 19-1257-101).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hitzenbichler, F., Mohr, A., Camboni, D. et al. Dalbavancin as long-term suppressive therapy for patients with Gram-positive bacteremia due to an intravascular source—a series of four cases. Infection 49, 181–186 (2021). https://doi.org/10.1007/s15010-020-01526-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-020-01526-0